Antagonists of Growth Hormone-Releasing Hormone Inhibit the Growth of Pituitary Adenoma Cells by Hampering Oncogenic Pathways and Promoting Apoptotic Signaling
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Reagents
2.2. Cell Culture
2.3. Human Samples and Isolation of PA Cell Cultures
2.4. Cell Viability
2.5. Annexin V Analysis
2.6. Colony Formation
2.7. Western Blot Analysis
2.8. Combination Studies
2.9. cAMP Assay
2.10. GH, PRL, and ACTH Secretion
2.11. Real-Time PCR
2.12. Statistical Analysis
3. Results
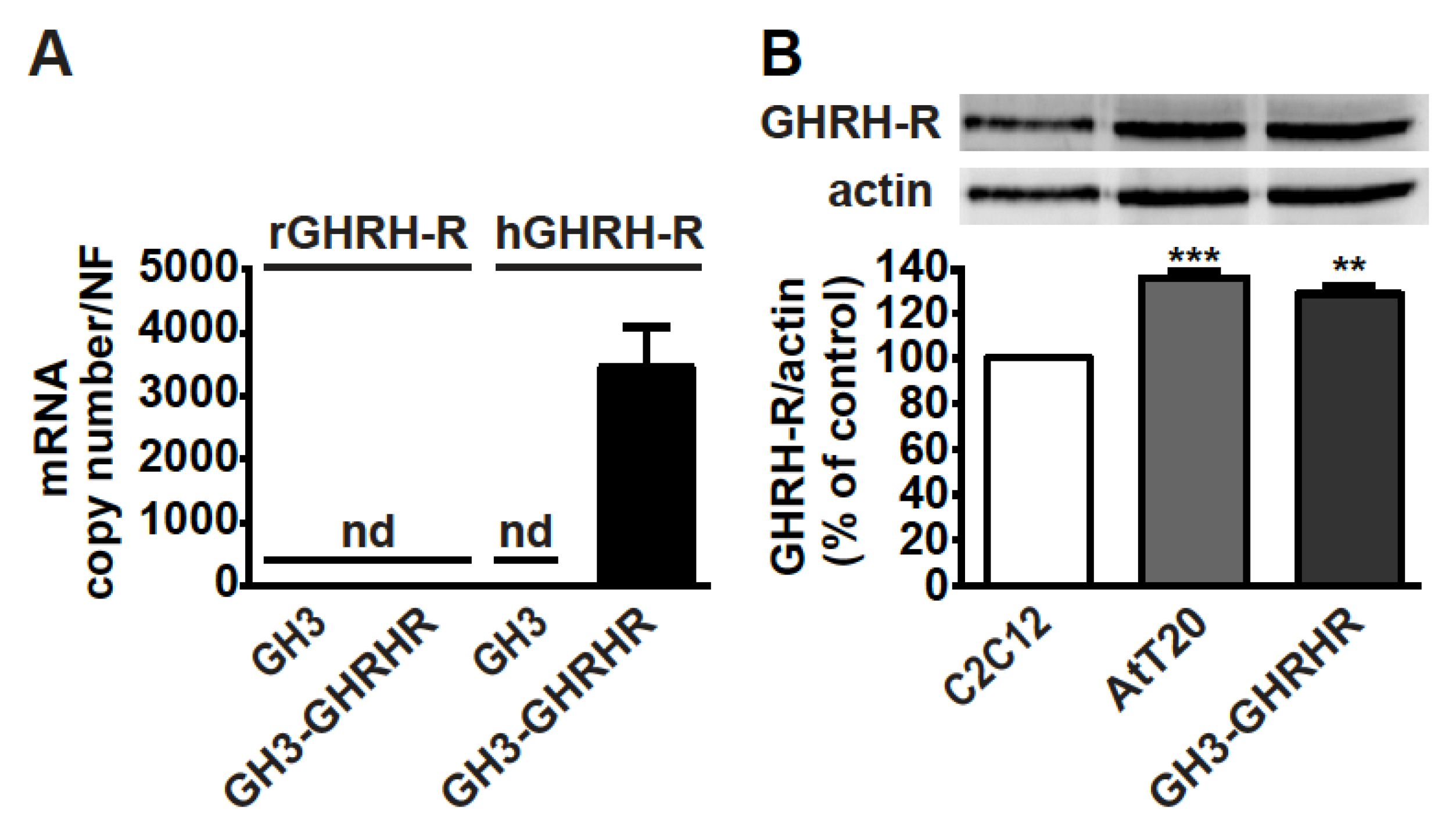
3.1. GHRH-R Is Expressed in GH3-GHRHR and AtT20 Cells
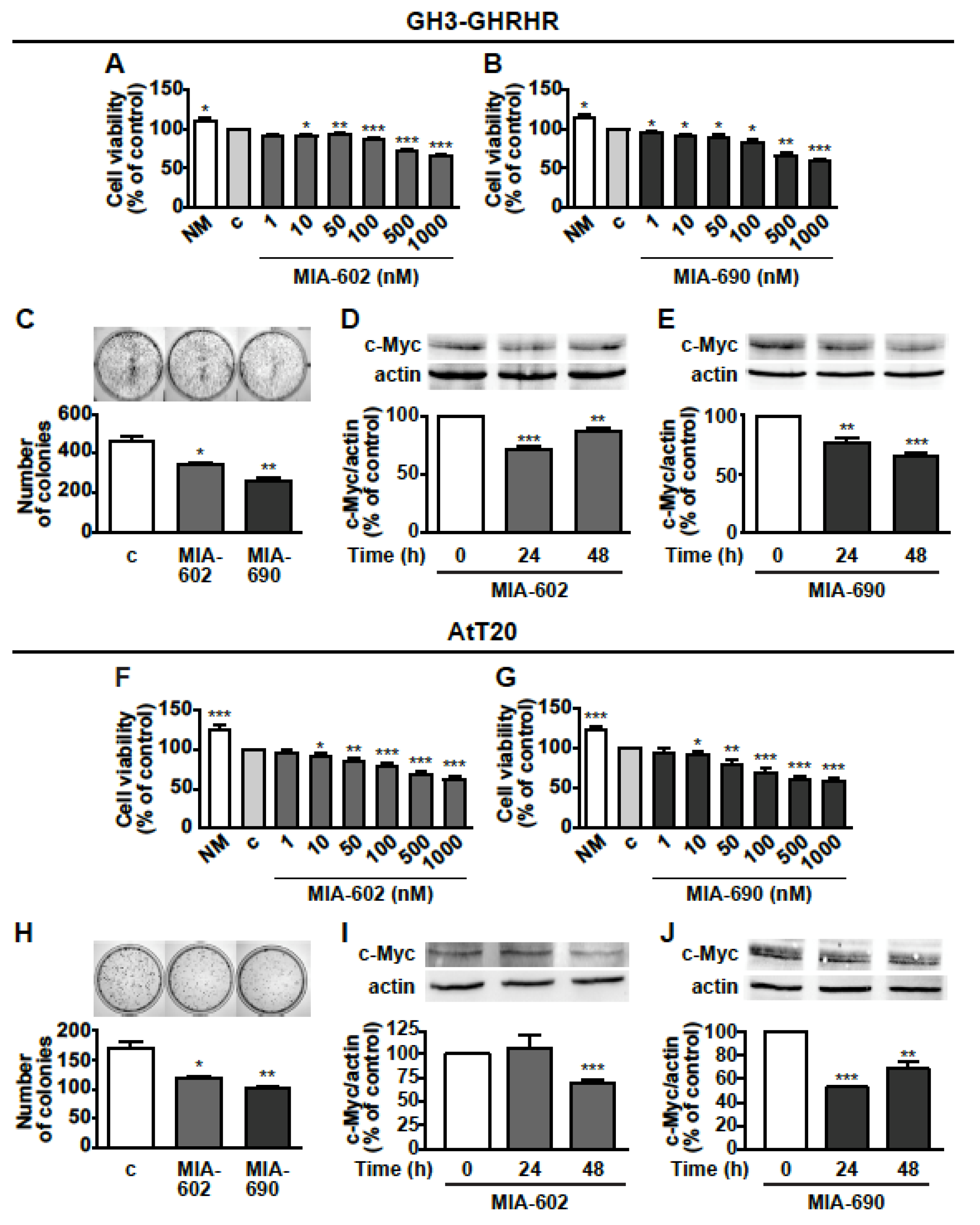
3.2. MIA-602 and MIA-690 Inhibit Cell Viability and Growth of GH3-GHRHR and AtT20 Cells
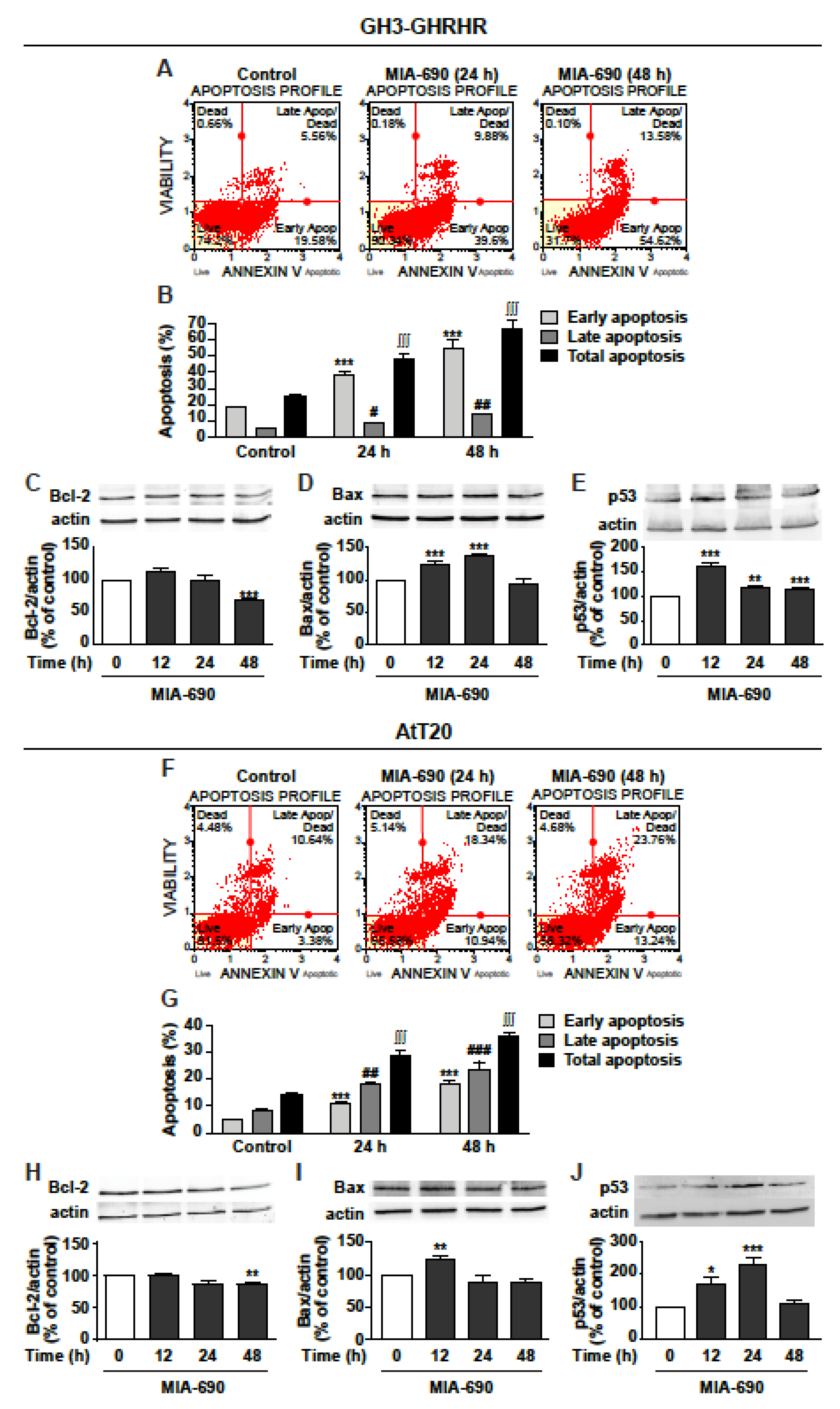
3.3. GHRH Antagonists Promote Apoptosis in GH3-GHRHR and AtT20 Cells
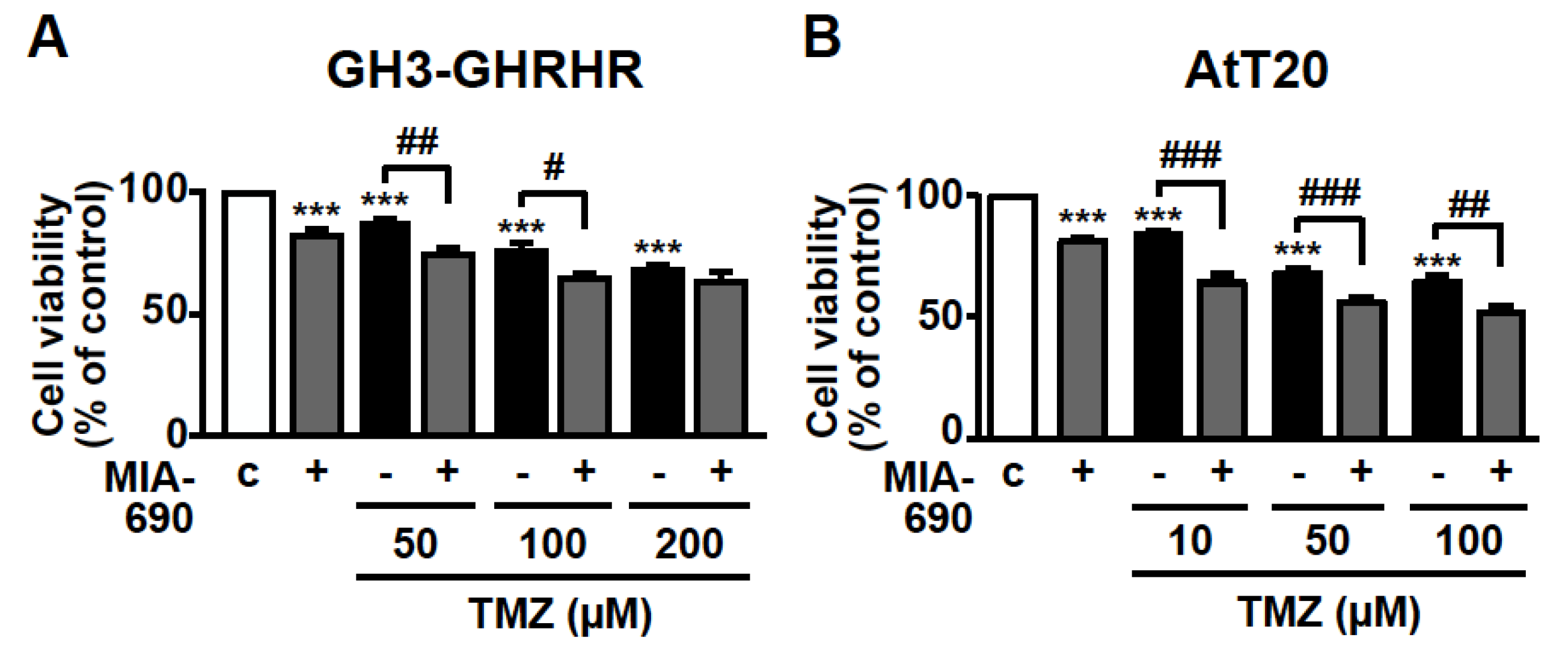
3.4. GHRH Antagonists and TMZ Synergistically Inhibit Cell Viability in PA Cell Lines
3.5. GHRH Antagonists Inhibit the Expression of GHRH-R in PA Cell Lines
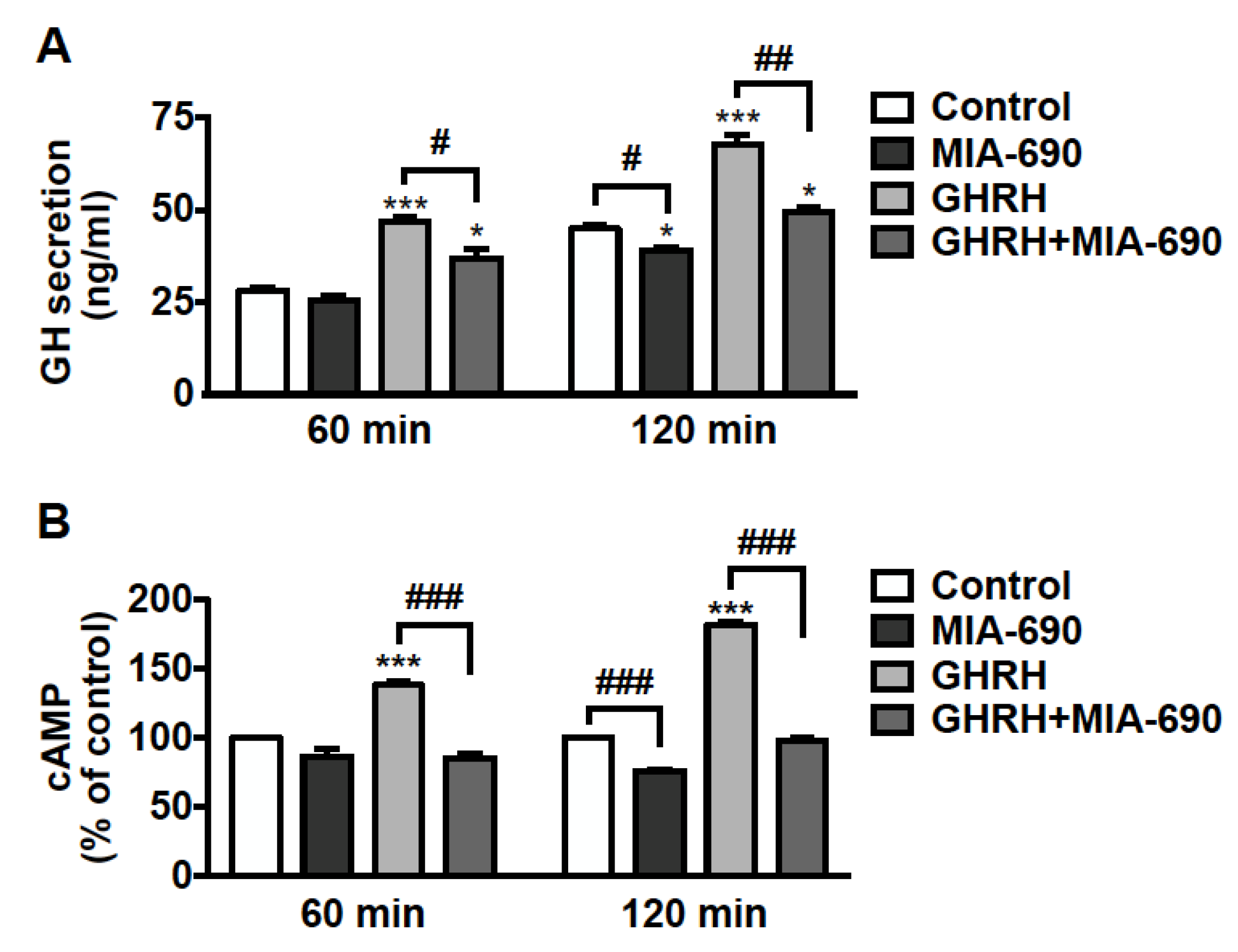
3.6. MIA-690 Inhibits GH Secretion and Intracellular cAMP Levels, but Not PRL and ACTH Release in PA Cell Lines
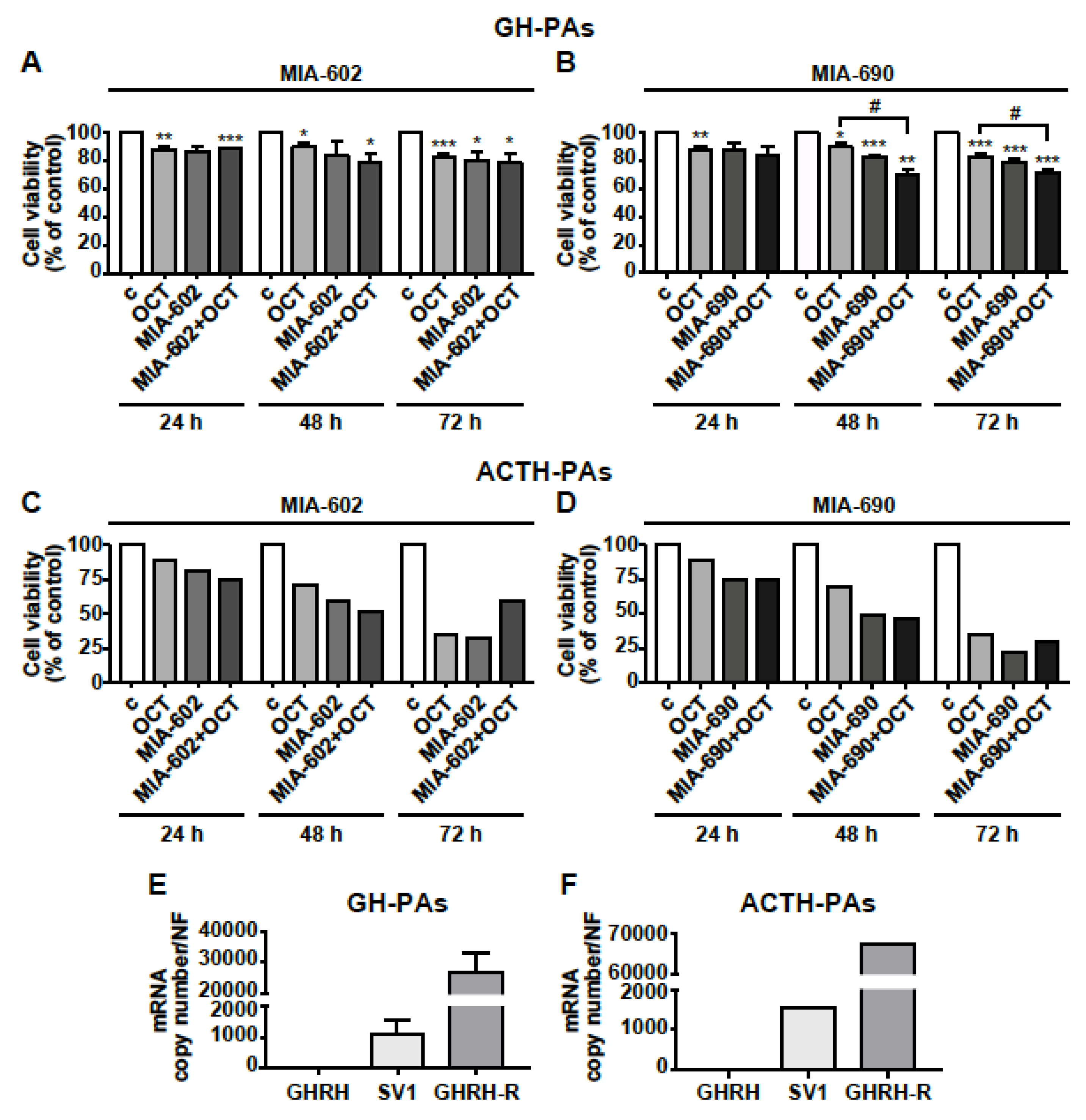
3.7. MIA-602 and MIA-690 Inhibit Cell Viability in Primary Human PA Cell Cultures
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Molitch, M.E. Diagnosis and Treatment of Pituitary Adenomas: A Review. JAMA 2017, 317, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, R.V.; Osamura, R.Y.; Klöppel, G.; Rosai, J. (Eds.) WHO Classification of Tumours of Endocrine Organs, 4th ed.; IARC Press: Lyon, France, 2017. [Google Scholar]
- Ho, K.; Fleseriu, M.; Kaiser, U.; Salvatori, R.; Brue, T.; Lopes, M.B.; Kunz, P.; Molitch, M.; Camper, S.A.; Gadelha, M.; et al. Pituitary Neoplasm Nomenclature Workshop: Does Adenoma Stand the Test of Time? J. Endocr. Soc. 2021, 5. [Google Scholar] [CrossRef] [PubMed]
- Melmed, S. Pituitary-Tumor Endocrinopathies. N. Engl. J. Med. 2020, 382, 937–950. [Google Scholar] [CrossRef]
- Aflorei, E.D.; Korbonits, M. Epidemiology and etiopathogenesis of pituitary adenomas. J. Neurooncol. 2014, 117, 379–394. [Google Scholar] [CrossRef] [PubMed]
- Gheorghiu, M.L.; Negreanu, F.; Fleseriu, M. Updates in the Medical Treatment of Pituitary Adenomas. Horm. Metab. Res. 2020, 52, 8–24. [Google Scholar] [CrossRef]
- Burman, P.; Lamb, L.; McCormack, A. Temozolomide therapy for aggressive pituitary tumours—Current understanding and future perspectives. Rev. Endocr. Metab. Disord. 2020, 21, 263–276. [Google Scholar] [CrossRef]
- Kiaris, H.; Chatzistamou, I.; Papavassiliou, A.G.; Schally, A.V. Growth hormone-releasing hormone: Not only a neurohormone. Trends Endocrinol. Metab. TEM 2011, 22, 311–317. [Google Scholar] [CrossRef]
- Granata, R. Peripheral activities of growth hormone-releasing hormone. J. Endocrinol. Investig. 2016, 39, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Schally, A.V.; Zhang, X.; Cai, R.; Hare, J.M.; Granata, R.; Bartoli, M. Actions and Potential Therapeutic Applications of Growth Hormone-Releasing Hormone Agonists. Endocrinology 2019, 160, 1600–1612. [Google Scholar] [CrossRef]
- Gesmundo, I.; Miragoli, M.; Carullo, P.; Trovato, L.; Larcher, V.; Di Pasquale, E.; Brancaccio, M.; Mazzola, M.; Villanova, T.; Sorge, M.; et al. Growth hormone-releasing hormone attenuates cardiac hypertrophy and improves heart function in pressure overload-induced heart failure. Proc. Natl. Acad. Sci. USA 2017, 114, 12033–12038. [Google Scholar] [CrossRef]
- Recinella, L.; Chiavaroli, A.; Di Valerio, V.; Veschi, S.; Orlando, G.; Ferrante, C.; Gesmundo, I.; Granata, R.; Cai, R.; Sha, W.; et al. Protective effects of growth hormone-releasing hormone analogs in DSS-induced colitis in mice. Sci. Rep. 2021, 11, 2530. [Google Scholar] [CrossRef] [PubMed]
- Rieger, A.C.; Bagno, L.L.; Salerno, A.; Florea, V.; Rodriguez, J.; Rosado, M.; Turner, D.; Dulce, R.A.; Takeuchi, L.M.; Kanashiro-Takeuchi, R.M.; et al. Growth hormone-releasing hormone agonists ameliorate chronic kidney disease-induced heart failure with preserved ejection fraction. Proc. Natl. Acad. Sci. USA 2021, 118, e2019835118. [Google Scholar] [CrossRef] [PubMed]
- Recinella, L.; Chiavaroli, A.; Orlando, G.; Ferrante, C.; Marconi, G.D.; Gesmundo, I.; Granata, R.; Cai, R.; Sha, W.; Schally, A.V.; et al. Antinflammatory, antioxidant, and behavioral effects induced by administration of growth hormone-releasing hormone analogs in mice. Sci. Rep. 2020, 10, 732. [Google Scholar] [CrossRef] [PubMed]
- Barabutis, N.; Schally, A.V. Growth hormone-releasing hormone: Extrapituitary effects in physiology and pathology. Cell Cycle 2010, 9, 4110–4116. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Villanova, T.; Gesmundo, I.; Audrito, V.; Vitale, N.; Silvagno, F.; Musuraca, C.; Righi, L.; Libener, R.; Riganti, C.; Bironzo, P.; et al. Antagonists of growth hormone-releasing hormone (GHRH) inhibit the growth of human malignant pleural mesothelioma. Proc. Natl. Acad. Sci. USA 2019, 116, 2226–2231. [Google Scholar] [CrossRef]
- Zarandi, M.; Cai, R.; Kovacs, M.; Popovics, P.; Szalontay, L.; Cui, T.; Sha, W.; Jaszberenyi, M.; Varga, J.; Zhang, X.; et al. Synthesis and structure-activity studies on novel analogs of human growth hormone releasing hormone (GHRH) with enhanced inhibitory activities on tumor growth. Peptides 2017, 89, 60–70. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, X.; Vidaurre, I.; Cai, R.; Sha, W.; Schally, A.V. Inhibition of experimental small-cell and non-small-cell lung cancers by novel antagonists of growth hormone-releasing hormone. Int. J. Cancer 2018, 142, 2394–2404. [Google Scholar] [CrossRef]
- Munoz-Moreno, L.; Schally, A.V.; Prieto, J.C.; Carmena, M.J.; Bajo, A.M. Growth hormone-releasing hormone receptor antagonists modify molecular machinery in the progression of prostate cancer. Prostate 2018, 78, 915–926. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, M.; Kineman, R.D.; Schally, A.V.; Zarandi, M.; Groot, K.; Frohman, L.A. Effects of antagonists of growth hormone-releasing hormone (GHRH) on GH and insulin-like growth factor I levels in transgenic mice overexpressing the human GHRH gene, an animal model of acromegaly. Endocrinology 1997, 138, 4536–4542. [Google Scholar] [CrossRef]
- Schally, A.V.; Varga, J.L.; Engel, J.B. Antagonists of growth-hormone-releasing hormone: An emerging new therapy for cancer. Nat. Clin. Pract. Endocrinol. Metab. 2008, 4, 33–43. [Google Scholar] [CrossRef]
- Szalontay, L.; Benveniste, R.J.; Schally, A.V.; Vidaurre, I.; Nadji, M.; Zarandi, M.; Block, N.L.; Kovacs, M. Inhibitory effects of GHRH antagonists on human GH-secreting adenoma tissue. Neuroendocrinology 2012, 96, 81–88. [Google Scholar] [CrossRef]
- Kovacs, M.; Schally, A.V.; Lee, E.J.; Busto, R.; Armatis, P.; Groot, K.; Varga, J.L. Inhibitory effects of antagonistic analogs of GHRH on GH3 pituitary cells overexpressing the human GHRH receptor. J. Endocrinol. 2002, 175, 425–434. [Google Scholar] [CrossRef][Green Version]
- Kovacs, M.; Schally, A.V.; Zarandi, M.; Groot, K. Inhibition of GH release of rats by new potent antagonists of growth hormone-releasing hormone (GH-RH). Peptides 1997, 18, 431–438. [Google Scholar] [CrossRef]
- Kovacs, M.; Zarandi, M.; Halmos, G.; Groot, K.; Schally, A.V. Effects of acute and chronic administration of a new potent antagonist of growth hormone-releasing hormone in rats: Mechanisms of action. Endocrinology 1996, 137, 5364–5369. [Google Scholar] [CrossRef] [PubMed]
- Varga, J.L.; Schally, A.V.; Csernus, V.J.; Zarandi, M.; Halmos, G.; Groot, K.; Rekasi, Z. Synthesis and biological evaluation of antagonists of growth hormone-releasing hormone with high and protracted in vivo activities. Proc. Natl. Acad. Sci. USA 1999, 96, 692–697. [Google Scholar] [CrossRef] [PubMed]
- Zarandi, M.; Kovacs, M.; Horvath, J.E.; Toth, K.; Halmos, G.; Groot, K.; Nagy, A.; Kele, Z.; Schally, A.V. Synthesis and in vitro evaluation of new potent antagonists of growth hormone-releasing hormone (GH-RH). Peptides 1997, 18, 423–430. [Google Scholar] [CrossRef]
- Gan, J.; Ke, X.; Jiang, J.; Dong, H.; Yao, Z.; Lin, Y.; Lin, W.; Wu, X.; Yan, S.; Zhuang, Y.; et al. Growth hormone-releasing hormone receptor antagonists inhibit human gastric cancer through downregulation of PAK1-STAT3/NF-kappaB signaling. Proc. Natl. Acad. Sci. USA 2016, 113, 14745–14750. [Google Scholar] [CrossRef]
- Perez, R.; Schally, A.V.; Vidaurre, I.; Rincon, R.; Block, N.L.; Rick, F.G. Antagonists of growth hormone-releasing hormone suppress in vivo tumor growth and gene expression in triple negative breast cancers. Oncotarget 2012, 3, 988–997. [Google Scholar] [CrossRef]
- Jimenez, J.J.; DelCanto, G.M.; Popovics, P.; Perez, A.; Vila Granda, A.; Vidaurre, I.; Cai, R.Z.; Rick, F.G.; Swords, R.T.; Schally, A.V. A new approach to the treatment of acute myeloid leukaemia targeting the receptor for growth hormone-releasing hormone. Br. J. Haematol. 2018, 181, 476–485. [Google Scholar] [CrossRef]
- Klukovits, A.; Schally, A.V.; Szalontay, L.; Vidaurre, I.; Papadia, A.; Zarandi, M.; Varga, J.L.; Block, N.L.; Halmos, G. Novel antagonists of growth hormone-releasing hormone inhibit growth and vascularization of human experimental ovarian cancers. Cancer 2012, 118, 670–680. [Google Scholar] [CrossRef]
- Solloso, A.; Barreiro, L.; Seoane, R.; Nogueira, E.; Canibano, C.; Alvarez, C.V.; Zalvide, J.; Dieguez, C.; Pombo, C.M. GHRH proliferative action on somatotrophs is cell-type specific and dependent on Pit-1/GHF-1 expression. J. Cell Physiol. 2008, 215, 140–150. [Google Scholar] [CrossRef]
- Lee, E.J.; Duan, W.R.; Kotlar, T.; Jameson, J.L. Restoration of growth hormone-releasing hormone (GHRH) responsiveness in pituitary GH3 cells by adenovirus-directed expression of the human GHRH receptor. Endocrinology 2001, 142, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Vazquez-Borrego, M.C.; Fuentes-Fayos, A.C.; Herrera-Martinez, A.D.; Venegas-Moreno, E.; Fernando, L.; Fanciulli, A.; Moreno-Moreno, P.; Alhambra-Exposito, M.R.; Barrera-Martin, A.; Dios, E.; et al. Statins Directly Regulate Pituitary Cell Function and Exert Antitumor Effects in Pituitary Tumors. Neuroendocrinology 2020, 110, 1028–1041. [Google Scholar] [CrossRef] [PubMed]
- Vazquez-Borrego, M.C.; Fuentes-Fayos, A.C.; Herrera-Martinez, A.D.; L-López, F.; Ibanez-Costa, A.; Moreno-Moreno, P.; Alhambra-Exposito, M.R.; Barrera-Martin, A.; Blanco-Acevedo, C.; Dios, E.; et al. Biguanides Exert Antitumoral Actions in Pituitary Tumor Cells Through AMPK-Dependent and -Independent Mechanisms. J. Clin. Endocrinol. Metab. 2019, 104, 3501–3513. [Google Scholar] [CrossRef]
- Gesmundo, I.; Silvagno, F.; Banfi, D.; Monica, V.; Fanciulli, A.; Gamba, G.; Congiusta, N.; Libener, R.; Riganti, C.; Ghigo, E.; et al. Calcitriol Inhibits Viability and Proliferation in Human Malignant Pleural Mesothelioma Cells. Front. Endocrinol. 2020, 11, 559586. [Google Scholar] [CrossRef] [PubMed]
- Ibanez-Costa, A.; Gahete, M.D.; Rivero-Cortes, E.; Rincon-Fernandez, D.; Nelson, R.; Beltran, M.; de la Riva, A.; Japon, M.A.; Venegas-Moreno, E.; Galvez, M.A.; et al. In1-ghrelin splicing variant is overexpressed in pituitary adenomas and increases their aggressive features. Sci. Rep. 2015, 5, 8714. [Google Scholar] [CrossRef]
- Zeytin, F.N.; Gick, G.G.; Brazeau, P.; Ling, N.; McLaughlin, M.; Bancroft, C. Growth hormone (GH)-releasing factor does not regulate GH release or GH mRNA levels in GH3 cells. Endocrinology 1984, 114, 2054–2059. [Google Scholar] [CrossRef]
- Gallo, D.; Gesmundo, I.; Trovato, L.; Pera, G.; Gargantini, E.; Minetto, M.A.; Ghigo, E.; Granata, R. GH-Releasing Hormone Promotes Survival and Prevents TNF-alpha-Induced Apoptosis and Atrophy in C2C12 Myotubes. Endocrinology 2015, 156, 3239–3252. [Google Scholar] [CrossRef]
- Sheehan, J.; Rainey, J.; Nguyen, J.; Grimsdale, R.; Han, S. Temozolomide-induced inhibition of pituitary adenoma cells. J. Neurosurg. 2011, 114, 354–358. [Google Scholar] [CrossRef]
- Dai, C.; Zhang, B.; Liu, X.; Guo, K.; Ma, S.; Cai, F.; Yang, Y.; Yao, Y.; Feng, M.; Bao, X.; et al. Pyrimethamine sensitizes pituitary adenomas cells to temozolomide through cathepsin B-dependent and caspase-dependent apoptotic pathways. Int. J. Cancer. 2013, 133, 1982–1993. [Google Scholar] [CrossRef][Green Version]
- Chou, T.C. Drug combination studies and their synergy quantification using the Chou-Talalay method. Cancer Res. 2010, 70, 440–446. [Google Scholar] [CrossRef]
- Kim, E.; Sohn, S.; Lee, M.; Park, C.; Jung, J.; Park, S. Effect of gsp oncogene on somatostatin receptor subtype 1 and 2 mRNA levels in GHRH-responsive GH3 cells. Pituitary 2005, 8, 155–162. [Google Scholar] [CrossRef]
- Schofield, J.G. Role of cyclic 3′,5′-adenosine monophosphate in the release of growth hormone in vitro. Nature 1967, 215, 1382–1383. [Google Scholar] [CrossRef] [PubMed]
- Billestrup, N.; Swanson, L.W.; Vale, W. Growth hormone-releasing factor stimulates proliferation of somatotrophs in vitro. Proc. Natl. Acad. Sci. USA 1986, 83, 6854–6857. [Google Scholar] [CrossRef]
- Cuny, T.; Gerard, C.; Saveanu, A.; Barlier, A.; Enjalbert, A. Physiopathology of somatolactotroph cells: From transduction mechanisms to cotargeting therapy. Ann. N. Y. Acad. Sci. 2011, 1220, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Kineman, R.D.; Luque, R.M. Evidence that ghrelin is as potent as growth hormone (GH)-releasing hormone (GHRH) in releasing GH from primary pituitary cell cultures of a nonhuman primate (Papio anubis), acting through intracellular signaling pathways distinct from GHRH. Endocrinology 2007, 148, 4440–4449. [Google Scholar] [CrossRef]
- Kanasaki, H.; Yonehara, T.; Yamamoto, H.; Takeuchi, Y.; Fukunaga, K.; Takahashi, K.; Miyazaki, K.; Miyamoto, E. Differential regulation of pituitary hormone secretion and gene expression by thyrotropin-releasing hormone. A role for mitogen-activated protein kinase signaling cascade in rat pituitary GH3 cells. Biol. Reprod. 2002, 67, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Tsukamoto, N.; Otsuka, F.; Miyoshi, T.; Inagaki, K.; Nakamura, E.; Terasaka, T.; Takeda, M.; Ogura, T.; Iwasaki, Y.; Makino, H. Functional interaction of bone morphogenetic protein and growth hormone releasing peptide in adrenocorticotropin regulation by corticotrope cells. Mol. Cell Endocrinol. 2011, 344, 41–50. [Google Scholar] [CrossRef]
- Schally, A.V.; Wang, H.; He, J.; Cai, R.; Sha, W.; Popovics, P.; Perez, R.; Vidaurre, I.; Zhang, X. Agonists of growth hormone-releasing hormone (GHRH) inhibit human experimental cancers in vivo by down-regulating receptors for GHRH. Proc. Natl. Acad. Sci. USA 2018, 115, 12028–12033. [Google Scholar] [CrossRef]
- Bogner, E.M.; Daly, A.F.; Gulde, S.; Karhu, A.; Irmler, M.; Beckers, J.; Mohr, H.; Beckers, A.; Pellegata, N.S. miR-34a is upregulated in AIP-mutated somatotropinomas and promotes octreotide resistance. Int. J. Cancer. 2020, 147, 3523–3538. [Google Scholar] [CrossRef]
- Hubina, E.; Nanzer, A.M.; Hanson, M.R.; Ciccarelli, E.; Losa, M.; Gaia, D.; Papotti, M.; Terreni, M.R.; Khalaf, S.; Jordan, S.; et al. Somatostatin analogues stimulate p27 expression and inhibit the MAP kinase pathway in pituitary tumours. Eur. J. Endocrinol. 2006, 155, 371–379. [Google Scholar] [CrossRef]
- Danila, D.C.; Haidar, J.N.; Zhang, X.; Katznelson, L.; Culler, M.D.; Klibanski, A. Somatostatin receptor-specific analogs: Effects on cell proliferation and growth hormone secretion in human somatotroph tumors. J. Clin. Endocrinol. Metab. 2001, 86, 2976–2981. [Google Scholar] [CrossRef]
- Lopes, M.B.; Gaylinn, B.D.; Thorner, M.O.; Stoler, M.H. Growth hormone-releasing hormone receptor mRNA in acromegalic pituitary tumors. Am. J. Pathol. 1997, 150, 1885–1891. [Google Scholar]
- Fairlie, W.D.; Lee, E.F. Co-Operativity between MYC and BCL-2 Pro-Survival Proteins in Cancer. Int. J. Mol. Sci. 2021, 22, 2841. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.G.; Johnston, C.F.; Atkinson, A.B.; Heaney, A.P.; Mirakhur, M.; Buchanan, K.D. Expression of bcl-2 oncoprotein in pituitary tumours: Comparison with c-myc. J. Clin. Pathol. 1996, 49, 795–797. [Google Scholar] [CrossRef] [PubMed]
- Barabutis, N.; Siejka, A. The highly interrelated GHRH, p53, and Hsp90 universe. Cell Biol. Int. 2020, 44, 1558–1563. [Google Scholar] [CrossRef]
- Chesnokova, V.; Zhou, C.; Ben-Shlomo, A.; Zonis, S.; Tani, Y.; Ren, S.G.; Melmed, S. Growth hormone is a cellular senescence target in pituitary and nonpituitary cells. Proc. Natl. Acad. Sci. USA 2013, 110, E3331–E3339. [Google Scholar] [CrossRef]
- Banks, W.A.; Morley, J.E.; Farr, S.A.; Price, T.O.; Ercal, N.; Vidaurre, I.; Schally, A.V. Effects of a growth hormone-releasing hormone antagonist on telomerase activity, oxidative stress, longevity, and aging in mice. Proc. Natl. Acad. Sci. USA 2010, 107, 22272–22277. [Google Scholar] [CrossRef]
- De Sousa, S.M.C.; McCormack, A.I. Aggressive Pituitary Tumors and Pituitary Carcinomas. In Endotext–Comprehensive Free Online Endocrinology Book (www.endotext.org); Feingold, K.R., Anawalt, B., Boyce, A., Chrousos, G., de Herder, W.W., Dhatariya, K., Dungan, K., Grossman, A., Hershman, J.M., Eds.; Endotext: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Perry, S.J.; Junger, S.; Kohout, T.A.; Hoare, S.R.; Struthers, R.S.; Grigoriadis, D.E.; Maki, R.A. Distinct conformations of the corticotropin releasing factor type 1 receptor adopted following agonist and antagonist binding are differentially regulated. J. Biol. Chem. 2005, 280, 11560–11568. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Ramirez, L.C.; Trivellin, G.; Stratakis, C.A. Cyclic 3′,5′-adenosine monophosphate (cAMP) signaling in the anterior pituitary gland in health and disease. Mol. Cell Endocrinol. 2018, 463, 72–86. [Google Scholar] [CrossRef]
- Vallar, L.; Spada, A.; Giannattasio, G. Altered Gs and adenylate cyclase activity in human GH-secreting pituitary adenomas. Nature 1987, 330, 566–568. [Google Scholar] [CrossRef] [PubMed]
- Ham, J.; Ivan, M.; Wynford-Thomas, D.; Scanlon, M.F. GH3 cells expressing constitutively active Gs alpha (Q227L) show enhanced hormone secretion and proliferation. Mol. Cell Endocrinol. 1997, 127, 41–47. [Google Scholar] [CrossRef]
- Ben-Shlomo, A.; Deng, N.; Ding, E.; Yamamoto, M.; Mamelak, A.; Chesnokova, V.; Labadzhyan, A.; Melmed, S. DNA damage and growth hormone hypersecretion in pituitary somatotroph adenomas. J. Clin. Investig. 2020, 130, 5738–5755. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gesmundo, I.; Granato, G.; Fuentes-Fayos, A.C.; Alvarez, C.V.; Dieguez, C.; Zatelli, M.C.; Congiusta, N.; Banfi, D.; Prencipe, N.; Leone, S.; et al. Antagonists of Growth Hormone-Releasing Hormone Inhibit the Growth of Pituitary Adenoma Cells by Hampering Oncogenic Pathways and Promoting Apoptotic Signaling. Cancers 2021, 13, 3950. https://doi.org/10.3390/cancers13163950
Gesmundo I, Granato G, Fuentes-Fayos AC, Alvarez CV, Dieguez C, Zatelli MC, Congiusta N, Banfi D, Prencipe N, Leone S, et al. Antagonists of Growth Hormone-Releasing Hormone Inhibit the Growth of Pituitary Adenoma Cells by Hampering Oncogenic Pathways and Promoting Apoptotic Signaling. Cancers. 2021; 13(16):3950. https://doi.org/10.3390/cancers13163950
Chicago/Turabian StyleGesmundo, Iacopo, Giuseppina Granato, Antonio C. Fuentes-Fayos, Clara V. Alvarez, Carlos Dieguez, Maria Chiara Zatelli, Noemi Congiusta, Dana Banfi, Nunzia Prencipe, Sheila Leone, and et al. 2021. "Antagonists of Growth Hormone-Releasing Hormone Inhibit the Growth of Pituitary Adenoma Cells by Hampering Oncogenic Pathways and Promoting Apoptotic Signaling" Cancers 13, no. 16: 3950. https://doi.org/10.3390/cancers13163950
APA StyleGesmundo, I., Granato, G., Fuentes-Fayos, A. C., Alvarez, C. V., Dieguez, C., Zatelli, M. C., Congiusta, N., Banfi, D., Prencipe, N., Leone, S., Brunetti, L., Castaño, J. P., Luque, R. M., Cai, R., Sha, W., Ghigo, E., Schally, A. V., & Granata, R. (2021). Antagonists of Growth Hormone-Releasing Hormone Inhibit the Growth of Pituitary Adenoma Cells by Hampering Oncogenic Pathways and Promoting Apoptotic Signaling. Cancers, 13(16), 3950. https://doi.org/10.3390/cancers13163950













