ANGPT2 and NOS3 Polymorphisms and Clinical Outcome in Advanced Hepatocellular Carcinoma Patients Receiving Sorafenib
Abstract
1. Introduction
2. Results
2.1. Patient Characteristics and Clinical Variables
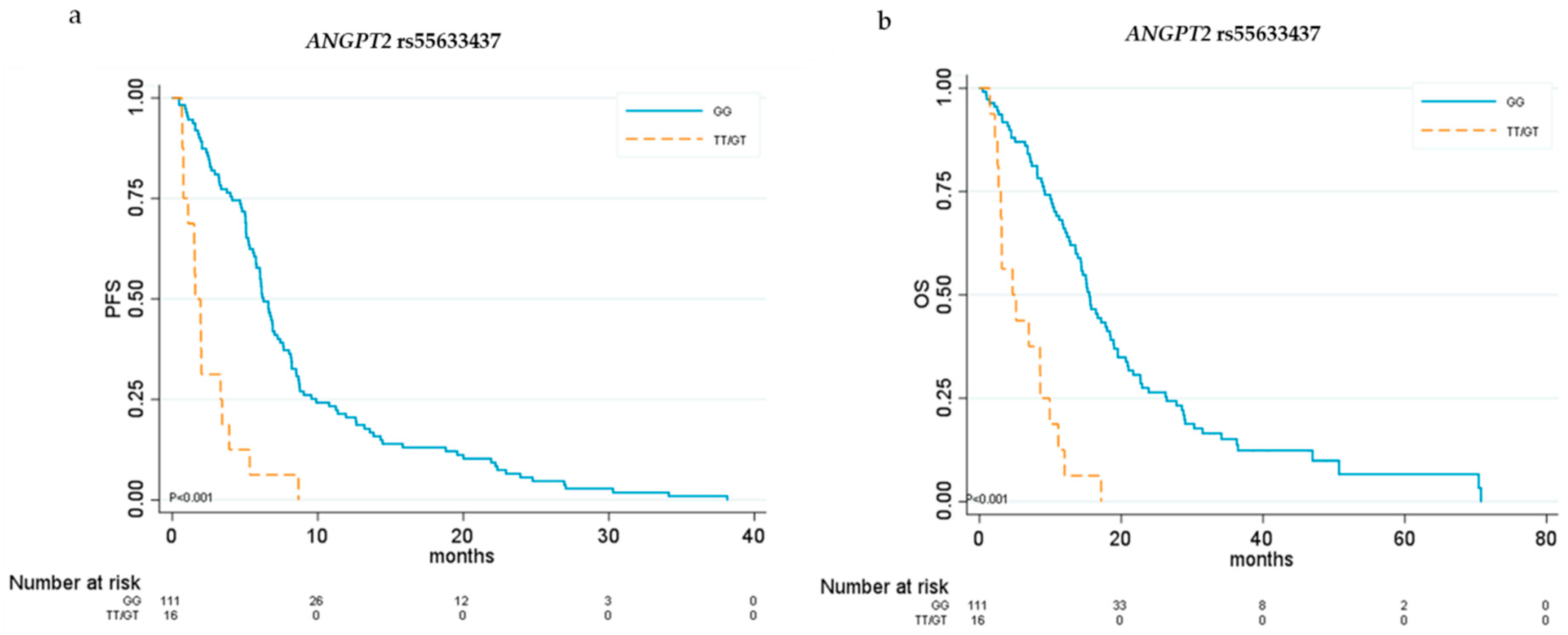
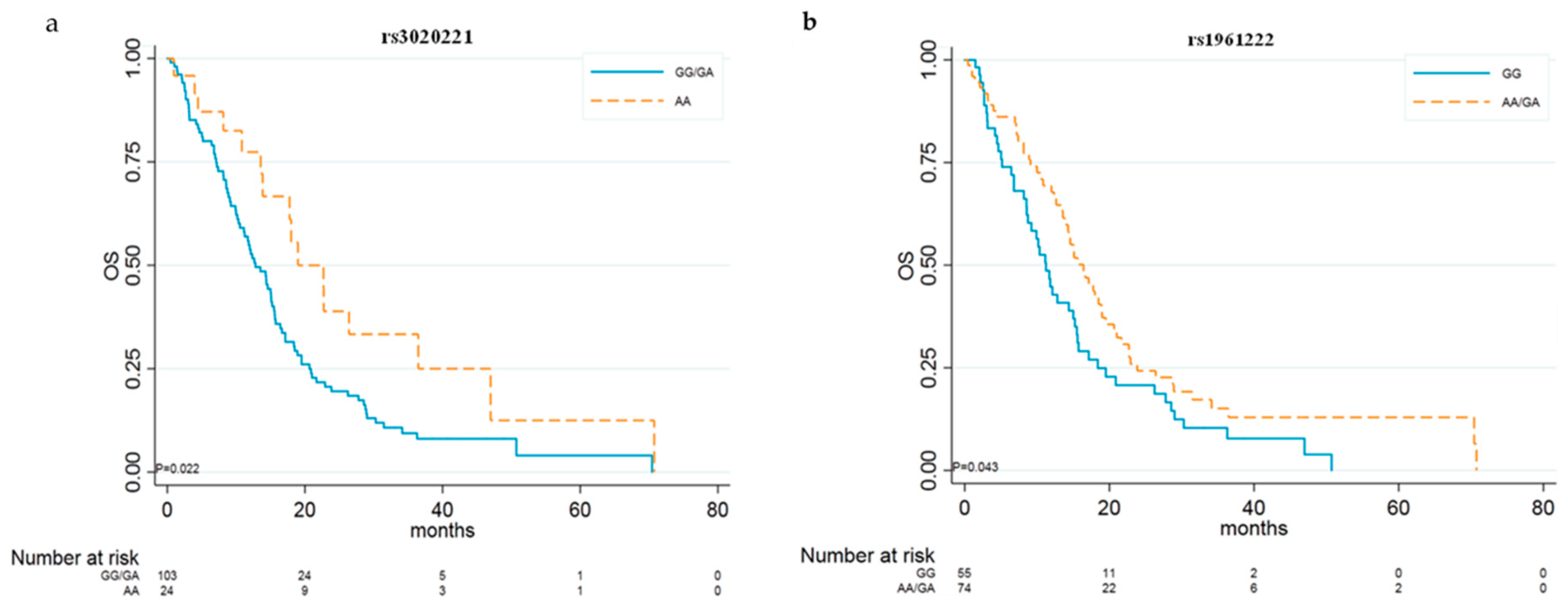
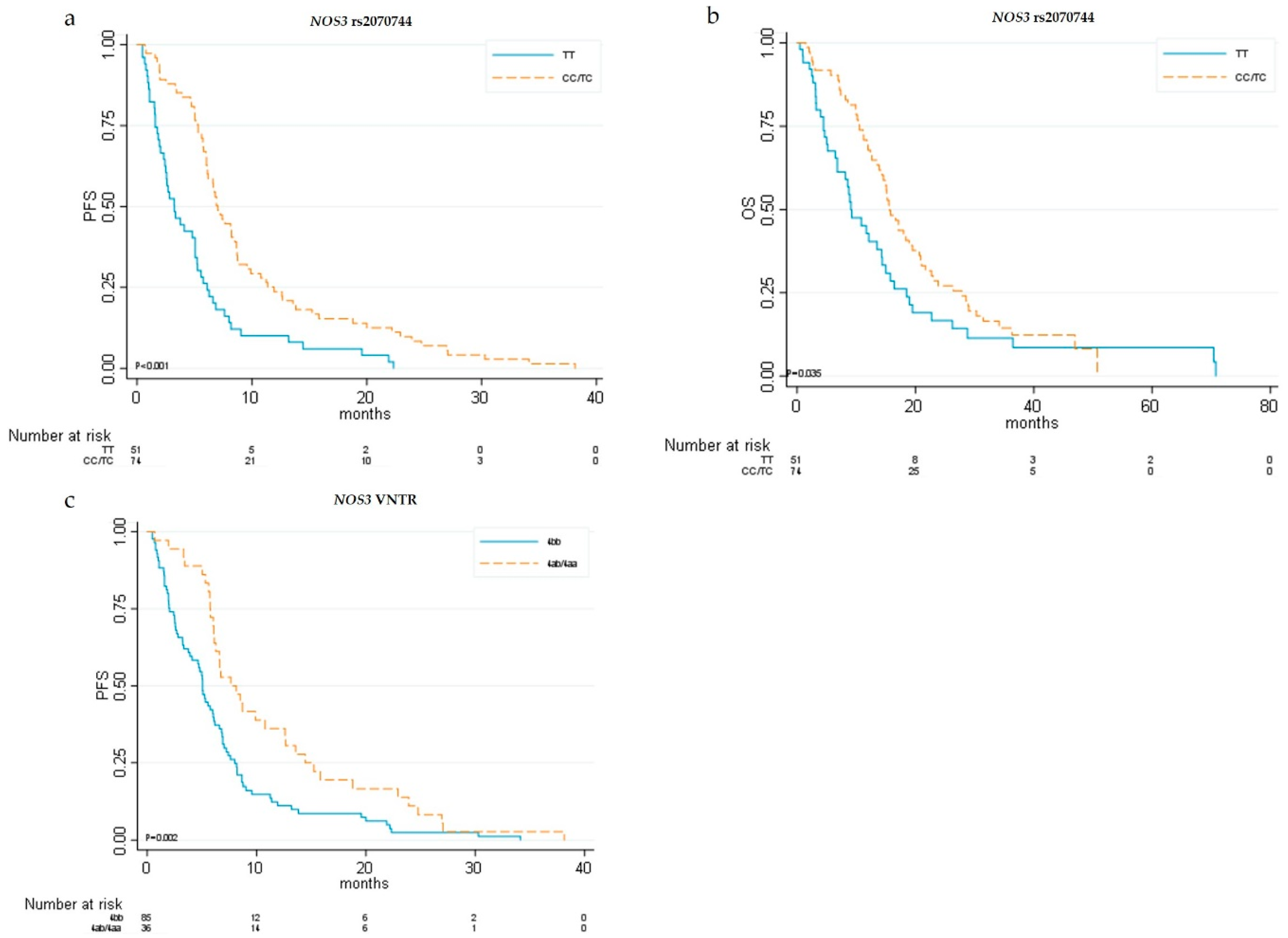
2.2. ANGPT2 and NOS3 Genotypes and Clinical Outcomes
2.3. ANGPT2 and NOS3 Genotypes and Disease Control Rate (DCR)
2.4. ANGPT2 and NOS3 Genotypes and Toxicities
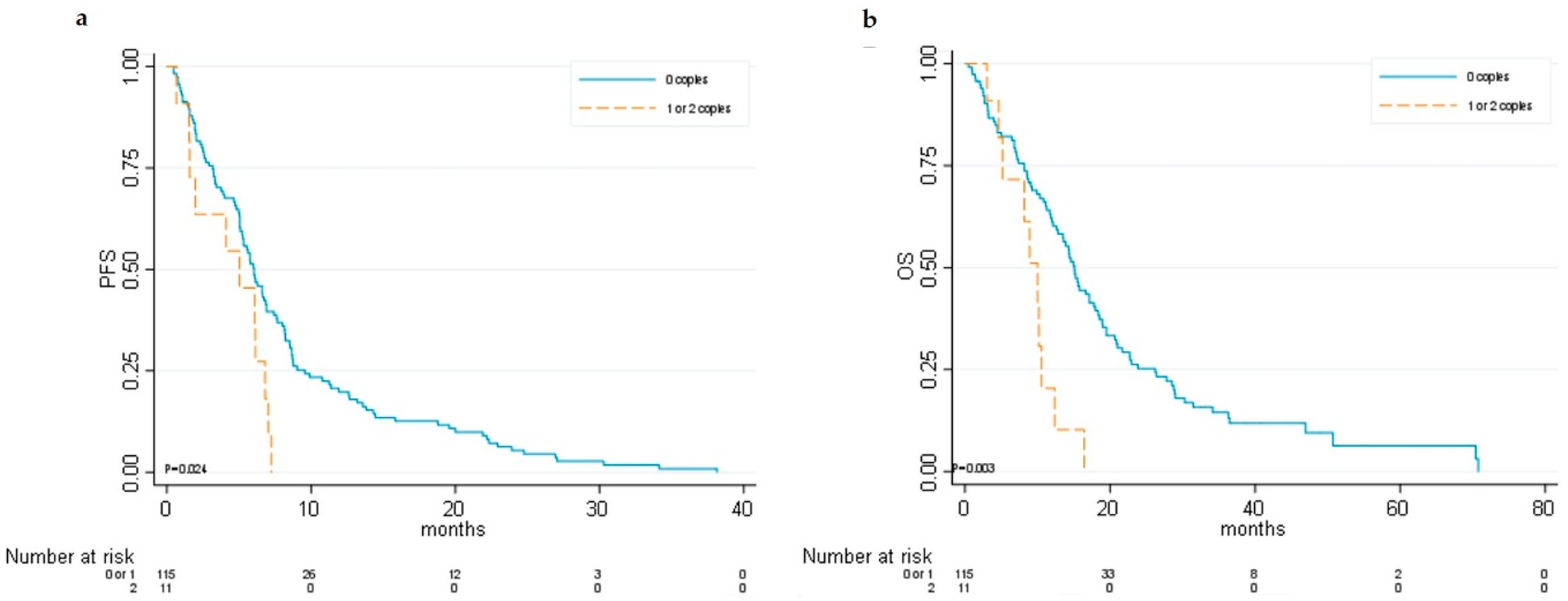
2.5. Haplotypes Analysis and Clinical Outcomes
2.6. Clustering Analysis
3. Discussion
4. Materials and Methods
4.1. Patient Enrollment
4.2. DNA Isolation and Genotyping
4.3. Statistical Analysis
4.4. Clustering Analysis Method
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- The Global Cancer Observatory Globocan 2018. Available online: Http://globocan.Iarc.Fr/ (accessed on 14 November 2018).
- Llovet, J.M.; Ricci, S.; Mazzaferro, V.; Hilgard, P.; Gane, E.; Blanc, J.F.; de Oliveira, A.C.; Santoro, A.; Raoul, J.L.; Forner, A.; et al. Sorafenib in Advanced Hepatocellular Carcinoma. N. Engl. J. Med. 2008, 359, 378–390. [Google Scholar] [CrossRef] [PubMed]
- Marisi, G.; Cucchetti, A.; Ulivi, P.; Canale, M.; Cabibbo, G.; Solaini, L.; Foschi, F.G.; De Matteis, S.; Ercolani, G.; Valgiusti, M.; et al. Ten Years of Sorafenib in Hepatocellular Carcinoma: Are there any Predictive and/or Prognostic Markers? World J. Gastroenterol. 2018, 24, 4152–4163. [Google Scholar] [CrossRef] [PubMed]
- Kudo, M.; Finn, R.S.; Qin, S.; Han, K.H.; Ikeda, K.; Piscaglia, F.; Baron, A.; Park, J.W.; Han, G.; Jassem, J.; et al. Lenvatinib Versus Sorafenib in First-Line Treatment of Patients with Unresectable Hepatocellular Carcinoma: A Randomised Phase 3 Non-Inferiority Trial. Lancet 2018, 391, 1163–1173. [Google Scholar] [CrossRef]
- Llovet, J.M.; Pena, C.E.; Lathia, C.D.; Shan, M.; Meinhardt, G.; Bruix, J.; SHARP Investigators Study Group. Plasma Biomarkers as Predictors of Outcome in Patients with Advanced Hepatocellular Carcinoma. Clin. Cancer Res. 2012, 18, 2290–2300. [Google Scholar] [CrossRef] [PubMed]
- Casadei Gardini, A.; Marisi, G.; Faloppi, L.; Scarpi, E.; Foschi, F.G.; Iavarone, M.; Lauletta, G.; Corbelli, J.; Valgiusti, M.; Facchetti, F.; et al. ENOS Polymorphisms and Clinical Outcome in Advanced HCC Patients Receiving Sorafenib: Final Results of the ePHAS Study. Oncotarget 2016, 7, 27988–27999. [Google Scholar] [CrossRef][Green Version]
- Bruix, J.; Cheng, A.L.; Meinhardt, G.; Nakajima, K.; De Sanctis, Y.; Llovet, J. Prognostic Factors and Predictors of Sorafenib Benefit in Patients with Hepatocellular Carcinoma: Analysis of Two Phase III Studies. J. Hepatol. 2017, 67, 999–1008. [Google Scholar] [CrossRef] [PubMed]
- Casadei Gardini, A.; Frassineti, G.L.; Foschi, F.G.; Ercolani, G.; Ulivi, P. Sorafenib and Regorafenib in HBV- Or HCV-Positive Hepatocellular Carcinoma Patients: Analysis of RESORCE and SHARP Trials. Dig. Liver Dis. 2017, 49, 943–944. [Google Scholar] [CrossRef]
- Duffy, M. Clinical use of Tumor Biomarkers: An Overview. Klin. Biochem. Metab. 2017, 25, 157–161. [Google Scholar]
- Miyahara, K.; Nouso, K.; Tomoda, T.; Kobayashi, S.; Hagihara, H.; Kuwaki, K.; Toshimori, J.; Onishi, H.; Ikeda, F.; Miyake, Y.; et al. Predicting the Treatment Effect of Sorafenib using Serum Angiogenesis Markers in Patients with Hepatocellular Carcinoma. J. Gastroenterol. Hepatol. 2011, 26, 1604–1611. [Google Scholar] [CrossRef]
- Scartozzi, M.; Faloppi, L.; Svegliati Baroni, G.; Loretelli, C.; Piscaglia, F.; Iavarone, M.; Toniutto, P.; Fava, G.; De Minicis, S.; Mandolesi, A.; et al. VEGF and VEGFR Genotyping in the Prediction of Clinical Outcome for HCC Patients Receiving Sorafenib: The ALICE-1 Study. Int. J. Cancer 2014, 135, 1247–1256. [Google Scholar] [CrossRef]
- Faloppi, L.; Casadei Gardini, A.; Masi, G.; Silvestris, N.; Loretelli, C.; Ulivi, P.; Vivaldi, C.; Bianconi, M.; Giampieri, R.; Bittoni, A.; et al. Angiogenesis Polymorphisms Profile in the Prediction of Clinical Outcome of Advanced HCC Patients Receiving Sorafenib: Combined Analysis of VEGF and HIF-1α. Final Results of the ALICE-2 Study. JCO 2016, 34, 280. [Google Scholar] [CrossRef]
- Ward, E.G.; Grosios, K.; Markham, A.F.; Jones, P.F. Genomic Structures of the Human Angiopoietins show Polymorphism in Angiopoietin-2. Cytogenet. Cell Genet. 2001, 94, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Hegen, A.; Koidl, S.; Weindel, K.; Marme, D.; Augustin, H.G.; Fiedler, U. Expression of Angiopoietin-2 in Endothelial Cells is Controlled by Positive and Negative Regulatory Promoter Elements. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 1803–1809. [Google Scholar] [CrossRef] [PubMed]
- Huber, A.; Grimm, C.; Pietrowski, D.; Zeillinger, R.; Bettendorf, H.; Husslein, P.; Hefler, L. An Angiopoietin-2 Gene Polymorphism in Unexplained Intrauterine Fetal Death: A Multi-Center Study. J. Reprod. Immunol. 2005, 65, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Banyasz, I.; Bokodi, G.; Vannay, A.; Szebeni, B.; Treszl, A.; Vasarhelyi, B.; Tulassay, T.; Szabo, A. Genetic Polymorphisms of Vascular Endothelial Growth Factor and Angiopoietin 2 in Retinopathy of Prematurity. Curr. Eye Res. 2006, 31, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Su, L.; Zhai, R.; Sheu, C.C.; Gallagher, D.C.; Gong, M.N.; Tejera, P.; Thompson, B.T.; Christiani, D.C. Genetic Variants in the Angiopoietin-2 Gene are Associated with Increased Risk of ARDS. Intensive Care Med. 2009, 35, 1024–1030. [Google Scholar] [CrossRef][Green Version]
- Stremitzer, S.; Zhang, W.; Yang, D.; Ning, Y.; Stintzing, S.; Sebio, A.; Sunakawa, Y.; Yamauchi, S.; Matsusaka, S.; El-Khoueiry, R.; et al. Genetic Variations in Angiopoietin and Pericyte Pathways and Clinical Outcome in Patients with Resected Colorectal Liver Metastases. Cancer 2015, 121, 1898–1905. [Google Scholar] [CrossRef]
- Makhoul, I.; Todorova, V.K.; Siegel, E.R.; Erickson, S.W.; Dhakal, I.; Raj, V.R.; Lee, J.Y.; Orloff, M.S.; Griffin, R.J.; Henry-Tillman, R.S.; et al. Germline Genetic Variants in TEK, ANGPT1, ANGPT2, MMP9, FGF2 and VEGFA are Associated with Pathologic Complete Response to Bevacizumab in Breast Cancer Patients. PLoS ONE 2017, 12, e0168550. [Google Scholar] [CrossRef]
- Branco, F.; Alencar, R.S.; Volt, F.; Sartori, G.; Dode, A.; Kikuchi, L.; Tani, C.M.; Chagas, A.L.; Pfiffer, T.; Hoff, P.; et al. The Impact of Early Dermatologic Events in the Survival of Patients with Hepatocellular Carcinoma Treated with Sorafenib. Ann. Hepatol. 2017, 16, 263–268. [Google Scholar] [CrossRef]
- M.Reig, M.; Boix, L.; Torres, F.; Darnell, A.; DiazGonzalez, A.; Llarch, N.; Belmonte, E.; Sapena, V.; Zamparelli, M.S.; Corominas, J.; et al. Towards Personalised Approach in Systemic Treatment for Hepatocellular Carcinoma. the Value of AGT M235T Gene Polymorphism. J. Hepatol. 2018, 68, S197. [Google Scholar] [CrossRef]
- Estfan, B.; Byrne, M.; Kim, R. Sorafenib in Advanced Hepatocellular Carcinoma: Hypertension as a Potential Surrogate Marker for Efficacy. Am. J. Clin. Oncol. 2013, 36, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Akutsu, N.; Sasaki, S.; Takagi, H.; Motoya, M.; Shitani, M.; Igarashi, M.; Hirayama, D.; Wakasugi, H.; Yamamoto, H.; Kaneto, H.; et al. Development of Hypertension within 2 Weeks of Initiation of Sorafenib for Advanced Hepatocellular Carcinoma is a Predictor of Efficacy. Int. J. Clin. Oncol. 2015, 20, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Casadei Gardini, A.; Scarpi, E.; Marisi, G.; Foschi, F.G.; Donati, G.; Giampalma, E.; Faloppi, L.; Scartozzi, M.; Silvestris, N.; Bisulli, M.; et al. Early Onset of Hypertension and Serum Electrolyte Changes as Potential Predictive Factors of Activity in Advanced HCC Patients Treated with Sorafenib: Results from a Retrospective Analysis of the HCC-AVR Group. Oncotarget 2016, 7, 15243–15251. [Google Scholar] [PubMed]
- Merkus, D.; Sorop, O.; Houweling, B.; Boomsma, F.; van den Meiracker, A.H.; Duncker, D.J. NO and Prostanoids Blunt Endothelin-Mediated Coronary Vasoconstrictor Influence in Exercising Swine. Am. J. Physiol. Heart Circ. Physiol. 2006, 291, H2075–H2081. [Google Scholar] [CrossRef] [PubMed]
- Wiley, K.E.; Davenport, A.P. Physiological Antagonism of Endothelin-1 in Human Conductance and Resistance Coronary Artery. Br. J. Pharmacol. 2001, 133, 568–574. [Google Scholar] [CrossRef] [PubMed]
- Casadei Gardini, A.; Faloppi, L.; Aprile, G.; Brunetti, O.; Caparello, C.; Corbelli, J.; Chessa, L.; Bruno, D.; Ercolani, G.; Leonetti, A.; et al. Multicenter Prospective Study of Angiogenesis Polymorphism Validation in HCC Patients Treated with Sorafenib. an INNOVATE Study Protocol. Tumori 2017, 104, 476–479. [Google Scholar] [CrossRef] [PubMed]
- Lencioni, R.; Llovet, J.M. Modified RECIST (mRECIST) Assessment for Hepatocellular Carcinoma. Semin. Liver Dis. 2010, 30, 52–60. [Google Scholar] [CrossRef]
- Savas, S.; Liu, G.; Xu, W. Special Considerations in Prognostic Research in Cancer Involving Genetic Polymorphisms. BMC Med. 2013, 11, 149. [Google Scholar] [CrossRef]
- Barrett, J.C.; Fry, B.; Maller, J.; Daly, M.J. Haploview: Analysis and Visualization of LD and Haplotype Maps. Bioinformatics 2005, 21, 263–265. [Google Scholar] [CrossRef]
- Gabriel, S.B.; Schaffner, S.F.; Nguyen, H.; Moore, J.M.; Roy, J.; Blumenstiel, B.; Higgins, J.; DeFelice, M.; Lochner, A.; Faggart, M.; et al. The Structure of Haplotype Blocks in the Human Genome. Science 2002, 296, 2225–2229. [Google Scholar] [CrossRef]
- French, B.; Lumley, T.; Cappola, T.P.; Mitra, N. Non-Iterative, Regression-Based Estimation of Haplotype Associations with Censored Survival Outcomes. Stat. Appl. Genet. Mol. Biol. 2012, 11. [Google Scholar] [CrossRef]
- McLaren, W.; Gil, L.; Hunt, S.E.; Riat, H.S.; Ritchie, G.R.; Thormann, A.; Flicek, P.; Cunningham, F. The Ensembl Variant Effect Predictor. Genome Biol. 2016, 17, 122. [Google Scholar] [CrossRef]
| Clinical and Pathologic Variables | No. (%) |
|---|---|
| Median age at start of treatment (min–max) | 70 (25–88) |
| Gender | |
| Male | 109 (80.7) |
| Female | 26 (19.3) |
| Etiology | |
| Metabolic syndrome | 18 (13.3) |
| Alcoholic | 10 (7.4) |
| Viral—HBV | 22 (16.3) |
| Viral—HCV | 78 (57.8) |
| Cryptogenic | 7 (5.2) |
| BCLC stage | |
| B | 37 (27.4) |
| C | 98 (72.6) |
| Child–Pugh | |
| A | 125 (92.6) |
| B | 10 (7.4) |
| ECOG Performance Status | |
| 0 | 83 (61.5) |
| 1–2 | 52 (38.5) |
| Sorafenib dose reduction | |
| No | 59 (61.5) |
| Yes | 37 (38.5) |
| Missing data | 39 |
| Extra-hepatic spread | |
| No | 81 (64.3) |
| Yes | 45 (35.7) |
| Serum α-FP level | |
| ≤400 | 54 (40) |
| >400 | 35 (25.9) |
| Missing data | 46 |
| Clinical and Pathologic Variables | PFS | OS | ||||
|---|---|---|---|---|---|---|
| Median PFS [95% CI] | HR [95% CI] | p | Median OS [95% CI] | HR [95% CI] | p | |
| Gender | ||||||
| Female | 6.11 [3.22–8.18] | 1 | 12.35 [5.72–20.89] | 1 | ||
| Male | 5.62 [5.03–6.27] | 0.96 [0.62–1.50] | 0.873 | 14.85 [11.83–15.80] | 0.94 [0.59–1.52] | 0.814 |
| Median age at start of treatment * | 0.92 [0.85–0.995] | 0.038 | 0.94 [0.87–1.02] | 0.118 | ||
| Etiology | ||||||
| Viral—HCV | 6.11 [5.06–6.90] | 1 | 14.29 [11.14–17.77] | 1 | ||
| Cryptogenic | 3.98 [3.19–21.91] | 0.96 [0.44–2.11] | 0.926 | 16.43 [3.98–NR] | 0.70 [0.29–1.76] | 0.453 |
| Alcoholic | 5.26 [1.41–8.71] | 0.98 [0.50–1.92] | 0.956 | 14.39 [1.41–17.15] | 1.23 [0.59–2.59] | 0.580 |
| Metabolic syndrome | 6.01 [3.25–8.51] | 1.21 [0.71–2.06] | 0.478 | 15.64 [6.80–21.68] | 1.11 [0.63–1.96] | 0.710 |
| Viral—HBV | 5.06 [2.33–6.90] | 1.45 [0.90–2.34] | 0.131 | 8.57 [4.66–15.24] | 1.95 [1.17–3.26] | 0.011 |
| Child–Pugh | ||||||
| A | 5.75 [5.06–6.60] | 1 | 14.59 [11.83–15.74] | 1 | ||
| B | 6.11 [0.69–11.37] | 0.76 [0.37–1.57] | 0.459 | 13.53 [1.48–26.41] | 1.16 [0.56–2.40] | 0.683 |
| BCLC | ||||||
| B | 6.60 [5.06–8.77] | 1 | 14.36 [11.24–16.43] | 1 | ||
| C | 5.32 [4.11–6.14] | 1.27 [0.86–1.88] | 0.225 | 14.59 [9.99–16.43] | 1.05 [0.68–1.62] | 0.819 |
| ECOG Performance Status | ||||||
| 0 | 5.75 [5.03–6.60] | 1 | 14.39 [11.7–15.74] | 1 | ||
| 1–2 | 6.01 [2.69–7.42] | 1.01 [0.71–1.45] | 0.949 | 15.01 [8.18–18.92] | 1.23 [0.84–1.80] | 0.294 |
| Extra-hepatic spread | ||||||
| Yes | 2.83 [1.94–5.22] | 1 | 10.84 [6.96–15.08] | 1 | ||
| No | 6.27 [5.72–7.65] | 0.50 [0.34–0.73] | <0.001 | 15.60 [12.81–18.00] | 0.65 [0.43–0.99] | 0.043 |
| Serum α-FP level | ||||||
| ≤400 | 5.75 [3.75–6.64] | 1 | 13.57 [10.35–16.66] | 1 | ||
| >400 | 5.72 [2.92–7.23] | 0.87 [0.56–1.34] | 0.526 | 13.86 [8.15–15.80] | 1.26 [0.80–2.01] | 0.320 |
| Gene Polymorphisms | Genetic Model | PFS | OS | ||||
|---|---|---|---|---|---|---|---|
| Median PFS [95% CI] | HR [95% CI] | p | Median OS [95% CI] | HR [95% CI] | p | ||
| ANGPT2 | |||||||
| rs3739392 | DOM | ||||||
| TT | 5.62 [5.03–6.73] | 1 | 14.39 [11.24–16.43] | 1 | |||
| CC/TC | 6.14 [3.91–8.54] | 0.94 [0.64–1.39] | 0.765 | 13.57 [8.15–18.00] | 0.92 [0.60–1.39] | 0.679 | |
| rs3739391 | DOM | ||||||
| CC | 5.75 [5.06–6.90] | 1 | 15.11 [12.65–18.50] | 1 | |||
| TT/CT | 6.04 [3.91–6.80] | 1.13 [0.79–1.63] | 0.506 | 11.14 [8.54–15.64] | 1.17 [0.79–1.73] | 0.445 | |
| rs3739390 | DOM | ||||||
| GG | 5.75 [5.03–6.60] | 1 | 14.36 [11.24–15.74] | 1 | |||
| CC/GC | 6.27 [2.60–12.61] | 0.83 [0.52–1.31] | 0.416 | 12.81 [8.15–20.89] | 0.88 [0.54–1.44] | 0.621 | |
| rs55633437 | DOM | ||||||
| GG | 6.27 [5.75–7.23] | 1 | 15.51 [13.57–18.40] | 1 | |||
| TT/GT | 1.58 [0.76–3.32] | 4.79 [2.73–8.35] | <0.001 | 4.66 [2.69–8.57] | 4.86 [2.73–8.67] | <0.001 | |
| rs3020221 | REC | ||||||
| GG/GA | 5.78 [5.06–6.60] | 1 | 12.81 [10.35–15.24] | 1 | |||
| AA | 8.77 [4.01–10.78] | 0.72 [0.45–1.14] | 0.163 | 18.99 [13.57–36.47] | 0.53 [0.31–0.92] | 0.024 | |
| rs1961222 | DOM | ||||||
| GG | 5.32 [3.19–6.60] | 1 | 11.24 [8.54–15.01] | 1 | |||
| AA /GA | 6.04 [5.09–8.02] | 0.93 [0.65–1.34] | 0.712 | 16.43 [13.57–18.99] | 0.67 [0.46–0.99] | 0.044 | |
| rs17063434 | DOM | ||||||
| TT | 5.62 [5.03–6.14] | 1 | 0.84 [11.99–17.77] | 1 | |||
| CC /TC | 6.80 [6.14–8.54] | 0.93 [0.55–1.56] | 0.779 | 11.24 [8.15–15.64] | 1.59 [0.94–2.69] | 0.084 | |
| rs2916747 | |||||||
| TT | 5.78 [5.06–6.60] | 1 | 14.39 [11.99–16.43] | 1 | |||
| TC | 6.27 [1.97–13.83] | 0.61 [0.34–1.10] | 0.102 | 11.70 [4.20–27.79] | 1.09 [0.61–1.94] | 0.784 | |
| NOS3 | |||||||
| NOS3 +894 (rs1799983) | DOM | ||||||
| GG | 5.22 [2.83–6.11] | 1 | 15.74 [9.23–18.50] | 1 | |||
| GT/TT | 6.60 [5.32–8.18] | 0.81 [0.57–1.16] | 0.251 | 14.29 [11.14–15.51] | 1.14 [0.77–1.68] | 0.527 | |
| VNTR4a4b | DOM | ||||||
| 4bb | 5.06 [3.75–6.11] | 1 | 11.99 [9.10–14.85] | 1 | |||
| 4aa/4ab | 7.65 [6.08–12.61] | 0.54 [0.36–0.80] | 0.002 | 17.15 [14.59–20.89] | 0.68 [0.44–1.05] | 0.080 | |
| NOS3-786 (rs2070744) | DOM | ||||||
| TT | 3.25 [2.33–5.06] | 1 | 9.10 [6.80–14.29] | 1 | |||
| CC/TC | 7.03 [6.08–8.67] | 0.43 [0.30–0.63] | <0.001 | 15.60 [13.86–19.51] | 0.65 [0.44–0.97] | 0.036 | |
| Patient Characteristics | HR [95% CI] | p |
|---|---|---|
| Extra-hepatic spread | ||
| Yes | 1 | |
| No | 0.54 [0.35–0.84] | 0.007 |
| Etiology | ||
| Viral—HCV | 1 | |
| Biliary cirrhosis/cryptogenic | 0.33 [0.08–1.39] | 0.131 |
| Alcoholic | 1.69 [0.75–3.84 | 0.207 |
| Metabolic syndrome | 1.50 [0.80–2.83] | 0.209 |
| Viral—HBV | 2.42 [1.38–4.26] | 0.002 |
| NOS3-786 (rs2070744) | ||
| TT | 1 | |
| CC/TC | 0.67 [0.47–0.96] | 0.030 |
| ANGPT2 rs55633437 | ||
| GG | 1 | |
| TT/GT | 5.48 [2.85–10.54] | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marisi, G.; Petracci, E.; Raimondi, F.; Faloppi, L.; Foschi, F.G.; Lauletta, G.; Iavarone, M.; Canale, M.; Valgiusti, M.; Neri, L.M.; et al. ANGPT2 and NOS3 Polymorphisms and Clinical Outcome in Advanced Hepatocellular Carcinoma Patients Receiving Sorafenib. Cancers 2019, 11, 1023. https://doi.org/10.3390/cancers11071023
Marisi G, Petracci E, Raimondi F, Faloppi L, Foschi FG, Lauletta G, Iavarone M, Canale M, Valgiusti M, Neri LM, et al. ANGPT2 and NOS3 Polymorphisms and Clinical Outcome in Advanced Hepatocellular Carcinoma Patients Receiving Sorafenib. Cancers. 2019; 11(7):1023. https://doi.org/10.3390/cancers11071023
Chicago/Turabian StyleMarisi, Giorgia, Elisabetta Petracci, Francesco Raimondi, Luca Faloppi, Francesco Giuseppe Foschi, Gianfranco Lauletta, Massimo Iavarone, Matteo Canale, Martina Valgiusti, Luca Maria Neri, and et al. 2019. "ANGPT2 and NOS3 Polymorphisms and Clinical Outcome in Advanced Hepatocellular Carcinoma Patients Receiving Sorafenib" Cancers 11, no. 7: 1023. https://doi.org/10.3390/cancers11071023
APA StyleMarisi, G., Petracci, E., Raimondi, F., Faloppi, L., Foschi, F. G., Lauletta, G., Iavarone, M., Canale, M., Valgiusti, M., Neri, L. M., Ulivi, P., Orsi, G., Rovesti, G., Vukotic, R., Conti, F., Cucchetti, A., Ercolani, G., Andrikou, K., Cascinu, S., ... Casadei-Gardini, A. (2019). ANGPT2 and NOS3 Polymorphisms and Clinical Outcome in Advanced Hepatocellular Carcinoma Patients Receiving Sorafenib. Cancers, 11(7), 1023. https://doi.org/10.3390/cancers11071023










