Botulinum Toxin Complex Serotype B-Okra Exerts Systemic Toxicity via the Oral Route by Disrupting the Intestinal Epithelial Barrier
Abstract
1. Introduction
2. Results
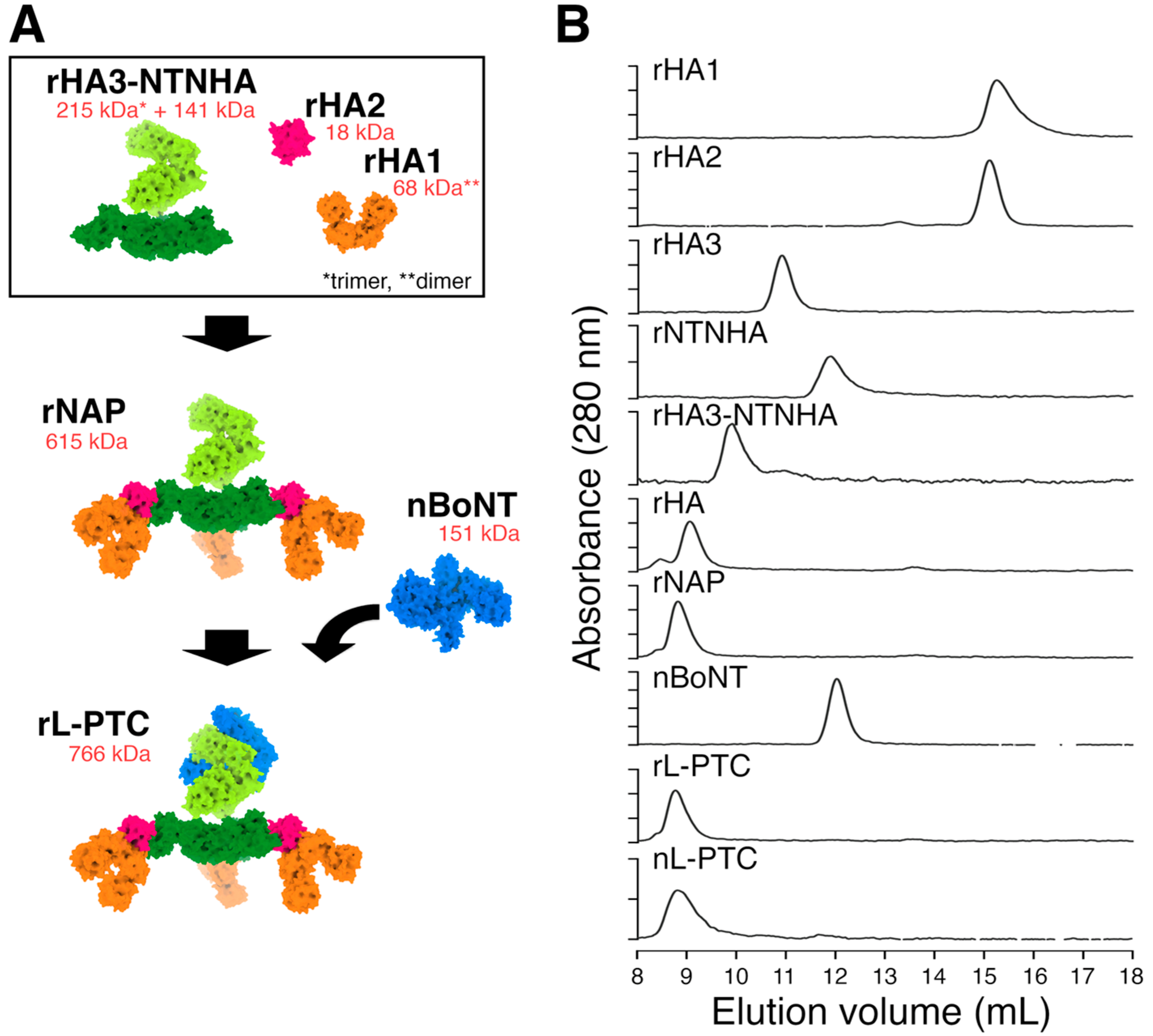
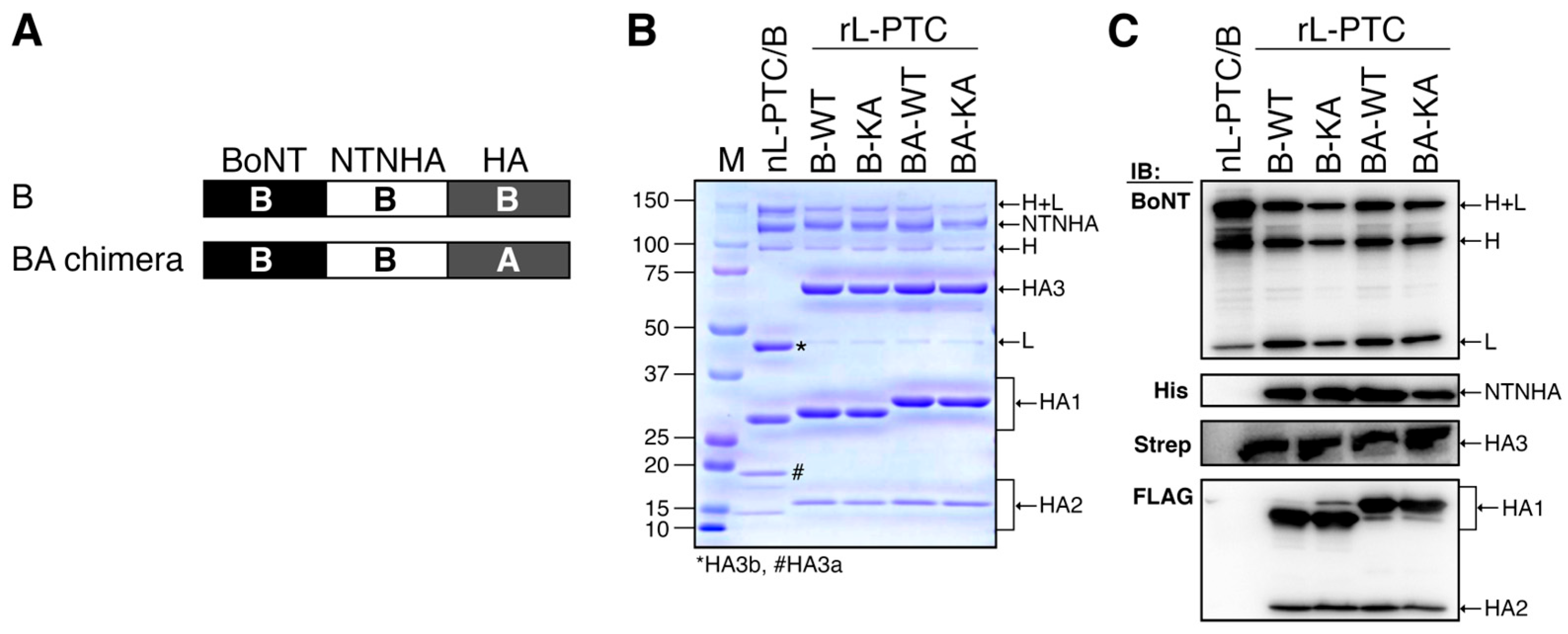
2.1. In Vitro Reconstitution and Purification of Recombinant L-PTC (rL-PTC)
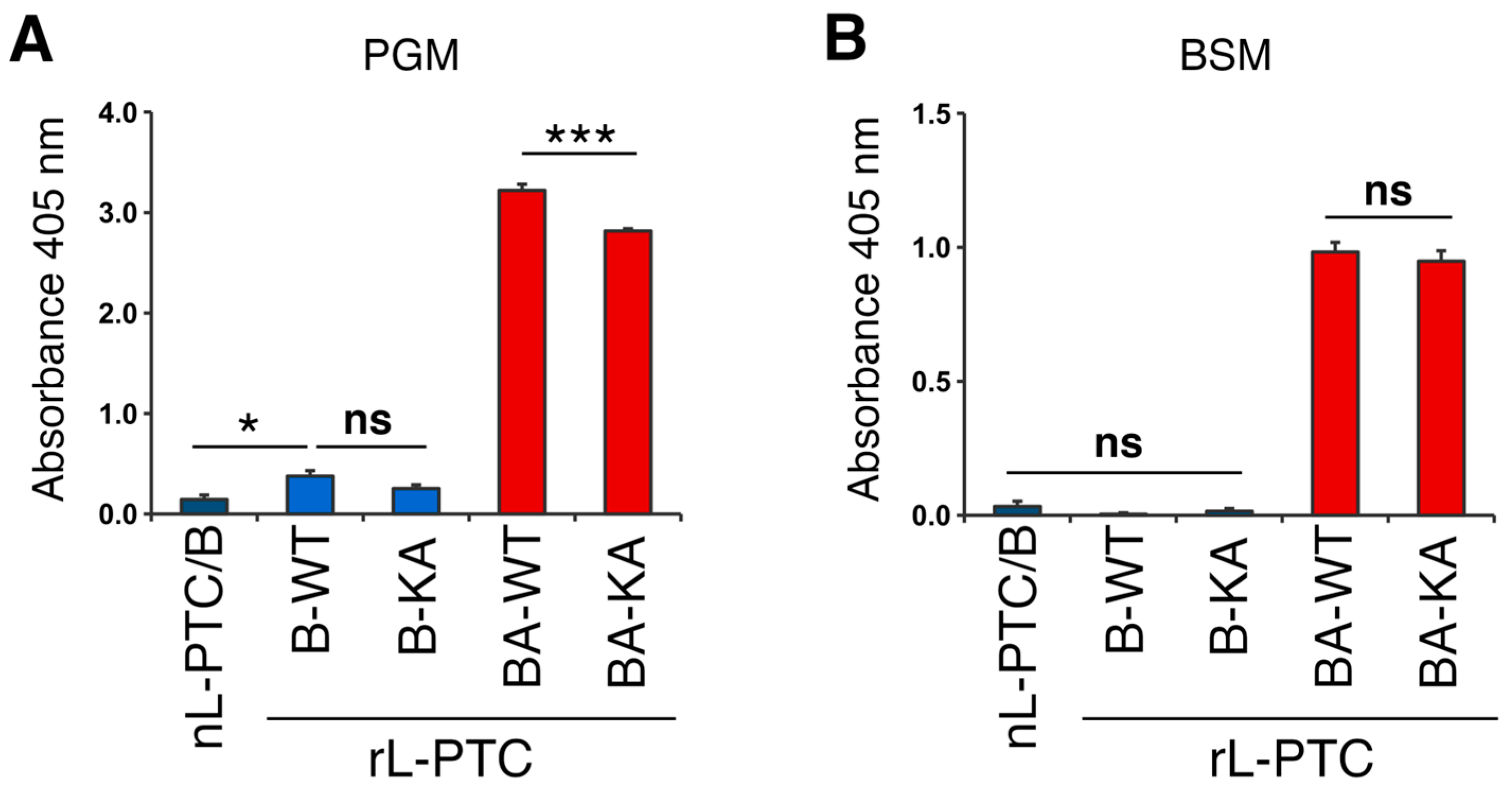
2.2. Carbohydrate-Binding Activity
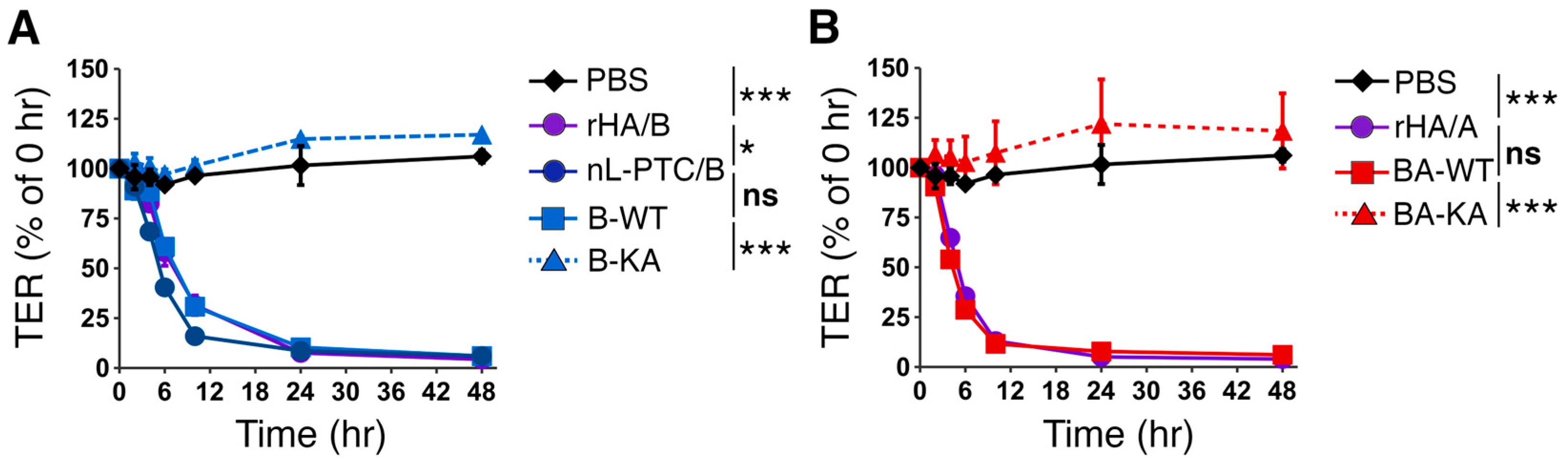
2.3. Epithelial Barrier-Disrupting Activity
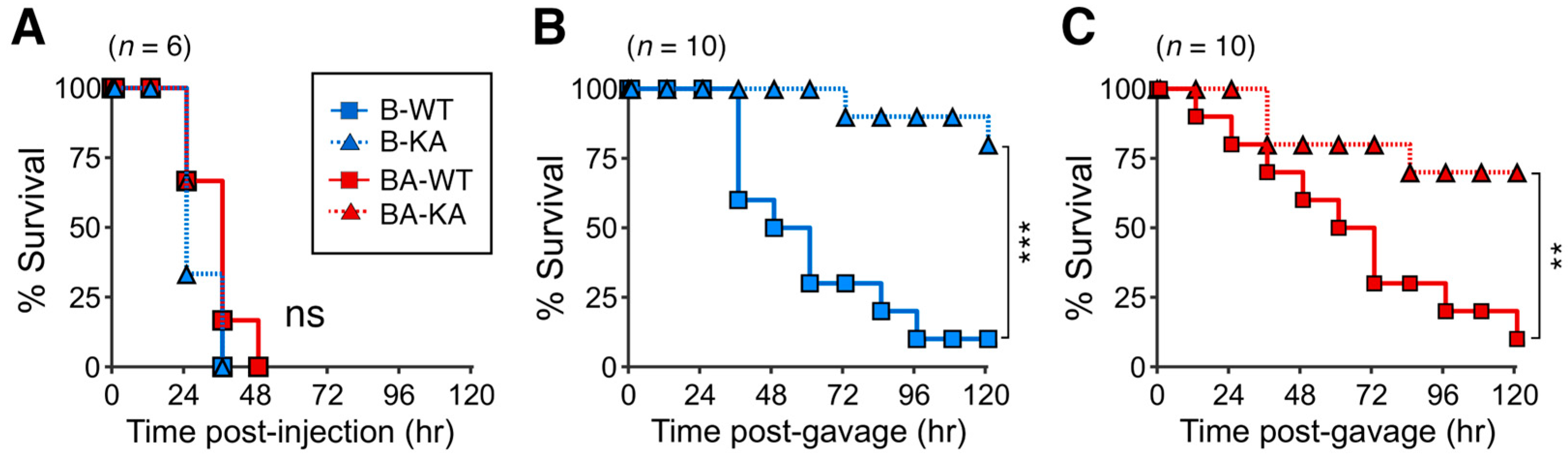
2.4. Toxicities of rL-PTC
3. Discussion
4. Materials and Methods
4.1. Plasmid Construction
4.2. Protein Expression and Purification
4.3. In Vitro Reconstitution and Purification
4.4. Size Exclusion Chromatography
4.5. Western Blotting
4.6. Mucin ELISA
4.7. Transepithelial Electrical Resistance (TER) Assay
4.8. Mouse Bioassay
4.9. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Schiavo, G.; Matteoli, M.; Montecucco, C. Neurotoxins Affecting Neuroexocytosis. Physiol. Rev. 2000, 80, 717–766. [Google Scholar] [CrossRef]
- Sakaguchi, G. Clostridium Botulinum Toxins. Pharmacol. Ther. 1982, 19, 165–194. [Google Scholar] [CrossRef] [PubMed]
- Sugii, S.; Ohishi, I.; Sakaguchi, G. Correlation between Oral Toxicity and in Vitro Stability of Clostridium botulinum Type A and B Toxins of Different Molecular Sizes. Infect. Immun. 1977, 16, 910–914. [Google Scholar] [CrossRef]
- Amatsu, S.; Sugawara, Y.; Matsumura, T.; Kitadokoro, K.; Fujinaga, Y. Crystal Structure of Clostridium botulinum Whole Hemagglutinin Reveals a Huge Triskelion-Shaped Molecular Complex. J. Biol. Chem. 2013, 288, 35617–35625. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Gu, S.; Jin, L.; Le, T.T.N.; Cheng, L.W.; Strotmeier, J.; Kruel, A.M.; Yao, G.; Perry, K.; Rummel, A.; et al. Structure of a Bimodular Botulinum Neurotoxin Complex Provides Insights into Its Oral Toxicity. PLoS Pathog. 2013, 9, e1003690. [Google Scholar] [CrossRef]
- Benefield, D.A.; Dessain, S.K.; Shine, N.; Ohi, M.D.; Lacy, D.B. Molecular Assembly of Botulinum Neurotoxin Progenitor Complexes. Proc. Natl. Acad. Sci. USA 2013, 110, 5630–5635. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, K.; Watanabe, T.; Suzuki, T.; Yamano, A.; Oikawa, T.; Sato, Y.; Kouguchi, H.; Yoneyama, T.; Niwa, K.; Ikeda, T.; et al. A Novel Subunit Structure of Clostridium Botulinum Serotype D Toxin Complex with Three Extended Arms. J. Biol. Chem. 2007, 282, 24777–24783. [Google Scholar] [CrossRef]
- Ohishi, I. Oral Toxicities of Clostridium botulinum Type A and B Toxins from Different Strains. Infect. Immun. 1984, 43, 487–490. [Google Scholar] [CrossRef]
- Fujinaga, Y.; Inoue, K.; Watanabe, S.; Yokota, K.; Hirai, Y.; Nagamachi, E.; Oguma, K. The Haemagglutinin of Clostridium botulinum Type C Progenitor Toxin Plays an Essential Role in Binding of Toxin to the Epithelial Cells of Guinea Pig Small Intestine, Leading to the Efficient Absorption of the Toxin. Microbiology 1997, 143, 3841–3847. [Google Scholar] [CrossRef]
- Inoue, K.; Sobhany, M.; Transue, T.R.; Oguma, K.; Pedersen, L.C.; Negishi, M. Structural Analysis by X-Ray Crystallography and Calorimetry of a Haemagglutinin Component (HA1) of the Progenitor Toxin from Clostridium botulinum. Microbiology 2003, 149, 3361–3370. [Google Scholar] [CrossRef]
- Lee, K.; Lam, K.H.; Kruel, A.M.; Perry, K.; Rummel, A.; Jin, R. High-Resolution Crystal Structure of HA33 of Botulinum Neurotoxin Type B Progenitor Toxin Complex. Biochem. Biophys. Res. Commun. 2014, 446, 568–573. [Google Scholar] [CrossRef] [PubMed]
- Tulin, E.K.C.; Nakazawa, C.; Nakamura, T.; Saito, S.; Phzono, N.; Hiemori, K.; Nakakita, S.I.; Tateno, H.; Tonozuka, T.; Nishikawa, A. Glycan Detecting Tools Developed from the Clostridium botulinum Whole Hemagglutinin Complex. Sci. Rep. 2021, 11, 21973. [Google Scholar] [CrossRef]
- Amatsu, S.; Matsumura, T.; Yutani, M.; Fujinaga, Y. Multivalency Effects of Hemagglutinin Component of Type B Botulinum Neurotoxin Complex on Epithelial Barrier Disruption: Multivalency Effect of HA. Microbiol. Immunol. 2018, 62, 80–89. [Google Scholar] [CrossRef]
- Amatsu, S.; Fujinaga, Y. Botulinum Hemagglutinin: Critical Protein for Adhesion and Absorption of Neurotoxin Complex in Host Intestine. Methods Mol. Biol. 2020, 2132, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, T.; Jin, Y.; Kabumoto, Y.; Takegahara, Y.; Oguma, K.; Lencer, W.I.; Fujinaga, Y. The HA Proteins of Botulinum Toxin Disrupt Intestinal Epithelial Intercellular Junctions to Increase Toxin Absorption. Cell. Microbiol. 2008, 10, 355–364. [Google Scholar] [CrossRef]
- Sugawara, Y.; Matsumura, T.; Takegahara, Y.; Jin, Y.; Tsukasaki, Y.; Takeichi, M.; Fujinaga, Y. Botulinum Hemagglutinin Disrupts the Intercellular Epithelial Barrier by Directly Binding E-Cadherin. J. Cell Biol. 2010, 189, 691–700. [Google Scholar] [CrossRef]
- Sugawara, Y.; Yutani, M.; Amatsu, S.; Matsumura, T.; Fujinaga, Y. Functional Dissection of the Clostridium botulinum Type B Hemagglutinin Complex: Identification of the Carbohydrate and E-Cadherin Binding Sites. PLoS ONE 2014, 9, e111170. [Google Scholar] [CrossRef]
- Lee, K.; Zhong, X.; Gu, S.; Kruel, A.M.; Dorner, M.B.; Perry, K.; Rummel, A.; Dong, M.; Jin, R. Molecular Basis for Disruption of E-Cadherin Adhesion by Botulinum Neurotoxin A Complex. Science 2014, 344, 1405–1410. [Google Scholar] [CrossRef]
- Amatsu, S.; Matsumura, T.; Zuka, M.; Fujinaga, Y. Molecular Engineering of a Minimal E-Cadherin Inhibitor Protein Derived from Clostridium botulinum Hemagglutinin. J. Biol. Chem. 2023, 299. [Google Scholar] [CrossRef]
- Fujinaga, Y.; Inoue, K.; Nomura, T.; Sasaki, J.; Marvaud, J.C.; Popoff, M.R.; Kozaki, S.; Oguma, K. Identification and Characterization of Functional Subunits of Clostridium botulinum Type A Progenitor Toxin Involved in Binding to Intestinal Microvilli and Erythrocytes. FEBS Lett. 2000, 467, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Arimitsu, H.; Sakaguchi, Y.; Lee, J.C.; Ochi, S.; Tsukamoto, K.; Yamamoto, Y.; Ma, S.; Tsuji, T.; Oguma, K. Molecular Properties of Each Subcomponent in Clostridium botulinum Type B Haemagglutinin Complex. Microb. Pathog. 2008, 45, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Yao, G.; Lee, K.; Gu, S.; Lam, K.H.; Jin, R. Botulinum Neurotoxin A Complex Recognizes Host Carbohydrates through Its Hemagglutinin Component. Toxins 2014, 6, 624–635. [Google Scholar] [CrossRef]
- Matsumura, T.; Sugawara, Y.; Yutani, M.; Amatsu, S.; Yagita, H.; Kohda, T.; Fukuoka, S.I.; Nakamura, Y.; Fukuda, S.; Hase, K.; et al. Botulinum Toxin A Complex Exploits Intestinal M Cells to Enter the Host and Exert Neurotoxicity. Nat. Commun. 2015, 6, 6255. [Google Scholar] [CrossRef]
- Lam, T.I.; Stanker, L.H.; Lee, K.; Jin, R.; Cheng, L.W. Translocation of Botulinum Neurotoxin Serotype A and Associated Proteins across the Intestinal Epithelia. Cell. Microbiol. 2015, 17, 1133–1143. [Google Scholar] [CrossRef]
- Amatsu, S.; Matsumura, T.; Morimoto, C.; Keisham, S.; Goto, Y.; Kohda, T.; Hirabayashi, J.; Kitadokoro, K.; Katayama, T.; Kiyono, H.; et al. Gut Mucin Fucosylation Dictates the Entry of Botulinum Toxin Complexes. bioRxiv 2025. [Google Scholar] [CrossRef]
- Hill, K.K.; Smith, T.J. Genetic Diversity Within Clostridium botulinum Serotypes, Botulinum Neurotoxin Gene Clusters and Toxin Subtypes. Curr. Top. Microbiol. Immunol. 2013, 364, 1–20. [Google Scholar] [CrossRef]
- Gao, L.; Nowakowska, M.B.; Selby, K.; Przykopanski, A.; Chen, B.; Krüger, M.; Douillard, F.P.; Lam, K.H.; Chen, P.; Huang, T.; et al. Botulinum Neurotoxins Exploit Host Digestive Proteases to Boost Their Oral Toxicity via Activating OrfXs/P47. Nat. Struct. Mol. Biol. 2025, 32, 864–875. [Google Scholar] [CrossRef]
- Arnon, S.S.; Schechter, R.; Inglesby, T.V.; Henderson, D.A.; Bartlett, J.G.; Ascher, M.S.; Eitzen, E.; Fine, A.D.; Hauer, J.; Layton, M.; et al. Botulinum Toxin as a Biological Weapon: Medical and Public Health Management. JAMA 2001, 285, 1059–1070. [Google Scholar] [CrossRef]
- Ohno, H.; Hase, K. Glycoprotein 2 (GP2): Grabbing the FimH bacteria into M cells for mucosal immunity. Gut Microbes 2010, 1, 407–410. [Google Scholar] [CrossRef] [PubMed]
- Van Der Flier, L.G.; Clevers, H. Stem Cells, Self-Renewal, and Differentiation in the Intestinal Epithelium. Annu. Rev. Physiol. 2009, 71, 241–260. [Google Scholar] [CrossRef] [PubMed]
- McGuckin, M.A.; Lindén, S.K.; Sutton, P.; Florin, T.H. Mucin Dynamics and Enteric Pathogens. Nat. Rev. Microbiol. 2011, 9, 265–278. [Google Scholar] [CrossRef]
- Wu, Y.; Wang, X.; Csencsits, K.L.; Haddad, A.; Walters, N.; Pascual, D.W. M Cell-Targeted DNA Vaccination. Proc. Natl. Acad. Sci. USA 2001, 98, 9318–9323. [Google Scholar] [CrossRef]
- Shima, H.; Watanabe, T.; Fukuda, S.; Fukuoka, S.I.; Ohara, O.; Ohno, H. A Novel Mucosal Vaccine Targeting Peyer’s Patch M Cells Induces Protective Antigen-Specific IgA Responses. Int. Immun. 2014, 26, 619–625. [Google Scholar] [CrossRef]
- Nochi, T.; Takagi, H.; Yuki, Y.; Yang, L.; Masumura, T.; Mejima, M.; Nakanishi, U.; Matsumura, A.; Uozumi, A.; Hiroi, T.; et al. Rice-Based Mucosal Vaccine as a Global Strategy for Cold-Chain- and Needle-Free Vaccination. Proc. Natl. Acad. Sci. USA 2007, 104, 10986–10991. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, M.; Pascual, D.W.; Kiyono, H. M Cell-Targeted Mucosal Vaccine Strategies. Curr. Top. Microbiol. Immunol. 2012, 354, 39–52. [Google Scholar] [CrossRef]
- Nochi, T.; Yuki, Y.; Matsumura, A.; Mejima, M.; Terahara, K.; Kim, D.Y.; Fukuyama, S.; Iwatsuki-Horimoto, K.; Kawaoka, Y.; Kohda, T.; et al. A Novel M Cell–Specific Carbohydrate-Targeted Mucosal Vaccine Effectively Induces Antigen-Specific Immune Responses. J. Exp. Med. 2007, 204, 2789–2796. [Google Scholar] [CrossRef] [PubMed]
- Zou, J.J.; Wei, G.; Xiong, C.; Yu, Y.; Li, S.; Hu, L.; Ma, S.; Tian, J. Efficient Oral Insulin Delivery Enabled by Transferrin-Coated Acid-Resistant Metal-Organic Framework Nanoparticles. Sci. Adv. 2022, 8, eabm4677. [Google Scholar] [CrossRef]
- Suzuki, H.; Tani, K.; Fujiyoshi, Y. Crystal Structures of Claudins: Insights into Their Intermolecular Interactions. Ann. N. Y. Acad. Sci. 2017, 1397, 25–34. [Google Scholar] [CrossRef]
- Katahira, J.; Sugiyama, H.; Inoue, N.; Horiguchi, Y.; Matsuda, M.; Sugimoto, N. Clostridium perfringens Enterotoxin Utilizes Two Structurally Related Membrane Proteins as Functional Receptors in Vivo. J. Biol. Chem. 1997, 272, 26652–26658. [Google Scholar] [CrossRef] [PubMed]
- Kondoh, M.; Masuyama, A.; Takahashi, A.; Asano, N.; Mizuguchi, H.; Koizumi, N.; Fujii, M.; Hayakawa, T.; Horiguchi, Y.; Watanbe, Y. A Novel Strategy for the Enhancement of Drug Absorption Using a Claudin Modulator. Mol. Pharmacol. 2005, 67, 749–756. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, T.; Amatsu, S.; Misaki, R.; Yutani, M.; Du, A.; Kohda, T.; Fujiyama, K.; Ikuta, K.; Fujinaga, Y. Fully Human Monoclonal Antibodies Effectively Neutralizing Botulinum Neurotoxin Serotype, B. Toxins 2020, 12, 302. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morimoto, C.; Amatsu, S.; Matsumura, T.; Zuka, M.; Fujinaga, Y. Botulinum Toxin Complex Serotype B-Okra Exerts Systemic Toxicity via the Oral Route by Disrupting the Intestinal Epithelial Barrier. Toxins 2025, 17, 443. https://doi.org/10.3390/toxins17090443
Morimoto C, Amatsu S, Matsumura T, Zuka M, Fujinaga Y. Botulinum Toxin Complex Serotype B-Okra Exerts Systemic Toxicity via the Oral Route by Disrupting the Intestinal Epithelial Barrier. Toxins. 2025; 17(9):443. https://doi.org/10.3390/toxins17090443
Chicago/Turabian StyleMorimoto, Chiyono, Sho Amatsu, Takuhiro Matsumura, Masahiko Zuka, and Yukako Fujinaga. 2025. "Botulinum Toxin Complex Serotype B-Okra Exerts Systemic Toxicity via the Oral Route by Disrupting the Intestinal Epithelial Barrier" Toxins 17, no. 9: 443. https://doi.org/10.3390/toxins17090443
APA StyleMorimoto, C., Amatsu, S., Matsumura, T., Zuka, M., & Fujinaga, Y. (2025). Botulinum Toxin Complex Serotype B-Okra Exerts Systemic Toxicity via the Oral Route by Disrupting the Intestinal Epithelial Barrier. Toxins, 17(9), 443. https://doi.org/10.3390/toxins17090443




