Hypnosis Sedation Reduces the Duration of Different Side Effects of Cancer Treatments in Breast Cancer Patients Receiving Neoadjuvant Chemotherapy
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Population and Data Collection
2.2. Description of Hypnosis Sedation Procedure and General Anesthesia
2.3. Polyneuropathy
2.4. Postoperative Pain
2.5. Musculoskeletal Pain
2.6. Cancer-Related Fatigue
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PNP | Polyneuropathy |
| MSP | Musculoskeletal pain |
| POP | Post-operative pain |
| CRF | Cancer-related fatigue |
| PNP intensity | MI = mild; MO = moderate; SE = severe |
| NA | Not assessed because absent |
| D0 | Date of surgical procedure, day 0 |
| D1 | Post-surgical procedure, day 1 |
| D8 | Post-surgical procedure, day 8 |
| M3 | Date of oncology follow-up, month 3 |
| M | Date of oncology follow-up, month 6 |
| M9 | Date of oncology follow-up, month 9 |
| M12 | Date of oncology follow- up, month 12 |
| M15 | Date of oncology follow-up, month 15 |
| M18 | Date of oncology follow-up, month 18 |
| M21 | Date of oncology follow-up, month 21 |
| M24 | Date of oncology follow-up, month 24 |
References
- Berlière, M.; Roelants, F.; Watremez, C.; Docquier, M.A.; Piette, N.; Lamerant, S.; Megevand, V.; Van Maanen, A.; Piette, P.; Gerday, A.; et al. The advantages of hypnosis intervention on breast cancer surgery and adjuvant therapy. Breast 2018, 37, 114–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lacroix, C.; Duhoux, F.P.; Bettendorff, J.; Watremez, C.; Roelants, F.; Docquier, M.-A.; Potié, A.; Coyette, M.; Gerday, A.; Samartzi, V.; et al. Impact of perioperative hypnosedation on postmastectomy chronic pain: Preliminary results. Integr. Cancer Ther. 2019, 18, 1534735419869494. [Google Scholar] [CrossRef]
- Swain, S.M.; Arezzo, J.C. Neuropathy associated with microtubiles inhibitors: Diagnosis, incidence and management. Clin. Adv. Hematol. Oncol. 2008, 6, 455–467. [Google Scholar] [PubMed]
- Park, S.B.; Goldstein, D.; Krishnan, A.V. Chemotherapy-induced peripheral neurotoxicity: A critical analysis. Cancer J. Clin. 2013, 63, 419–437. [Google Scholar] [CrossRef] [PubMed]
- Eckhoff, L.; Knoop, A.; Jansen, M.; Ewertz, M. Persistence of docetaxel-induced neuropathy and impact on quality of life among breast cancer survivors. Eur. J. Cancer 2015, 51, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Hurtz, H.J.; Tesch, H.; Göhler, T.; Hutzschenreuter, U.; Harde, J.; Kruggel, L.; Jänicke, M.; Marschner, N.; TM-Group (Tumour Registry Breast Cancer). Persistent impairments 3 years after (neo)adjuvant chemotherapy for breast cancer: Results from the MaTox project. Breast Cancer Res. Treatment 2017, 165, 721–731. [Google Scholar] [CrossRef] [Green Version]
- Ciruelos, E.; Apellaniz-Ruiz, M.; Cantos, B.; Martinez-Janez, N.; Bueno-Muino, C.; Echarri, M.J.; Enrech, S.; Guerra, J.A.; Manso, L.; Pascual, T.; et al. A pilot, phase II randomized, open-label clinical trial comparing the neurotoxicity of three dose regimens of nab-Paclitaxel to that of solvent-based paclitaxel as the first line treatment for patients with Human epidermal Growth Factor receptor Type 2-negative metastatic breast cancer. Oncologist 2019, 24, e1024–e1033. [Google Scholar]
- Ilhan, E.; Chee, E.; Kush, J.; Moloney, N. The prevalence of neuropathic pain is high after treatment for breast cancer. Pain 2017, 158, 2082–2091. [Google Scholar] [CrossRef]
- Postma, T.J.; Aaronson, N.K.; Heimans, J.J.; Muller, M.J.; Hildebrand, J.G.; Delattre, J.Y.; Hoang-Xuan, K.; Lantéri-Minet, M.; Grant, R.; Huddart, R.; et al. The development of an EORTC quality of life questionnaire to assess chemotherapy-induced peripheral neuropathy: The QLQ-CIPN20. Eur. J. Cancer 2005, 41, 1135–1139. [Google Scholar] [CrossRef]
- Niravath, P. Aromatase inhibitor-induced arthralgia: A review. Ann. Oncol. 2013, 24, 1443–1449. [Google Scholar] [CrossRef]
- Wang, L.; Guyatt, G.H.; Kennedy, S.A.; Romerosa, B.; Kwon, H.Y.; Kaushal, A.; Chang, Y.; Craigie, S.; de Almeida, C.P.B.; Couban, R.J.; et al. Predictors of persistent pain after breast cancer surgery: A systematic review and meta-analysis of observational studies. Can. Med. Assoc. J. 2016, 11, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Hamood, R.; Hamood, H.; Merhasin, I.; Keinan-Boer, L. Chronic pain and other symptoms among breast cancer survivors: Prevalence, predictors and effects on quality of life. Breast Cancer Res. Treat. 2017, 167, 157–169. [Google Scholar] [CrossRef]
- Lancaster, R.B.; Balkin, D.; Esserman, L. Post-mastectomy pain syndrome management. Curr. Surf. Rep. 2016, 4, 6. [Google Scholar] [CrossRef]
- Alves Nogueira Fabro, E.; Bergmann, A.; do Amaral, E.; Silva, B.; Padula Ribeiro, A.C.; de Souza Abrahao, K.; de Costa Leite Ferreira, M.G.; de Almeida Dias, R.; Santos Thuler, L.C. Post-mastectomy pain syndrome: Incidence and risks. Breast 2012, 21, 321–325. [Google Scholar] [CrossRef]
- Andersen, K.G.; Kehlet, H. Persistent pain after breast cancer treatment: A critical review of risk factors and strategies for prevention. J. Pain 2011, 12, 725–746. [Google Scholar] [CrossRef]
- Gärtner, R.; Jensen, M.; Nielsen, J.; Ewertz, M.; Kroman, N.; Kehlet, H. Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA 2009, 302, 1985–1992. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kehlet, H.; Jensen, T.S.; Woolf, C.J. Persistent postsurgical pain: Risk factors and prevention. Lancet 2006, 367, 1618–1625. [Google Scholar] [CrossRef]
- Jensen, M.P.; Chang, H.Y.; Lai, Y.H.; Syrjala, K.L.; Fann, J.R.; Gralow, J.R. Pain in long-term breast cancer survivors: Frequency, severity, and impact. Pain Med. 2010, 11, 1099–1106. [Google Scholar] [CrossRef] [Green Version]
- Meretoja, T.J.; Andersen, K.J.; Bruce, J.; Haasio, L.; Sipilä, R.; Scott, N.W.; Ripatti, S.; Kehle, H.; Kalso, M.E.A. Clinical prediction modelland tool for assessing risk of persistent pain after breast cancer surgery. J. Clin. Oncol. 2017, 35, 1660–1667. [Google Scholar] [CrossRef]
- Fabi, A.; Bargava, R.; Fatigoni, S.; Guglielmo, M.; Horneber, M.; Roila, F.; Weis, J.; Jordan, K.; Ripamonti, C.I. On behalf of the ESMO guidelines Committee. Cancer-related fatigue: ESMO Clinical practice Guidelines for diagnosis and treatment. Ann. Oncol. 2020, 31, 713–722. [Google Scholar] [CrossRef]
- Donovan, K.A.; McGinty, H.L.; Jacobsen, P.B. A systematic review of research using the diagnostic criteria for cancer-related fatigue. Psychooncology 2013, 22, 737–744. [Google Scholar] [CrossRef]
- Berger, A.M.; Mitchell, S.A.; Jacobse, P.B.; Pirl, W.F. Screening, evaluation, and management of cancer-related fatigue: Ready for implementation to practice? CA Cancer J. Clin. 2015, 65, 190–211. [Google Scholar] [CrossRef]
- Berger, A.M.; Moone, K.; Alarez-Perez, A.; Breibart, W.S.; Carpenter, K.M.; Cella, D.; Cleeland, C.; Dotan, E.; Eisenberger, M.A.; Escalante, C.P.; et al. Cancer-related fatigue, version 2.2015: Clinical practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2015, 13, 1012–1039. [Google Scholar] [CrossRef]
- R Core Team. A Language and Environment for Statistical Computing; R. Foundation for Statistical Computing: Vienna, Austria, 2021; Available online: https://www.R.project.org/ (accessed on 24 May 2021).
- Forget, P.; Sitter, T.M.; Hollick, R.J.; Dixon, D.; Van Maane, A.; Dekleermaker, A.; Duhoux, F.P.; De Kock, M.; Berliere, M.; On behalf of the KBCt Group. Characterization of Preoperative, Postsurgical, Acute and Chronic Pain in High Risk Breast Cancer Patients. J. Clin. Med. 2020, 9, 3831. [Google Scholar] [CrossRef] [PubMed]
- Gewandter, J.S.; Kleckner, A.S.; Marshall, J.H.; Brown, J.S.; Curtis, L.H.; Nautista, J.; Dworkin, R.H.; Klecner, I.R.; Kolb, N.; Mohile, S.G.; et al. Chemotherapy-induced peripheral neuropathy (CIPN) and its treatment: An NIH collaboratory study of claims data. Support Care Cancer 2020, 28, 2553–2562. [Google Scholar] [CrossRef] [PubMed]
- Jordan, B.; Jahn, F.; Sauer, S.; Jordan, K. Prevention and Management of Chemotherapy-Induced Polyneuropathy. Breast Care 2019, 14, 79–84. [Google Scholar] [CrossRef]
- Liampas, A.; Rekatsina, M.; Vadalouca, A.; Paladini, A.; Varrassi, G.; Panagiotis, Z. Pharmacological Management of Painful Peripheral Neuropathies: A Systematic Review. Pain Ther. 2021, 10, 55–68. [Google Scholar] [CrossRef]
- Seretny, M.; Currie, G.L.; Sena, E.S.; Ramnarine, S.; Grant, R.; MacLeod, M.R.; Colvin, L.A.; Fallon, M. Incidence, prevalence, and predictors of chemotherapy-induced peripheral neuropathy: A systematic review and meta-analysis. Pain 2014, 155, 2661–2670. [Google Scholar] [CrossRef] [Green Version]
- Staff, N.P.; Grisold, A.; Grisold, W.; Windebank, A.J. Chemotherapy-induced peripheral neuropathy: A current review. Ann. Neurol. 2017, 81, 772–781. [Google Scholar] [CrossRef]
- Bao, T.; Seidman, A.D.; Piulson, L.; Vertosick, E.; Chen, X.; Vickers, A.J.; Blinder, V.S.; Zhi, W.I.; LI, Q.; Vahdat, L.T.; et al. A Phase IIA trial of acupuncture to reduce chemotherapy-induced peripheral neuropahy severity during neoadjuvant or adjuvant weekly paclitaxel chemotherapy in breast cancer patients. Eur. J. Cancer 2018, 101, 2–19. [Google Scholar] [CrossRef] [PubMed]
- Syrjala, K.L.; Jensen, M.P.; Mendoza, M.E.; Yi, J.C.; Fisher, H.M.; Keefe, G.J. Psychological and behavioral approaches to cancer pain management. J. Clin. Oncol. 2014, 32, 1703–1711. [Google Scholar] [CrossRef] [Green Version]
- Jensen, M.P.; Hanley, M.A.; Engel, J.M.; Romano, J.M.; Barber, J.; Cardenas, D.D.; Patterson, D.R. Hypnotic analgesia for chronic pain in persons with disabilities: A case series. Int. J. Clin. Exp. Hypnosis 2005, 53, 198–228. [Google Scholar] [CrossRef]
- Cramer, H.; Lauche, R.; Paul, A.; Dobos, J.; Langhof, S.T.; Kummel, S. Hypnosis in breast cancer care: A systematic review of randomized controlled trials. Integr. Cancer Ther. 2015, 14, 5–15. [Google Scholar] [CrossRef] [Green Version]
- Montgomery, G.H.; David, D.; Winkel, G.; Silverstei, J.H.; Bovbjerg, D.H. The effectiveness of adjunctive hypnosis with surgical patients: A meta-analysis. Anesth. Analg. 2002, 94, 1639–1645. [Google Scholar] [CrossRef]
- Montgomery, G.H.; Weltz, C.R.; Seltz, M.; Bovbjerg, D.H. Brief presurgery hypnosis reduces distress and pain in excisional breast biopsy patients. Int. J. Clin. Exp. Hypn. 2002, 50, 17–32. [Google Scholar] [CrossRef]
- Montgomery, G.H.; Bovbjerg, D.H.; Schnur, J.B.; David, D.; Goldfarb, A.; Weltz, C.R.; Schechter, C.; Graff-Zivin, J.; Tatrow, K.; Price, D.D.; et al. A randomized clinical trial of a brief hypnosis intervention to control side effects in breast surgery patients. J. Natl. Cancer Inst. 2007, 99, 1304–1312. [Google Scholar] [CrossRef]
- Malik, U.R.; Makower, D.F.; Wadler, S. Interferon mediated fatigue. Cancer 2001, 92, 1664–1668. [Google Scholar] [CrossRef]
- Bower, J.E. Cancer-related fatigue: Links with inflammation in cancer patients and survivors. Brain Behav. Immun. 2007, 21, 863–871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montgomery, G.H.; Kangas, M.; David, D.; Hallquist, M.N.; Green, S.; Bovbjerg, D.H.; Schnur, J.B. Fatigue during breast cancer radiotherapy: An initial randomized study of cognitive- behavioral therapy plus hypnosis. Health Psychol. 2009, 28, 317–322. [Google Scholar] [CrossRef]
- Goedendorp, M.M.; Gielissen, M.F.; Verhagen, C.A.; Beijener, G. Psychosocial interventions for reducing fatigue during cancer treatment in adults. Cochrane Database Syst. Rev. 2009, 2009, CD006953. [Google Scholar] [CrossRef] [Green Version]
- Molassiotis, A.; Ream, E.; Richardson, A.A.; Bardy, J.; Finnegan-John, J.; Mackereth, P.; Ryder, D.W.; Filshie, J. Acupuncture for cancer-related fatigue in patients with breast cancer: A pragmatic randomized controlled trial. J. Clin. Oncol. 2012, 30, 4470–4476. [Google Scholar] [CrossRef]
- Molassiotis, A.; Bardy, J.; Finnegan-John, J. A randomized, controlled trial of acupuncture self-needling as maintenance therapy for cancer-related fatigue after therapist-delivered acupuncture. Ann. Oncol. 2013, 24, 1645–1652. [Google Scholar] [CrossRef]
- Berliere, M.; Piette, N.; Gerday, A.; Roelants, F.; Docquier, M.-A.; Piette, P.; Duhoux, F.P.; Watremez, C. Mechanisms Involved in Hypnosis Analgesia Explaining Potential Benefits Observed among Breast Cancer Patients Undergoing Breast Surgery; Poster Session, Abstract P2, 14–11, AACR; American Association for Cancer Research: Philadelphia, PA, USA, 2019; Volume 79, Issue 4 SABCS. [Google Scholar]
- Balkwill, F.; Mantovani, A. Inflammation and cancer: Back to Virchow? Lancet 2001, 357, 539–545. [Google Scholar] [CrossRef]
- Balkwill, F.R.; Mantovani, A. Cancer-related inflammation: Common themes and therapeutic opportunities. Semin. Cancer Biol. 2012, 22, 33–40. [Google Scholar] [CrossRef]
- Diakos, C.I.; Charles, K.A.; McMillan, D.; Clarke, S.J. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014, 15, e493–e503. [Google Scholar] [CrossRef]
- Crusz, S.M.; Balkwill, F.R. Inflammation and cancer: Advances and new agents. Nat. Rev. Clin. Oncol. 2015, 12, 584–596. [Google Scholar] [CrossRef]
- Munn, L.L. Cancer and Inflammation. Wiley Interdiscip. Rev. Syst. Biol. Med. 2017, 9, e1370. [Google Scholar] [CrossRef] [Green Version]
- Laird, B.J.; McMillan, D.C.; Fayers, P.; Fearon, K.; Kaasa, S.; Fallon, M.T.; Klepstad, P. The systemic inflammatory response and its relationship to pain and other symptoms in advanced cancer. Oncologist 2013, 18, 1050. [Google Scholar] [CrossRef] [Green Version]
- Defechereux, T.; Degaugue, C.; Fumal, T.; Faymonville, M.E.; Joris, J.; Hamoir, E.; Meurisse, M. L’hypnosédation, un nouveau mode d’anesthésie pour la chirurgie endocrinienne cervicale. Etude prospective randomisée. Ann. Chir. 2000, 125, 539–546. [Google Scholar] [CrossRef]
- Hammond, D.C. Hypnosis in the treatment of anxiety-and stress-related disorders. Expert Rev. Neurother. 2010, 10, 263–273. [Google Scholar] [CrossRef]
- Grégoire, C.; Nicolas, H.; Bragard, I.; Delevallez, F.; Merckaert, I.; Razavi, D.; Waltregny, D.; Faymonville, M.E.; Vanhaudenhuyse, A. Efficacy of a hypnosis-based intervention to improve well-being during cancer: A comparison between prostate and breast cancer patients. BMC Cancer 2018, 18, 677. [Google Scholar] [CrossRef] [Green Version]
- Faller, H.; Schuler, M.; Richard, M.; Heckl, U.; Weis, J.; Kǜffner, R. Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: Systematic review and meta-anamysis. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2013, 31, 782–793. [Google Scholar] [CrossRef] [Green Version]
- Gorin, S.S.; Krebs, P.; Badr, H.; Janke, E.A.; Jim, H.S.L.; Spring, B.; Mohr, D.C.; Berendsen, M.A.; Jacobsen, P.B. Meta-analysis of psychosocial interventions to reduce pain in patients with cancer. J. Clin. Oncol. 2012, 30, 539–547. [Google Scholar] [CrossRef]
- Johannsen, M.; Farver, I.; Beck, N.; Zachariae, R. The efficacy of psychosocial intervention for pain in breast cancer patients and survivors: A systematic review and meta-analysis. Breast Cancer Res. Treat. 2013, 138, 675–690. [Google Scholar] [CrossRef] [Green Version]
- Guarino, A.; Polini, C.; Forte, G.; Favieri, F.; Boncompagni, I.; Casagrande, M. The effectiveness of psychological treatments in women with breast cancer: A systematic review and meta-analysis. J. Clin. Med. 2020, 9, 209. [Google Scholar] [CrossRef] [Green Version]
| Characteristics | GA Group (n = 32) | HYP Group (n = 31) |
|---|---|---|
| Mean age | 53 | - |
| Standard deviation | 11.39 | - |
| Menopausal status | ||
| Pre | 15 | 16 |
| Post | 17 | 15 |
| Medical history of | ||
| Polyneuropathy | 2 | 1 |
| Depression | 2 | 2 |
| Polyarthritis | 1 | 1 |
| Histological subtype | ||
| IDC | 30 | 29 |
| Mixed (IDC + ILC) | 2 | 2 |
| Hormone receptors | ||
| HR+ | 17 | 15 |
| HR− | 15 | 16 |
| HER2 SISH+ | 10 | 10 |
| Triple negative | 10 | 11 |
| Characteristics | GA Group (n = 32) | HYP Group (n = 31) |
|---|---|---|
| Chemotherapy regimen | ||
| 4 EC/4 Docetaxel | 5 | 5 |
| 4 EC dd/12 Paclitaxel | 20 | 20 |
| 4 EC/12 Paclitaxel | 7 | 6 |
| Surgery | ||
| Breast conserving | 28 | 29 |
| Mastectomy | 4 | 2 |
| Sentinel lymph node dissection | 18 | 19 |
| Axillary dissection | 14 | 12 |
| Radiotherapy | ||
| Yes | 30 | 30 |
| No | 2 | 1 |
| Traztuzumab alone | 8 | 7 |
| Trastuzumab + pertuzumab | 2 | 3 |
| Endocrine therapy | ||
| Tamoxifen | 2 | 2 |
| Aromatase inhibitors | 9 | 7 |
| Aromatase inhibitors + GnRH agonists | 3 | 3 |
| Tamoxifen + GnRH agonists | 3 | 3 |
| Characteristics | GA Group (n = 32) | HYP Group (n = 31) |
|---|---|---|
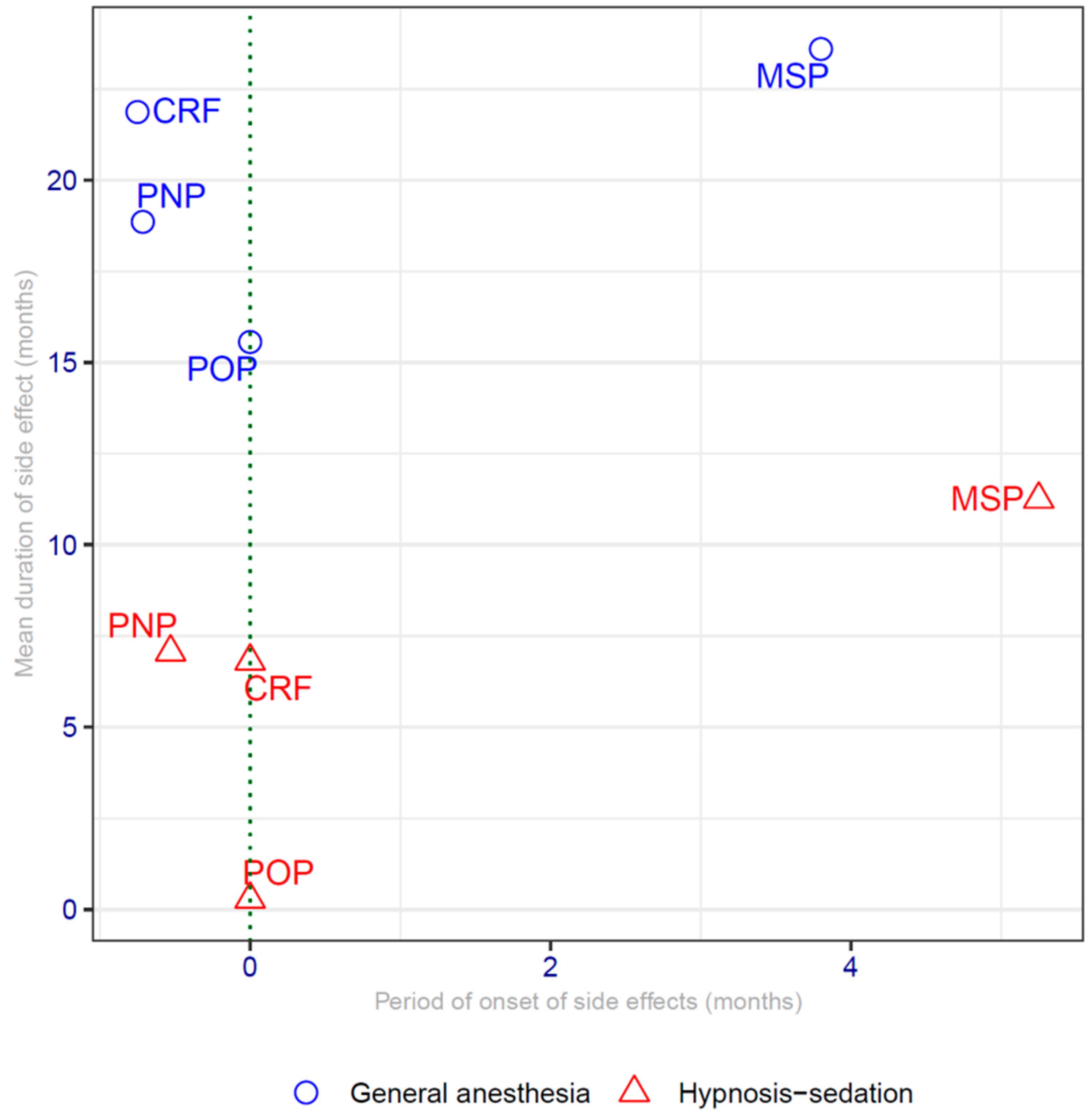
| PNP | 21 (65%) | 18 (58%) |
| Grade III | 3 (9%) | 2 (6%) |
| Difference duration | p = 5 × 10−11 | |
| 95% confidence interval | (9.4–14.2) | |
| Mean duration (months) | 18.9 | 7.1 |
| MSP | 15 (46%) | 8 (29%) |
| Difference duration | p = 1 × 10−8 | |
| 95% confidence interval | (10–14) | |
| Mean duration (months) | 24 | 11 |
| POP | All patients | All patients |
| Difference duration | p = 2 × 10−16 | |
| 95% confidence interval | (13–17) | |
| Mean duration (months) | 15.6 | 0.28 |
| Consumption of NSAIDs >8 days | 31/32 | 1/1 |
| CRF | All patients | All patients |
| Difference duration | p = 2 × 10−16 | |
| 95% confidence interval | (14–16) | |
| Mean duration (months) | 21.9 | 6.8 |
| Moment | Mean POP HYP | SD HYP | Mean POP GA | SD GA | p-Value |
|---|---|---|---|---|---|
| D0 | 0.580 | 0.501 | 2.375 | 0.491 | 1.58 × 10−12 |
| D1 | 1.096 | 0.3005 | 2.531 | 0.507 | 3.08 × 10−12 |
| D8 | 0.741 | 0.444 | 4 | 0.254 | 1.11 × 10−13 |
| M3 | NA | NA | 2.593 | 0.614 | NA |
| M6 | NA | NA | 2.187 | 0.859 | NA |
| M9 | NA | NA | 2.655 | 0.720 | NA |
| M12 | NA | NA | 1.862 | 0.915 | NA |
| M15 | NA | NA | 2.428 | 0.646 | NA |
| M18 | NA | NA | 2.428 | 0.646 | NA |
| M21 | NA | NA | 2.857 | 0.690 | NA |
| M24 | NA | NA | 2.857 | 0.690 | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berliere, M.; Piette, N.; Bernard, M.; Lacroix, C.; Gerday, A.; Samartzi, V.; Coyette, M.; Roelants, F.; Docquier, M.-A.; Touil, N.; et al. Hypnosis Sedation Reduces the Duration of Different Side Effects of Cancer Treatments in Breast Cancer Patients Receiving Neoadjuvant Chemotherapy. Cancers 2021, 13, 4147. https://doi.org/10.3390/cancers13164147
Berliere M, Piette N, Bernard M, Lacroix C, Gerday A, Samartzi V, Coyette M, Roelants F, Docquier M-A, Touil N, et al. Hypnosis Sedation Reduces the Duration of Different Side Effects of Cancer Treatments in Breast Cancer Patients Receiving Neoadjuvant Chemotherapy. Cancers. 2021; 13(16):4147. https://doi.org/10.3390/cancers13164147
Chicago/Turabian StyleBerliere, Martine, Nathan Piette, Marion Bernard, Camille Lacroix, Amandine Gerday, Vasiliki Samartzi, Maude Coyette, Fabienne Roelants, Marie-Agnes Docquier, Nassim Touil, and et al. 2021. "Hypnosis Sedation Reduces the Duration of Different Side Effects of Cancer Treatments in Breast Cancer Patients Receiving Neoadjuvant Chemotherapy" Cancers 13, no. 16: 4147. https://doi.org/10.3390/cancers13164147
APA StyleBerliere, M., Piette, N., Bernard, M., Lacroix, C., Gerday, A., Samartzi, V., Coyette, M., Roelants, F., Docquier, M.-A., Touil, N., Watremez, C., Piette, P., & Duhoux, F. P. (2021). Hypnosis Sedation Reduces the Duration of Different Side Effects of Cancer Treatments in Breast Cancer Patients Receiving Neoadjuvant Chemotherapy. Cancers, 13(16), 4147. https://doi.org/10.3390/cancers13164147






