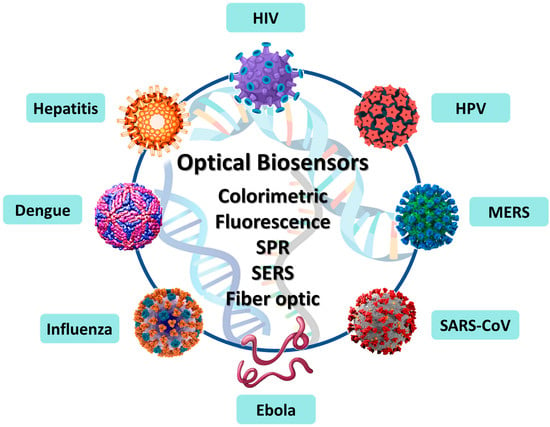
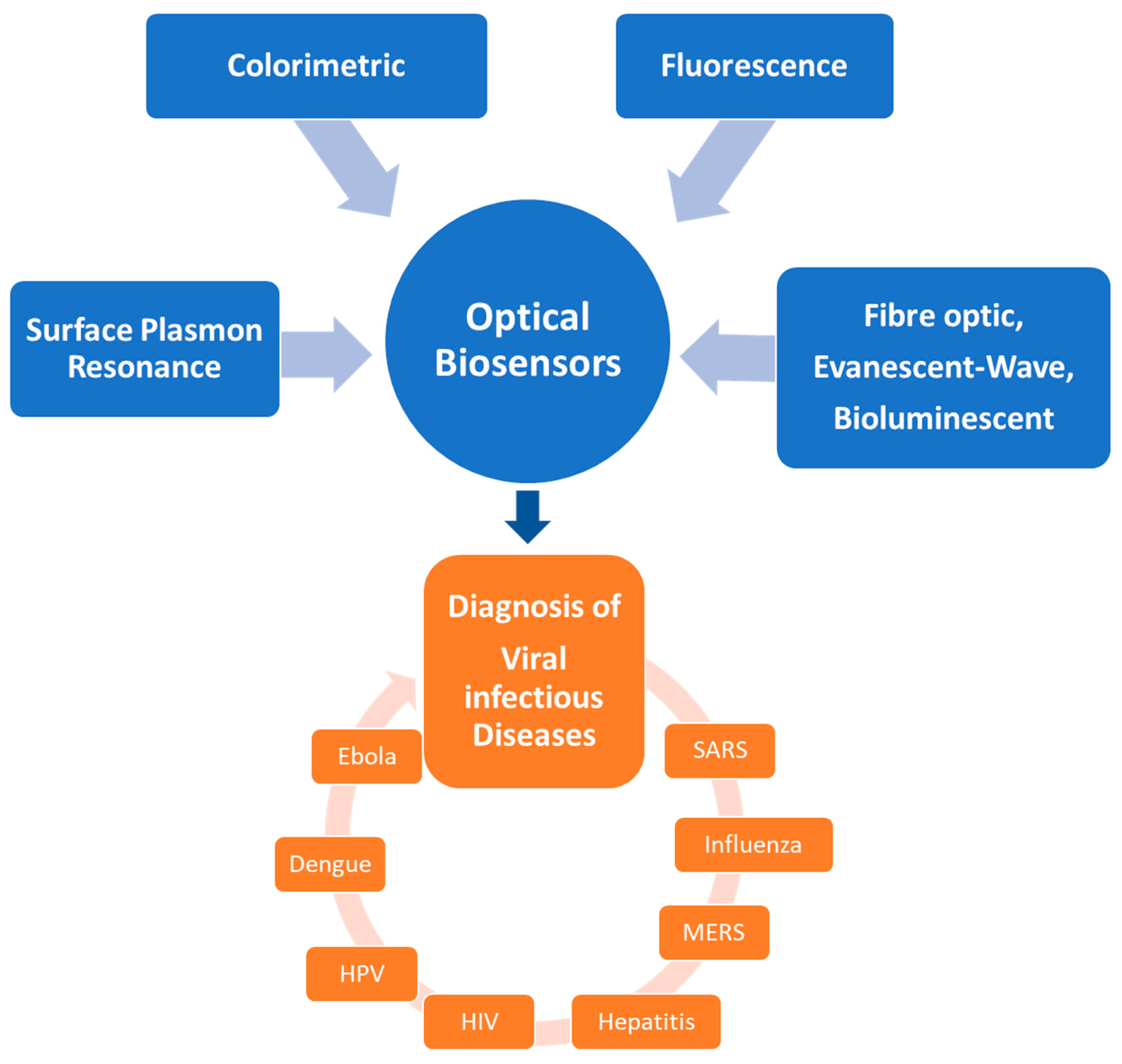
Recent Progress on Optical Biosensors Developed for Nucleic Acid Detection Related to Infectious Viral Diseases
Abstract
1. Introduction
2. Infectious Viral Diseases
2.1. Severe Acute Respiratory Syndrome (SARS)
2.2. Influenza
2.3. Middle East Respiratory Syndrome (MERS)
2.4. Hepatitis
2.5. Human Immunodeficiency Virus (HIV)
2.6. Human Papilloma Virus (HPV)
2.7. Dengue
2.8. Ebola
3. Diagnostics of Infectious Viral Diseases with Optical Biosensors
3.1. Colorimetric Biosensors
3.2. Fluorescence-Based Biosensors
3.3. Surface-Enhanced Raman Spectroscopy-Based Biosensors
3.4. Surface Plasmon Resonance-Based Biosensors and Localized Surface Plasmon (LSP)-Based Biosensors
3.5. Other Optical Biosensors (Evanescent-Wave Optical Biosensors, Fiber Optic Biosensors, Bioluminescent Optical Fibre Biosensors)
4. Conclusions and Future Prospects
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Maddali, H.; Miles, C.E.; Kohn, J.; O’Carroll, D.M. Optical Biosensors for Virus Detection: Prospects for SARS-CoV-2/COVID-19. ChemBioChem 2021, 22, 1176–1189. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, D.S.; Pekker, D.; Goldbart, P.M.; Bezryadin, A. Quantum interference device made by DNA templating of superconducting nanowires. Science 2005, 308, 1762–1765. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Balasubramanian, S.; Kagan, D.; Manesh, K.M.; Campuzano, S.; Wang, J. Motion-based DNA detection using catalytic nanomotors. Nat. Commun. 2010, 1, 36. [Google Scholar] [CrossRef]
- Kerman, K.; Kobayashi, M.; Tamiya, E. Recent trends in electrochemical DNA biosensor technology. Meas. Sci. Technol. 2004, 15, R1–R11. [Google Scholar] [CrossRef]
- Erdem, A.; Ozsoz, M. Nucleic Acids as Biorecognition Element in Biosensor Development. In Nucleic Acid Biosensors for Environmental Pollution Monitoring; Palchetti, I., Mascini, M., Eds.; Royal Society of Chemistry: London, UK, 2011; pp. 17–33. [Google Scholar]
- Huang, R.; He, N.; Li, Z. Recent progresses in DNA nanostructure-based biosensors for detection of tumor markers. Biosens. Bioelectron. 2018, 109, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekaran, A.R.; Punnoose, J.A.; Zhou, L.; Dey, P.; Dey, B.K.; Halvorsen, K. DNA nanotechnology approaches for microRNA detection and diagnosis. Nucleic Acids Res. 2019, 47, 10489–10505. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.Y.; Seelig, G. Dynamic DNA nanotechnology using strand-displacement reactions. Nat. Chem. 2011, 3, 103–113. [Google Scholar] [CrossRef]
- Zheng, X.T.; Tan, Y.N. Recent development of nucleic acid nanosensors to detect sequence-specific binding interactions: From metal ions, small molecules to proteins and pathogens. Sens. Int. 2020, 1, 100034. [Google Scholar] [CrossRef]
- Fortunati, S.; Pedrini, F.; Del Grosso, E.; Baranda Pellejero, L.; Bertucci, A. Design of Specific Nucleic Acid-Based Biosensors for Protein Binding Activity. Anal. Sens. 2022, 2, e202200037. [Google Scholar] [CrossRef]
- Zhang, H.; Li, F.; Dever, B.; Wang, C.; Li, X.F.; Le, X.C. Assembling DNA through affinity binding to achieve ultrasensitive protein detection. Angew. Chem. Int. Ed. Engl. 2013, 52, 10698–10705. [Google Scholar] [CrossRef]
- Koyun, S.; Akgonullu, S.; Yavuz, H.; Erdem, A.; Denizli, A. Surface Plasmon Resonance Aptasensor for Detection of Human Activated Protein C. Talanta 2019, 194, 528–533. [Google Scholar] [CrossRef]
- Chen, C.; Wang, J. Optical biosensors: An exhaustive and comprehensive review. Analyst 2020, 145, 1605–1628. [Google Scholar] [CrossRef]
- Strauss, J.H.; Strauss, E.G. Overview of Viruses and Virus Infection. Viruses Hum. Dis. 2008, 1–33. [Google Scholar] [CrossRef]
- Louten, J. Virus Transmission and Epidemiology. Essent. Hum. Virol. 2016, 71–92. [Google Scholar] [CrossRef]
- Peiris, J.S. Severe Acute Respiratory Syndrome (SARS). J. Clin. Virol. 2003, 28, 245–247. [Google Scholar] [CrossRef] [PubMed]
- Goud, K.Y.; Reddy, K.K.; Khorshed, A.; Kumar, V.S.; Mishra, R.K.; Oraby, M.; Ibrahim, A.H.; Kim, H.; Gobi, K.V. Electrochemical diagnostics of infectious viral diseases: Trends and challenges. Biosens. Bioelectron. 2021, 180, 113112. [Google Scholar] [CrossRef]
- Sharma, A.; Mishra, R.K.; Goud, K.Y.; Mohamed, M.A.; Kummari, S.; Tiwari, S.; Li, Z.; Narayan, R.; Stanciu, L.A.; Marty, J.L. Optical Biosensors for Diagnostics of Infectious Viral Disease: A Recent Update. Diagnostics 2021, 11, 2083. [Google Scholar] [CrossRef] [PubMed]
- Moghadami, M. A Narrative Review of Influenza: A Seasonal and Pandemic Disease. Iran. J. Med. Sci. 2017, 42, 2–13. [Google Scholar]
- Tan, J.; Asthagiri-Arunkumar, G.; Krammer, F. Universal influenza virus vaccines and therapeutics: Where do we stand with influenza B virus? Curr. Opin. Immunol. 2018, 53, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Middle East Respiratory Syndrome Coronavirus (MERS-CoV). Available online: https://www.who.int/health-topics/middle-east-respiratory-syndrome-coronavirus-mers#tab=tab_1 (accessed on 29 November 2022).
- Parlak, E. Middle East Respiratory Syndrome: MERS. J. Microbiol. Infect. Dis. 2015, 5, 93–98. [Google Scholar] [CrossRef]
- Groot, R.J.d.; Baker, S.C.; Baric, R.S.; Brown, C.S.; Drosten, C.; Enjuanes, L.; Fouchier, R.A.; Galiano, M.; Gorbalenya, A.E.; Memish, Z.A.; et al. Middle East respiratory syndrome coronavirus (MERS-CoV): Announcement of the Coronavirus Study Group. J. Virol. 2013, 87, 7790–7792. [Google Scholar] [CrossRef] [PubMed]
- Krajden, M. Hepatitis. Can. J. Infect. Dis. 2001, 12, 329–331. [Google Scholar] [CrossRef]
- Mehta, P.; Reddivari, A.K.R. Hepatitis; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Birjandi, M.M.; Oroei, M. The prevalence of positive rapid diagnostic test of hepatitis C virus infection in Ghana. Pan Afr. Med. J. 2020, 36, 322. [Google Scholar] [PubMed]
- Sharp, P.M.; Hahn, B.H. Origins of HIV and the AIDS pandemic. Cold Spring Harb. Perspect. Med. 2011, 1, a006841. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.who.int/news-room/fact-sheets/detail/hiv-aids (accessed on 29 November 2022).
- Zulfiqar, H.F.; Javed, A.; Sumbal; Afroze, B.; Ali, Q.; Akbar, K.; Nadeem, T.; Rana, M.A.; Nazar, Z.A.; Nasir, I.A.; et al. HIV Diagnosis and Treatment through Advanced Technologies. Front. Public Health 2017, 5, 32. [Google Scholar] [CrossRef] [PubMed]
- Martel, C.d.; Ferlay, J.; Franceschi, S.; Vignat, J.; Bray, F.; Forman, D.; Plummer, M. Global burden of cancers attributable to infections in 2008: A review and synthetic analysis. Lancet Oncol. 2012, 13, 607–615. [Google Scholar] [CrossRef]
- Wang, C.J.; Palefsky, J.M. Human Papillomavirus (HPV) Infections and the Importance of HPV Vaccination. Curr. Epidemiol. Rep. 2015, 2, 101–109. [Google Scholar] [CrossRef]
- Kularatne, S.A.; Dalugama, C. Dengue infection: Global importance, immunopathology and management. Clin. Med. 2022, 22, 9–13. [Google Scholar] [CrossRef]
- Qavi, A.; Meserve, K.; Aman, M.J.; Vu, H.; Zeitlin, L.; Dye, J.M.; Froude, J.W.; Leung, D.W.; Yang, L.; Holtsberg, F.W.; et al. Rapid detection of an Ebola biomarker with optical microring resonators. Cell Rep. Methods 2022, 2, 100234. [Google Scholar] [CrossRef]
- Hasan, S.; Ahmad, S.A.; Masood, R.; Saeed, S. Ebola virus: A global public health menace: A narrative review. J. Family Med. Prim. Care 2019, 8, 2189–2201. [Google Scholar]
- Karunakaran, C.; Rajkumar, R.; Bhargava, K. Introduction to Biosensors. In Biosensors and Bioelectronics; Karunakaran, C., Bhargava, K., Benjamin, R., Eds.; Elsevier Inc.: Amsterdam, The Netherlands, 2015; pp. 1–68. [Google Scholar]
- Ensafi, A.A. An introduction to sensors and biosensors. In Electrochemical Biosensors; Ensafi, A.A., Ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2019; pp. 1–10. [Google Scholar]
- Junhui, Z.; Hong, C.; Ruifu, Y. DNA based biosensors. Biotechnol. Adv. 1997, 15, 43–58. [Google Scholar]
- Wang, J. Electrochemical nucleic acid biosensors. Anal. Chim. Acta 2002, 469, 63–71. [Google Scholar] [CrossRef]
- Wang, J. From DNA biosensors to gene chips. Nucleic Acid Res. 2000, 28, 3011–3016. [Google Scholar] [CrossRef]
- Rashid, J.I.A.; Yusof, N.A. The strategies of DNA immobilization and hybridization detection mechanism in the construction of electrochemical DNA sensor: A review. Sens. Bio-Sens Res. 2017, 16, 19–31. [Google Scholar] [CrossRef]
- D’Agata, R.; Giuffrida, M.C.; Spoto, G. Peptide Nucleic Acid-Based Biosensors for Cancer Diagnosis. Molecules 2017, 22, 1951. [Google Scholar] [CrossRef] [PubMed]
- Moreau, V.; Voirin, E.; Paris, C.; Kotera, M.; Nothisen, M.; Remy, J.S.; Behr, J.P.; Erbacher, P.; Lenne-Samuel, N. Zip nucleic acids: New high affinity oligonucleotides as potent primers for PCR and reverse transcription. Nucleic Acids Res. 2009, 37, e130. [Google Scholar] [CrossRef] [PubMed]
- Noir, R.; Kotera, M.; Pons, B.; Remy Behr, J.S.J.P. Oligonucleotide-oligospermine conjugates (zip nucleic acids): A convenient means of finely tuning hybridization temperatures. J. Am. Chem. Soc. 2008, 9, 13500–13505. [Google Scholar] [CrossRef]
- Paris, C.; Moreau, V.; Deglane, G.; Voirin, E.; Erbacher, P.; Lenne-Samuel, N. Zip nucleic acids are potent hydrolysis probes for quantitative PCR. Nucleic Acids Res. 2010, 38, e95. [Google Scholar] [CrossRef]
- Erdem, A.; Eksin, E. Magnetic beads assay based on Zip nucleic acid for electrochemical detection of Factor V Leiden mutation. Int. J. Biol. Macromol. 2019, 125, 839–846. [Google Scholar] [CrossRef]
- Erdem, A.; Eksin, E. Impedimetric Sensing of Factor V Leiden Mutation by Zip Nucleic Acid Probe and Electrochemical Array. Biosensors 2020, 10, 116. [Google Scholar] [CrossRef]
- Erdem, A.; Eksin, E. Zip Nucleic Acid Based Single-use Biosensor for Electrochemical Detection of Factor V Leiden Mutation. Sens. Actuators B Chem. 2019, 288, 634–640. [Google Scholar] [CrossRef]
- Erdem, A.; Eksin, E. ZNA Probe Immobilized Single-Use Electrodes for Impedimetric Detection of Nucleic Acid Hybridization Related to Single Nucleotide Mutation. Anal. Chim. Acta 2019, 1071, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, L.C.; Cepeda, D.I.; Torres, A.F.L.; Cortes, M.M.A.; Monroy, Z.J.R.; Castaneda, J.E.G. Nucleic acid-based biosensors: Analytical devices for prevention, diagnosis and treatment of diseases. J. Vitae 2021, 28, 347259. [Google Scholar]
- Song, Y.; Wei, W.; Qu, X. Colorimetric Biosensing Using Smart Materials. Adv. Mater. 2011, 23, 4215–4236. [Google Scholar] [CrossRef]
- Stewart, M.E.; Anderton, C.R.; Thompson, L.B.; Maria, J.; Gray, S.K.; Rogers, J.A.; Nuzzo, R.G. Nanostructured plasmonic sensors. Chem. Rev. 2008, 108, 494–521. [Google Scholar]
- Soper, S.A.; Brown, K.; Ellington, A.; Frazier, B.; Garcia-Manero, G.; Gau, V.; Gutman, S.I.; Hayes, D.F.; Korte, B.; Landers, J.L.; et al. Point-of-care biosensor systems for cancer diagnostics/prognostics. Biosens. Bioelectron. 2006, 21, 1932–1942. [Google Scholar] [CrossRef]
- Frens, G. Controlled nucleation for the regulation of the particle size in monodisperse gold suspensions. Nat. Phys. Sci. 1973, 241, 20. [Google Scholar] [CrossRef]
- Mirkin, C.A.; Letsinger, R.L.; Mucic, R.C.; Storhoff, J.J. A DNA-based method for rationally assembling nanoparticles into macroscopic materials. Nature 1996, 382, 607. [Google Scholar] [CrossRef]
- Li, H.; Rothberg, L. Colorimetric detection of DNA sequences based on electrostatic interactions with unmodified gold nanoparticles. Proc. Natl. Acad. Sci. USA 2004, 101, 14036–14039. [Google Scholar] [CrossRef]
- Yang, T.; Luo, Z.; Tian, Y.; Qian, C.; Duan, Y. Design strategies of AuNPs-based nucleic acid colorimetric biosensors. Trends Anal. Chem. 2020, 124, 115795. [Google Scholar] [CrossRef]
- Rahman, S.A.; Saadun, R.; Azmi, N.E.; Ariffin, N.; Abdullah, J.; Yusof, N.A.; Sidek, H.; Hajian, R. Label-free dengue detection utilizing PNA/DNA hybridization based on the aggregation process of unmodified gold nanoparticles. J. Nanomater. 2014, 2014, 839286. [Google Scholar]
- Liu, Y.; Zhang, L.; Wei, W.; Zhao, H.; Zhou, Z.; Zhang, Y.; Liu, S. Colorimetric detection of influenza A virus using antibody-functionalized gold nanoparticles. Analyst 2015, 140, 3989–3995. [Google Scholar] [CrossRef] [PubMed]
- Teengam, P.; Siangproh, W.; Tuantanont, A.; Vilaivan, T.; Chailapakul, O.; Henry, C.S. Multiplex Paper-Based Colorimetric DNA Sensor Using Pyrrolidinyl Peptide Nucleic Acid-Induced AgNPs Aggregation for Detecting MERS-CoV, MTB, and HPV Oligonucleotides. Anal. Chem. 2017, 89, 5428–5435. [Google Scholar] [CrossRef] [PubMed]
- Notomi, T.; Okayama, H.; Masubuchi, H.; Yonekawa, T.; Watanabe, K.; Amino, N.; Hase, T. Loop-mediated isothermal amplification of DNA. Nucleic Acids Res. 2000, 28, e63. [Google Scholar] [CrossRef]
- Ma, X.-J.; Shu, Y.; Qin, M.; Nie, K.; Wang, D.-M.; Gao, R.-B.; Wang, M.; Wen, L.-Y.; Han, F.; Zhou, S.-M.; et al. Visual detection of pandemic influenza A H1N1 Virus 2009 by reverse-transcription loop-mediated isothermal amplification with hydroxynaphthol blue dye. J. Virol. Methods 2010, 167, 214–217. [Google Scholar] [CrossRef]
- Kumvongpin, R.; Jearanaikool, P.; Wilailuckana, C.; Sae-Ung, N.; Prasongdee, P.; Daduang, S.; Wongsena, M.; Boonsiri, P.; Kiatpathomchai, W.; Swangvaree, S.S.; et al. High sensitivity, loop-mediated isothermal amplification combined with colorimetric gold-nanoparticle probes for visual detection of high risk human papillomavirus genotypes 16 and 18. J. Virol. Methods 2016, 234, 90–95. [Google Scholar] [CrossRef]
- Zhou, C.-H.; Zhao, J.-Y.; Pang, D.W.; Zhang, Z.-L. Enzyme-Induced Metallization as a Signal Amplification Strategy for Highly Sensitive Colorimetric Detection of Avian Influenza Virus Particles. Anal. Chem. 2014, 86, 2752–2759. [Google Scholar] [CrossRef]
- Nikaeen, G.; Abbaszadeh, S.; Yousefinejad, S. Application of nano-materials in treatment, anti-infection and detection of corona viruses. Nanomedicine 2020, 15, 1501–1512. [Google Scholar] [CrossRef]
- Kumar, V.; Mishra, S.; Sharma, R.; Agarwal, J.; Ghoshal, U.; Khanna, T.; Sharma, L.K.; Verma, S.K.; Mishra, P.; Tiwari, S. Development of RNA-based assay for rapid detection of SARS-CoV-2 in clinical samples. Intervirology 2022, 65, 181–187. [Google Scholar] [CrossRef]
- Guo, Y.J.; Deng, L.; Li, J.; Guo, S.J.; Wang, E.K.; Dong, S.J. Hemin-Graphene Hybrid Nanosheets with Intrinsic Peroxidase-like Activity for Label-free Colorimetric Detection of Single-Nucleotide Polymorphism. ACS Nano 2011, 5, 1282–1290. [Google Scholar] [CrossRef]
- Zhu, D.; Liu, B.; Wei, G. Two-Dimensional Material-Based Colorimetric Biosensors: A Review. Biosensors 2021, 11, 259. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Dong, X.; Zhang, K.; Han, X.; Fang, X.; Zhang, Y. A gold nanorods-based fluorescent biosensor for the detection of hepatitis B virus DNA based on fluorescence resonance energy transfer. Analyst 2013, 138, 642–650. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.F.; Pang, D.W.; Zhang, Z.L.; Zheng, H.Z.; Cao, J.P.; Shen, J.T. Visual gene diagnosis of HBV and HCV based on nanoparticle probe amplification and silver staining enhancement. J. Med. Virol. 2003, 70, 205–211. [Google Scholar] [CrossRef]
- Le, T.T.; Chang, P.; Benton, D.J.; McCauley, J.W.; Iqbal, M.; Cass, A.E.G. Dual Recognition Element Lateral Flow Assay Toward Multiplex Strain Specific Influenza Virus Detection. Anal. Chem. 2017, 89, 6781–6786. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Mauk, M.G.; Hackett, B.A.; Cherry, S.; Bau, H.H.; Liu, C. Instrument-Free Point-of-Care Molecular Detection of Zika Virus. Anal. Chem. 2016, 88, 7289–7294. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, M.; Jiang, L.; Cesarman, E.; Erickson, D. Multiplexed colorimetric detection of Kaposi’s sarcoma associated herpesvirus and Bartonella DNA using gold and silver nanoparticles. Nanoscale 2013, 5, 1678–1686. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.; Yeom, G.; Jang, H.; Park, C.-J.; Kim, M.-G. Highly sensitive and universal detection strategy based on a colorimetric assay using target-specific heterogeneous sandwich DNA aptamer. Anal. Chim. Acta 2020, 1123, 73–80. [Google Scholar] [CrossRef]
- Mao, X.; Liu, S.; Yang, C.; Liu, F.; Wang, K.; Chen, G. Colorimetric detection of hepatitis B virus (HBV) DNA based on DNA-templated copper nanoclusters. Anal. Chim. Acta 2016, 909, 101–108. [Google Scholar] [CrossRef]
- Mohammed, A.S.; Balapure, A.; Khaja, M.N.; Ganesan, R.; Dutta, J.R. Naked-eye colorimetric detection of HCV RNA mediated by a 50 UTR-targeted antisense oligonucleotide and plasmonic gold nanoparticles. Analyst 2021, 146, 1569–1578. [Google Scholar] [CrossRef]
- Saleh, M.; El-Matbouli, M. Rapid detection of Cyprinid herpesvirus-3 (CyHV-3) using a gold nanoparticle-based hybridization assay. J. Virol. Methods 2015, 217, 50–54. [Google Scholar] [CrossRef]
- Pan, H.; Zhang, P.; Gao, D.; Zhang, Y.; Li, P.; Liu, L.; Wang, C.; Wang, H.; Ma, Y.; Cai, L. Noninvasive Visualization of Respiratory Viral Infection Using Bioorthogonal Conjugated Near-Infrared-Emitting Quantum Dots. ACS Nano 2014, 8, 5468–5477. [Google Scholar] [CrossRef] [PubMed]
- Weissleder, R.; Ntziachristos, V. Shedding light onto live molecular targets. Nat. Med. 2003, 9, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Kircher, M.F.; Gambhir, S.S.; Grimm, J. Noninvasive cell-tracking methods. Nat. Rev. Clin. Oncol. 2011, 8, 677. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.; Dodani, S.C.; Chang, C.J. Reaction-based small-molecule fluorescent probes for chemoselective bioimaging. Nat. Chem. 2012, 4, 973–984. [Google Scholar] [CrossRef] [PubMed]
- Cotruvo, J.A., Jr.; Aron, A.T.; Ramos-Torres, K.M.; Chang, C.J. Synthetic fluorescent probes for studying copper in biological systems. Chem. Soc. Rev. 2015, 44, 4400–4414. [Google Scholar] [CrossRef]
- Huang, Z.; Liu, S.; Pei, X.; Li, S.; He, Y.; Tong, Y.; Liu, G. Fluorescence Signal-Readout of CRISPR/Cas Biosensors for Nucleic Acid Detection. Biosensors 2022, 12, 779. [Google Scholar] [CrossRef] [PubMed]
- Pang, Y.; Rong, Z.; Wang, J.; Xiao, R.; Wang, S. A fluorescent aptasensor for H5N1 influenza virus detection based-on the core–shell nanoparticles metal-enhanced fluorescence (MEF). Biosens. Bioelectron. 2015, 66, 527–532. [Google Scholar] [CrossRef]
- Qu, H.; Fan, C.; Chen, M.; Zhang, X.; Yan, Q.; Wang, Y.; Zhang, S.; Gong, Z.; Shi, L.; Li, X.; et al. Recent advances of fluorescent biosensors based on cyclic signal amplification technology in biomedical detection. J. Nanobiotechnol. 2021, 19, 403. [Google Scholar] [CrossRef]
- Gnaim, S.; Shabat, D. Activity-Based Optical Sensing Enabled by Self Immolative Scafolds: Monitoring of Release Events by Fluorescence or Chemiluminescence Output. Acc. Chem Res. 2019, 52, 2806–2817. [Google Scholar] [CrossRef]
- Liang, K.; Wang, H.; Li, P.; Zhu, Y.; Liu, J.; Tang, B. Detection of microRNAs using toehold-initiated rolling circle amplification and fluorescence resonance energy transfer. Talanta 2020, 207, 120285. [Google Scholar] [CrossRef]
- Wu, Z.; Zhou, H.; He, J.; Li, M.; Ma, X.; Xue, J.; Li, X.; Fan, X. G-triplex based molecular beacon with duplex-specific nuclease amplification for the specific detection of microRNA. Analyst 2019, 144, 5201–5206. [Google Scholar] [CrossRef]
- Du, M.; Mao, G.; Tian, S.; Liu, Y.; Zheng, J.; Ke, X.; Zheng, Z.; Wang, H.; Ji, X.; He, Z. Target-Induced Cascade Amplification for Homogeneous Virus Detection. Anal. Chem. 2019, 91, 15099–15106. [Google Scholar] [CrossRef] [PubMed]
- Ciftci, S.; Neumann, F.; Abdurahman, S.; Appelberg, K.S.; Mirazimi, A.; Nilsson, M.; Madaboosi, N. Digital Rolling Circle Amplification-Based Detection of Ebola and Other Tropical Viruses. J. Mol. Diagn. 2020, 22, 272–283. [Google Scholar] [CrossRef] [PubMed]
- Wen, J.; Li, W.; Li, J.; Tao, B.; Xu, Y.; Li, H.; Lu, A.; Sun, S. Study on rolling circle amplification of Ebola virus and fluorescence detection based on graphene oxide. Sens. Actuators B Chem. 2016, 227, 655–659. [Google Scholar] [CrossRef]
- Qaddare, S.H.; Salimi, A. Amplified fluorescent sensing of DNA using luminescent carbon dots and AuNPs/GO as a sensing platform: A novel coupling of FRET and DNA hybridization for homogeneous HIV-1 gene detection at femtomolar level. Biosens. Bioelectron. 2017, 89, 773–780. [Google Scholar] [CrossRef]
- Zhang, S.; Wang, K.; Li, K.-B.; Shi, W.; Jia, W.P.; Chen, X.; Sun, T.; Han, D.M. A DNA-stabilized silver nanoclusters/graphene oxide-based platform for the sensitive detection of DNA through hybridization chain reaction. Biosens. Bioelectron. 2017, 91, 374–379. [Google Scholar] [CrossRef]
- Xiao, Y.; Sheng, Y.; Zhou, J.; Chen, M.; Wen, W.; Zhang, X.; Wang, S. A novel label-free strategy for pathogenic DNA detection based on metal ions binding-induced fluorescence quenching of graphitic carbon nitride nanosheets. Analyst 2017, 142, 2617–2623. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Yuan, L.; Liu, Q.; Tong, C. An ultrasensitive and simple assay for the Hepatitis C virus using a reduced graphene oxide-assisted hybridization chain reaction. Analyst 2019, 144, 3972–3979. [Google Scholar] [CrossRef]
- Jeong, S.; Kim, D.; Kim, D.H.; Kim, D. Fluorometric detection of influenza viral RNA using graphene oxide. Anal. Biochem. 2018, 561–562, 66–69. [Google Scholar] [CrossRef]
- Ming, K.; Kim, J.; Biondi, M.J.; Syed, A.; Chen, K.; Lam, A.; Ostrowski, M.; Rebbapragada, A.; Feld, J.J.; Chan, W.C. Integrated quantum dot barcode smartphone optical device for wireless multiplexed diagnosis of infected patients. ACS Nano 2015, 9, 3060–3074. [Google Scholar] [CrossRef]
- Zhang, J.; Tian, J.; He, Y.; Chen, S.; Jiang, Y.; Zhao, Y.; Zhao, S. Protein-binding aptamer assisted signal amplification for the detection of influenza A (H1N1) DNA sequences based on quantum dot fluorescence polarization analysis. Analyst 2013, 138, 4722–4727. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Han, Y.; Wang, C.; Qiang, L.; Gao, J.; Wang, Y.; Liu, H.; Han, L.; Zhang, Y. Rapid and sensitive triple-mode detection of causative SARS-CoV-2 virus specific genes through interaction between genes and nanoparticles. Anal. Chim. Acta 2021, 1154, 338330. [Google Scholar] [CrossRef] [PubMed]
- Luo, S.-C.; Sivashanmugan, K.; Liao, J.-D.; Yao, C.-K.; Peng, H.-C. Nanofabricated SERS-active substrates for single-molecule to virus detection in vitro: A review. Biosens. Bioelectron. 2014, 61, 232–240. [Google Scholar] [CrossRef]
- Neng, J.; Harpster, M.H.; Wilson, W.C.; Johnson, P.A. Surface-enhanced Raman scattering (SERS) detection of multiple viral antigens using magnetic capture of SERS-active nanoparticles. Biosens. Bioelectron. 2013, 41, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Ambartsumyan, Q.; Gribanyov, D.; Kukushkin, V.; Kopylov, A.; Zavyalova, E. SERS-Based Biosensors for Virus Determination with Oligonucleotides as Recognition Elements. Int. J. Mol. Sci. 2020, 21, 3373. [Google Scholar] [CrossRef]
- Damborsky, P.; Svitel, J.; Katrlik, J. Optical biosensors. Essays Biochem. 2016, 60, 91–100. [Google Scholar]
- Lee, T.; Kim, G.H.; Kim, S.M.; Hong, K.; Kim, Y.; Park, C.; Sohn, H.; Min, J. Label-free localized surface plasmon resonance biosensor composed of multi-functional DNA 3 way junction on hollow Au spike-like nanoparticles (HAuSN) for avian influenza virus detection. Colloids Surf. B 2019, 182, 110341. [Google Scholar] [CrossRef]
- Qiu, G.; Gai, Z.; Tao, Y.; Schmitt, J.; Kullak-Ublick, G.A.; Wang, J. Dual-functional plasmonic photothermal biosensors for highly accurate severe acute respiratory syndrome coronavirus 2 detection. ACS Nano 2020, 14, 5268–5277. [Google Scholar] [CrossRef]
- Park, J.-H.; Cho, Y.-W.; Kim, T.-H. Recent Advances in Surface Plasmon Resonance Sensors for Sensitive Optical Detection of Pathogens. Biosensors 2022, 12, 180. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.A.; Kim, S.J. Detection of avian influenza-DNA hybridization using wavelength-scanning surface plasmon resonance biosensor. J. Opt. Soc. Korea 2009, 13, 392–397. [Google Scholar] [CrossRef]
- Shin, W.-R.; Sekhon, S.S.; Rhee, S.-K.; Ko, J.H.; Ahn, J.-Y.; Min, J.; Kim, Y.-H. Aptamer-Based Paper Strip Sensor for Detecting Vibrio fischeri. ACS Comb. Sci. 2018, 20, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Pang, Y.; Wang, J.; Xiao, R.; Wang, S. SERS molecular sentinel for the RNA genetic marker of PB1-F2 protein in highly pathogenic avian influenza (HPAI) virus. Biosens. Bioelectron. 2014, 61, 460–464. [Google Scholar] [CrossRef] [PubMed]
- Kukushkin, V.I.; Ivanov, N.M.; Novoseltseva, A.A.; Gambaryan, A.S.; Yaminsky, I.V.; Kopylov, A.M.; Zavyalova, E.G. Highly sensitive detection of influenza virus with SERS aptasensor. PLoS ONE 2019, 14, e0216247. [Google Scholar] [CrossRef] [PubMed]
- Zengin, A.; Tamer, U.; Caykara, T. SERS detection of hepatitis B virus DNA in a temperature-responsive sandwich-hybridization assay: SERS detection of HBV DNA. J. Raman Spectrosc. 2017, 48, 668–672. [Google Scholar] [CrossRef]
- Chuang, C.-S.; Wu, C.-Y.; Juan, P.-H.; Hou, N.-C.; Fan, Y.-J.; Wei, P.-K.; Sheen, H.-J. LMP1 gene detection using a capped gold nanowire array surface plasmon resonance sensor in a microfluidic chip. Analyst 2020, 145, 52–60. [Google Scholar] [CrossRef]
- Vázquez-Guardado, A.; Mehta, F.; Jimenez, B.; Biswas, A.; Ray, K.; Baksh, A.; Lee, S.; Saraf, N.; Seal, S.; Chanda, D. DNA Modified Plasmonic Sensor for the Direct Detection of Virus Biomarkers from the Blood. Nano Lett. 2021, 21, 7505–7511. [Google Scholar] [CrossRef]
- Liu, Y.; Huang, C.Z. One-step conjugation chemistry of DNA with highly scattered silver nanoparticles for sandwich detection of DNA. Analyst 2012, 137, 3434–3436. [Google Scholar] [CrossRef]
- Bai, H.; Wang, R.; Hargis, B.; Lu, H.; Li, Y. A SPR aptasensor for detection of avian influenza virus H5N1. Sensors 2012, 12, 12506–12518. [Google Scholar] [CrossRef]
- Biagetti, M.; Cuccioloni, M.; Bonfili, L.; Cecarini, V.; Sebastiani, C.; Curcio, L.; Giammarioli, M.; De Mia, G.M.; Eleuteri, A.M.; Angeletti, M. Chimeric DNA/LNA-based biosensor for the rapid detection of African swine fever virus. Talanta 2018, 184, 35–41. [Google Scholar] [CrossRef]
- Manzano, M. Labelled and unlabelled probes for pathogen detection with molecular biology methods and biosensors. Methods Microbiol. 2021, 48, 179–225. [Google Scholar]
- Malhotra, B.D.; Ali, M.A. Plasmonic nanostructures: Fiber-optic biosensors. In Nanomaterials for Biosensors: Fundamentals and Applications; Elsevier: Amsterdam, The Netherlands, 2018; pp. 161–181. [Google Scholar]
- Hutchinson, A.M. Evanescent wave biosensors. Mol. Biotechnol. 1995, 3, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Taitt, C.R.; Anderson, G.P.; Ligler, F.S. Evanescent wave fluorescence biosensors. Biosens. Bioelectron. 2005, 20, 2470–2487. [Google Scholar] [CrossRef] [PubMed]
- Linuma, M.; Tanaka, R.; Takahama, E.; Ikeda, T.; Kadoya, Y.; Kuroda, A. Investigation of bioluminescence at an optical fiber end for a high-sensitive ATP detection system. In Current Developments in Optical Fiber Technology; InTech: Rijeka, Croatia, 2013; pp. 293–317. [Google Scholar]
| Material | Virus/Disease | Recognition Element | Dynamic Range | LOD | Real Sample | Reference |
|---|---|---|---|---|---|---|
| AuNPs | Dengue | PNA | 0–12 µM | 0.12 µM | - | [57] |
| AgNPs | MERS-CoV, HPV | PNA | 20–1000 nM (MERS-CoV), 20–2500 nM (HPV) | 1.53 nM (MERS-CoV), | - | [59] |
| AuNPs | HPV genotype 16 and 18 | DNA probe | 105 to 100 copies | 102 (HPV 16) and 101 (HPV 18) | clinical cervical tissue specimens | [62] |
| AuNRs | HBV | DNA | 0.045 to 6.0 nM | 15 pM | Human blood | [68] |
| AuNPs | HBV, HCV | DNA | - | HBV: 3.6 × 104 fM; HCV: 3.6 × 105 fM | Serum | [69] |
| AuNPs | Influenza | aptamer | - | 2 × 106 copies/mL | - | [70] |
| Zika virus | Nucleic acids | - | 5 PFU/mL | Saliva | [71] | |
| AuNPs, AgNPs | Herpesvirus | DNA | 10 pM–1 µM | 1 nM | - | [72] |
| Influenza A and B virus | aptamer | 0.1 pg/mL– 1 mg/mL | 0.30 pg/mL, 0.16 pg/mL | Patient samples | [73] | |
| Copper nanoclusters | HBV | DNA | 12 × 109 to 12 × 1013 molecules | 12 × 109 molecules | Human serum | [74] |
| AuNPs | HCV | oligonucleotides | 7.50 × 102 to 2.00 × 106 IU/mL | 100 IU/mL (0.4 IU/µL) | Human blood | [75] |
| AuNPs | Cyprinid herpesvirus-3 (CyHV-3) | DNA | 100 ng/µL to 0.1 fg/µL | 10 fg CyHV-3-AuNP DNA (30 virions) | Infected fish tissues | [76] |
| Material | Virus/Disease | Recognition Element | Dynamic Range | LOD | Real Sample | Reference |
|---|---|---|---|---|---|---|
| AuNRs | HBV | ssDNA | 0.045 to 6.0 nM | 15 pM | Human blood | [68] |
| Ag@SiO2 nanoparticles | H5N1 influenza virus | aptamer | 2 to 200 ng/mL (in buffer) 3.5 to 100 ng/mL (in serum) | 2 ng/mL (in buffer) 3.5 ng/mL (in serum) | Human serum | [83] |
| GO | Ebola virus gene influenza | dsDNA | 30 fM–3 nM | 1.4 pM | Human serum | [90] |
| AuNPs-GO | HIV-1 gene | dsDNA | 50 fM–1 nM | 15 fM | Human serum | [91] |
| AgNCs/GO | HIV | dsDNA | 10–200 nM | 1.18 nM | Human serum | [92] |
| g-C3N4 Graphitic carbon nitride (gC3N4) nanosheets | HBV gene | DNA | 2–100 nM | 1 nM | Human serum | [93] |
| rGONs | HCV | dsDNA | - | 10 fM | Human serum | [94] |
| GO | Influenza virus H3N2 Henagglutinin gene | RNA | 37–9400 pg | 3.8 pg | - | [95] |
| QDs | HIV, HBV | DNA | 103 to 109 copies/mL | 1 × 103 copies/mL | Human serum | [96] |
| QDs | Influenza (H1N1) | aptamer | 10 nM–100 nM | 3.45 nM | - | [97] |
| AuNPs | SARS-CoV-2 | DNA | 0.01–1 pM | 160 fM | - | [98] |
| Technique | Material | Virus/Disease | Recognition Element | Dynamic Range | LOD | Real Sample | Reference |
|---|---|---|---|---|---|---|---|
| SERS | Au-Gr film | Influenza | Hairpin DNA probe | 0–60 amole | 2.67 amole | - | [108] |
| SERS | - | Influenza | aptamer | - | 104 virus particles per sample | - | [109] |
| SERS | AuNPs | HBV | oligonucleotide | 0.01 fM–6 µM | 0.14 fM | serum | [110] |
| SPR | - | Epstein-Barr virus (LMP1 DNA) | LMP1 DNA probe | - | 4.1 × 10−5 RIU | - | [111] |
| SPR | Au-Al bilayer | Dengue virus (NS1 protein) | DNA | 0.1–10 µg/mL | - | Bovine whole blood | [112] |
| SPR | AgNPs | HIV | DNA | 0.3–2.0 nM | 195 pM | - | [113] |
| SPR | - | Avian influenza H5N1 | aptamer | 0.128 to 1.28 HAU | 0.128 HAU | poultry swab samples | [114] |
| SPR | - | African swine fever (ASF) virus vp72 gene | ssDNA/LNA probe | 0–15,000 copies/μL | 178 copies/µL | Pig blood | [115] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eksin, E.; Erdem, A. Recent Progress on Optical Biosensors Developed for Nucleic Acid Detection Related to Infectious Viral Diseases. Micromachines 2023, 14, 295. https://doi.org/10.3390/mi14020295
Eksin E, Erdem A. Recent Progress on Optical Biosensors Developed for Nucleic Acid Detection Related to Infectious Viral Diseases. Micromachines. 2023; 14(2):295. https://doi.org/10.3390/mi14020295
Chicago/Turabian StyleEksin, Ece, and Arzum Erdem. 2023. "Recent Progress on Optical Biosensors Developed for Nucleic Acid Detection Related to Infectious Viral Diseases" Micromachines 14, no. 2: 295. https://doi.org/10.3390/mi14020295
APA StyleEksin, E., & Erdem, A. (2023). Recent Progress on Optical Biosensors Developed for Nucleic Acid Detection Related to Infectious Viral Diseases. Micromachines, 14(2), 295. https://doi.org/10.3390/mi14020295