Does the Lightning Process Training Programme Reduce Chronic Fatigue in Adolescent and Young Adult Cancer Survivors? A Mixed-Methods Pilot Study
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Demographics and Clinical Information
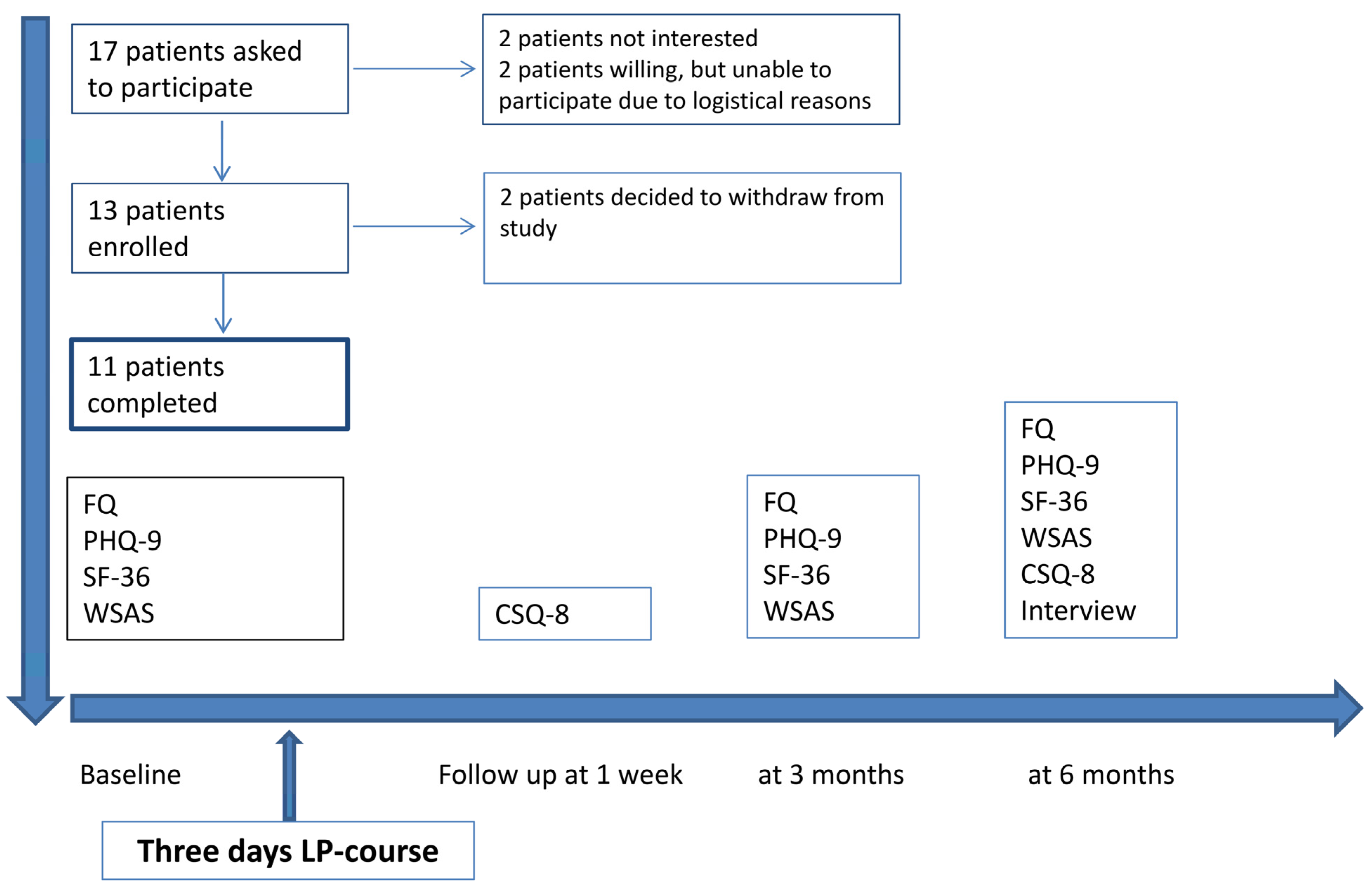
2.2. Study Procedures
2.2.1. Quantitative Study
2.2.2. Statistical Analyses
2.2.3. Qualitative Study
2.2.4. Analysis
2.3. Description of the Intervention
3. Results
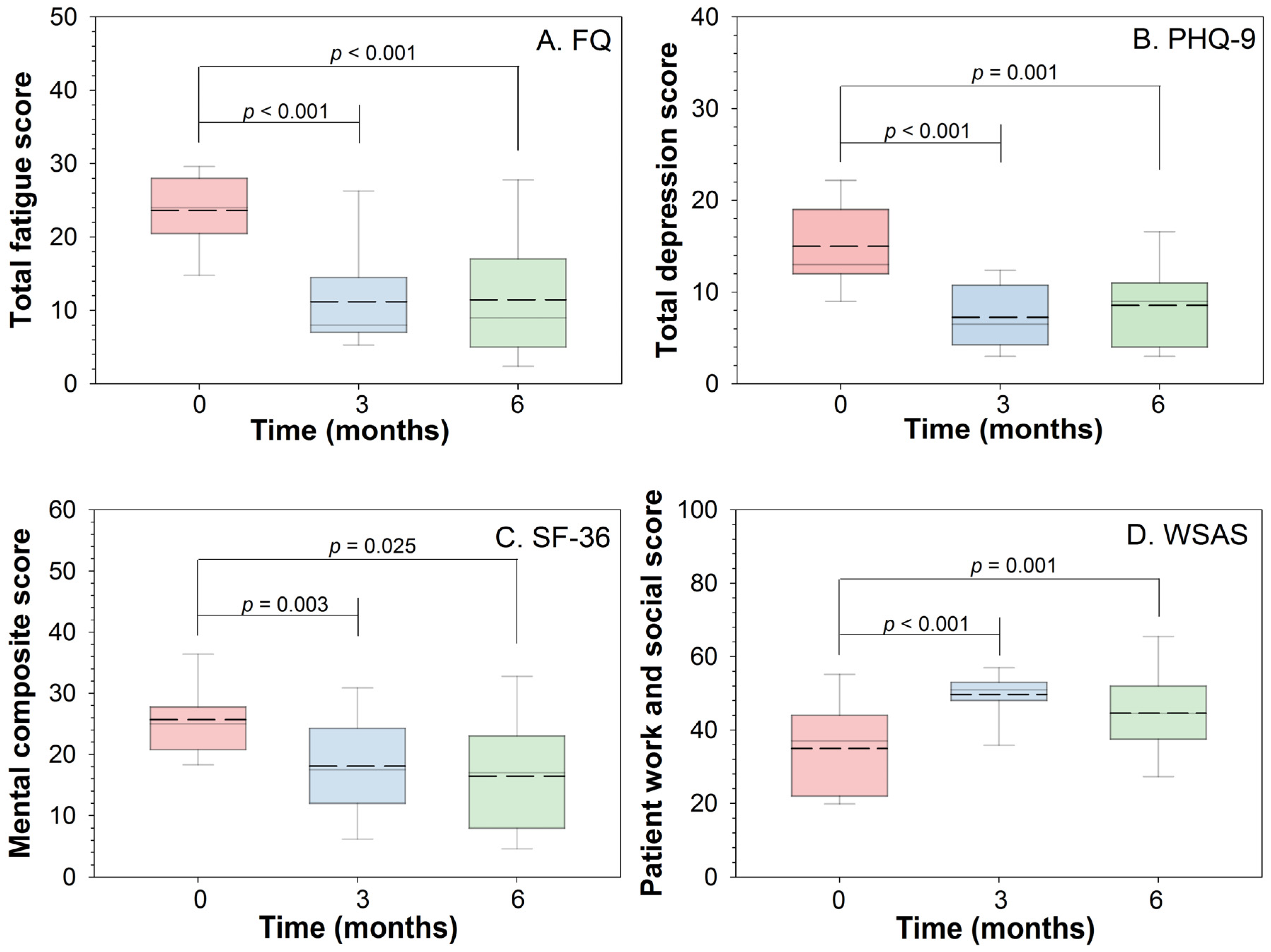
3.1. Quantitative Study
3.2. Qualitative Study
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bower, J.E. Cancer-related fatigue—Mechanisms, risk factors, and treatments. Nat. Rev. Clin. Oncol. 2014, 11, 597–609. [Google Scholar] [CrossRef]
- Berger, A.M.; Mooney, K.; Alvarez-Perez, A.; Breitbart, W.S.; Carpenter, K.M.; Cella, D.; Cleeland, C.; Dotan, E.; Eisenberger, M.A.; Escalante, C.P.; et al. Cancer-related fatigue, version 2. 2015. J. Natl. Compr. Cancer Netw. 2015, 13, 1012–1039. [Google Scholar] [CrossRef]
- Smith, M.E.; Haney, E.; McDonagh, M.; Pappas, M.; Daeges, M.; Wasson, N.; Fu, R.; Nelson, H.D. Treatment of myalgic encephalomyelitis/chronic fatigue syndrome: A systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann. Intern Med. 2015, 162, 841–850. [Google Scholar] [CrossRef] [Green Version]
- White, P.D.; Goldsmith, K.A.; Johnson, A.L.; Potts, L.; Walwyn, R.; DeCesare, J.C.; Baber, H.L.; Burgess, M.; Clark, L.V.; Cox, D.L.; et al. Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome (PACE): A randomised trial. Lancet 2011, 377, 823–836. [Google Scholar] [CrossRef] [Green Version]
- Arring, N.M.; Barton, D.L.; Brooks, T.; Zick, S.M. Integrative therapies for cancer-related fatigue. Cancer J. 2019, 25, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Corbett, T.K.; Groarke, A.; Devane, D.; Carr, E.; Walsh, J.E.; McGuire, B.E. The effectiveness of psychological interventions for fatigue in cancer survivors: Systematic review of randomised controlled trials. Syst. Rev. 2019, 8, 324. [Google Scholar] [CrossRef]
- Coccia, P.F.; Altman, J.; Bhatia, S.; Borinstein, S.C.; Flynn, J.; George, S.; Goldsby, R.; Hayashi, R.; Huang, M.S.; Johnson, R.H.; et al. Adolescent and young adult oncology. Clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 2012, 10, 1112–1150. [Google Scholar] [CrossRef]
- Barnett, M.; McDonnell, G.; DeRosa, A.; Schuler, T.; Philip, E.; Peterson, L.; Touza, K.; Jhanwar, S.; Atkinson, T.M.; Ford, J.S. Psychosocial outcomes and interventions among cancer survivors diagnosed during adolescence and young adulthood (AYA): A systematic review. J. Cancer Surviv. 2016, 10, 814–831. [Google Scholar] [CrossRef] [Green Version]
- Richter, D.; Koehler, M.; Friedrich, M.; Hilgendorf, I.; Mehnert, A.; Weissflog, G. Psychosocial interventions for adolescents and young adult cancer patients: A systematic review and meta-analysis. Crit. Rev. Oncol. Hematol. 2015, 95, 370–386. [Google Scholar] [CrossRef] [PubMed]
- Robinson, P.D.; Oberoi, S.; Tomlinson, D.; Duong, N.; Davis, H.; Cataudella, D.; Culos-Reed, N.; Gibson, F.; Götte, M.; Hinds, P.; et al. Management of fatigue in children and adolescents with cancer and in paediatric recipients of haemopoietic stem-cell transplants: A clinical practice guideline. Lancet Child. Adolesc. Health 2018, 2, 371–378. [Google Scholar] [CrossRef]
- Parker, P.; Aston, J.; Finch, F. Understanding the Lightning Process Approach to CFS/ME; a Review of the Disease Process and the Approach. J. Exp. Psychother./Rev. Psihoter. Exp. 2018, 21, 21–28. [Google Scholar]
- Crawley, E.M.; Gaunt, D.M.; Garfield, K.; Hollingworth, W.; Sterne, J.A.C.; Beasant, L.; Collin, S.M.; Mills, N.; Montgomery, A.A. Clinical and cost-effectiveness of the Lightning Process in addition to specialist medical care for paediatric chronic fatigue syndrome: Randomised controlled trial. Arch. Dis. Child. 2018, 103, 155–164. [Google Scholar] [CrossRef]
- Reme, S.E.; Archer, N.; Chalder, T. Experiences of young people who have undergone the Lightning Process to treat chronic fatigue syndrome/myalgic encephalomyelitis—A qualitative study. Br. J. Health Psychol. 2013, 18, 508–525. [Google Scholar] [CrossRef]
- Chalder, T.; Berelowitz, G.; Pawlikowska, T.; Watts, L.; Wessely, S.; Wright, D.; Wallace, E.P. Development of a fatigue scale. J. Psychosom. Res. 1993, 37, 147–153. [Google Scholar] [CrossRef] [Green Version]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Löwe, B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: A systematic review. Gen. Hosp. Psychiatry 2010, 32, 345–359. [Google Scholar] [CrossRef] [PubMed]
- Mundt, J.C.; Marks, I.M.; Shear, M.K.; Greist, J.H. The Work and Social Adjustment Scale: A simple measure of impairment in functioning. Br. J. Psychiatry 2002, 180, 461–464. [Google Scholar] [CrossRef]
- Larsen, D.L.; Attkisson, C.C.; Hargreaves, W.A.; Nguyen, T.D. Assessment of client/patient satisfaction: Development of a general scale. Eval. Program Plan. 1979, 2, 197–207. [Google Scholar] [CrossRef]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Gandek, B.; Ware, J.E., Jr.; Aaronson, N.K.; Alonso, J.; Apolone, G.; Bjorner, J.; Brazier, J.; Bullinger, M.; Fukuhara, S.; Kaasa, S.; et al. Tests of data quality, scaling assumptions, and reliability of the SF-36 in eleven countries: Results from the IQOLA Project. International Quality of Life Assessment. J. Clin. Epidemiol. 1998, 51, 1149–1158. [Google Scholar] [CrossRef]
- Sloan, J. Detecting worms, ducks, and elephants: A simple approach for defining clinically relevant effects in quality-of-life measures. J. Cancer Integr. Med. 2003, 1, 41–47. [Google Scholar]
- Kvale, S.; Brinkmann, S. Interviews: Learning the Craft of Qualitative Research Interviewing; Sage: Los Angeles, CA, USA, 2009. [Google Scholar]
- Braun, V.C.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Braun, V.C.; Clarke, V. Reflecting on reflexive thematic analysis. Qual. Res. Sport Exerc. Health 2019, 11, 589–597. [Google Scholar] [CrossRef]
- Gubrium, J.F.; Holstein, J.A.; Marvasti, A.B.; McKinney, K.D. The SAGE Handbook of Interview Research: The Complexity of the Craft; Sage: Thousand Oaks, CA, USA, 2012. [Google Scholar]
- Wyller, V.B.; Eriksen, H.R.; Malterud, K. Can sustained arousal explain the chronic fatigue syndrome? Behav. Brain Funct. 2009, 5, 10. [Google Scholar] [CrossRef] [Green Version]
- Ursin, H.; Eriksen, H.R. The cognitive activation theory of stress. Psychoneuroendocrinology 2004, 29, 567–592. [Google Scholar] [CrossRef]
- Kube, T.; Rozenkrantz, L.; Rief, W.; Barsky, A. Understanding persistent physical symptoms: Conceptual integration of psychological expectation models and predictive processing accounts. Clin. Psychol. Rev. 2020, 76, 101829. [Google Scholar] [CrossRef] [PubMed]
- Barrett, L.F.; Simmons, W.K. Interoceptive predictions in the brain. Nat. Rev. Neurosci. 2015, 16, 419–429. [Google Scholar] [CrossRef] [Green Version]
- Van den Bergh, O.; Witthoft, M.; Petersen, S.; Brown, R.J. Symptoms and the body: Taking the inferential leap. Neurosci. Biobehav. Rev. 2017, 74 Pt A, 185–203. [Google Scholar] [CrossRef] [Green Version]
- Colloca, L.; Barsky, A.J. Placebo and nocebo effects. N. Engl. J. Med. 2020, 382, 554–561. [Google Scholar] [CrossRef]
| Demographics and Diagnosis | Numbers |
|---|---|
| Total number of patients | 13 |
| Median age (years and range) | 30 (21–36) |
| Sex | |
| Female | 10 |
| Male | 3 |
| Relationship status | |
| Married | 1 |
| Co-habitant | 7 |
| Single | 5 |
| Children | 4 |
| Time since primary diagnosis (median in years and range) | 7 (2–12) |
| Time since receiving last systemic therapy (median in years and range) | 6 (1–11) |
| Diagnosis | |
| Bone sarcomas | 4 |
| Osteosarcoma | 2 |
| Ewing sarcoma | 1 |
| Chondrosarcoma | 1 |
| Soft tissue sarcoma | 2 |
| Rhabdomyosarcoma | 1 |
| Synovial sarcoma | 1 |
| Hodgkin lymphoma | 7 |
| Oncological Treatments | Number of Patients |
|---|---|
| Sarcomas | |
| Surgery only | 1 |
| Surgery and adjuvant treatment | 5 |
| Radiotherapy | 3 |
| Chemotherapy | 5 |
| Ewing sarcoma combo | 2 |
| Osteosarcoma combo | 2 |
| Doxorubicin/ifosfamide | 1 |
| Number of chemotherapy combinations | - |
| One line | 3 |
| Two lines | 2 |
| Surgery for metastatic recurrence in lungs | 2 |
| Hodgkin lymphoma | |
| Radiotherapy | 4 |
| Chemotherapy | 7 |
| Number of conventional chemotherapy combinations | - |
| One line | 3 |
| Two lines | 3 |
| Three lines or more | 1 |
| High-dose chemotherapy with stem cell support | 4 |
| Autologous | 2 |
| Allogeneic | 2 |
| Immunotherapy | 3 |
| Themes | Selected Quotations |
|---|---|
| A feeling of more energy and “joie de vivre” | • Before the course I could sleep for four hours when I came home from work. Now I actually cannot remember the last time I slept after I got home. P1 • I felt much more exhausted before the course. I have got a lot more energy now […]. I feel things have gone much better since the course. […]. My body works better, I am less agitated, I have less pain and my energy level is a bit higher. And I can sleep better. P3 • After the course, I felt so positive. I had been given a new boost, I was happy in my daily life and I felt much more hopeful. P9 • The main thing for me, I think, was that I rediscovered my energy, that is where I have felt the most change. P6 |
| Changing dysfunctional thought patterns using a well-learned process | • What I benefited most from was noticing how I responded to stress […] after the course, I completely changed the way I thought about my physical condition. P2 • We have been given different exercises to think about, when we are stuck in situations, for example, then I have done those exercises and trained my brain to think in a different way […]. I am more aware of the things I do and think—that everything is linked to feeling lethargic and tired. P5 • It is all about appreciating and thinking about all the good things in life instead of constantly focusing on what is not good, or what I did not manage to do, then you get into a vicious circle again. So, it has been helpful to become aware of that. P9 |
| Has integrated the technique into daily life and uses the process as needed | • When I feel I am in an awful state, I do the whole process, like some days I do it many times and sometimes I do it a couple of times a week, you see. It depends on how my life is at the time. P11 • I have got a tool I can use for the rest of my life […]. I go through the process instead of resting and I start the rest of the day from there. P4 • I mostly use it in my head from day to day […], but if I have any negative feelings or thoughts […] I notice there is a greater effect if I use it physically. P12 |
| Daring to challenge oneself and move outside one’s comfort zone | • I dare to do things a bit more without thinking so much about what sort of consequences they will have for me physically. It has helped me to be a bit more relaxed and then that maybe gives me a bit more energy. P2 • The most important progress has been to see that I can actually manage to do things. P9 • I find it a bit easier to trust that things will get better and that my body is healthy and things will be fine. [..]. After working two days a week, I can still get a visit on the Saturday and that does not make me feel worse. P11 • I now realize I cope better than I thought with stressful situations or situations that I find difficult mentally and I understand better what makes me depressed […]. I am now more robust, I would say. P2 |
| A better life with family and friends and increased energy at work | • My family life is much better now I have got more energy and more stamina […]. Before the course I really was not sociable, and I was not up to much […] now things are better in every possible way. My partner would agree completely. P3 • I felt that I could work a bit more efficiently and I had a bit more energy to do things after work that were very important to me. This June I started a full-time job in another company (compared to part-time, 30%, before the course), which would have been impossible without the lightning process […]. Now I am financially independent of my parents, which has been my dream for about ten years. P4 • Before the course I did nothing, and I was hardly ever in social situations […]. Now I have the energy to be sociable and not be completely exhausted afterwards. (laughs) […]. I am really pleased about that. That was what I was hoping for, to start being with my family and friends again. P7 • The way I see it now, I feel that I can cope with daily life, I can cope with life as a mother, I can function properly, and I can get things done. I take the initiative to do things, which was a good bit more difficult before. P9 |
| Importance of follow-up dialogues to maintain the process/improvements | • The most important thing has been the follow-up. The phone calls. One-on-one dialogues, definitely […]. I think it has been useful to have those talks regularly so that you keep going with the process and what you have learned. P1 • I really liked the follow-up afterwards, there were regular phone calls where we talked about how things were going and some homework for the next time. P7 • I think the most important thing was the period after the course where you were in touch with the instructor […] it was great to have someone you could hold on to. P4 |
| Feeling that the course/intervention was good but I do not think the process suited me | • The process is not quite me […] I cannot keep up the daily exercises. P3 • In general, everything was very good, but the process itself was very strange to me […] mainly perhaps a bit outside my comfort zone. P6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fauske, L.; Bruland, Ø.S.; Dahl, A.A.; Myklebostad, A.; Reme, S.E. Does the Lightning Process Training Programme Reduce Chronic Fatigue in Adolescent and Young Adult Cancer Survivors? A Mixed-Methods Pilot Study. Cancers 2021, 13, 4076. https://doi.org/10.3390/cancers13164076
Fauske L, Bruland ØS, Dahl AA, Myklebostad A, Reme SE. Does the Lightning Process Training Programme Reduce Chronic Fatigue in Adolescent and Young Adult Cancer Survivors? A Mixed-Methods Pilot Study. Cancers. 2021; 13(16):4076. https://doi.org/10.3390/cancers13164076
Chicago/Turabian StyleFauske, Lena, Øyvind S. Bruland, Alv A. Dahl, Aase Myklebostad, and Silje E. Reme. 2021. "Does the Lightning Process Training Programme Reduce Chronic Fatigue in Adolescent and Young Adult Cancer Survivors? A Mixed-Methods Pilot Study" Cancers 13, no. 16: 4076. https://doi.org/10.3390/cancers13164076
APA StyleFauske, L., Bruland, Ø. S., Dahl, A. A., Myklebostad, A., & Reme, S. E. (2021). Does the Lightning Process Training Programme Reduce Chronic Fatigue in Adolescent and Young Adult Cancer Survivors? A Mixed-Methods Pilot Study. Cancers, 13(16), 4076. https://doi.org/10.3390/cancers13164076






