Survival Following Relapse in Children with Acute Myeloid Leukemia: A Report from AML-BFM and COG
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Definitions and Cohorts
2.3. Statistical Analyses
3. Results
3.1. Patient Characteristics and Previous Treatment
3.2. Post-Relapse Therapy
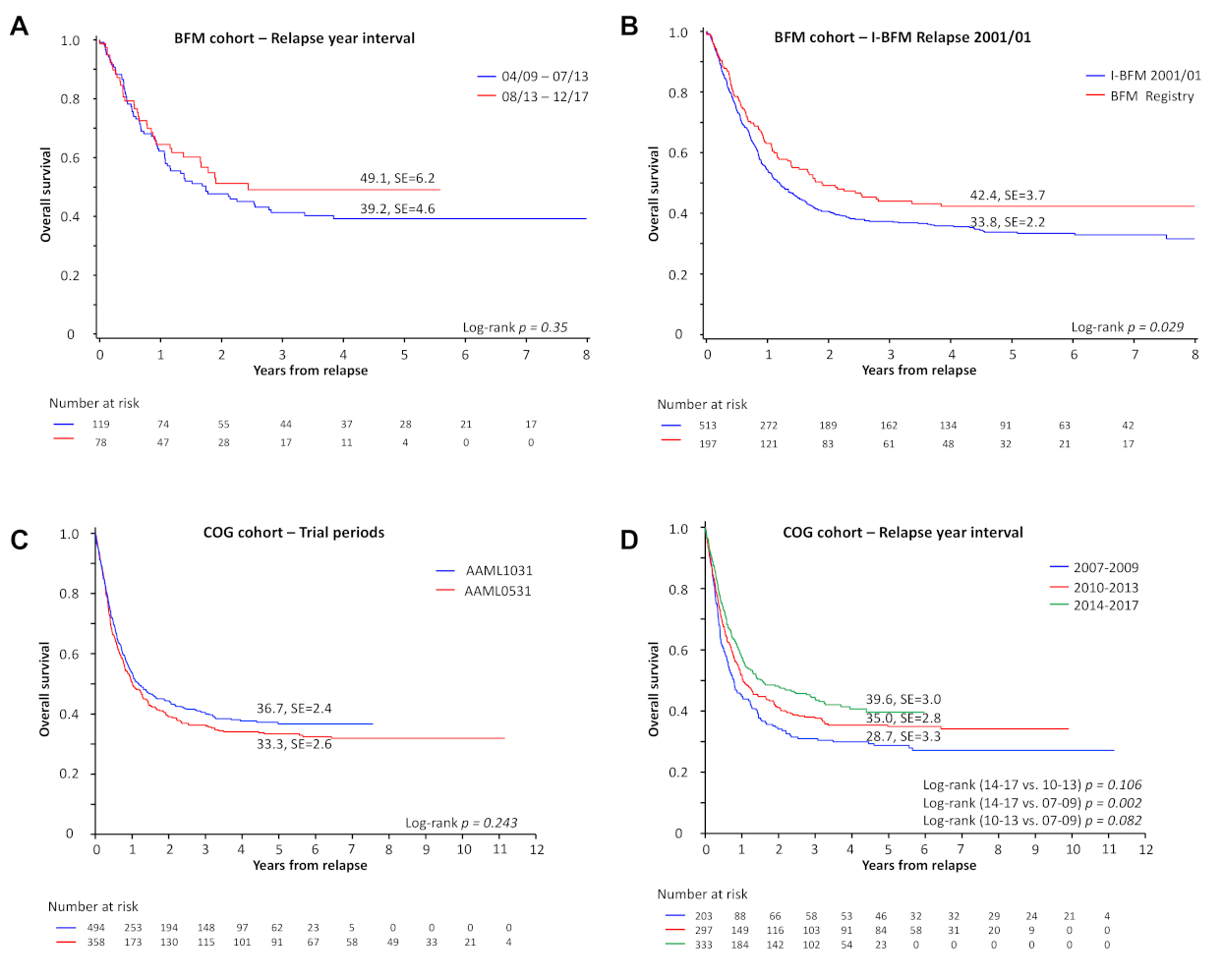
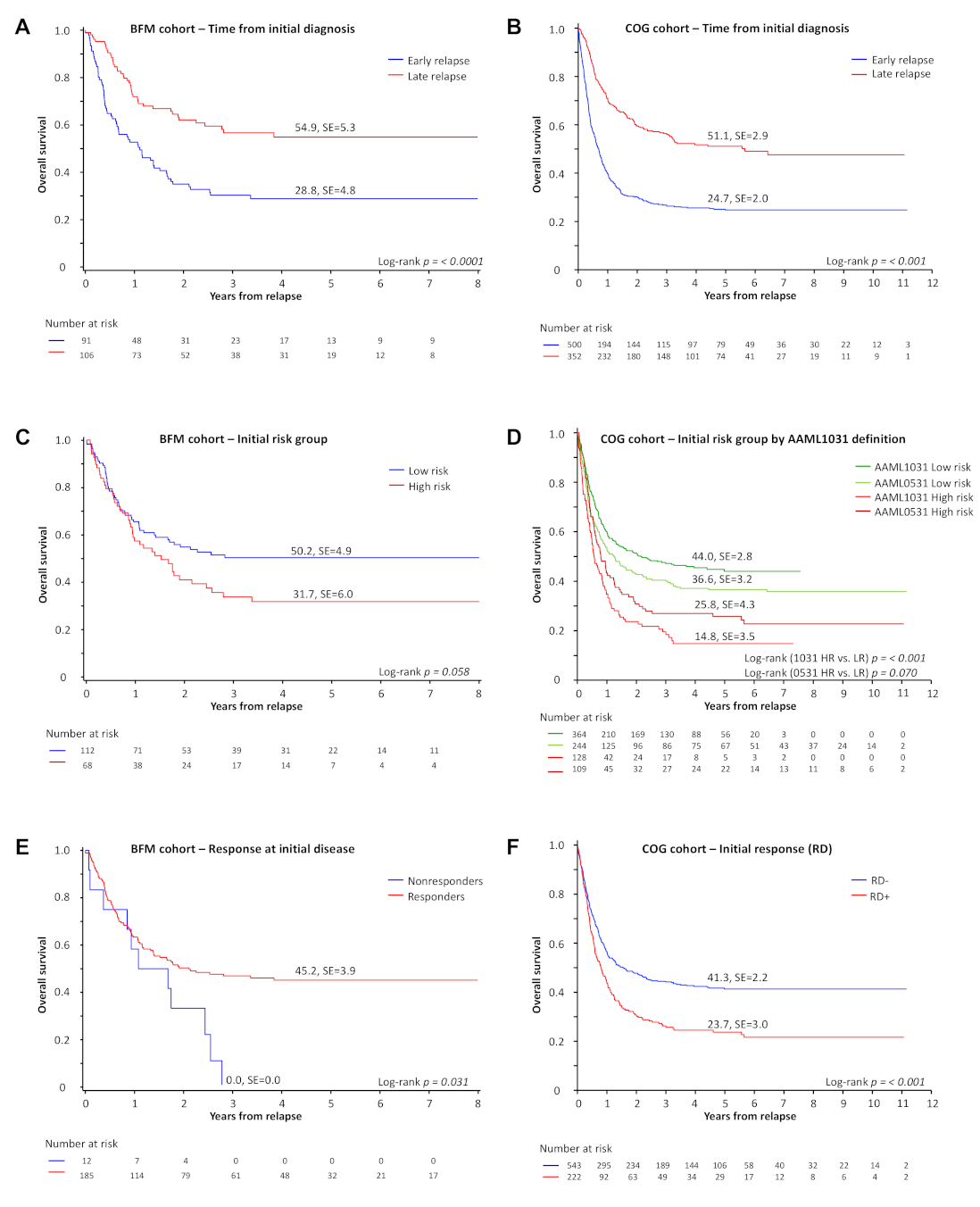
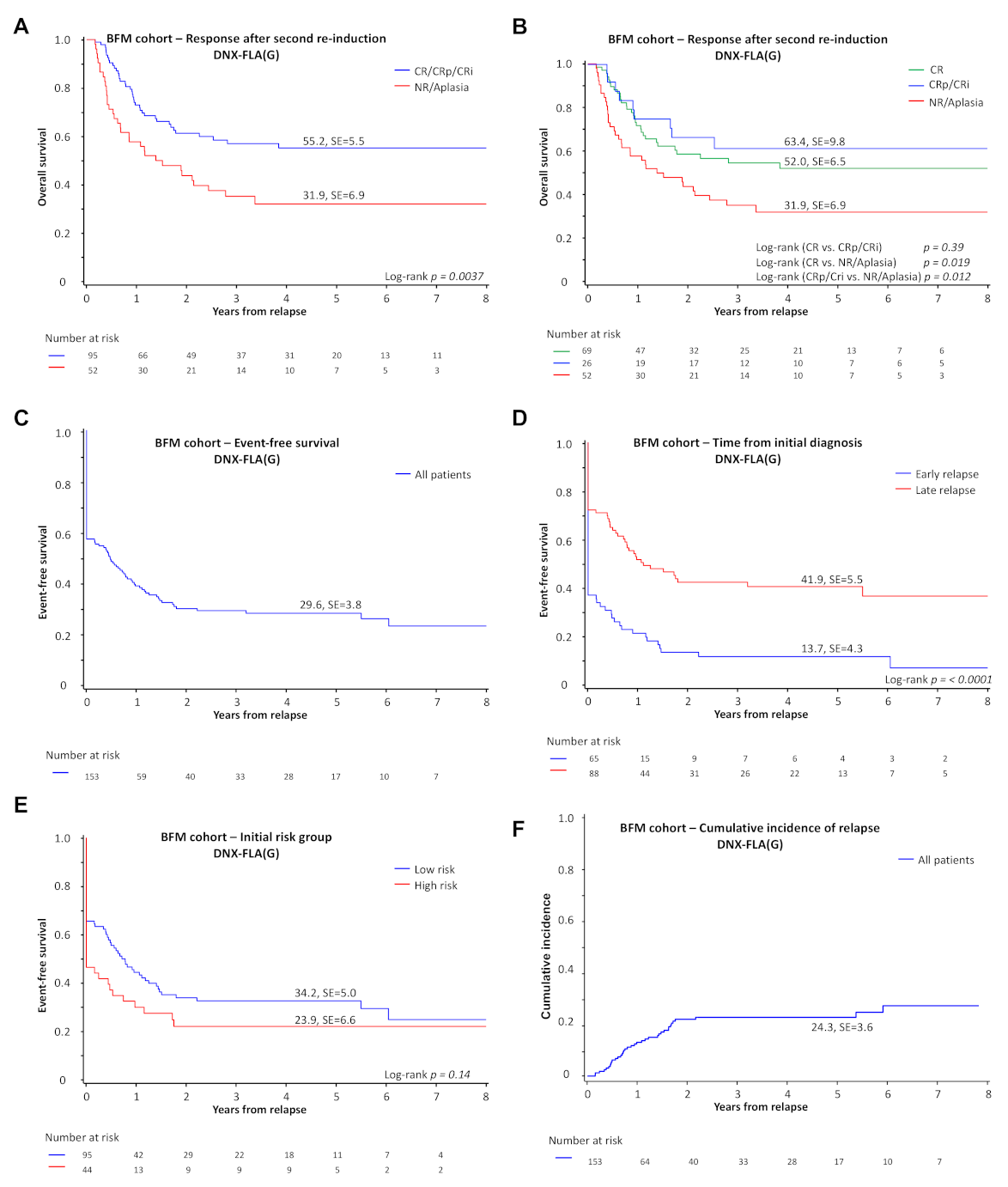
3.3. Survival and Prognostic Factors at First Relapse
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abrahamsson, J.; Forestier, E.; Heldrup, J.; Jahnukainen, K.; Jonsson, O.G.; Lausen, B.; Palle, J.; Zeller, B.; Hasle, H. Response-guided induction therapy in pediatric acute myeloid leukemia with excellent remission rate. J. Clin. Oncol. 2011, 29, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Gibson, B.E.; Wheatley, K.; Hann, I.M.; Stevens, R.F.; Webb, D.; Hills, R.K.; De Graaf, S.S.; Harrison, C.J. Treatment strategy and long-term results in paediatric patients treated in consecutive UK AML trials. Leukemia 2005, 19, 2130–2138. [Google Scholar] [CrossRef] [PubMed]
- Pession, A.; Masetti, R.; Rizzari, C.; Putti, M.C.; Casale, F.; Fagioli, F.; Luciani, M.; Lo Nigro, L.; Menna, G.; Micalizzi, C.; et al. Results of the AIEOP AML 2002/01 multicenter prospective trial for the treatment of children with acute myeloid leukemia. Blood 2013, 122, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Rubnitz, J.E.; Inaba, H.; Dahl, G.; Ribeiro, R.C.; Bowman, W.P.; Taub, J.; Pounds, S.; Razzouk, B.I.; Lacayo, N.J.; Cao, X.; et al. Minimal residual disease-directed therapy for childhood acute myeloid leukaemia: Results of the AML02 multicentre trial. Lancet Oncol. 2010, 11, 543–552. [Google Scholar] [CrossRef]
- Rasche, M.; Zimmermann, M.; Borschel, L.; Bourquin, J.P.; Dworzak, M.; Klingebiel, T.; Lehrnbecher, T.; Creutzig, U.; Klusmann, J.H.; Reinhardt, D. Successes and challenges in the treatment of pediatric acute myeloid leukemia: A retrospective analysis of the AML-BFM trials from 1987 to 2012. Leukemia 2018, 32, 2167–2177. [Google Scholar] [CrossRef]
- Aplenc, R.; Meshinchi, S.; Sung, L.; Alonzo, T.; Choi, J.; Fisher, B.; Gerbing, R.; Hirsch, B.; Horton, T.; Khawash, S.; et al. Bortezomib with standard chemotherapy for children with acute myeloid leukemia does not improve treatment outcomes: A report from the Children’s Oncology Group. Haematologica 2020. [Google Scholar] [CrossRef]
- Zwaan, C.M.; Kolb, E.A.; Reinhardt, D.; Abrahamsson, J.; Adachi, S.; Aplenc, R.; De Bont, E.S.; De Moerloose, B.; Dworzak, M.; Gibson, B.E.; et al. Collaborative Efforts Driving Progress in Pediatric Acute Myeloid Leukemia. J. Clin. Oncol. 2015, 33, 2949–2962. [Google Scholar] [CrossRef]
- Creutzig, U.; van den Heuvel-Eibrink, M.M.; Gibson, B.; Dworzak, M.N.; Adachi, S.; de Bont, E.; Harbott, J.; Hasle, H.; Johnston, D.; Kinoshita, A.; et al. Diagnosis and management of acute myeloid leukemia in children and adolescents: Recommendations from an international expert panel. Blood 2012, 120, 3187–3205. [Google Scholar] [CrossRef]
- Kaspers, G.J.; Zimmermann, M.; Reinhardt, D.; Gibson, B.E.; Tamminga, R.Y.; Aleinikova, O.; Armendariz, H.; Dworzak, M.; Ha, S.Y.; Hasle, H.; et al. Improved outcome in pediatric relapsed acute myeloid leukemia: Results of a randomized trial on liposomal daunorubicin by the International BFM Study Group. J. Clin. Oncol. 2013, 31, 599–607. [Google Scholar] [CrossRef]
- Sander, A.; Zimmermann, M.; Dworzak, M.; Fleischhack, G.; von Neuhoff, C.; Reinhardt, D.; Kaspers, G.J.; Creutzig, U. Consequent and intensified relapse therapy improved survival in pediatric AML: Results of relapse treatment in 379 patients of three consecutive AML-BFM trials. Leukemia 2010, 24, 1422–1428. [Google Scholar] [CrossRef]
- Rubnitz, J.E.; Razzouk, B.I.; Lensing, S.; Pounds, S.; Pui, C.H.; Ribeiro, R.C. Prognostic factors and outcome of recurrence in childhood acute myeloid leukemia. Cancer 2007, 109, 157–163. [Google Scholar] [CrossRef]
- Stahnke, K.; Boos, J.; Bender-Gotze, C.; Ritter, J.; Zimmermann, M.; Creutzig, U. Duration of first remission predicts remission rates and long-term survival in children with relapsed acute myelogenous leukemia. Leukemia 1998, 12, 1534–1538. [Google Scholar] [CrossRef]
- Webb, D.K.; Wheatley, K.; Harrison, G.; Stevens, R.F.; Hann, I.M. Outcome for children with relapsed acute myeloid leukaemia following initial therapy in the Medical Research Council (MRC) AML 10 trial. MRC Childhood Leukaemia Working Party. Leukemia 1999, 13, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, H.; Tabuchi, K.; Tawa, A.; Tsukimoto, I.; Tsuchida, M.; Morimoto, A.; Yabe, H.; Horibe, K.; Hanada, R.; Imaizumi, M.; et al. Outcome of children with relapsed acute myeloid leukemia following initial therapy under the AML99 protocol. Int. J. Hematol. 2014, 100, 171–179. [Google Scholar] [CrossRef]
- Karlsson, L.; Forestier, E.; Hasle, H.; Jahnukainen, K.; Jonsson, O.G.; Lausen, B.; Noren Nystrom, U.; Palle, J.; Tierens, A.; Zeller, B.; et al. Outcome after intensive reinduction therapy and allogeneic stem cell transplant in paediatric relapsed acute myeloid leukaemia. Br. J. Haematol. 2017, 178, 592–602. [Google Scholar] [CrossRef]
- Hoffman, A.E.; Schoonmade, L.J.; Kaspers, G.J. Pediatric relapsed acute myeloid leukemia: A systematic review. Expert Rev. Anticancer Ther. 2020, 21, 45–52. [Google Scholar] [CrossRef]
- Creutzig, U.; Zimmermann, M.; Dworzak, M.N.; Gibson, B.; Tamminga, R.; Abrahamsson, J.; Ha, S.Y.; Hasle, H.; Maschan, A.; Bertrand, Y.; et al. The prognostic significance of early treatment response in pediatric relapsed acute myeloid leukemia: Results of the international study Relapsed AML 2001/01. Haematologica 2014, 99, 1472–1478. [Google Scholar] [CrossRef]
- Goemans, B.F.; Tamminga, R.Y.; Corbijn, C.M.; Hahlen, K.; Kaspers, G.J. Outcome for children with relapsed acute myeloid leukemia in the Netherlands following initial treatment between 1980 and 1998: Survival after chemotherapy only? Haematologica 2008, 93, 1418–1420. [Google Scholar] [CrossRef]
- Abrahamsson, J.; Clausen, N.; Gustafsson, G.; Hovi, L.; Jonmundsson, G.; Zeller, B.; Forestier, E.; Heldrup, J.; Hasle, H.; Nordic Society for Paediatric Haematology and Oncology (NOPHO); et al. Improved outcome after relapse in children with acute myeloid leukaemia. Br. J. Haematol. 2007, 136, 229–236. [Google Scholar] [CrossRef]
- Wells, R.J.; Adams, M.T.; Alonzo, T.A.; Arceci, R.J.; Buckley, J.; Buxton, A.B.; Dusenbery, K.; Gamis, A.; Masterson, M.; Vik, T.; et al. Mitoxantrone and cytarabine induction, high-dose cytarabine, and etoposide intensification for pediatric patients with relapsed or refractory acute myeloid leukemia: Children’s Cancer Group Study 2951. J. Clin. Oncol. 2003, 21, 2940–2947. [Google Scholar] [CrossRef]
- Aladjidi, N.; Auvrignon, A.; Leblanc, T.; Perel, Y.; Benard, A.; Bordigoni, P.; Gandemer, V.; Thuret, I.; Dalle, J.H.; Piguet, C.; et al. Outcome in children with relapsed acute myeloid leukemia after initial treatment with the French Leucemie Aique Myeloide Enfant (LAME) 89/91 protocol of the French Society of Pediatric Hematology and Immunology. J. Clin. Oncol. 2003, 21, 4377–4385. [Google Scholar] [CrossRef] [PubMed]
- Gamis, A.S.; Alonzo, T.A.; Meshinchi, S.; Sung, L.; Gerbing, R.B.; Raimondi, S.C.; Hirsch, B.A.; Kahwash, S.B.; Heerema-McKenney, A.; Winter, L.; et al. Gemtuzumab ozogamicin in children and adolescents with de novo acute myeloid leukemia improves event-free survival by reducing relapse risk: Results from the randomized phase III Children’s Oncology Group trial AAML0531. J. Clin. Oncol. 2014, 32, 3021–3032. [Google Scholar] [CrossRef] [PubMed]
- Loken, M.R.; Alonzo, T.A.; Pardo, L.; Gerbing, R.B.; Raimondi, S.C.; Hirsch, B.A.; Ho, P.A.; Franklin, J.; Cooper, T.M.; Gamis, A.S.; et al. Residual disease detected by multidimensional flow cytometry signifies high relapse risk in patients with de novo acute myeloid leukemia: A report from Children’s Oncology Group. Blood 2012, 120, 1581–1588. [Google Scholar] [CrossRef]
- Brodersen, L.E.; Gerbing, R.B.; Pardo, M.L.; Alonzo, T.A.; Paine, D.; Fritschle, W.; Hsu, F.C.; Pollard, J.A.; Aplenc, R.; Kahwash, S.B.; et al. Morphologic remission status is limited compared to DeltaN flow cytometry: A Children’s Oncology Group AAML0531 report. Blood Adv. 2020, 4, 5050–5061. [Google Scholar] [CrossRef]
- Cheson, B.D.; Cassileth, P.A.; Head, D.R.; Schiffer, C.A.; Bennett, J.M.; Bloomfield, C.D.; Brunning, R.; Gale, R.P.; Grever, M.R.; Keating, M.J.; et al. Report of the National Cancer Institute-sponsored workshop on definitions of diagnosis and response in acute myeloid leukemia. J. Clin. Oncol. 1990, 8, 813–819. [Google Scholar] [CrossRef]
- Cheson, B.D.; Bennett, J.M.; Kopecky, K.J.; Buchner, T.; Willman, C.L.; Estey, E.H.; Schiffer, C.A.; Doehner, H.; Tallman, M.S.; Lister, T.A.; et al. Revised recommendations of the International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia. J. Clin. Oncol. 2003, 21, 4642–4649. [Google Scholar] [CrossRef]
- Kaspers, G.J.; Creutzig, U. Pediatric acute myeloid leukemia: International progress and future directions. Leukemia 2005, 19, 2025–2029. [Google Scholar] [CrossRef]
- Creutzig, U.; Zimmermann, M.; Ritter, J.; Reinhardt, D.; Hermann, J.; Henze, G.; Jurgens, H.; Kabisch, H.; Reiter, A.; Riehm, H.; et al. Treatment strategies and long-term results in paediatric patients treated in four consecutive AML-BFM trials. Leukemia 2005, 19, 2030–2042. [Google Scholar] [CrossRef]
- Chen, X.; Xie, H.; Wood, B.L.; Walter, R.B.; Pagel, J.M.; Becker, P.S.; Sandhu, V.K.; Abkowitz, J.L.; Appelbaum, F.R.; Estey, E.H. Relation of clinical response and minimal residual disease and their prognostic impact on outcome in acute myeloid leukemia. J. Clin. Oncol. 2015, 33, 1258–1264. [Google Scholar] [CrossRef]
- Walter, R.B.; Kantarjian, H.M.; Huang, X.; Pierce, S.A.; Sun, Z.; Gundacker, H.M.; Ravandi, F.; Faderl, S.H.; Tallman, M.S.; Appelbaum, F.R.; et al. Effect of complete remission and responses less than complete remission on survival in acute myeloid leukemia: A combined Eastern Cooperative Oncology Group, Southwest Oncology Group, and M. D. Anderson Cancer Center Study. J. Clin. Oncol. 2010, 28, 1766–1771. [Google Scholar] [CrossRef] [PubMed]
- Short, N.J.; Rafei, H.; Daver, N.; Hwang, H.; Ning, J.; Jorgensen, J.L.; Kadia, T.M.; DiNardo, C.D.; Wang, S.A.; Jabbour, E.; et al. Prognostic impact of complete remission with MRD negativity in patients with relapsed or refractory AML. Blood Adv. 2020, 4, 6117–6126. [Google Scholar] [CrossRef]
- Bloomfield, C.D.; Estey, E.; Pleyer, L.; Schuh, A.C.; Stein, E.M.; Tallman, M.S.; Wei, A. Time to repeal and replace response criteria for acute myeloid leukemia? Blood Rev. 2018, 32, 416–425. [Google Scholar] [CrossRef]
- Woods, W.G.; Kobrinsky, N.; Buckley, J.D.; Lee, J.W.; Sanders, J.; Neudorf, S.; Gold, S.; Barnard, D.R.; DeSwarte, J.; Dusenbery, K.; et al. Timed-sequential induction therapy improves postremission outcome in acute myeloid leukemia: A report from the Children’s Cancer Group. Blood 1996, 87, 4979–4989. [Google Scholar] [CrossRef]
| Patients (%) | ||
|---|---|---|
| First Relapse Treatment of Pediatric AML | n = 197 | |
| Chemotherapy | Re-Induction with DNX-FLA(G) +/−FLA (G) | 156 (81%) |
| Re-Induction with FLA(G) +/−FLA (G) | 5 (3%) | |
| Re-Induction with Ida-FLA +/− FLA | 3 (2%) | |
| Re-Induction with FLA + others +/− FLA | 3 (2%) | |
| Re-Induction with a Clofarabine-containing regimen | 8 (4%) | |
| Others (e.g., Gemtuzumab Ozagamicin, Sorafenib, intrathecal treatment only) | 10 (5%) | |
| Palliative care | 8 (4%) | |
| Unknown | 4 | |
| HSCT | No HSCT | 37 (19%) |
| HSCT | 157 (81%) | |
| 142 (90%) | |
| 15 (10%) | |
| Unknown | 3 | |
| First relapse response and HSCT after DNX-FLA +/−FLA | n = 156 | |
| HSCT | No HSCT | 20 (13%) |
| HSCT | 134 (87%) | |
| 123 (92%) | |
| 11 (8%) | |
| Unknown | 2 | |
| Response after 2 induction cycles | CR | 69 (45%) |
| CRp | 20 (13%) | |
| Cri | 6 (4%) | |
| Aplasia | 20 (13%) | |
| NR | 32 (21%) | |
| Early death before CR evaluation | 7 (5%) | |
| Unknown | 2 | |
| Early Treatment Response | Death before evaluable BM | 4 (3%) |
| BM after first induction not available or not applicable | 12 (8%) | |
| Evaluable BM after first induction | 140 (90%) | |
| 18 (13%) | |
| 122 (87%) | |
| BFM | COG | |||||||
|---|---|---|---|---|---|---|---|---|
| Criteria | pOS | pOS | ||||||
| n (all pts.) | HR | 95% CI | p (Chi) | n (all pts.) | HR | 95% CI | p (Chi) | |
| Univariable analysis | ||||||||
| Time from initial diagnosis <1 year | 91 (197) | 2.24 | 1.52–3.30 | <0.001 | 500 (852) | 2.31 | 1.92–2.79 | <0.001 |
| Age at relapse <2 years | 36 (197) | 1.00 | 0.53–1.87 | 0.998 | 116 (852) | 1.41 | 1.09–1.83 | 0.009 |
| Age at relapse 2–9 years | 67 (197) | 0.88 | 0.57–1.36 | 0.558 | 316 (852) | 0.93 | 0.76–1.14 | 0.497 |
| Age at relapse 10–13 years | 39 (197) | 0.68 | 0.36–1.27 | 0.228 | 124 (852) | 0.93 | 0.71–1.22 | 0.601 |
| Age at relapse >13 years | 55 (197) | 1 | 296 (852) | 1 | ||||
| inv(16)(p13.1q22) | 7 (190) | 0.83 | 0.26–2.62 | 0.751 | 72 (841) | 0.32 | 0.21–0.49 | <0.001 |
| t(8;21)(q22;q22.1) | 20 (192) | 0.62 | 0.30–1.27 | 0.188 | 71 (841) | 0.66 | 0.47–0.93 | 0.018 |
| Nonresponse at initial disease | 12 (197) | 2.04 | 1.39–2.99 | <0.001 | -- | -- | -- | -- |
| RD at EOI of initial disease | -- | -- | -- | -- | 222 (765) | 1.55 | 1.28–1.88 | <0.001 |
| High-risk group * | 68 (180) | 1.47 | 0.98–2.19 | 0.060 | 237 (845) | 1.57 | 1.33–1.85 | <0.001 |
| Poor response (> 20% leukemic blasts) after first re-induction | 18 (140) | 1.74 | 0.95–3.18 | 0.071 | -- | -- | -- | -- |
| Relapse year interval 2007–2009 | -- | -- | -- | -- | 203 (852) | 1.43 | 1.15–1.78 | 0.001 |
| Relapse year interval 2010–2013 † | 119 (197) | 1.21 | 0.81–1.81 | 0.350 | 297 (852) | 1.18 | 0.96–1.45 | 0.112 |
| Relapse year interval 2014–2017 ‡ | 78 (197) | 1 | 333 (852) | 1 | ||||
| Relapse year interval 2018–2019 | -- | -- | -- | -- | 19 (852) | 1.26 | 0.64–2.45 | 0.507 |
| Multivariable analysis | ||||||||
| Time from initial diagnosis < 1 year | 81 (177) | 1.95 | 1.23–3.09 | 0.005 | 493 (839) | 2.17 | 1.78–2.65 | <0.001 |
| Age at relapse < 2 years | 17 (177) | 0.52 | 0.24–1.12 | 0.095 | 114 (839) | 0.96 | 0.73–1.27 | 0.768 |
| Age at relapse 2–9 years | 68 (177) | 0.76 | 0.47–1.22 | 0.256 | 311 (839) | 0.79 | 0.64–0.98 | 0.029 |
| Age at relapse 10–13 years | 28 (177) | 0.67 | 0.35–1.28 | 0.223 | 122 (839) | 0.78 | 0.59–1.02 | 0.073 |
| Age at relapse >13 years | 64 (177) | 1 | 292 (839) | 1 | ||||
| inv(16)(p13.1q22) | 7 (177) | 1.26 | 0.37–4.24 | 0.713 | 72 (839) | 0.36 | 0.23–0.56 | <0.001 |
| t(8;21)(q22;q22.1) | 20 (177) | 0.96 | 0.44–2.11 | 0.922 | 71 (839) | 0.73 | 0.51–1.03 | 0.075 |
| Nonresponse at initial disease | 11 (177) | 1.80 | 1.18–2.76 | 0.006 | -- | -- | -- | -- |
| High-risk group * | 66 (177) | 1.51 | 0.97–2.33 | 0.065 | 237 (839) | 1.50 | 1.23–1.81 | <0.001 |
| Relapse year interval 2007–2009 | -- | -- | -- | -- | 200 (839) | 1.22 | 0.97–1.52 | 0.090 |
| Relapse year interval 2010–2013 † | 103 (177) | 1.13 | 0.73–1.74 | 0.586 | 294 (839) | 1.10 | 0.89–1.35 | 0.376 |
| Relapse year interval 2014–2017 ‡ | 74 (177) | 1 | 326 (839) | 1 | ||||
| Relapse year interval 2018–2019 | -- | -- | -- | -- | 19 (839) | 1.42 | 0.72–2.80 | 0.311 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rasche, M.; Zimmermann, M.; Steidel, E.; Alonzo, T.; Aplenc, R.; Bourquin, J.-P.; Boztug, H.; Cooper, T.; Gamis, A.S.; Gerbing, R.B.; et al. Survival Following Relapse in Children with Acute Myeloid Leukemia: A Report from AML-BFM and COG. Cancers 2021, 13, 2336. https://doi.org/10.3390/cancers13102336
Rasche M, Zimmermann M, Steidel E, Alonzo T, Aplenc R, Bourquin J-P, Boztug H, Cooper T, Gamis AS, Gerbing RB, et al. Survival Following Relapse in Children with Acute Myeloid Leukemia: A Report from AML-BFM and COG. Cancers. 2021; 13(10):2336. https://doi.org/10.3390/cancers13102336
Chicago/Turabian StyleRasche, Mareike, Martin Zimmermann, Emma Steidel, Todd Alonzo, Richard Aplenc, Jean-Pierre Bourquin, Heidrun Boztug, Todd Cooper, Alan S. Gamis, Robert B. Gerbing, and et al. 2021. "Survival Following Relapse in Children with Acute Myeloid Leukemia: A Report from AML-BFM and COG" Cancers 13, no. 10: 2336. https://doi.org/10.3390/cancers13102336
APA StyleRasche, M., Zimmermann, M., Steidel, E., Alonzo, T., Aplenc, R., Bourquin, J.-P., Boztug, H., Cooper, T., Gamis, A. S., Gerbing, R. B., Janotova, I., Klusmann, J.-H., Lehrnbecher, T., Mühlegger, N., Neuhoff, N. v., Niktoreh, N., Sramkova, L., Stary, J., Waack, K., ... Reinhardt, D. (2021). Survival Following Relapse in Children with Acute Myeloid Leukemia: A Report from AML-BFM and COG. Cancers, 13(10), 2336. https://doi.org/10.3390/cancers13102336







