Depatuxizumab Mafodotin (Depatux-M) Plus Temozolomide in Recurrent Glioblastoma Patients: Real-World Experience from a Multicenter Study of Italian Association of Neuro-Oncology (AINO)
Abstract
Simple Summary
Abstract
1. Introduction
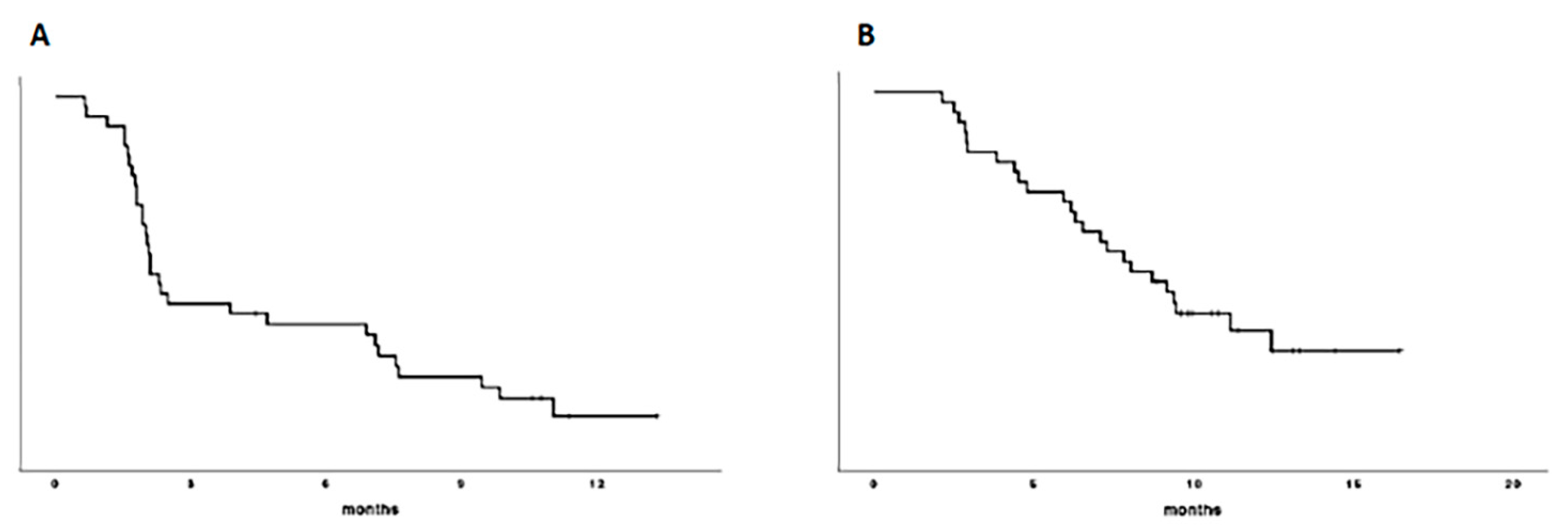
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Design and Patients
4.2. Study Procedures
4.3. Outcomes and Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stupp, R.; Mason, W.P.; van den Bent, M.J.; Weller, M.; Fisher, B.; Taphoorn, M.J.; Belanger, K.; Brandes, A.A.; Marosi, C.; Bogdahn, U.; et al. Radiotherapy plus Concomitant and Adjuvant Temozolomide for Glioblastoma. N. Engl. J. Med. 2005, 352, 987–996. [Google Scholar] [CrossRef]
- Birzu, C.; French, P.; Caccese, M.; Cerretti, G.; Idbaih, A.; Zagonel, V.; Lombardi, G. Recurrent Glioblastoma: From Molecular Landscape to New Treatment Perspectives. Cancers 2020, 13, 47. [Google Scholar] [CrossRef] [PubMed]
- Lombardi, G.; Idbaih, A.; Le Rhun, E.; Preusser, M.; Zagonel, V.; French, P. A New Landscape for Systemic Pharmacotherapy of Recurrent Glioblastoma? Cancers 2020, 12, 3775. [Google Scholar] [CrossRef] [PubMed]
- Wick, W.; Gorlia, T.; Bendszus, M.; Taphoorn, M.; Sahm, F.; Harting, I.; Brandes, A.A.; Taal, W.; Domont, J.; Idbaih, A.; et al. Lomustine and Bevacizumab in Progressive Glioblastoma. N. Engl. J. Med. 2017, 377, 1954–1963. [Google Scholar] [CrossRef] [PubMed]
- Lombardi, G.; Barresi, V.; Indraccolo, S.; Simbolo, M.; Fassan, M.; Mandruzzato, S.; Simonelli, M.; Caccese, M.; Pizzi, M.; Fassina, A.; et al. Pembrolizumab Activity in Recurrent High-Grade Gliomas with Partial or Complete Loss of Mismatch Repair Protein Expression: A Monocentric, Observational and Prospective Pilot Study. Cancers 2020, 12, 2283. [Google Scholar] [CrossRef]
- Reardon, D.A.; Brandes, A.A.; Omuro, A.; Mulholland, P.; Lim, M.; Wick, A.; Baehring, J.; Ahluwalia, M.S.; Roth, P.; Bähr, O.; et al. Effect of Nivolumab vs Bevacizumab in Patients With Recurrent Glioblastoma: The CheckMate 143 Phase 3 Randomized Clinical Trial. JAMA Oncol. 2020. [Google Scholar] [CrossRef]
- Lombardi, G.; De Salvo, G.L.; Brandes, A.A.; Eoli, M.; Ruda, R.; Faedi, M.; Lolli, I.; Pace, A.; Daniele, B.; Pasqualetti, F.; et al. Regorafenib Compared with Lomustine in Patients with Relapsed Glioblastoma (REGOMA): A Multicentre, Open-Label, Randomised, Controlled, Phase 2 Trial. Lancet Oncol. 2019, 20, 110–119. [Google Scholar] [CrossRef]
- Kaley, T.; Touat, M.; Subbiah, V.; Hollebecque, A.; Rodon, J.; Lockhart, A.C.; Keedy, V.; Bielle, F.; Hofheinz, R.-D.; Joly, F.; et al. BRAF Inhibition in BRAFV600-Mutant Gliomas: Results From the VE-BASKET Study. J. Clin. Oncol. 2018, 36, 3477–3484. [Google Scholar] [CrossRef] [PubMed]
- Brennan, C.W.; Verhaak, R.G.; McKenna, A.; Campos, B.; Noushmehr, H.; Salama, S.R.; Zheng, S.; Chakravarty, D.; Sanborn, J.Z.; Berman, S.H.; et al. The Somatic Genomic Landscape of Glioblastoma. Cell 2013, 155, 462–477. [Google Scholar] [CrossRef]
- Chakravarti, A.; Wang, M.; Robins, H.I.; Lautenschlaeger, T.; Curran, W.J.; Brachman, D.G.; Schultz, C.J.; Choucair, A.; Dolled-Filhart, M.; Christiansen, J.; et al. RTOG 0211: A Phase 1/2 Study of Radiation Therapy with Concurrent Gefitinib for Newly Diagnosed Glioblastoma Patients. Int. J. Radiat. Oncol. Biol. Phys. 2013, 85, 1206–1211. [Google Scholar] [CrossRef]
- Raizer, J.J.; Abrey, L.E.; Lassman, A.B.; Chang, S.M.; Lamborn, K.R.; Kuhn, J.G.; Yung, W.K.A.; Gilbert, M.R.; Aldape, K.A.; Wen, P.Y.; et al. A Phase II Trial of Erlotinib in Patients with Recurrent Malignant Gliomas and Nonprogressive Glioblastoma Multiforme Postradiation Therapy. Neuro Oncol. 2010, 12, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Reardon, D.A.; Nabors, L.B.; Mason, W.P.; Perry, J.R.; Shapiro, W.; Kavan, P.; Mathieu, D.; Phuphanich, S.; Cseh, A.; Fu, Y.; et al. Phase I/Randomized Phase II Study of Afatinib, an Irreversible ErbB Family Blocker, with or without Protracted Temozolomide in Adults with Recurrent Glioblastoma. Neuro Oncol. 2015, 17, 430–439. [Google Scholar] [CrossRef] [PubMed]
- Phillips, A.C.; Boghaert, E.R.; Vaidya, K.S.; Mitten, M.J.; Norvell, S.; Falls, H.D.; DeVries, P.J.; Cheng, D.; Meulbroek, J.A.; Buchanan, F.G.; et al. ABT-414, an Antibody-Drug Conjugate Targeting a Tumor-Selective EGFR Epitope. Mol. Cancer Ther. 2016, 15, 661–669. [Google Scholar] [CrossRef] [PubMed]
- French, P.J.; Eoli, M.; Sepulveda, J.M.; de Heer, I.; Kros, J.M.; Walenkamp, A.; Frenel, J.-S.; Franceschi, E.; Clement, P.M.; Weller, M.; et al. Defining EGFR Amplification Status for Clinical Trial Inclusion. Neuro Oncol. 2019, 21, 1263–1272. [Google Scholar] [CrossRef]
- Lassman, A.B.; van den Bent, M.J.; Gan, H.K.; Reardon, D.A.; Kumthekar, P.; Butowski, N.; Lwin, Z.; Mikkelsen, T.; Nabors, L.B.; Papadopoulos, K.P.; et al. Safety and Efficacy of Depatuxizumab Mafodotin + Temozolomide in Patients with EGFR-Amplified, Recurrent Glioblastoma: Results from an International Phase I Multicenter Trial. Neuro Oncol. 2019, 21, 106–114. [Google Scholar] [CrossRef]
- Van Den Bent, M.; Eoli, M.; Sepulveda, J.M.; Smits, M.; Walenkamp, A.; Frenel, J.-S.; Franceschi, E.; Clement, P.M.; Chinot, O.; De Vos, F.; et al. INTELLANCE 2/EORTC 1410 Randomized Phase II Study of Depatux-M Alone and with Temozolomide vs Temozolomide or Lomustine in Recurrent EGFR Amplified Glioblastoma. Neuro Oncol. 2020, 22, 684–693. [Google Scholar] [CrossRef]
- Draaisma, K.; Chatzipli, A.; Taphoorn, M.; Kerkhof, M.; Weyerbrock, A.; Sanson, M.; Hoeben, A.; Lukacova, S.; Lombardi, G.; Leenstra, S.; et al. Molecular Evolution of IDH Wild-Type Glioblastomas Treated With Standard of Care Affects Survival and Design of Precision Medicine Trials: A Report From the EORTC 1542 Study. J. Clin. Oncol. 2020, 38, 81–99. [Google Scholar] [CrossRef]
- Brandes, A.A.; Gil-Gil, M.; Saran, F.; Carpentier, A.F.; Nowak, A.K.; Mason, W.; Zagonel, V.; Dubois, F.; Finocchiaro, G.; Fountzilas, G.; et al. A Randomized Phase II Trial (TAMIGA) Evaluating the Efficacy and Safety of Continuous Bevacizumab Through Multiple Lines of Treatment for Recurrent Glioblastoma. Oncologist 2019, 24, 521–528. [Google Scholar] [CrossRef]
- Parrozzani, R.; Lombardi, G.; Midena, E.; Londei, D.; Padovan, M.; Marchione, G.; Caccese, M.; Midena, G.; Zagonel, V.; Frizziero, L. Ocular Side Effects of EGFR-Inhibitor ABT-414 in Recurrent Glioblastoma: A Long-Term Safety Study. Front. Oncol. 2020, 10, 593461. [Google Scholar] [CrossRef]
- Parrozzani, R.; Lombardi, G.; Midena, E.; Leonardi, F.; Londei, D.; Padovan, M.; Caccese, M.; Marchione, G.; Bini, S.; Zagonel, V.; et al. Corneal Side Effects Induced by EGFR-Inhibitor Antibody-Drug Conjugate ABT-414 in Patients with Recurrent Glioblastoma: A Prospective Clinical and Confocal Microscopy Study. Ther. Adv. Med. Oncol. 2020, 12, 1758835920907543. [Google Scholar] [CrossRef] [PubMed]
- Hoogstrate, Y.; Vallentgoed, W.; Kros, J.M.; de Heer, I.; de Wit, M.; Eoli, M.; Sepulveda, J.M.; Walenkamp, A.M.E.; Frenel, J.-S.; Franceschi, E.; et al. EGFR Mutations Are Associated with Response to Depatux-m in Combination with Temozolomide and Result in a Receptor That Is Hypersensitive to Ligand. Neuro Oncol. Adv. 2020, 2, vdz051. [Google Scholar] [CrossRef] [PubMed]
- Wen, P.Y.; Macdonald, D.R.; Reardon, D.A.; Cloughesy, T.F.; Sorensen, A.G.; Galanis, E.; Degroot, J.; Wick, W.; Gilbert, M.R.; Lassman, A.B.; et al. Updated Response Assessment Criteria for High-Grade Gliomas: Response Assessment in Neuro-Oncology Working Group. J. Clin. Oncol. 2010, 28, 1963–1972. [Google Scholar] [CrossRef] [PubMed]
| Variables | Number (%) |
|---|---|
| Median age (range) | 57 (38–73) |
| Gender | |
| Male | 25 (69%) |
| Female | 11 (31%) |
| ECOG PS | |
| 0–1 | 28 (88%) |
| 2 | 8 (12%) |
| MGMT status | |
| Methylated | 23 (64%) |
| Unmethylated | 13 (36%) |
| IDH 1–2 status | |
| Mutated | 1 (3%) |
| Wild Type | 34 (94%) |
| Not available | 1 (3%) |
| Line of treatment | |
| 2nd line | 15 (42%) |
| >2nd line | 21 (58%) |
| Start of Depatux-M since TMZ | |
| >16 weeks | 29 (81%) |
| ≤16 weeks | 7 (19%) |
| Variables | Subgroups | PFS | OS | ||
|---|---|---|---|---|---|
| Median (ms) | p | Median (ms) | p | ||
| MGMT status | 0.05 | 0.02 | |||
| Met | 2.3 | 11.7 | |||
| Unmet | 2.004 | 6.5 | |||
| ECOG PS | 0–1 | 2.1 | 0.5 | 9.3 | 0.1 |
| 2 | 2.1 | 7.09 | |||
| Line of Depatux-M treatment | 0.14 | 0.3 | |||
| 2nd line | 2.3 | 9.4 | |||
| >2nd line | 2.04 | 7.1 | |||
| Start of Depatux-M since TMZ | 0.14 | 0.45 | |||
| ≤16 wks | 4.6 | 9.1 | |||
| >16 wks | 2.1 | 8.04 | |||
| Variables | PFS | OS | ||
|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | |
| MGMT status | 0.6 (0.2–1.2) | 0.1 | 0.3 (0.1–0.9) | 0.03 |
| ECOG PS | - | - | 1.7 (0.6–4.8) | 0.3 |
| Line of treatment | 0.9 (0.3–2.5) | 0.9 | - | - |
| Start of Depatux-M since TMZ | 2.2 (0.3–2.5) | 0.14 | - | - |
| Type of Response | N (%) |
|---|---|
| Complete response | 1 (3%) |
| Partial response | 4 (11%) |
| Objective response | 5 (14%) |
| Stable disease | 13 (36%) |
| Disease control | 18 (50%) |
| Progressive disease | 18 (50%) |
| Variable | χ2 | p Value |
|---|---|---|
| MGMT | 1.4 | 0.2 |
| ECOG PS | 0.04 | 0.8 |
| Line of treatment | 0.3 | 0.53 |
| Start of Depatux-M since TMZ | 0.34 | 0.2 |
| Adverse Event | Grade | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Eye disorders | 5 (14%) | 20 (56%) | 4 (11%) | 0 |
| Keratitis | 5 (14%) | 15 (42%) | 4 (11%) | 0 |
| Photophobia | 0 | 3 (8%) | 0 | 0 |
| Eye Pain | 0 | 1 (3%) | 0 | 0 |
| Conjunctivitis | 0 | 1 (3%) | 0 | 0 |
| Hematology | 7 (19%) | 4 (11%) | 4 (11%) | 2 (6%) |
| Hypertransaminasemia | 1 (3%) | 1 (3%) | 2 (6%) | 0 |
| Hypertension | 1 (3%) | 0 | 0 | 0 |
| Venous Thrombosis | 0 | 0 | 2 (6%) | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Padovan, M.; Eoli, M.; Pellerino, A.; Rizzato, S.; Caserta, C.; Simonelli, M.; Michiara, M.; Caccese, M.; Anghileri, E.; Cerretti, G.; et al. Depatuxizumab Mafodotin (Depatux-M) Plus Temozolomide in Recurrent Glioblastoma Patients: Real-World Experience from a Multicenter Study of Italian Association of Neuro-Oncology (AINO). Cancers 2021, 13, 2773. https://doi.org/10.3390/cancers13112773
Padovan M, Eoli M, Pellerino A, Rizzato S, Caserta C, Simonelli M, Michiara M, Caccese M, Anghileri E, Cerretti G, et al. Depatuxizumab Mafodotin (Depatux-M) Plus Temozolomide in Recurrent Glioblastoma Patients: Real-World Experience from a Multicenter Study of Italian Association of Neuro-Oncology (AINO). Cancers. 2021; 13(11):2773. https://doi.org/10.3390/cancers13112773
Chicago/Turabian StylePadovan, Marta, Marica Eoli, Alessia Pellerino, Simona Rizzato, Claudia Caserta, Matteo Simonelli, Maria Michiara, Mario Caccese, Elena Anghileri, Giulia Cerretti, and et al. 2021. "Depatuxizumab Mafodotin (Depatux-M) Plus Temozolomide in Recurrent Glioblastoma Patients: Real-World Experience from a Multicenter Study of Italian Association of Neuro-Oncology (AINO)" Cancers 13, no. 11: 2773. https://doi.org/10.3390/cancers13112773
APA StylePadovan, M., Eoli, M., Pellerino, A., Rizzato, S., Caserta, C., Simonelli, M., Michiara, M., Caccese, M., Anghileri, E., Cerretti, G., Rudà, R., Zagonel, V., & Lombardi, G. (2021). Depatuxizumab Mafodotin (Depatux-M) Plus Temozolomide in Recurrent Glioblastoma Patients: Real-World Experience from a Multicenter Study of Italian Association of Neuro-Oncology (AINO). Cancers, 13(11), 2773. https://doi.org/10.3390/cancers13112773









