Modeling of Endothelial Calcium Responses within a Microfluidic Generator of Spatio-Temporal ATP and Shear Stress Signals
Abstract
1. Introduction
2. Mathematical Methods
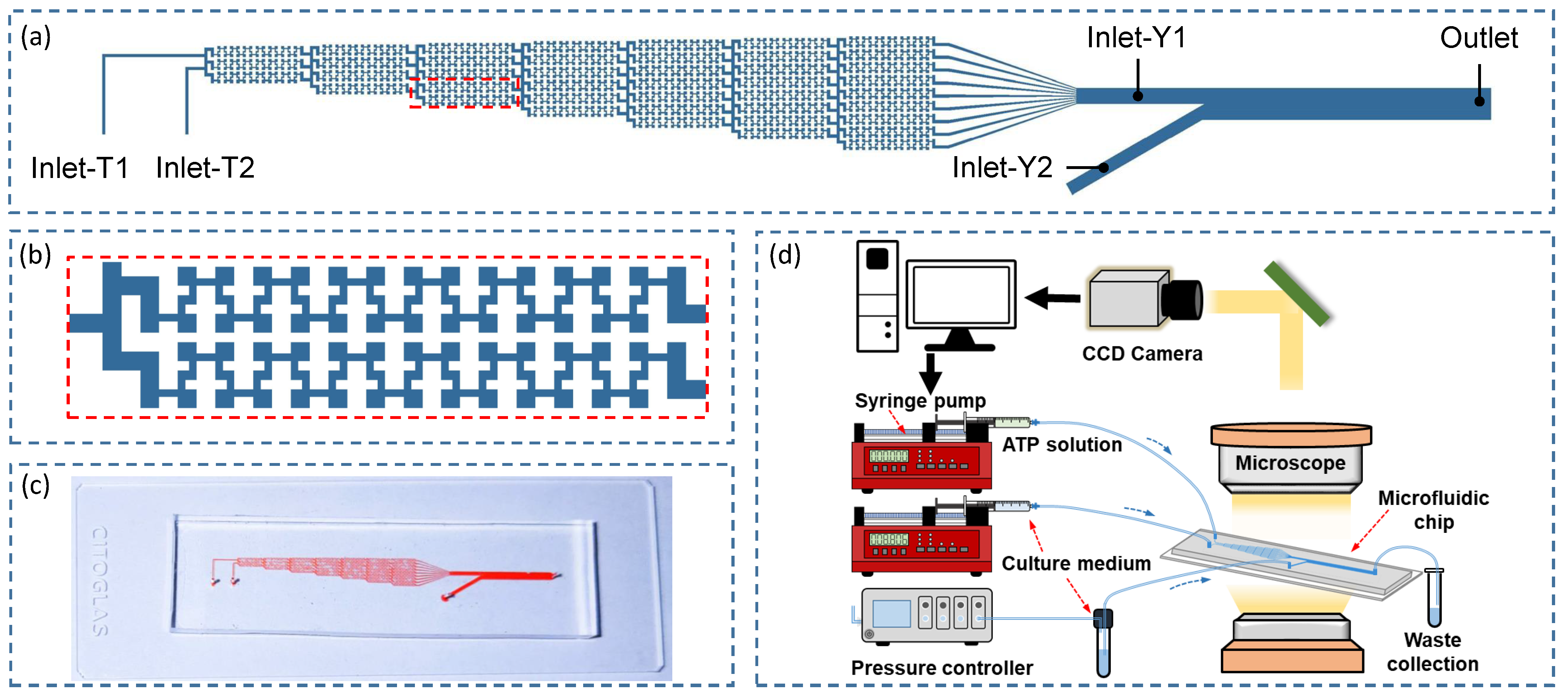
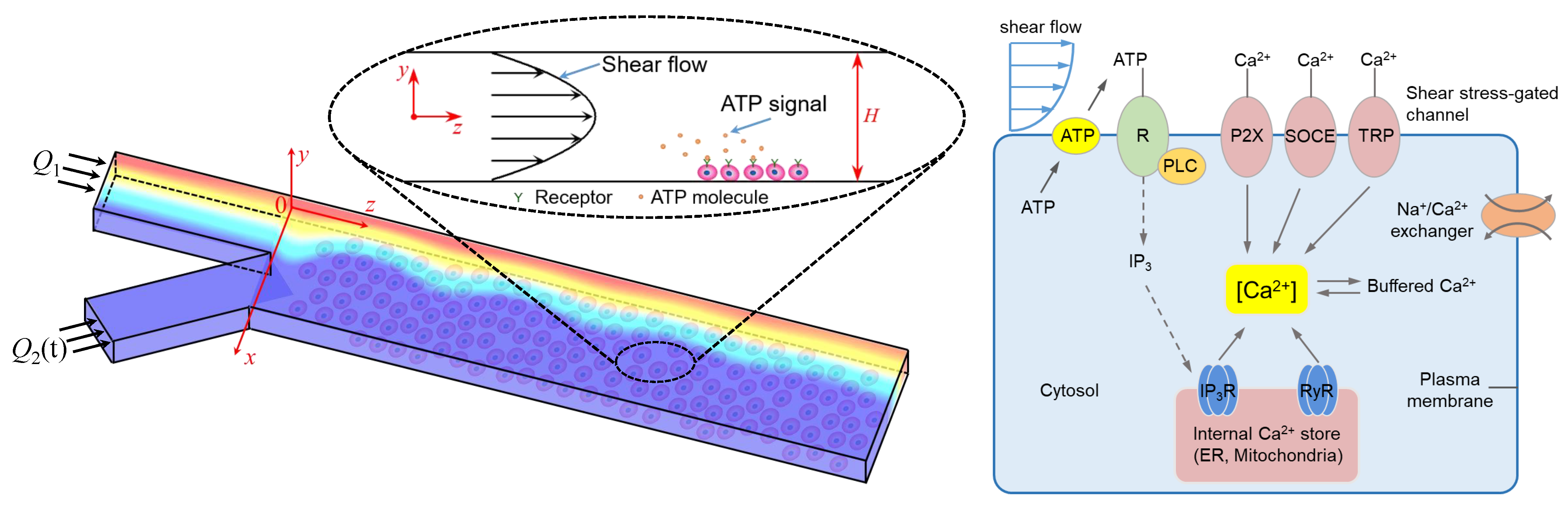
2.1. Microfluidic Chip and Model Development
2.2. Mathematical Modeling
2.2.1. Sub-Model of Extracellular ATP Transport
2.2.2. Sub-Model of Intracellular Calcium Dynamics
2.2.3. Model Parameters and Simulation Methods
3. Results
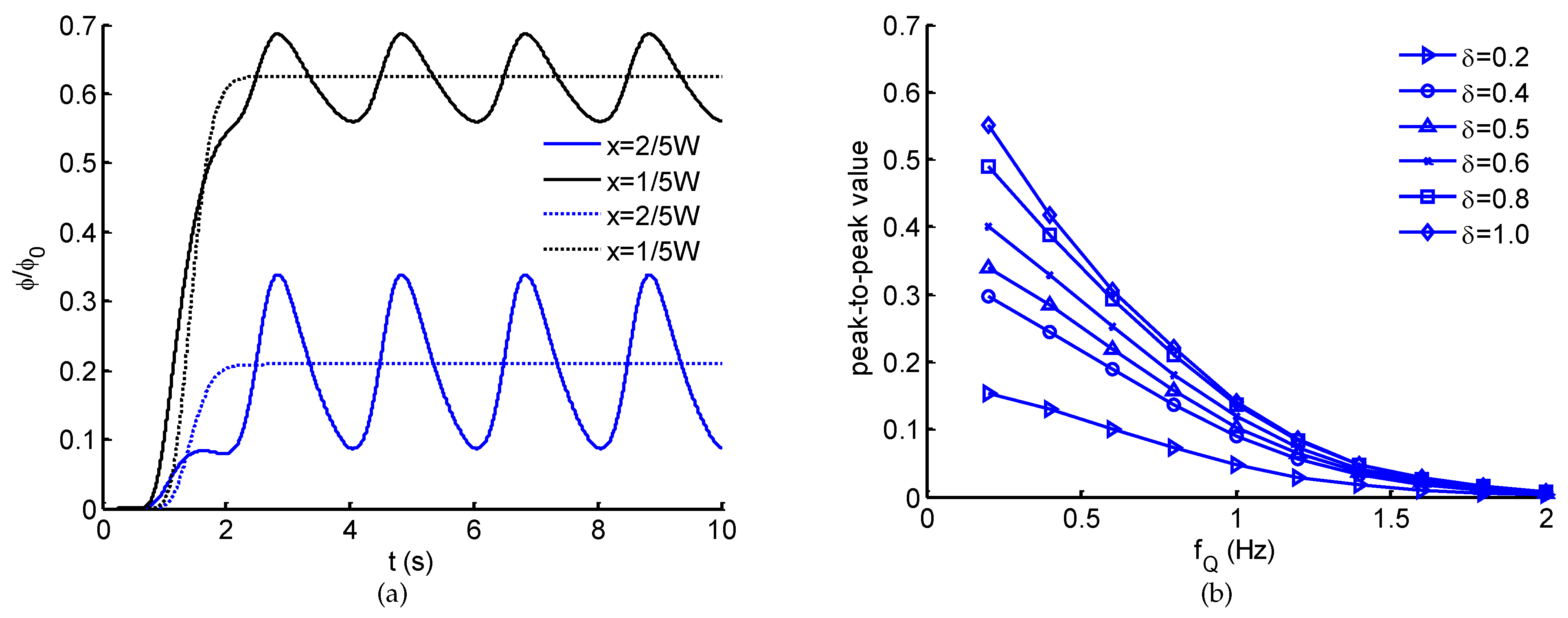
3.1. Generation and Transport of ATP Signals
3.2. Model Validation of Calcium Dynamics
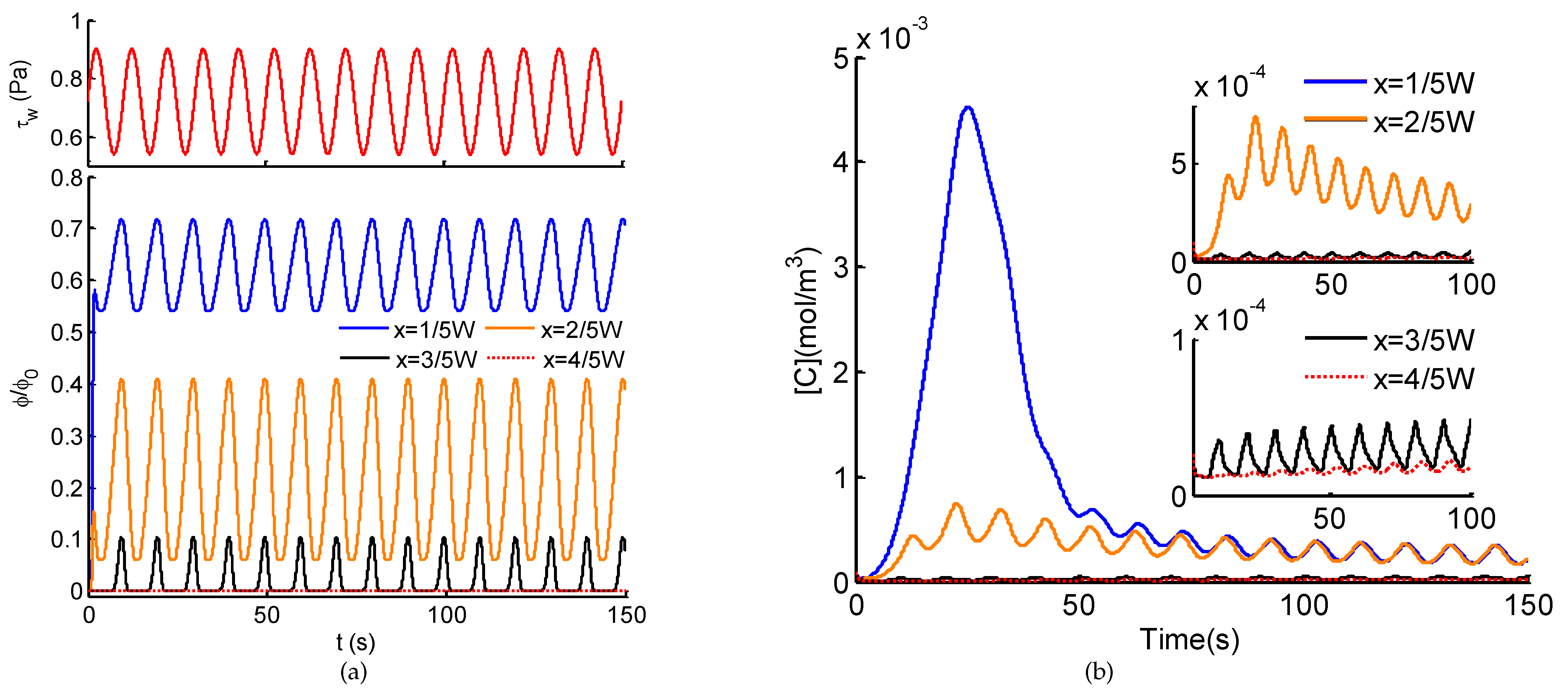
3.3. Ca2+ Dynamics Regulated by Spatio-Temporal ATP and Shear Stress Stimuli
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Giorgi, C.; Danese, A.; Missiroli, S.; Patergnani, S.; Pinton, P. Calcium Dynamics as a Machine for Decoding Signals. Trends Cell Biol. 2018, 28, 258–273. [Google Scholar] [CrossRef] [PubMed]
- Berridge, M.J.; Bootman, M.D.; Lipp, P. Calcium-a life and death signal. Nature 1998, 395, 645–648. [Google Scholar] [CrossRef]
- Berridge, M.J.; Bootman, M.D.; Roderick, H.L. Calcium signalling: Dynamics, homeostasis and remodelling. Nat. Rev. Mol. Cell Biol. 2003, 4, 517–529. [Google Scholar] [CrossRef] [PubMed]
- Rizzuto, R.; Pozzan, T. Microdomains of intracellular Ca2+: Molecular determinants and functional consequences. Physiol. Rev. 2006, 86, 369–408. [Google Scholar] [CrossRef]
- Dupont, G.; Combettes, L.; Leybaert, L. Calcium dynamics: Spatiotemporal organization from the subcellular to the organ level. Int. Rev. Cytol. 2007, 261, 193–245. [Google Scholar]
- Paupe, V.; Prudent, J. New insights into the role of mitochondrial calcium homeostasis in cell migration. Biochem. Biophys. Res. Commun. 2018, 500, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Rutter, G.A.; Hodson, D.J.; Chabosseau, P.; Haythorne, E.; Pullen, T.J.; Leclerc, I. Local and regional control of calcium dynamics in the pancreatic islet. Diabetes Obes. Metab. 2017, 19, 30–41. [Google Scholar] [CrossRef]
- Hoang-Trong, T.M.; Ullah, A.; Jafri, M.S. Calcium sparks in the heart: Dynamics and regulation. Res. Rep. Biol. 2015, 6, 203–214. [Google Scholar]
- Borrachero-Conejo, A.I.; Adams, W.R.; Saracino, E.; Mola, M.G.; Wang, M.Q.; Posati, T.; Formaggio, F.; De Bellis, M.; Frigeri, A.; Caprini, M.; et al. Stimulation of water and calcium dynamics in astrocytes with pulsed infrared light. FASEB J. 2020, 34, 6539–6553. [Google Scholar] [CrossRef]
- Tang, X.Q.; Luo, Y.X.; Chen, H.Z.; Liu, D.P. Mitochondria, endothelial cell function, and vascular diseases. Front. Physiol. 2014, 5, 175. [Google Scholar] [CrossRef] [PubMed]
- Huang, P.H.; Chan, C.Y.; Li, P.; Wang, Y.Q.; Nama, N.; Bachman, H.; Huang, T.J. A sharp-edge-based acoustofluidic chemical signal generator. Lab Chip 2018, 18, 1411–1421. [Google Scholar] [CrossRef]
- Marchi, S.; Pinton, P. Alterations of calcium homeostasis in cancer cells. Curr. Opin. Pharmacol. 2016, 29, 1–6. [Google Scholar] [CrossRef] [PubMed]
- O’Hayre, M.; Salanga, C.L.; Handel, T.M.; Allen, S.J. Chemokines and cancer: Migration, intracellular signalling and intercellular communication in the microenvironment. Biochem. J. 2008, 409, 635–649. [Google Scholar] [CrossRef] [PubMed]
- White, C.R.; Haidekker, M.; Bao, X.; Frangos, J.A. Temporal Gradients in Shear, but Not Spatial Gradients, Stimulate Endothelial Cell Proliferation. Circulation 2001, 103, 2508–2513. [Google Scholar] [CrossRef]
- Noren, D.P.; Chou, W.H.; Lee, S.H.; Qutub, A.A.; Warmflash, A.; Wagner, D.S.; Popel, A.S.; Levchenko, A. Endothelial cells decode VEGF-mediated Ca2+ signaling patterns to produce distinct functional responses. Sci. Signal. 2016, 9, ra20. [Google Scholar] [CrossRef] [PubMed]
- Munaron, L. Intracellular calcium, endothelial cells and angiogenesis. Recent Patents Anti-Cancer Drug Discov. 2006, 1, 105–119. [Google Scholar] [CrossRef] [PubMed]
- Munaron, L.; Scianna, M. Multilevel complexity of calcium signaling: Modeling angiogenesis. World J. Biol. Chem. 2012, 3, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Savage, A.M.; Kurusamy, S.; Chen, Y.; Jiang, Z.; Chhabria, K.; MacDonald, R.B.; Kim, H.R.; Wilson, H.L.; van Eeden, F.J.M.; Armesilla, A.L.; et al. tmem33 is essential for VEGF-mediated endothelial calcium oscillations and angiogenesis. Nat. Commun. 2019, 10, 732. [Google Scholar] [CrossRef]
- Moccia, F.; Negri, S.; Shekha, M.; Faris, P.; Guerra, G. Endothelial Ca2+ Signaling, Angiogenesis and Vasculogenesis: Just What It Takes to Make a Blood Vessel. Int. J. Mol. Sci. 2019, 20, 3962. [Google Scholar] [CrossRef] [PubMed]
- Brossa, A.; Buono, L.; Fallo, S.; Fiorio Pla, A.; Munaron, L.; Bussolati, B. Alternative Strategies to Inhibit Tumor Vascularization. Int. J. Mol. Sci. 2019, 20, 6180. [Google Scholar] [CrossRef] [PubMed]
- Moccia, F. Endothelial Ca2+ Signaling and the Resistance to Anticancer Treatments: Partners in Crime. Int. J. Mol. Sci. 2018, 19, 217. [Google Scholar] [CrossRef]
- Kou, S.Z.; Pan, L.T.; van Noort, D.; Meng, G.X.; Wu, X.; Sun, H.Y.; Xu, J.J.; Lee, I. A multishear microfluidic device for quantitative analysis of calcium dynamics in osteoblasts. Biochem. Biophys. Res. Commun. 2011, 408, 350–355. [Google Scholar] [CrossRef]
- Park, S.H.; Shin, J.W.; Kim, D.W.; Kim, S.H.; Jeong, O.C.; Kim, J.K.; Shin, J.W. Quantitative analyses of changes in intracellular calcium ion concentrations under flow-induced mechanical stimuli utilising a microchip. Micro Nano Lett. 2011, 6, 296–300. [Google Scholar] [CrossRef]
- Chen, P.; Feng, X.; Chen, D.; Liu, C.; Du, W.; Liu, B.F. Investigating intercellular calcium waves by microfluidic gated pinched-flow. Sens. Actuators B Chem. 2016, 234, 583–592. [Google Scholar] [CrossRef]
- Chen, P.; Guo, Y.R.; Feng, X.J.; Yan, S.Q.; Wang, J.; Li, Y.W.; Liu, B.F. A microfluidic chemical function generator for probing dynamic cell signaling. Anal. Chem. 2017, 89, 9209–9217. [Google Scholar] [CrossRef]
- Lembong, J.; Sabass, B.; Sun, B.; Rogers, M.E.; Stone, H.A. Mechanics regulates ATP-stimulated collective calcium response in fibroblast cells. J. R. Soc. Interface 2015, 12, 20150140. [Google Scholar] [CrossRef] [PubMed]
- Roy, B.; Das, T.; Mishra, D.; Maiti, T.K.; Chakraborty, S. Oscillatory shear stress induced calcium flickers in osteoblast cells. Integr. Biol. 2014, 6, 289–299. [Google Scholar] [CrossRef]
- Pessina, G.P.; Aldinucci, C.; Palmi, M.; Sgaragli, G.; Benocci, A.; Meini, A.; Pessina, F. Pulsed electromagnetic fields affect the intracellular calcium concentrations in human astrocytoma cells. Bioelectromagnetics 2001, 22, 503–510. [Google Scholar] [CrossRef]
- Yamamoto, K.; Sokabe, T.; Ohura, N.; Nakatsuka, H.; Kamiya, A.; Ando, J. Endogenously released ATP mediates shear stress-induced Ca2+ influx into pulmonary artery endothelial cells. Am. J. Physiol. Heart Circ. Physiol. 2003, 285, H793–H803. [Google Scholar] [CrossRef] [PubMed]
- Jafarnejad, M.; Cromer, W.E.; Kaunas, R.R.; Zhang, S.L.; Zawieja, D.C.; Moore, J.E. Measurement of shear stress-mediated intracellular calcium dynamics in human dermal lymphatic endothelial cells. Am. J. Physiol. Heart Circ. Physiol. 2015, 308, H697–H706. [Google Scholar] [CrossRef]
- Jovic, A.; Wade, S.M.; Neubig, R.R.; Linderman, J.J.; Takayama, S. Microfluidic interrogation and mathematical modeling of multi-regime calcium signaling dynamics. Integr. Biol. 2013, 5, 932–939. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Li, Y.J.; Li, Y.Z.; Cao, T.; Qin, K.R. Transport of Dynamic Biochemical Signals in Steady Flow in a Shallow Y-shaped Microfluidic Channel: Effect of Transverse Diffusion and Longitudinal Dispersion. ASME J. Biomech. Eng. 2013, 135, 121011. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.J.; Cao, T.; Qin, K.R. Transmission of Dynamic Biochemical Signals in the Shallow Microfluidic Channel: Nonlinear Modulation of the Pulsatile Flow. Microfluid. Nanofluid. 2018, 22, 81. [Google Scholar] [CrossRef]
- Jovic, A.; Howell, B.; Cote, M.; Wade, S.M.; Mehta, K.; Miyawaki, A.; Neubig, R.R.; Linderman, J.J.; Takayama, S. Phase-Locked Signals Elucidate Circuit Architecture of an Oscillatory Pathway. PLoS Comput. Biol. 2010, 6, e1001040. [Google Scholar] [CrossRef] [PubMed]
- Schuster, S.; Marhl, M.; Hofer, T. Modelling of simple and complex calcium oscillations—From single-cell responses to intercellular signalling. Eur. J. Biochem. 2002, 256, 1333–1355. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.Q.; Xiang, C.; Cao, L.L.; Xu, Z.; Qin, K.R. A mathematical model for ATP-mediated calcium, dynamics in vascular endothelial cells induced by fluid shear stress. Appl. Math. Mech. 2008, 29, 1291–1298. [Google Scholar] [CrossRef]
- Qin, K.R.; Xiang, C.; Xu, Z.; Cao, L.L.; Ge, S.S.; Jiang, Z.L. Dynamic modeling for shear stress induced ATP release from vascular endothelial cells. Biomech. Model. Mechanobiol. 2008, 7, 345–353. [Google Scholar] [CrossRef]
- Li, L.F.; Xiang, C.; Qin, K.R. Modeling of TRPV4-C1-mediated calcium signaling in vascular endothelial cells induced by fluid shear stress and ATP. Biomech. Model. Mechanobiol. 2015, 14, 979–993. [Google Scholar] [CrossRef]
- Wiesner, T.F.; Berk, B.C.; Nerem, R.M. A mathematical model of cytosolic calcium dynamics in human umbilical vein endothelial cells. Am. J. Physiol. 1996, 270, C1556–C1569. [Google Scholar] [CrossRef]
- Wiesner, T.F.; Berk, B.C.; Nerem, R.M. A mathematical model of the cytosolic-free calcium response in endothelial cells to fluid shear stress. Proc. Natl. Acad. Sci. USA 1997, 94, 3726–3731. [Google Scholar] [CrossRef]
- Wang, J.H.; Huang, X.D.; Huang, W.D. A quantitative kinetic model for ATP-induced intracellular Ca2+ oscillations. J. Theor. Biol. 2007, 245, 510–519. [Google Scholar] [CrossRef]
- Maurya, M.R.; Subramaniam, S. Kinetic model for calcium dynamics in RAW 264.7 cells: 1. Mechanisms, parameters, and subpopulational variability. Biophys. J. 2007, 93, 709–728. [Google Scholar] [CrossRef] [PubMed]
- Maurya, M.R.; Subramaniam, S. Kinetic model for calcium dynamics in RAW 264.7 cells: 2. Knockdown response and long-term response. Biophys. J. 2007, 93, 729–740. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gerhold, K.A.; Schwartz, M.A. Ion Channels in Endothelial Responses to Fluid Shear Stress. Physiology 2016, 31, 359–369. [Google Scholar] [CrossRef]
- Xue, C.D.; Li, Y.J.; Na, J.T.; Wang, Y.X.; Yu, H.J.; Liu, B.; Cao, T.; Qin, K.R. A microfluidic platform enabling real-time control of dynamic biochemical stimuli to biological cells. J. Micromech. Microeng. 2020, 30, 095011. [Google Scholar] [CrossRef]
- Na, J.T.; Xue, C.D.; Li, Y.J.; Wang, Y.; Liu, B.; Qin, K.R. Precise generation of dynamic biochemical signals by controlling the programmable pump in a Y-shaped microfluidic chip with a “christmas tree” inlet. Electrophoresis 2020, 41, 883–890. [Google Scholar] [CrossRef]
- Dertinger, S.K.W.; Chiu, D.T.; Jeon, N.L.; Whitesides, G.M. Generation of gradients having complex shapes using microfluidic networks. Anal. Chem. 2001, 73, 1240–1246. [Google Scholar] [CrossRef]
- Kuczenski, B.; Ruder, W.C.; Messner, W.C.; LeDuc, P.R. Probing Cellular Dynamics with a Chemical Signal Generator. PLoS ONE 2009, 4, e4847. [Google Scholar] [CrossRef]
- Kim, Y.; Joshi, S.D.; Messner, W.C.; LeDuc, P.R.; Davidson, L.A. Detection of Dynamic Spatiotemporal Response to Periodic Chemical Stimulation in a Xenopus Embryonic Tissue. PLoS ONE 2011, 6, e14624. [Google Scholar] [CrossRef]
- Wang, Y.X.; Xiang, C.; Liu, B.; Zhu, Y.; Luan, Y.; Liu, S.T.; Qin, K.R. A multi-component parallel-plate flow chamber system for studying the effect of exercise-induced wall shear stress on endothelial cells. Biomed. Eng. Online 2016, 15, 154. [Google Scholar] [CrossRef] [PubMed]
- Plank, M.J.; Wall, D.J.N.; David, T. Atherosclerosis and calcium signalling in endothelial cells. Prog. Biophys. Mol. Biol. 2006, 91, 287–313. [Google Scholar] [CrossRef] [PubMed]
- Handy, G.; Taheri, M.; White, J.A.; Borisyuk, A. Mathematical investigation of IP3-dependent calcium dynamics in astrocytes. J. Comput. Neurosci. 2017, 42, 257–273. [Google Scholar] [CrossRef] [PubMed]




| Parameters | Values |
|---|---|
| L | 1 × 10−2 m |
| H | 1 × 10−3 m |
| W | 5 × 10−5 m |
| D | 5 × 10−10 m2/s |
| 1.5 × 10−10 m3/s | |
| 1 × 10−3 Pa·s | |
| 10 μM |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.-J.; Yu, M.; Xue, C.-D.; Zhang, H.-J.; Wang, G.-Z.; Chen, X.-M.; Qin, K.-R. Modeling of Endothelial Calcium Responses within a Microfluidic Generator of Spatio-Temporal ATP and Shear Stress Signals. Micromachines 2021, 12, 161. https://doi.org/10.3390/mi12020161
Li Y-J, Yu M, Xue C-D, Zhang H-J, Wang G-Z, Chen X-M, Qin K-R. Modeling of Endothelial Calcium Responses within a Microfluidic Generator of Spatio-Temporal ATP and Shear Stress Signals. Micromachines. 2021; 12(2):161. https://doi.org/10.3390/mi12020161
Chicago/Turabian StyleLi, Yong-Jiang, Miao Yu, Chun-Dong Xue, Hai-Jun Zhang, Guo-Zhen Wang, Xiao-Ming Chen, and Kai-Rong Qin. 2021. "Modeling of Endothelial Calcium Responses within a Microfluidic Generator of Spatio-Temporal ATP and Shear Stress Signals" Micromachines 12, no. 2: 161. https://doi.org/10.3390/mi12020161
APA StyleLi, Y.-J., Yu, M., Xue, C.-D., Zhang, H.-J., Wang, G.-Z., Chen, X.-M., & Qin, K.-R. (2021). Modeling of Endothelial Calcium Responses within a Microfluidic Generator of Spatio-Temporal ATP and Shear Stress Signals. Micromachines, 12(2), 161. https://doi.org/10.3390/mi12020161







