A Nomogram Predicting Progression Free Survival in Patients with Gastrointestinal Stromal Tumor Receiving Sunitinib: Incorporating Pre-Treatment and Post-Treatment Parameters
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Study Design and Follow-Up Study
2.3. Analysis of KIT and PDGFRA Mutations
2.4. Definition of Sarcopenia
2.5. Nomogram Creation
2.6. Statistical Analysis
3. Results
3.1. Clinicopathological Characteristics of Patients
3.2. Independent Prognostic Factors in the Training Cohort
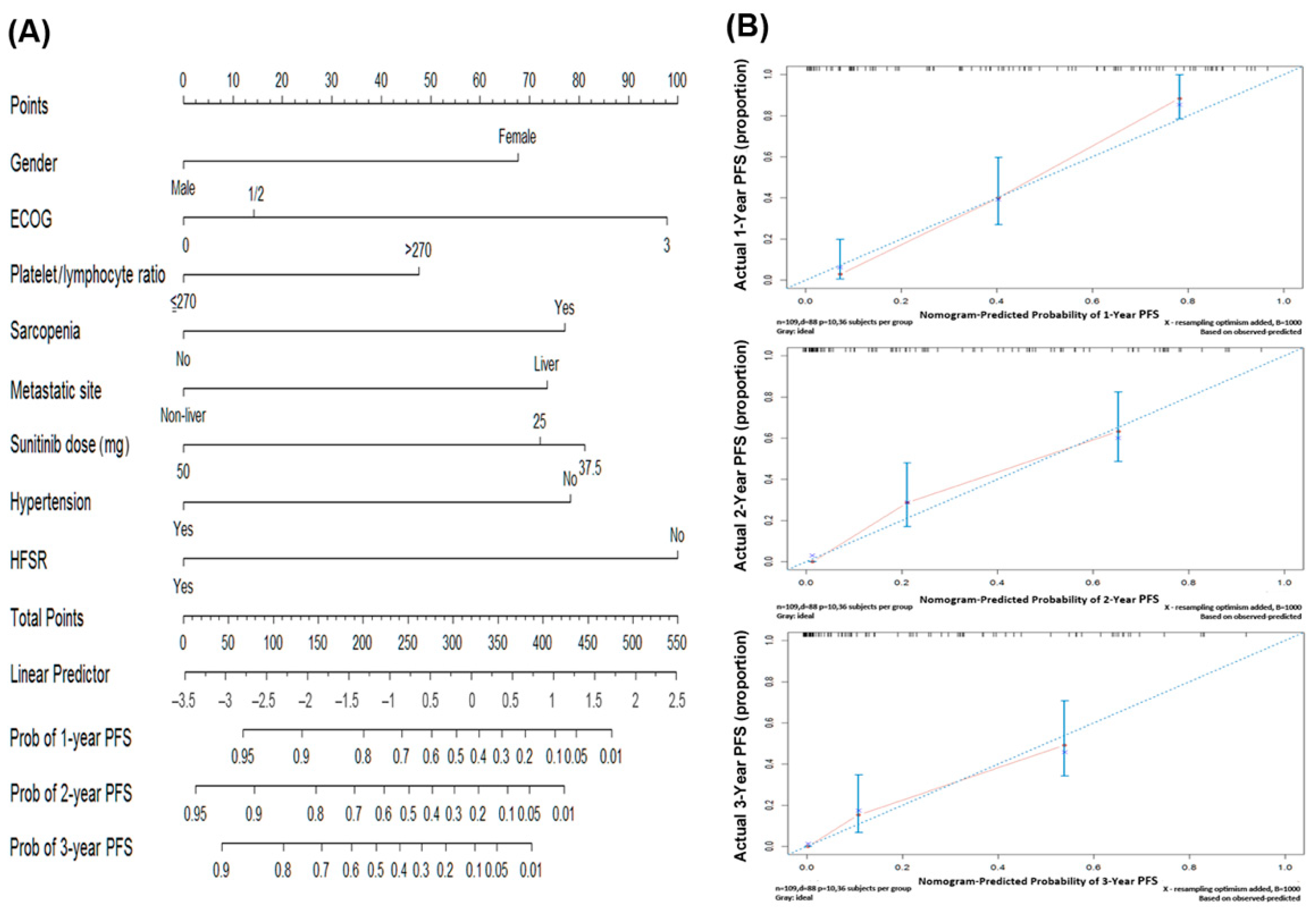
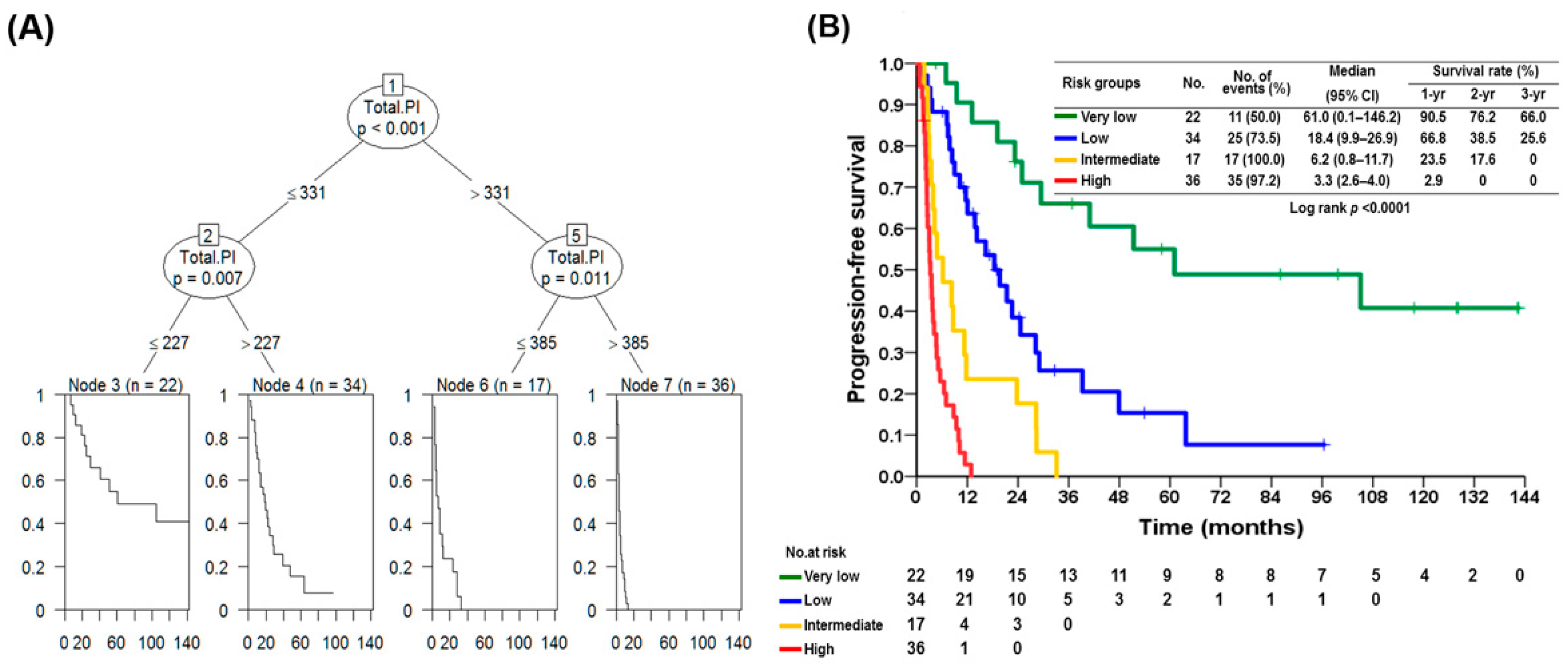
3.3. Prognostic Nomogram for PFS and Risk Strastification
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rossi, C.R.; Mocellin, S.; Mencarelli, R.; Foletto, M.; Pilati, P.; Nitti, D.; Lise, M. Gastrointestinal stromal tumors: From a surgical to a molecular approach. Int. J. Cancer 2003, 107, 171–176. [Google Scholar] [CrossRef]
- De Matteo, R.P.; Lewis, J.J.; Leung, D.; Mudan, S.S.; Woodruff, J.M.; Brennan, M.F. Two hundred gastrointestinal stromal tumors: Recurrence patterns and prognostic factors for survival. Ann. Surg. 2000, 231, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Kindblom, L.G.; Remotti, H.E.; Aldenborg, F.; Meis-Kindblom, J.M. Gastrointestinal pacemaker cell tumor (GIPACT): Gastrointestinal stromal tumors show phenotypic characteristics of the interstitial cells of Cajal. Am. J. Pathol. 1998, 152, 1259–1269. [Google Scholar] [PubMed]
- Hirota, S.; Isozaki, K.; Moriyama, Y.; Hashimoto, K.; Nishida, T.; Ishiguro, S.; Kawano, K.; Hanada, M.; Kurata, A.; Takeda, M.; et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science 1998, 279, 577–580. [Google Scholar] [CrossRef]
- Demetri, G.D.; von Mehren, M.; Blanke, C.D.; Van den Abbeele, A.D.; Eisenberg, B.; Roberts, P.J.; Heinrich, M.C.; Tuveson, D.A.; Singer, S.; Janicek, M.; et al. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N. Engl. J. Med. 2002, 347, 472–480. [Google Scholar] [CrossRef] [PubMed]
- Verweij, J.; Casali, P.G.; Zalcberg, J.; LeCesne, A.; Reichardt, P.; Blay, J.Y.; Issels, R.; van Oosterom, A.; Hogendoorn, P.C.; Van Glabbeke, M.; et al. Progression-free survival in gastrointestinal stromal tumours with high-dose imatinib: Randomised trial. Lancet 2004, 364, 1127–1134. [Google Scholar] [CrossRef]
- Yeh, C.N.; Chen, T.W.; Wu, T.J.; Hsueh, S.; Jan, Y.Y. Treatment of patients with advanced gastrointestinal stromal tumor of small bowel: Implications of imatinib mesylate. World J. Gastroenterol. 2006, 12, 3760–3765. [Google Scholar] [CrossRef]
- Yeh, C.N.; Chen, T.W.; Lee, H.L.; Liu, Y.Y.; Chao, T.C.; Hwang, T.L.; Jan, Y.Y.; Chen, M.F. Kinase mutations and imatinib mesylate response for 64 Taiwanese with advanced GIST: Preliminary experience from Chang Gung Memorial Hospital. Ann. Surg. Oncol. 2007, 14, 1123–1128. [Google Scholar] [CrossRef]
- Yeh, C.N.; Chen, Y.Y.; Tseng, J.H.; Chen, J.S.; Chen, T.W.; Tsai, C.Y.; Cheng, C.T.; Jan, Y.Y.; Chen, M.F. Imatinib Mesylate for Patients with Recurrent or Metastatic Gastrointestinal Stromal Tumors Expressing KIT: A Decade Experience from Taiwan. Transl. Oncol. 2011, 4, 328–335. [Google Scholar] [CrossRef]
- Osusky, K.L.; Hallahan, D.E.; Fu, A.; Ye, F.; Shyr, Y.; Geng, L. The receptor tyrosine kinase inhibitor SU11248 impedes endothelial cell migration, tubule formation, and blood vessel formation in vivo, but has little effect on existing tumor vessels. Angiogenesis 2004, 7, 225–233. [Google Scholar] [CrossRef]
- Abrams, T.J.; Lee, L.B.; Murray, L.J.; Pryer, N.K.; Cherrington, J.M. SU11248 inhibits KIT and platelet-derived growth factor receptor beta in preclinical models of human small cell lung cancer. Mol. Cancer Ther. 2003, 2, 471–478. [Google Scholar] [PubMed]
- Mendel, D.B.; Laird, A.D.; Xin, X.; Louie, S.G.; Christensen, J.G.; Li, G.; Schreck, R.E.; Abrams, T.J.; Ngai, T.J.; Lee, L.B.; et al. In vivo antitumor activity of SU11248, a novel tyrosine kinase inhibitor targeting vascular endothelial growth factor and platelet-derived growth factor receptors: Determination of a pharmacokinetic/pharmacodynamic relationship. Clin. Cancer Res. 2003, 9, 327–337. [Google Scholar] [PubMed]
- Murray, L.J.; Abrams, T.J.; Long, K.R.; Ngai, T.J.; Olson, L.M.; Hong, W.; Keast, P.K.; Brassard, J.A.; O’Farrell, A.M.; Cherrington, J.M.; et al. SU11248 inhibits tumor growth and CSF-1R-dependent osteolysis in an experimental breast cancer bone metastasis model. Clin. Exp. Metastasis 2003, 20, 757–766. [Google Scholar] [CrossRef]
- O’Farrell, A.M.; Abrams, T.J.; Yuen, H.A.; Ngai, T.J.; Louie, S.G.; Yee, K.W.; Wong, L.M.; Hong, W.; Lee, L.B.; Town, A.; et al. SU11248 is a novel FLT3 tyrosine kinase inhibitor with potent activity in vitro and in vivo. Blood 2003, 101, 3597–3605. [Google Scholar] [CrossRef]
- Schueneman, A.J.; Himmelfarb, E.; Geng, L.; Tan, J.; Donnelly, E.; Mendel, D.; McMahon, G.; Hallahan, D.E. SU11248 maintenance therapy prevents tumor regrowth after fractionated irradiation of murine tumor models. Cancer Res. 2003, 63, 4009–4016. [Google Scholar]
- Demetri, G.D.; van Oosterom, A.T.; Garrett, C.R.; Blackstein, M.E.; Shah, M.H.; Verweij, J.; McArthur, G.; Judson, I.R.; Heinrich, M.C.; Morgan, J.A.; et al. Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: A randomised controlled trial. Lancet 2006, 368, 1329–1338. [Google Scholar] [CrossRef]
- International Bladder Cancer Nomogram, C.; Bochner, B.H.; Kattan, M.W.; Vora, K.C. Postoperative nomogram predicting risk of recurrence after radical cystectomy for bladder cancer. J. Clin. Oncol. 2006, 24, 3967–3972. [Google Scholar]
- Karakiewicz, P.I.; Briganti, A.; Chun, F.K.; Trinh, Q.D.; Perrotte, P.; Ficarra, V.; Cindolo, L.; De la Taille, A.; Tostain, J.; Mulders, P.F.; et al. Multi-institutional validation of a new renal cancer-specific survival nomogram. J. Clin. Oncol. 2007, 25, 1316–1322. [Google Scholar] [CrossRef] [PubMed]
- Wierda, W.G.; O’Brien, S.; Wang, X.; Faderl, S.; Ferrajoli, A.; Do, K.A.; Cortes, J.; Thomas, D.; Garcia-Manero, G.; Koller, C.; et al. Prognostic nomogram and index for overall survival in previously untreated patients with chronic lymphocytic leukemia. Blood 2007, 109, 4679–4685. [Google Scholar] [CrossRef]
- Mariani, L.; Miceli, R.; Kattan, M.W.; Brennan, M.F.; Colecchia, M.; Fiore, M.; Casali, P.G.; Gronchi, A. Validation and adaptation of a nomogram for predicting the survival of patients with extremity soft tissue sarcoma using a three-grade system. Cancer 2005, 103, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Sternberg, C.N. Are nomograms better than currently available stage groupings for bladder cancer? J. Clin. Oncol. 2006, 24, 3819–3820. [Google Scholar] [CrossRef]
- Wang, L.; Hricak, H.; Kattan, M.W.; Chen, H.N.; Scardino, P.T.; Kuroiwa, K. Prediction of organ-confined prostate cancer: Incremental value of MR imaging and MR spectroscopic imaging to staging nomograms. Radiology 2006, 238, 597–603. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer. 2009, 45, 228–247. [Google Scholar] [CrossRef] [PubMed]
- Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0. Available online: https://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03/CTCAE_4.03_2010-06-14_QuickReference_8.5x11.pdf (accessed on 20 August 2020).
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef]
- Hamaguchi, Y.; Kaido, T.; Okumura, S.; Kobayashi, A.; Hammad, A.; Tamai, Y.; Inagaki, N.; Uemoto, S. Proposal for new diagnostic criteria for low skeletal muscle mass based on computed tomography imaging in Asian adults. Nutrition 2016, 32, 1200–1205. [Google Scholar] [CrossRef] [PubMed]
- Rasband, W.S.; Image, J. U.S. National Institutes of Health, Bethesda, Maryland, USA, 1997–2012. Available online: http://imagej.nih.gov/ij/ (accessed on 14 June 2020).
- Tanadini, L.G.; Steeves, J.D.; Hothorn, T.; Abel, R.; Maier, D.; Schubert, M.; Weidner, N.; Rupp, R.; Curt, A. Identifying Homogeneous Subgroups in Neurological Disorders: Unbiased Recursive Partitioning in Cervical Complete Spinal Cord Injury. Neurorehabil. Neural. Repair 2014, 28, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Reichardt, P.; Kang, Y.K.; Rutkowski, P.; Schuette, J.; Rosen, L.S.; Seddon, B.; Yalcin, S.; Gelderblom, H.; Williams, C.C., Jr.; Fumagalli, E.; et al. Clinical outcomes of patients with advanced gastrointestinal stromal tumors: Safety and efficacy in a worldwide treatment-use trial of sunitinib. Cancer 2015, 121, 1405–1413. [Google Scholar] [CrossRef]
- Yoon, D.H.; Ryu, M.H.; Ryoo, B.Y.; Beck, M.; Choi, D.R.; Cho, Y.; Lee, J.L.; Chang, H.M.; Kim, T.W.; Kang, Y.K. Sunitinib as a second-line therapy for advanced GISTs after failure of imatinib: Relationship between efficacy and tumor genotype in Korean patients. Investig. New Drugs 2012, 30, 819–827. [Google Scholar] [CrossRef]
- Matsumoto, K.; Sawaki, A.; Mizuno, N.; Hara, K.; Hijioka, S.; Niwa, Y.; Tajika, M.; Kawai, H.; Kondo, S.; Yamao, K. Clinical efficacy and safety of sunitinib after imatinib failure in Japanese patients with gastrointestinal stromal tumor. Jpn. J. Clin. Oncol. 2011, 41, 57–62. [Google Scholar] [CrossRef]
- Den Hollander, D.; Van der Graaf, W.T.A.; Desar, I.M.E.; Le Cesne, A. Predictive factors for toxicity and survival of second-line sunitinib in advanced gastrointestinal stromal tumours (GIST). Acta Oncol. 2019, 58, 1648–1654. [Google Scholar] [CrossRef]
- Demetri, G.D.; Garrett, C.R.; Schoffski, P.; Shah, M.H.; Verweij, J.; Leyvraz, S.; Hurwitz, H.I.; Pousa, A.L.; Le Cesne, A.; Goldstein, D.; et al. Complete longitudinal analyses of the randomized, placebo-controlled, phase III trial of sunitinib in patients with gastrointestinal stromal tumor following imatinib failure. Clin. Cancer Res. 2012, 18, 3170–3179. [Google Scholar] [CrossRef] [PubMed]
- Call, J.W.; Wang, Y.; Montoya, D.; Scherzer, N.J.; Heinrich, M.C. Survival in advanced GIST has improved over time and correlates with increased access to post-imatinib tyrosine kinase inhibitors: Results from Life Raft Group Registry. Clin. Sarcoma Res. 2019, 9, 4. [Google Scholar] [CrossRef]
- Simonsen, C.; de Heer, P.; Bjerre, E.D.; Suetta, C.; Hojman, P.; Pedersen, B.K.; Svendsen, L.B.; Christensen, J.F. Sarcopenia and Postoperative Complication Risk in Gastrointestinal Surgical Oncology: A Meta-analysis. Ann. Surg. 2018, 268, 58–69. [Google Scholar] [CrossRef]
- Moryoussef, F.; Dhooge, M.; Volet, J.; Barbe, C.; Brezault, C.; Hoeffel, C.; Coriat, R.; Bouche, O. Reversible sarcopenia in patients with gastrointestinal stromal tumor treated with imatinib. J. Cachexia Sarcopenia Muscle 2015, 6, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Shirao, K.; Nishida, T.; Doi, T.; Komatsu, Y.; Muro, K.; Li, Y.; Ueda, E.; Ohtsu, A. Phase I/II study of sunitinib malate in Japanese patients with gastrointestinal stromal tumor after failure of prior treatment with imatinib mesylate. Investig. New Drugs 2010, 28, 866–875. [Google Scholar] [CrossRef] [PubMed]
- George, S.; Reichardt, P.; Lechner, T.; Li, S.; Cohen, D.P.; Demetri, G.D. Hypertension as a potential biomarker of efficacy in patients with gastrointestinal stromal tumor treated with sunitinib. Ann. Oncol. 2012, 23, 3180–3187. [Google Scholar] [CrossRef] [PubMed]
- Donskov, F.; Michaelson, M.D.; Puzanov, I.; Davis, M.P.; Bjarnason, G.A.; Motzer, R.J.; Goldstein, D.; Lin, X.; Cohen, D.P.; Wiltshire, R.; et al. Sunitinib-associated hypertension and neutropenia as efficacy biomarkers in metastatic renal cell carcinoma patients. Br. J. Cancer 2015, 113, 1571–1580. [Google Scholar] [CrossRef] [PubMed]
- Kucharz, J.; Budnik, M.; Dumnicka, P.; Pastuszczak, M.; Kusnierz-Cabala, B.; Demkow, T.; Popko, K.; Wiechno, P. Hand-Foot Syndrome and Progression-Free Survival in Patients Treated with Sunitinib for Metastatic Clear Cell Renal Cell Carcinoma. Adv. Exp. Med. Biol. 2019, 1133, 35–40. [Google Scholar]
- Poprach, A.; Pavlik, T.; Melichar, B.; Puzanov, I.; Dusek, L.; Bortlicek, Z.; Vyzula, R.; Abrahamova, J.; Buchler, T.; Czech Renal Cancer Cooperative, G. Skin toxicity and efficacy of sunitinib and sorafenib in metastatic renal cell carcinoma: A national registry-based study. Ann. Oncol. 2012, 23, 3137–3143. [Google Scholar] [CrossRef] [PubMed]
- McLellan, B.; Ciardiello, F.; Lacouture, M.E.; Segaert, S.; Van Cutsem, E. Regorafenib-associated hand-foot skin reaction: Practical advice on diagnosis, prevention, and management. Ann. Oncol. 2015, 26, 2017–2026. [Google Scholar] [CrossRef]
- Luo, P.; Yan, H.; Chen, X.; Zhang, Y.; Zhao, Z.; Cao, J.; Zhu, Y.; Du, J.; Xu, Z.; Zhang, X.; et al. s-HBEGF/SIRT1 circuit-dictated crosstalk between vascular endothelial cells and keratinocytes mediates sorafenib-induced hand-foot skin reaction that can be reversed by nicotinamide. Cell Res. 2020, 30, 779–793. [Google Scholar] [CrossRef] [PubMed]
- Antonescu, C.R. The GIST paradigm: Lessons for other kinase-driven cancers. J. Pathol. 2011, 223, 251–261. [Google Scholar] [CrossRef] [PubMed]
- Antonescu, C.R.; Besmer, P.; Guo, T.; Arkun, K.; Hom, G.; Koryotowski, B.; Leversha, M.A.; Jeffrey, P.D.; Desantis, D.; Singer, S.; et al. Acquired resistance to imatinib in gastrointestinal stromal tumor occurs through secondary gene mutation. Clin. Cancer Res. 2005, 11, 4182–4190. [Google Scholar] [CrossRef]
- Heinrich, M.C.; Maki, R.G.; Corless, C.L.; Antonescu, C.R.; Harlow, A.; Griffith, D.; Town, A.; McKinley, A.; Ou, W.B.; Fletcher, J.A.; et al. Primary and secondary kinase genotypes correlate with the biological and clinical activity of sunitinib in imatinib-resistant gastrointestinal stromal tumor. J. Clin. Oncol. 2008, 26, 5352–5359. [Google Scholar] [CrossRef] [PubMed]
- Rutkowski, P.; Bylina, E.; Klimczak, A.; Switaj, T.; Falkowski, S.; Kroc, J.; Lugowska, I.; Brzeskwiniewicz, M.; Melerowicz, W.; Osuch, C.; et al. The outcome and predictive factors of sunitinib therapy in advanced gastrointestinal stromal tumors (GIST) after imatinib failure—One institution study. BMC Cancer 2012, 12, 107. [Google Scholar] [CrossRef]
- Nishida, T.; Takahashi, T.; Nishitani, A.; Doi, T.; Shirao, K.; Komatsu, Y.; Nakajima, K.; Hirota, S.; Japanese Study Group on GIST. Sunitinib-resistant gastrointestinal stromal tumors harbor cis-mutations in the activation loop of the KIT gene. Int. J. Clin. Oncol. 2009, 14, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Liegl, B.; Kepten, I.; Le, C.; Zhu, M.; Demetri, G.D.; Heinrich, M.C.; Fletcher, C.D.; Corless, C.L.; Fletcher, J.A. Heterogeneity of kinase inhibitor resistance mechanisms in GIST. J. Pathol. 2008, 216, 64–74. [Google Scholar] [CrossRef] [PubMed]

| Variables | No. | Percentage (%) or Mean ± SD |
|---|---|---|
| Basic data | ||
| Gender | ||
| Male/Female | 63/46 | 57.8/42.2 |
| Age (years) | 60.9 ± 13.6 | |
| ECOG when start | ||
| 0/1/2 | 24/47/22 | 22.0/43.1/20.2 |
| 3 | 16 | 14.7 |
| Body composition | ||
| Weight (kg) | 61.0 ± 12.6 | |
| Height (cm) | 160.0 ± 8.5 | |
| BMI (kg/m2) | 23.7 ± 4.0 | |
| BMI grading (kg/m2) | ||
| <18.5 | 8 | 7.3 |
| 18.5–27 | 83 | 76.2 |
| >27 | 18 | 16.5 |
| Albumin > 3.5 (g/dL) | ||
| Yes | 65 | 40.4 |
| No | 44 | 59.6 |
| Tumor characteristics | ||
| Tumor size (cm) | 10.4 ± 6.0 | |
| Location | ||
| Stomach | 39 | 35.8 |
| Small bowel | 53 | 48.7 |
| Colorectal | 8 | 7.3 |
| Peritoneum | 1 | 0.9 |
| Other | 8 | 7.3 |
| Liver Metastasis | ||
| Yes/No | 70/39 | 64.2/35.8 |
| Genetic mutation when using sunitinib (N = 109) | ||
| Exon 9 | 15 | 13.8 |
| Exon 9 and 17 | 2 | 1.8 |
| Exon11 | 36 | 33.0 |
| Exon 11 and 13 | 14 | 12.8 |
| Exon 11 and 17 | 8 | 7.3 |
| Wild type | 5 | 4.6 |
| Unknown | 29 | 26.6 |
| Sunitinib dosage | ||
| Dosage divided b | ||
| Yes/No | 70/39 | 64.2/35.8 |
| Initial dosage (mg) | ||
| 25 | 17 | 15.6 |
| 37.5 | 79 | 72.5 |
| 50 | 13 | 11.9 |
| Directly shift to sunitinib c | ||
| Yes/No | 49/60 | 45.0/55.0 |
| Predictor Variables | Median Survival (m) (95% CI) | 1-Year PFS (%) | 3-Year PFS (%) | p Value |
|---|---|---|---|---|
| Age (years) | 0.692 | |||
| ≤61 (n = 56) | 9.5 (5.5–13.5) | 44.1 | 25.3 | |
| >61 (n = 53) | 10.2 (6.4–14.0) | 43.5 | 16.0 | |
| Gender | 0.024 | |||
| Male (n = 63) | 12.9 (3.3–22.5) | 52.4 | 29.6 | |
| Female (n = 46) | 8.3 (5.8–10.8) | 32.3 | 11.5 | |
| Body mass index | 0.001 | |||
| <18.5 (n = 8) | 3.2 (2.5–4.0) | 0 | 0 | |
| 18.5–27 (n = 83) | 11.4 (6.5–16.3) | 46.7 | 22.3 | |
| >27 (n = 18) | 11.3 (7.5–15.1) | 50.0 | 26.7 | |
| Sarcopenia | 0.005 | |||
| Yes (n = 25) | 4.6 (3.3–6.0) | 16.8 | 4.6 | |
| No (n = 84) | 13.1 (6.3–19.9) | 51.6 | 13.1 | |
| Lymphocyte count | 0.008 | |||
| ≤858 (n = 29) | 6.2 (3.3–9.2) | 20.7 | 10.3 | |
| >858 (n = 80) | 12.9 (4.5–21.3) | 52.5 | 25.6 | |
| Neutrophil/lymphocyte ratio | 0.122 | |||
| ≤2.14 (n = 32) | 14.3 (6.4–22.2) | 58.6 | 27.4 | |
| >2.14 (n = 61) | 7.2 (3.8–10.5) | 34.4 | 16.8 | |
| Monocyte/lymphocyte ratio | 0.106 | |||
| ≤0.19 (n = 33) | 12.0 (3.2–20.9) | 53.1 | 34.0 | |
| >0.19 (n = 60) | 7.4 (5.1–9.7) | 35.6 | 13.7 | |
| Platelet/lymphocyte ratio | 0.009 | |||
| ≤270 (n = 75) | 13.8 (7.1–20.7) | 53.4 | 25.9 | |
| >270 (n = 34) | 6.2 (2.5–9.9) | 23.5 | 11.8 | |
| ECOG | 0.017 | |||
| 0 (n = 24) | 24.6 (5.2–44.0) | 62.5 | 30.8 | |
| 1/2 (n = 69) | 9.0 (57.3–12.6) | 42.8 | 20.9 | |
| 3 (n = 16) | 3.0 (51.8–4.2) | 16.7 | 8.4 | |
| Albumin (g/dL) | 0.343 | |||
| ≤3.5 (n = 44) | 5.6 (52.2–8.9) | 36.7 | 19.9 | |
| >3.5 (n = 65) | 11.7 (58.2–15.3) | 48.7 | 22.8 | |
| Direct to Sunitinib | 0.223 | |||
| No (n = 49) | 8.3 (56.1–10.5) | 33.4 | 13.4 | |
| Yes (n = 60) | 12.9 (55.1–20.7) | 51.6 | 27.4 | |
| Sunitinib dose (mg) | 0.029 | |||
| 25 (n = 17) | 6.5 (1.3–11.7) | 35.3 | N/A | |
| 37.5 (n = 79) | 10.2 (6.3–14.0) | 43.5 | 20.3 | |
| 50 (n = 13) | 19.1 (-) | 56.4 | 47.0 | |
| Primary site | 0.658 | |||
| Stomach (n = 39) | 11.3 (8.3–14.3) | 50.2 | 23.2 | |
| Small bowel (n = 53) | 10.2 (4.7–15.6) | 44.7 | 21.6 | |
| Colorectum (n = 8) | 14.3 (0.1–28.7) | 62.5 | 23.4 | |
| Others (n = 9) | 8.3 (6.9–9.6) | 33.3 | 11.1 | |
| Metastatic site | 0.005 | |||
| Non-liver (n = 39) | 22.6 (14.4–30.8) | 70.6 | 34.1 | |
| Liver (n = 70) | 7.0 (3.4–10.5) | 29.1 | 14.5 | |
| Genetic status (Secondary mutation) | 0.232 | |||
| Exon 13 (n = 14) | 23.3 (9.0–37.5) | 69.6 | 31.3 | |
| Exon 17 (n = 10) | 8.3 (0.4–16.2) | 50.0 | 0.0 | |
| Hypertension | 0.001 | |||
| No (n = 81) | 8.3 (5.3–11.2) | 35.7 | 12.4 | |
| Yes (n = 28) | 28.3 (17.9–38.7) | 67.1 | 44.7 | |
| Hand–foot syndrome | <0.0001 | |||
| No (n = 66) | 5.6 (2.4–8.7) | 29.5 | 13.1 | |
| Yes (n = 43) | 19.7 (12.6–26.7) | 65.0 | 33.5 | |
| Diarrhea | 0.021 | |||
| No (n = 67) | 7.4 (3.5–11.4) | 33.4 | 15.1 | |
| Yes (n = 42) | 19.7 (7.3–32.0) | 59.5 | 30.6 | |
| Fatigue | 0.141 | |||
| No (n = 72) | 11.4 (7.0–15.9) | 47.4 | 25.5 | |
| Yes (n = 37) | 9.4 (2.5–16.3) | 36.9 | 14.2 | |
| Anemia | 0.548 | |||
| No (n = 39) | 11.4 (8.3–14.5) | 46.2 | 17.9 | |
| Yes (n = 70) | 9.0 (5.1–12.9) | 42.7 | 23.8 | |
| Thrombocytopenia | 0.268 | |||
| No (n = 82) | 9.4 (7.1–11.7) | 41.0 | 19.2 | |
| Yes (n = 27) | 13.8 (6.3–21.4) | 52.8 | 28.8 | |
| Leukopenia | 0.726 | |||
| No (n = 80) | 9.0 (5.7–12.3) | 42.7 | 22.1 | |
| Yes (n = 29) | 11.6 (7.2–16.0) | 46.7 | 19.4 | |
| Anorexia | 0.162 | |||
| No (n = 83) | 11.3 (7.0–15.6) | 47.1 | 24.4 | |
| Yes (n = 26) | 9.4 (3.7–15.1) | 32.8 | 12.3 | |
| Edema | 0.053 | |||
| No (n = 90) | 10.2 (6.2–14.1) | 47.6 | 24.5 | |
| Yes (n = 19) | 4.6 (3.2–6.1) | 24.6 | 6.1 | |
| Hepatic toxicity | 0.559 | |||
| No (n = 94) | 9.5 (6.2–12.8) | 42.3 | 21.3 | |
| Yes (n = 18) | 16.3 (0.1–35.1) | 53.3 | 22.9 | |
| Hypothyroid | 0.152 | |||
| No (n = 104) | 9.5 (6.7–12.3) | 42.0 | 19.3 | |
| Yes (n = 5) | 39.2 (17.3–61.1) | 80.0 | 60.0 |
| Predictor Variables | Hazard Ratio (HR) | 95% CI of HR | p Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Gender | ||||
| Male | 1 | |||
| Female | 2.100 | 1.270 | 3.470 | 0.004 |
| ECOG | ||||
| 0 | 1 | |||
| 1/2 | 1.168 | 0.649 | 2.101 | 0.604 |
| 3 | 2.922 | 1.363 | 6.265 | 0.006 |
| Platelet/lymphocyte ratio | ||||
| ≤270 | 1 | |||
| >270 | 1.687 | 1.051 | 2.710 | 0.030 |
| Sarcopenia | ||||
| Yes | 2.333 | 1.251 | 4.349 | 0.008 |
| No | 1 | |||
| Metastatic site | ||||
| Non-liver | 1 | |||
| Liver | 2.241 | 1.369 | 3.671 | 0.001 |
| Sunitinib dose (mg) | ||||
| 25 | 2.205 | 0.809 | 6.008 | 0.122 |
| 37.5 | 2.437 | 1.011 | 5.872 | 0.047 |
| 50 | 1 | |||
| Hypertension | ||||
| No | 2.361 | 1.331 | 4.186 | 0.003 |
| Yes | 1 | |||
| Hand–foot syndrome | ||||
| No | 2.995 | 1.835 | 4.888 | <0.0001 |
| Yes | 1 | |||
| Predictor Variables | Points Assigned | Total Point Score | Probability of 1-Year PFS |
| 476 | 0.01 | ||
| Gender | 437 | 0.05 | |
| 413 | 0.10 | ||
| Male | 0 | 381 | 0.20 |
| Female | 68 | 354 | 0.30 |
| ECOG | 329 | 0.40 | |
| 304 | 0.50 | ||
| 0 | 0 | 276 | 0.60 |
| 1/2 | 14 | 243 | 0.70 |
| 3 | 98 | 200 | 0.80 |
| Platelet/lymphocyte ratio | 132 | 0.90 | |
| 66 | 0.95 | ||
| ≤270 | 0 | Total point score | Probability of 2-year PFS |
| >270 | 48 | 424 | 0.01 |
| Sarcopenia | 385 | 0.05 | |
| 361 | 0.10 | ||
| Yes | 77 | 328 | 0.20 |
| No | 0 | 301 | 0.30 |
| Metastatic site | 277 | 0.40 | |
| 251 | 0.50 | ||
| Non-liver | 0 | 223 | 0.60 |
| Liver | 74 | 191 | 0.70 |
| Sunitinib dose (mg) | 148 | 0.80 | |
| 79 | 0.90 | ||
| 25 | 72 | 14 | 0.95 |
| 37.5 | 81 | Total point score | Probability of 3-year PFS |
| 50 | 0 | 387 | 0.01 |
| Hypertension | 348 | 0.05 | |
| 324 | 0.10 | ||
| No | 78 | 292 | 0.20 |
| Yes | 0 | 265 | 0.30 |
| Hand–foot syndrome | 240 | 0.40 | |
| 215 | 0.50 | ||
| No | 100 | 187 | 0.60 |
| Yes | 0 | 154 | 0.70 |
| 112 | 0.80 | ||
| 43 | 0.90 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, Y.-R.; Huang, W.-K.; Wang, S.-Y.; Wu, C.-E.; Chen, J.-S.; Yeh, C.-N. A Nomogram Predicting Progression Free Survival in Patients with Gastrointestinal Stromal Tumor Receiving Sunitinib: Incorporating Pre-Treatment and Post-Treatment Parameters. Cancers 2021, 13, 2587. https://doi.org/10.3390/cancers13112587
Chang Y-R, Huang W-K, Wang S-Y, Wu C-E, Chen J-S, Yeh C-N. A Nomogram Predicting Progression Free Survival in Patients with Gastrointestinal Stromal Tumor Receiving Sunitinib: Incorporating Pre-Treatment and Post-Treatment Parameters. Cancers. 2021; 13(11):2587. https://doi.org/10.3390/cancers13112587
Chicago/Turabian StyleChang, Yau-Ren, Wen-Kuan Huang, Shang-Yu Wang, Chiao-En Wu, Jen-Shi Chen, and Chun-Nan Yeh. 2021. "A Nomogram Predicting Progression Free Survival in Patients with Gastrointestinal Stromal Tumor Receiving Sunitinib: Incorporating Pre-Treatment and Post-Treatment Parameters" Cancers 13, no. 11: 2587. https://doi.org/10.3390/cancers13112587
APA StyleChang, Y.-R., Huang, W.-K., Wang, S.-Y., Wu, C.-E., Chen, J.-S., & Yeh, C.-N. (2021). A Nomogram Predicting Progression Free Survival in Patients with Gastrointestinal Stromal Tumor Receiving Sunitinib: Incorporating Pre-Treatment and Post-Treatment Parameters. Cancers, 13(11), 2587. https://doi.org/10.3390/cancers13112587







