Diminished but Not Abolished Effect of Two His351 Mutants of Anthrax Edema Factor in a Murine Model
Abstract
:1. Introduction
2. Results and Discussion
2.1. Site-Directed Mutagenesis, Expression, and Purification of Mutant EF Proteins

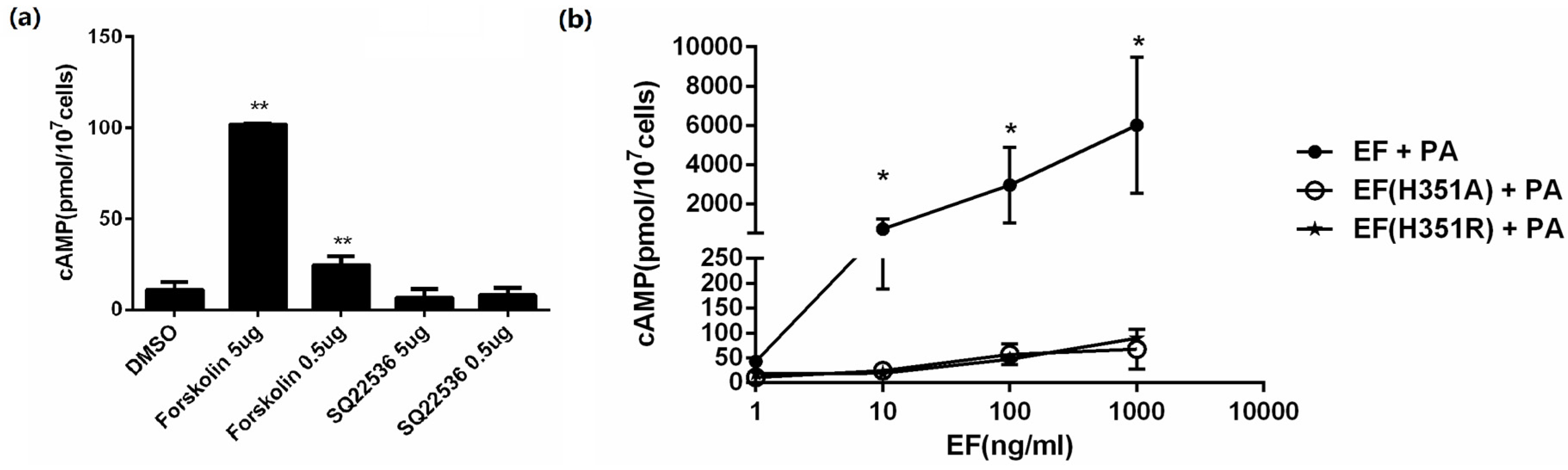
2.2. Adenylate Cyclase Activity of Wild-Type and Mutant Proteins
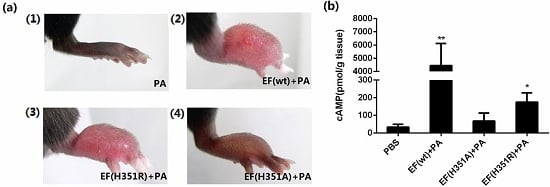
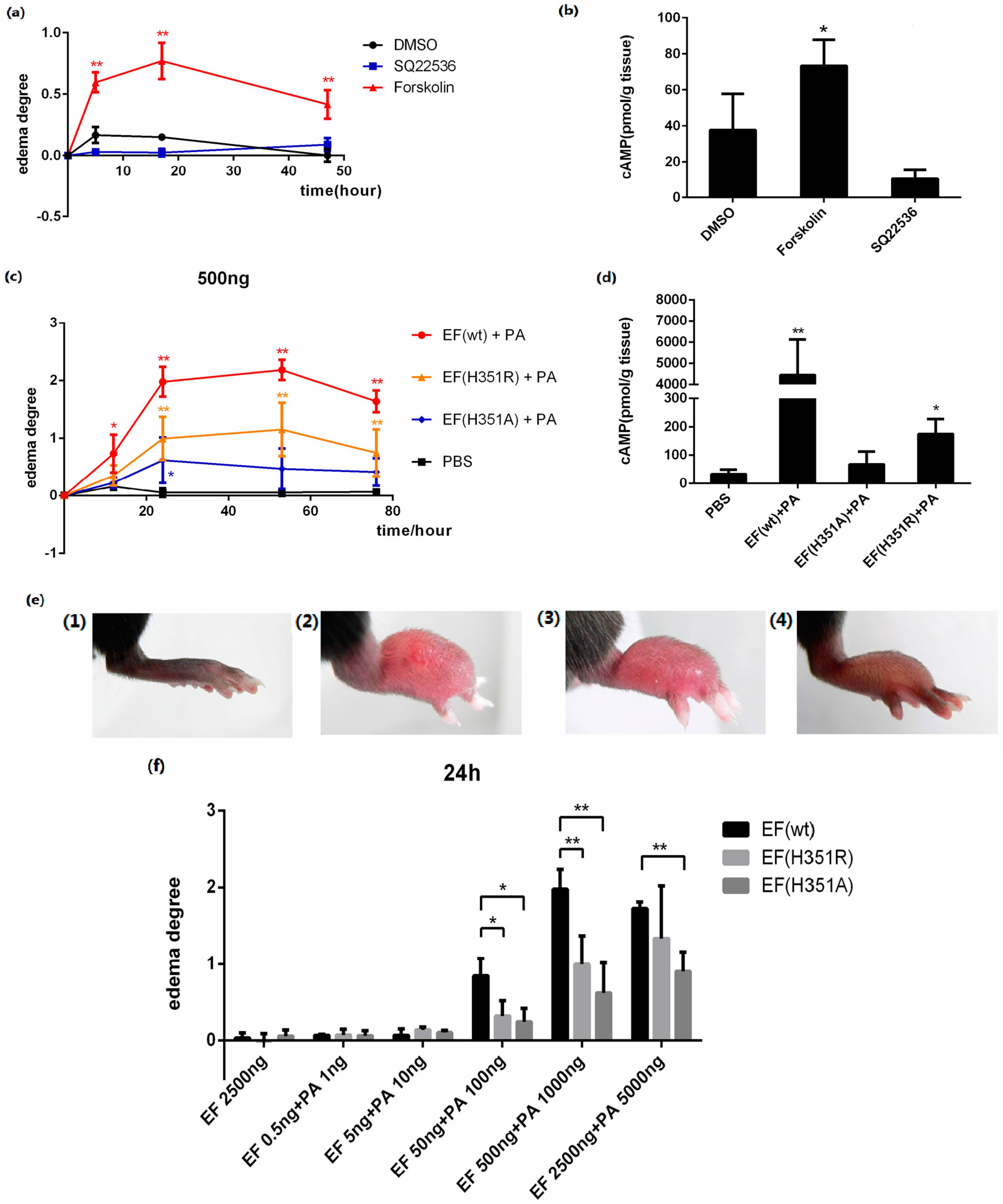
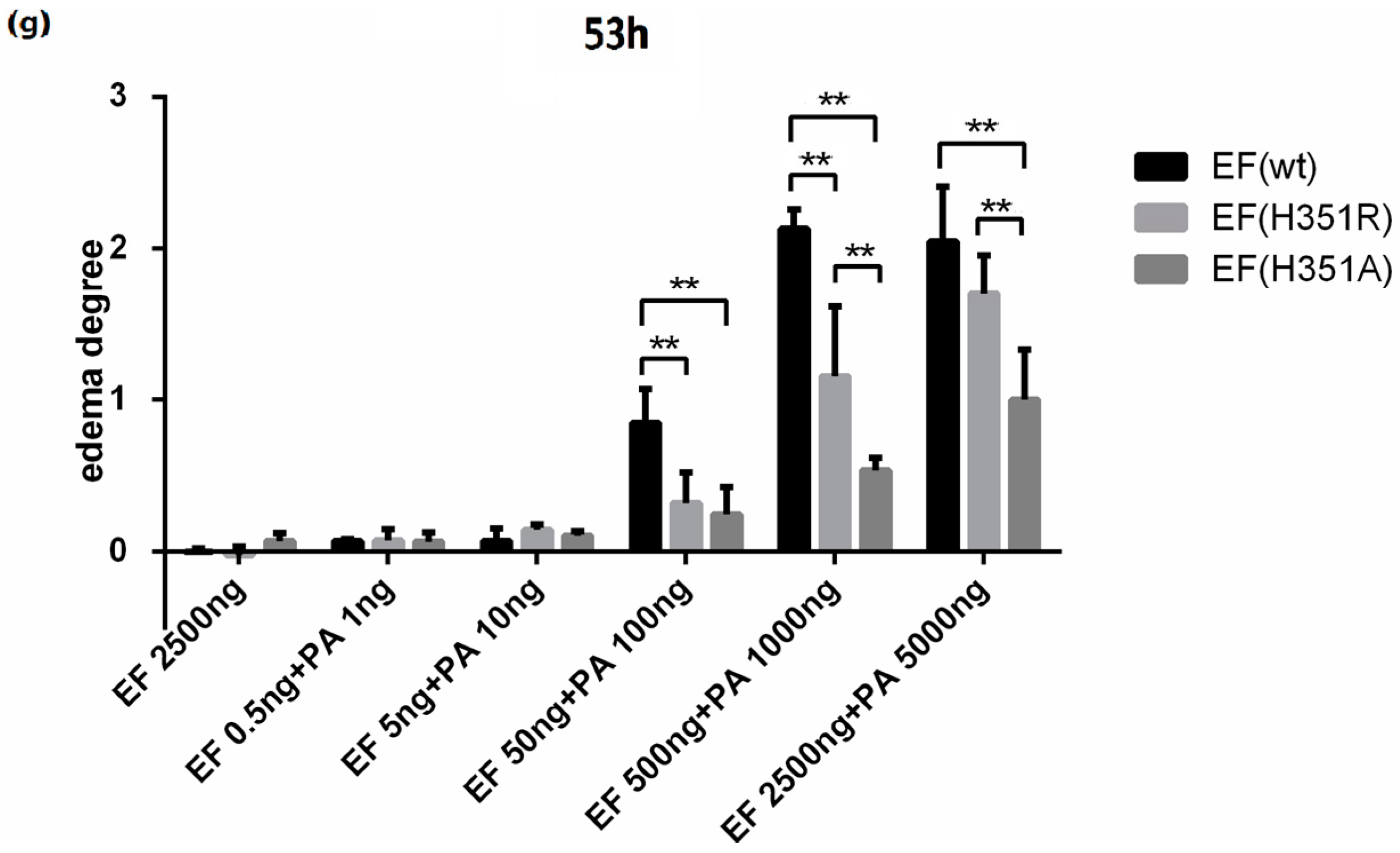
2.3. Footpad Edema Induced by Wild-Type and Mutant Toxins
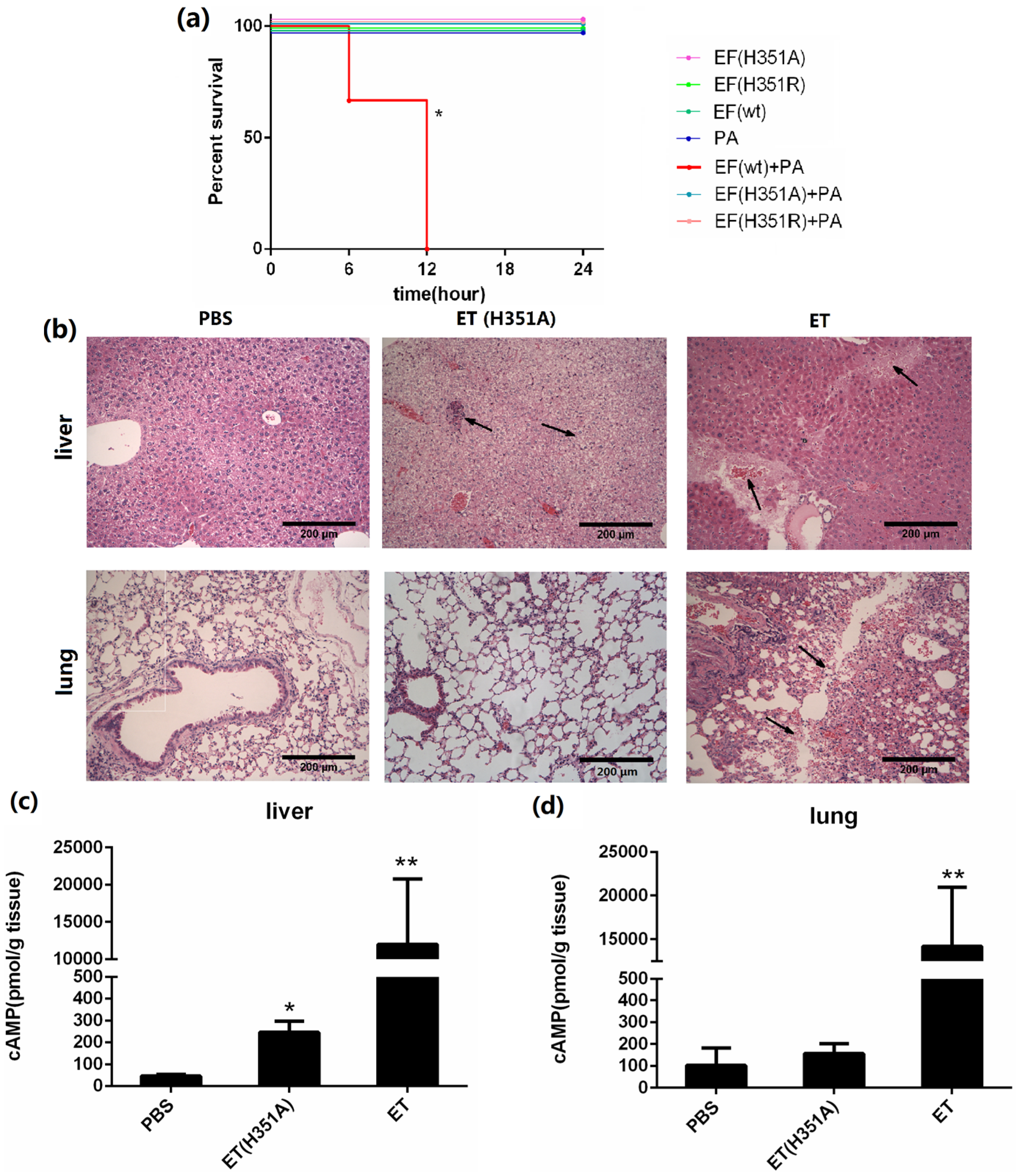
2.4. Systemic Effects of Wild-type and His351 EF Mutants
3. Experimental Section
3.1. Materials
3.2. Plasmid Construction
- 5-StuI-EF: 5′-TTTAGGCCTGTTAATAAG-3′
- 3-ApaI-H351A: 5′-CAGGGCCCCAATCCGAACTCTTTCCCGCAACATTCAATC-3′
- 3-ApaI-H351R: 5′-CAGGGCCCCAATCCGAACTCTTTCCACGAACATTCAATC-3′
3.3. Expression and Purification of EF and Mutant Proteins
| Solution | Ingredient | pH |
|---|---|---|
| Buffer A | 50 mM sodium phosphate, 300 mM sodium chloride | 8.0 |
| Buffer B1 | 1% Glycerin and 2 mM β-mercaptoethanol added to buffer A | 8.0 |
| Buffer B2 | 20 mM imidazole added to buffer B1 | 8.0 |
| Buffer B3 | 100 mM imidazole added to buffer B1 | 8.0 |
| Buffer C | 20 mM potassium phosphate, 1 mM EDTA, 1% glycerin and 2 mM β-mercaptoethanol | 7.0 |
3.4. Intracellular cAMP Level Analysis
3.5. Animal Experiments
3.6. Mouse Lethality Assay
3.7. Paw Edema Induction
3.8. Histological Studies
3.9. Tissue cAMP Level Analysis
3.10. Statistical Analysis
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Green, B.D.; Battisti, L.; Koehler, T.M.; Thorne, C.B.; Ivins, B.E. Demonstration of a capsule plasmid in Bacillus anthracis. Infect. Immun. 1985, 49, 291–297. [Google Scholar] [PubMed]
- Pezard, C.; Berche, P.; Mock, M. Contribution of individual toxin components to virulence of Bacillus anthracis. Infect. Immun. 1991, 59, 3472–3477. [Google Scholar] [PubMed]
- Vitale, G.; Bernardi, L.; Napolitani, G.; Mock, M.; Montecucco, C. Susceptibility of mitogen-activated protein kinase kinase family members to proteolysis by anthrax lethal factor. Biochem. J. 2000, 352, 739–745. [Google Scholar] [CrossRef] [PubMed]
- Ebrahimi, C.M.; Sheen, T.R.; Renken, C.W.; Gottlieb, R.A.; Doran, K.S. Contribution of lethal toxin and edema toxin to the pathogenesis of anthrax meningitis. Infect. Immun. 2011, 79, 2510–2518. [Google Scholar] [CrossRef] [PubMed]
- Drum, C.L.; Yan, S.-Z.; Bard, J.; Shen, Y.-Q.; Lu, D.; Soelaiman, S.; Grabarek, Z.; Bohm, A.; Tang, W.-J. Structural basis for the activation of anthrax adenylyl cyclase exotoxin by calmodulin. Nature 2002, 415, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Ulmer, T.S.; Soelaiman, S.; Li, S.; Klee, B.C.; Tang, W.-J.; Bax, A. Calcium dependence of the interaction between calmodulin and anthrax edema factor. J. Biol. Chem. 2003, 278, 29261–29266. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.; Alam, S.; Bhatnagar, R. Kinetic characterization and ligand binding studies of His351 mutants of Bacillus anthracis adenylate cyclase. Arch. Biochem. Biophys. 2006, 446, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Zhukovskaya, N.; Guo, Q.; Florian, J.; Tang, W. Calcium-independent calmodulin binding and two-metal-ion catalytic mechanism of anthrax edema factor. Embo J. Mol. Bio. Organ. 2005, 24, 929–941. [Google Scholar] [CrossRef] [PubMed]
- Ramasamy, S.; Liu, C.Q.; Tran, H.; Gubala, A.; Gauci, P.; McAllister, J.; Vo, T. Principles of antidote pharmacology: An update on prophylaxis, post-exposure treatment recommendations and research initiatives for biological agents. Br. J. Pharmacol. 2010, 161, 721–748. [Google Scholar] [CrossRef] [PubMed]
- Maldonadoarocho, F.; Fulcher, J.; Lee, B.; Bradley, K. Anthrax oedema toxin induces anthrax toxin receptor expression in monocyte-derived cells. Mol. Microbiol. 2006, 61, 324–337. [Google Scholar] [CrossRef] [PubMed]
- Gottle, M.; Dove, S.; Seifert, R. Bacillus anthracis edema factor substrate specificity: Evidence for new modes of action. Toxins 2012, 4, 505–535. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Moayeri, M.; Zhao, H.; Crown, D.; Leppla, S.H.; Purcell, R.H. Potent neutralization of anthrax edema toxin by a humanized monoclonal antibody that competes with calmodulin for edema factor binding. Proc. Natl. Acad. Sci. USA 2009, 106, 13487–13492. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.; Alam, S.; Bhatnagar, R. Catalytically inactive anthrax toxin(s) are potential prophylactic agents. Vaccine 2007, 25, 8410–8419. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Zhang, Y.; Moayeri, M.; Liu, J.; Crown, D.; Fattah, R.J.; Wein, A.N.; Yu, Z.X.; Finkel, T.; Leppla, S.H. Key tissue targets responsible for anthrax-toxin-induced lethality. Nature 2013, 501, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Firoved, A.M.; Miller, G.F.; Moayeri, M.; Kakkar, R.; Shen, Y.; Wiggins, J.F.; McNally, E.M.; Tang, W.-J.; Leppla, S.H. Bacillus anthracis Edema Toxin Causes Extensive Tissue Lesions and Rapid Lethality in Mice. Am. J. Pathol. 2005, 167, 1309–1320. [Google Scholar] [CrossRef]
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, T.; Zhao, X.; Liu, J.; Meng, Y.; Feng, Y.; Fang, T.; Zhang, J.; Yang, X.; Li, J.; Xu, J.; et al. Diminished but Not Abolished Effect of Two His351 Mutants of Anthrax Edema Factor in a Murine Model. Toxins 2016, 8, 35. https://doi.org/10.3390/toxins8020035
Zhao T, Zhao X, Liu J, Meng Y, Feng Y, Fang T, Zhang J, Yang X, Li J, Xu J, et al. Diminished but Not Abolished Effect of Two His351 Mutants of Anthrax Edema Factor in a Murine Model. Toxins. 2016; 8(2):35. https://doi.org/10.3390/toxins8020035
Chicago/Turabian StyleZhao, Taoran, Xinghui Zhao, Ju Liu, Yingying Meng, Yingying Feng, Ting Fang, Jinlong Zhang, Xiuxu Yang, Jianmin Li, Junjie Xu, and et al. 2016. "Diminished but Not Abolished Effect of Two His351 Mutants of Anthrax Edema Factor in a Murine Model" Toxins 8, no. 2: 35. https://doi.org/10.3390/toxins8020035
APA StyleZhao, T., Zhao, X., Liu, J., Meng, Y., Feng, Y., Fang, T., Zhang, J., Yang, X., Li, J., Xu, J., & Chen, W. (2016). Diminished but Not Abolished Effect of Two His351 Mutants of Anthrax Edema Factor in a Murine Model. Toxins, 8(2), 35. https://doi.org/10.3390/toxins8020035