The Elias University Hospital Approach: A Visual Guide to Ultrasound-Guided Botulinum Toxin Injection in Spasticity: Part III—Proximal Lower Limb Muscles
Abstract
1. Introduction
2. General Methodology
3. Proximal Lower Limb Muscles Implicated in Post-Stroke Spasticity
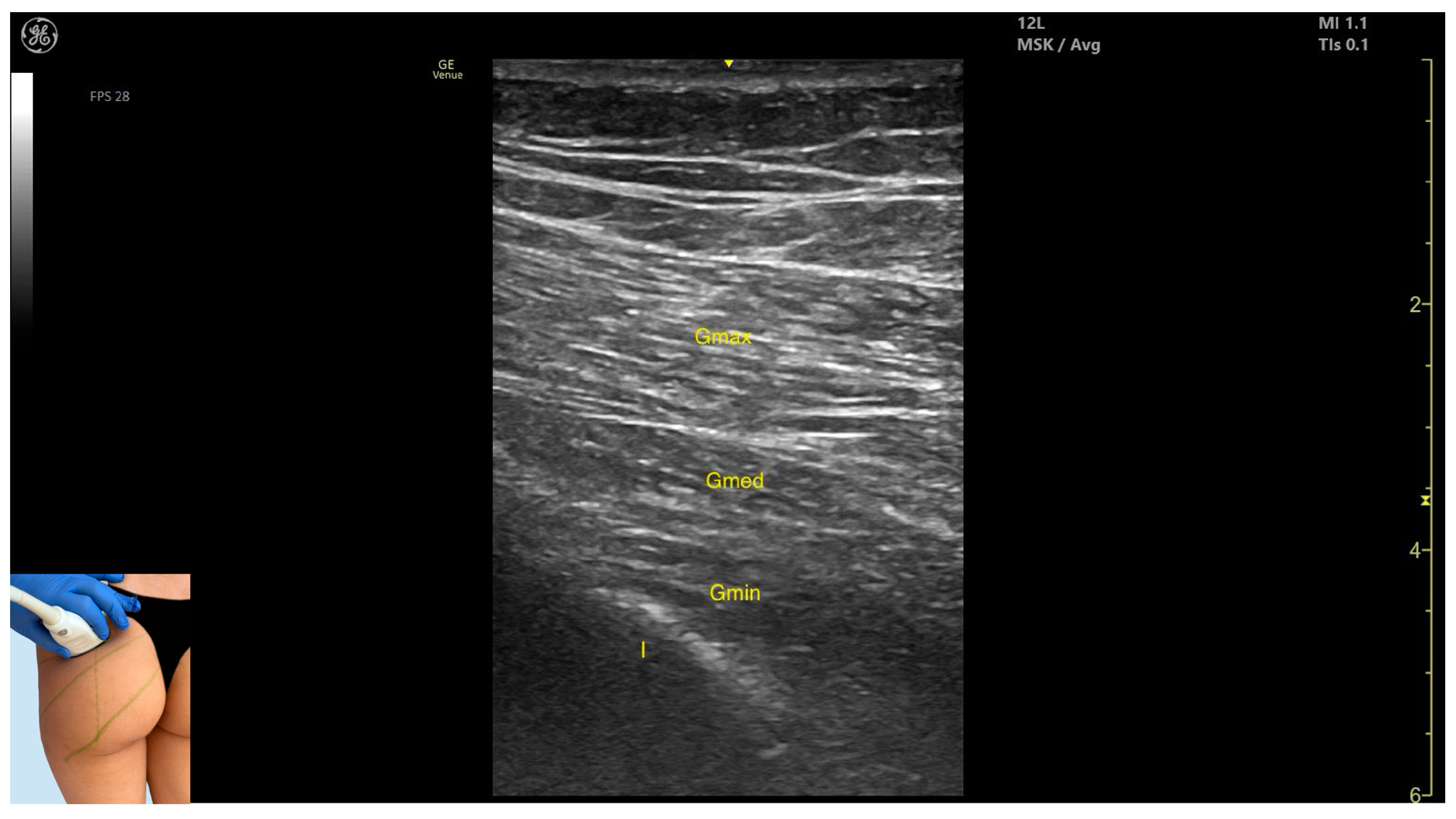
3.1. Gluteus Maximus (Gmax)
3.1.1. Overview
3.1.2. Ultrasound Identification
3.1.3. Key Ultrasound Landmarks
- Muscle morphology: It is the strongest and most superficial muscle in the gluteal group.
- Muscle position: It represents the most superficial muscle mass at this level. It lies superficial to both the gluteus medius and gluteus minimus.
- External fascia: It is enclosed by a pronounced fascia, which separates it from the subcutaneous tissue and the gluteus medius, facilitating botulinum toxin injection.
- Dynamic evaluation: During dynamic evaluation, scanning laterally toward the hip joint reveals an increase in muscle thickness of the gluteus medius and gluteus minimus. Muscle contraction is visible during hip extension and external rotation maneuvers.
3.1.4. Clinical Implications and Strategy
- Line (a): from the posterior superior iliac spine (PSIS) to the greater trochanter (GT) of the femur;
- Line (c): from the coccyx (CO) to the ischial tuberosity (IT);
- Line (b): drawn midway between lines a and c.
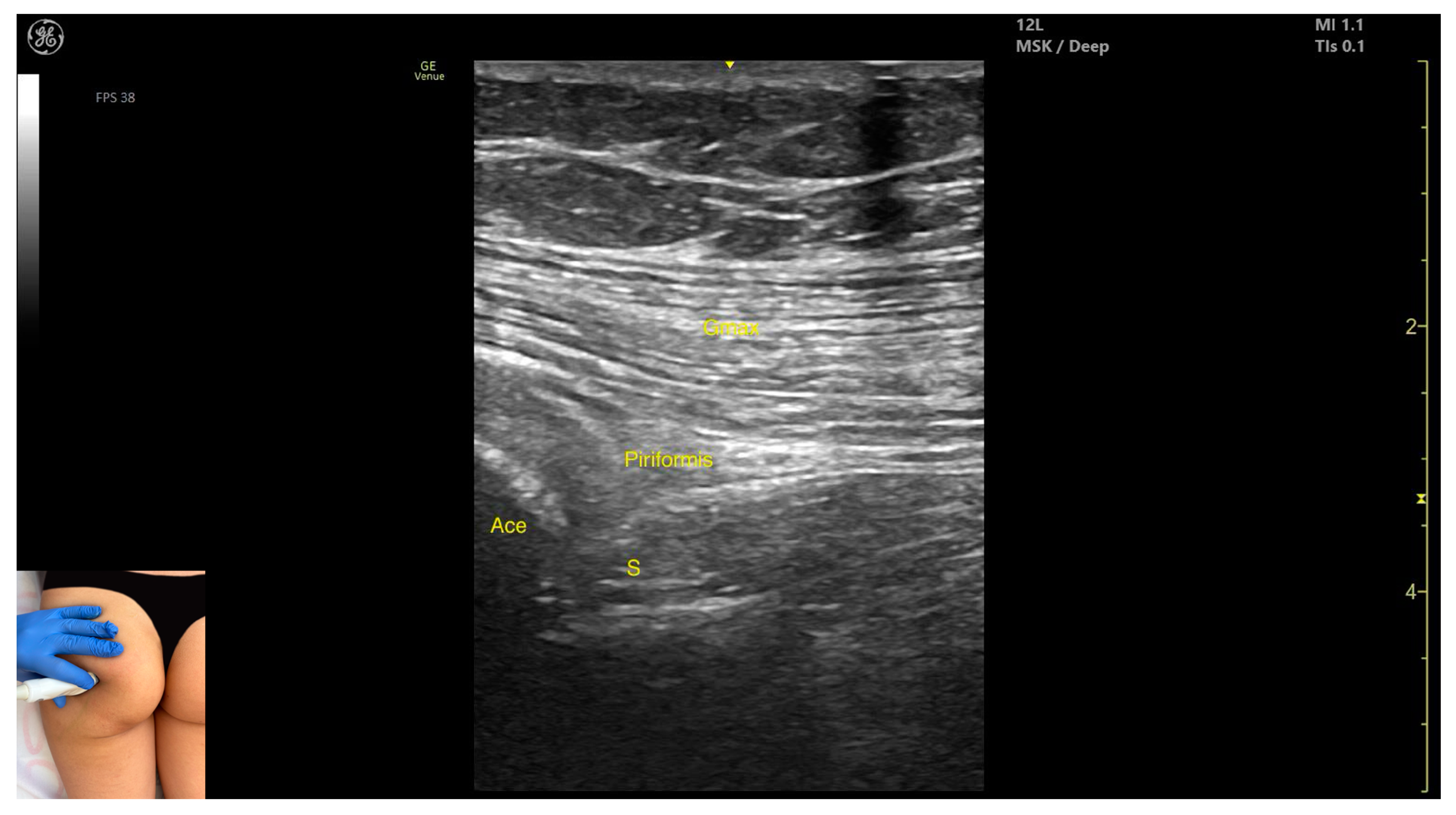
3.2. Piriformis
3.2.1. Overview
3.2.2. Ultrasound Identification
3.2.3. Key Ultrasound Landmarks
- Muscle morphology: It is part of the deep gluteal muscle group, along with the obturator internus, obturatorus externus, superior gemellus, inferior gemellus, and quadratus femoris.
- Muscle position: At this level, it appears as the first muscle mass superficial to the acetabular cortex. The sciatic nerve lies in close proximity, located deep to the piriformis.
- External fascia: It presents a well-defined fascia separating it from the gluteus maximus, which is important during botulinum toxin injection.
- Dynamic evaluation: During dynamic evaluation, scanning 2–3 cm distally toward the ischial tuberosity, the piriformis muscle tapers and disappears, and the obturator internus muscle becomes visible. Superficial to the obturator internus, the gluteus maximus and the sciatic nerve (within the intermuscular fascia) can be observed. Muscle contraction is visible during the external rotation and abduction of the femur at the hip joint.
3.2.4. Clinical Implications and Injection Strategy
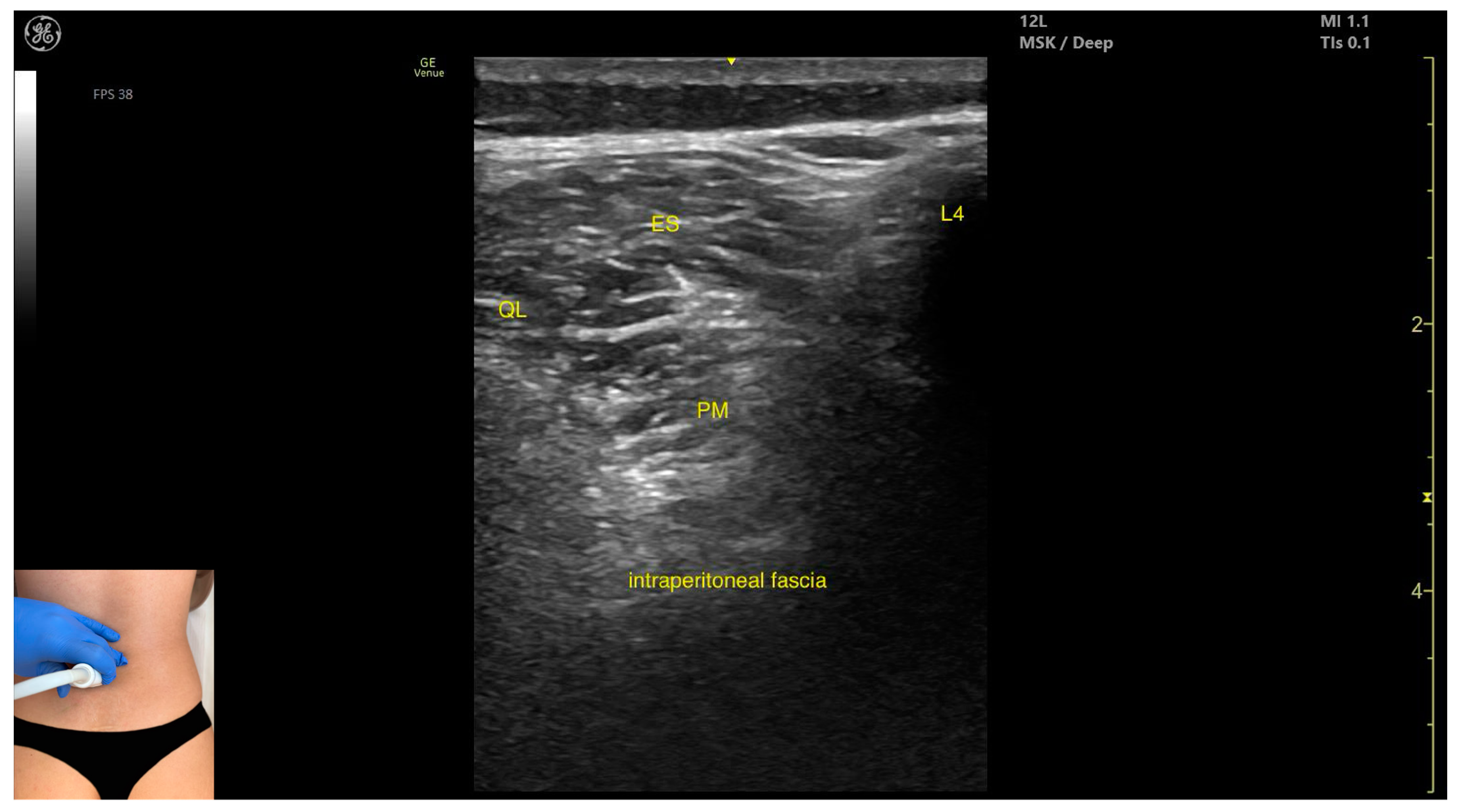
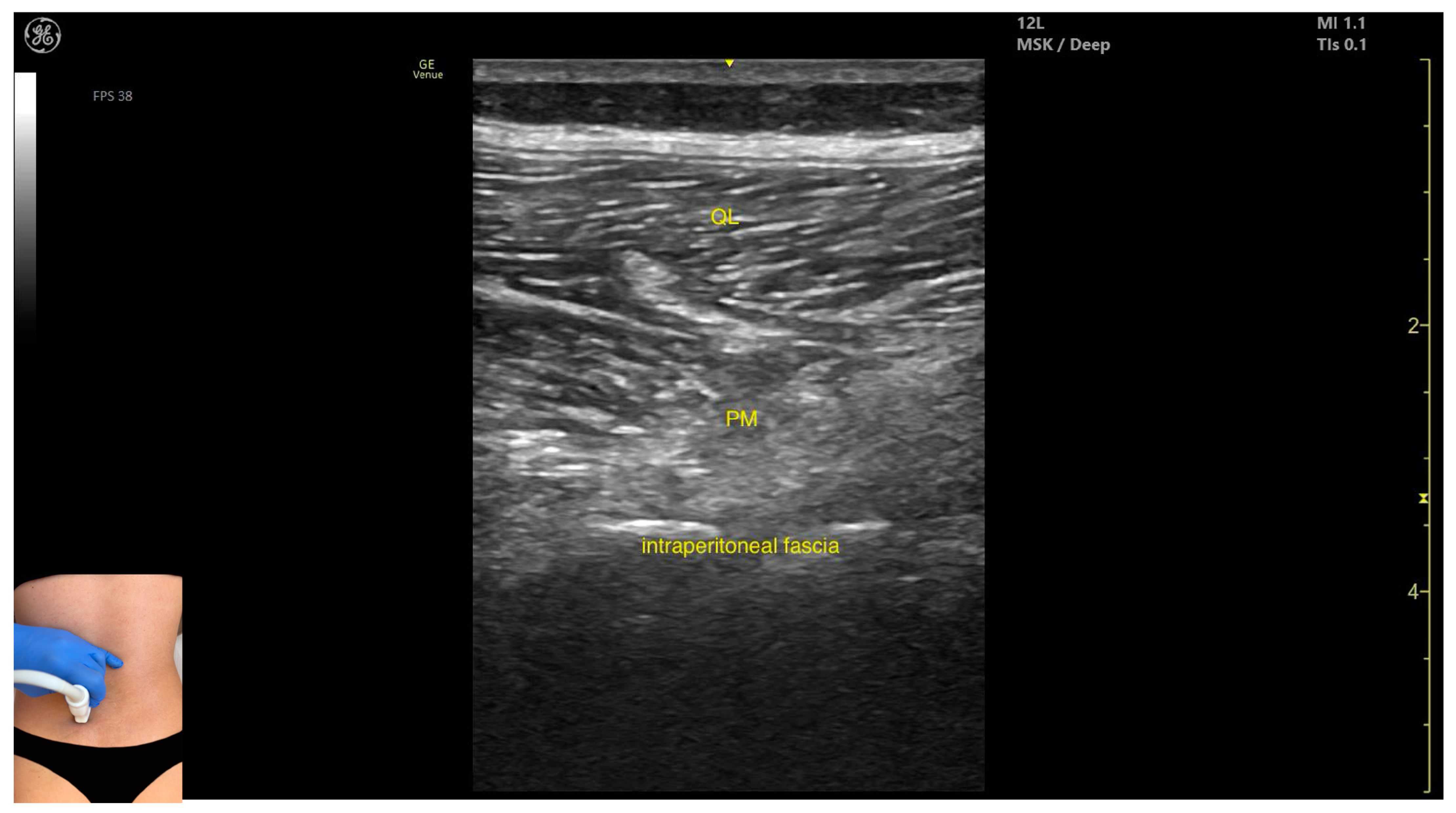
3.3. Psoas Major
3.3.1. Overview
3.3.2. Ultrasound Identification
3.3.3. Key Ultrasound Landmarks
- Muscle position: It is the deepest muscle mass at this level.
- External fascia: It presents a pronounced fascia that separates it from the erector spinae and quadratus lumborum, aiding in safe botulinum toxin injection.
- Dynamic evaluation: During dynamic evaluation, when scanning proximo-medially toward the costal arch, its origin is visualized from the T12 to L5 vertebrae.
- Contraction is visible during hip flexion, as well as lumbar spine flexion and lateral inflection maneuvers.
- The psoas major can also be visualized using a longitudinal transducer position, placed superior to the iliac crest and 2 cm lateral to the L4 spinous process. In this view, both the psoas major and the overlying quadratus lumborum are seen superficial to the intraperitoneal space.
3.3.4. Clinical Implications and Injection Strategy
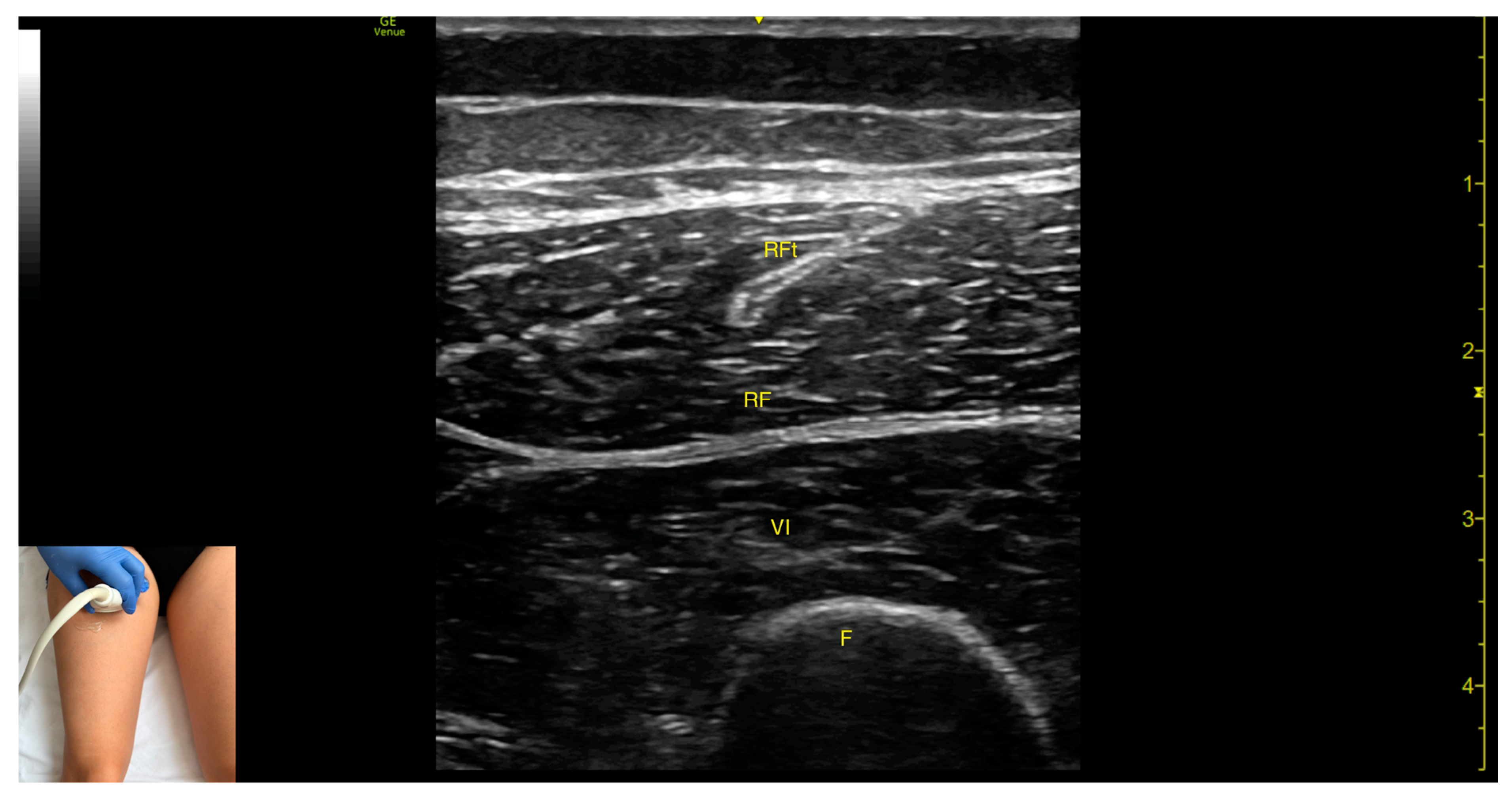
3.4. Rectus Femoris (RF)
3.4.1. Overview
3.4.2. Ultrasound Identification
3.4.3. Key Ultrasound Landmarks
- Muscle morphology: The RF is a bipennate muscle, characterized by a central septum, with muscle fibers attached on both sides and continuing into a central tendon. These two fiber regions should be individually targeted during injection
- Muscle position: It is the most superficial muscle mass at this level. Lateral to the rectus femoris lies the vastus lateralis, and medial to it, the vastus medialis.
- External fascia: A pronounced fascia separates the rectus femoris from the subcutaneous plane and adjacent muscles: vastus intermedius, vastus lateralis, and vastus medialis.
- Dynamic evaluation: During dynamic evaluation, scanning distally toward the knee joint, the muscle bulk of the RF decreases, but its central tendon remains visible until the distal third of the thigh (Video S1). Muscle contraction is visible during hip flexion and knee extension maneuvers.
3.4.4. Clinical Implications and Injection Strategy
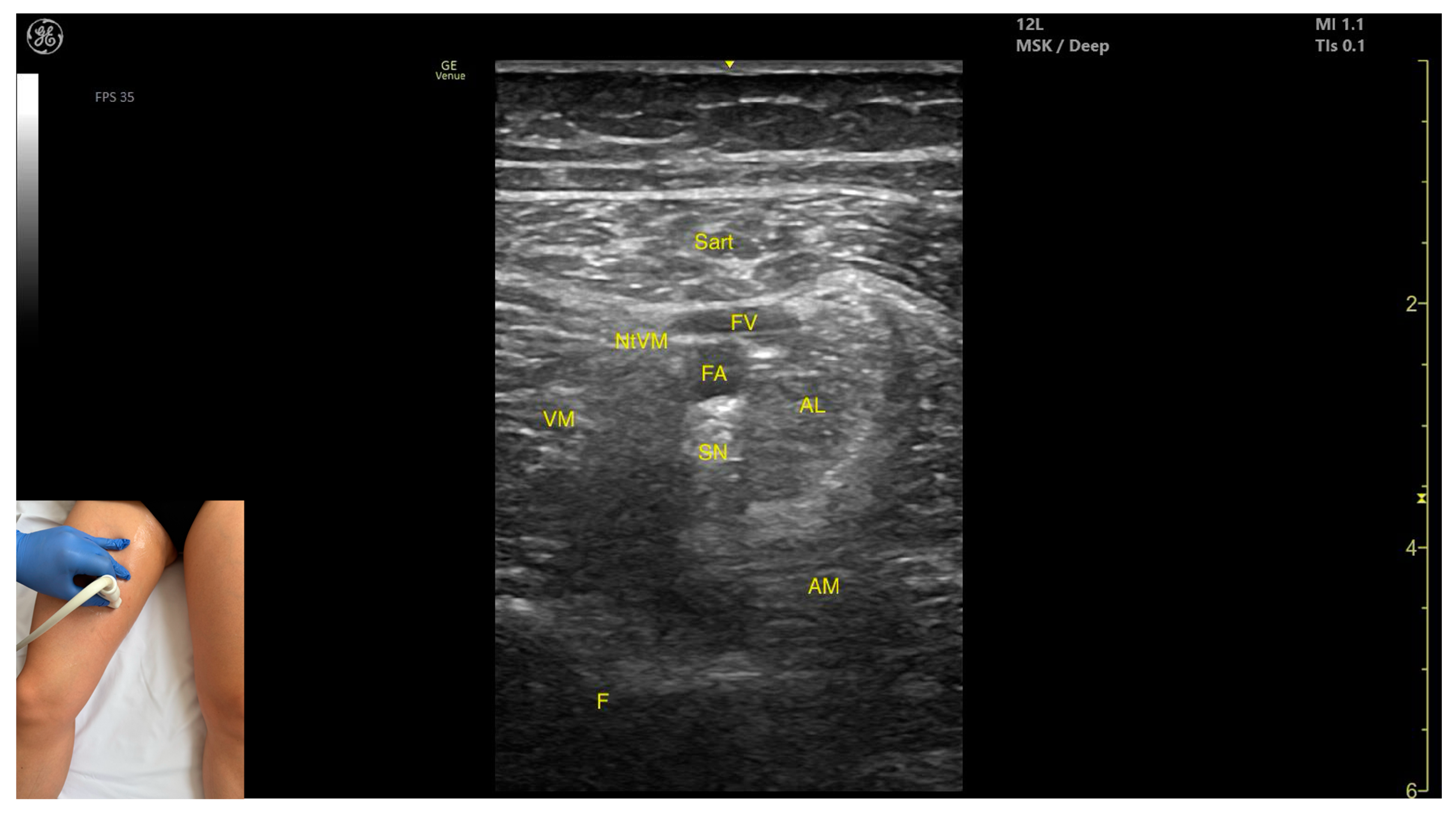
3.5. Sartorius (Sart)
3.5.1. Overview
3.5.2. Ultrasound Identification
3.5.3. Key Ultrasound Landmarks
- Muscle position: It is the most superficial muscle in the anterior compartment of the thigh. Deep and lateral to the sartorius lies the vastus medialis; deep and medial to the sartorius lies the adductor longus. At this level, the adductor canal is visualized beneath the Sart, containing the femoral artery, femoral vein, saphenous nerve, and nerve to vastus medialis.
- External fascia: A pronounced fascia separates the Sart from the subcutaneous plane, vastus medialis, adductor longus, and adductor magnus, aiding in precise botulinum toxin injection.
- Dynamic evaluation: During dynamic evaluation, scanning proximally toward the hip joint, at the proximal third of the anterior thigh, the adductor longus thickens medial and deep to the Sart, while the rectus femoris appears deep and lateral. At this level, the adductor canal shifts to lie medial to the Sart and lateral to the adductor longus. During distal scanning toward the knee joint, in the distal third of the anterior thigh, the gracilis is seen medial to the Sart, and the vastus medialis lies deep and lateral to it. Muscle contraction is visible during hip flexion, abduction, and internal rotation, as well as knee flexion maneuvers.
3.5.4. Clinical Implications and Injection Strategy
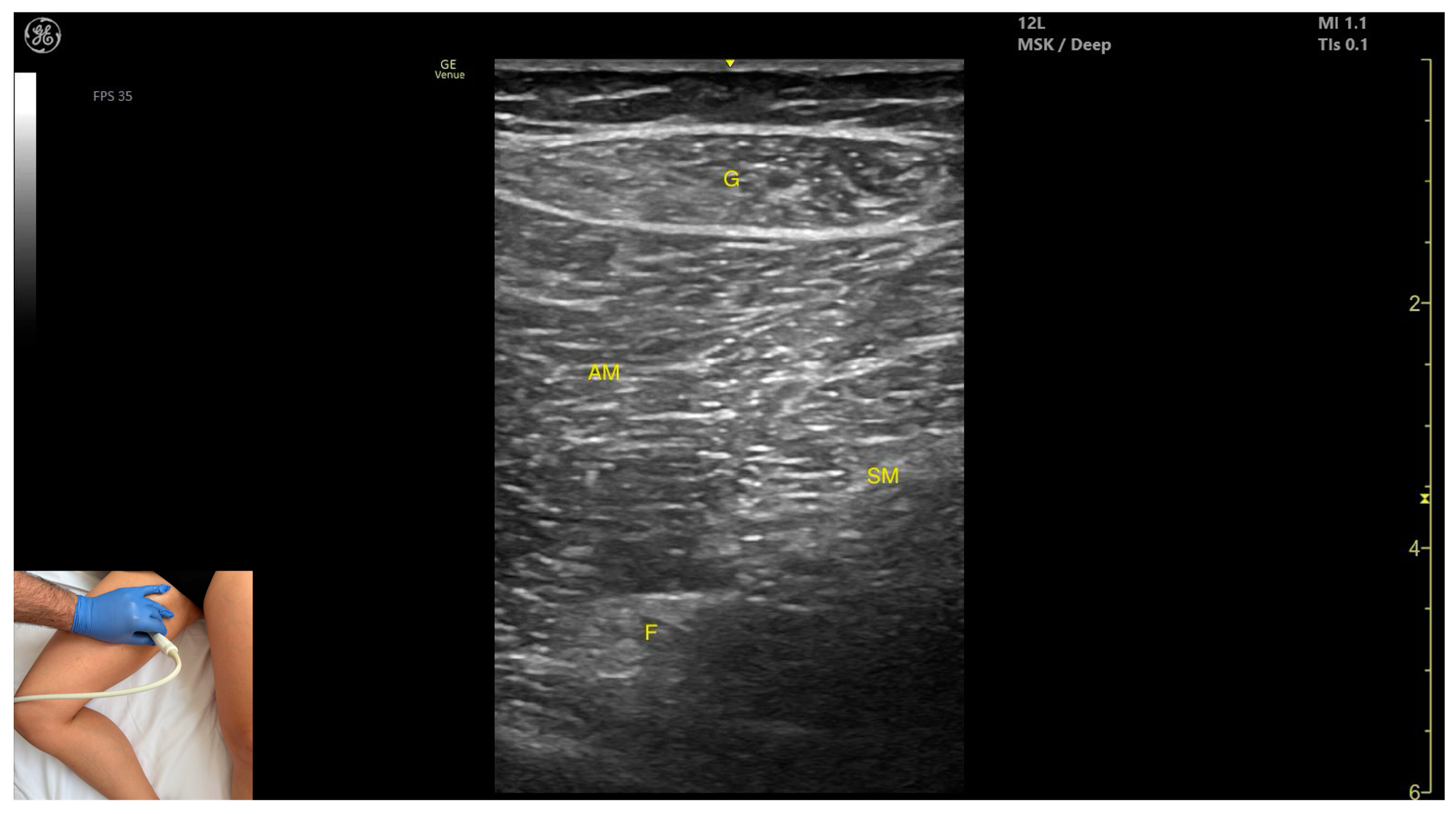
3.6. Gracilis (G)
3.6.1. Overview
3.6.2. Ultrasound Identification
3.6.3. Key Ultrasound Landmarks
- Muscle position: It is the most superficial and medial muscle mass of the thigh. Lateral and deep to the G lies the adductor longus, while medial and deep to the G lies the semimembranosus.
- External fascia: It presents a well-defined fascia that separates it from the subcutaneous plane and from the adductor magnus, adductor longus, and semimembranosus, which is relevant for BoNT-A injections.
- Dynamic evaluation: During dynamic evaluation, scanning toward the distal third of the medial thigh, the following are observed: the relationship between the G and adductor magnus remains consistent, the adductor longus disappears from view, the Sart muscle appears, joining the gracilis, and the adductor canal becomes visible, located deep and lateral to the gracilis. In the distal third of the medial thigh, the G is positioned lateral to the semitendinosus. Scanning further distally beyond the knee joint, the tendons of the G, sartorius, and semitendinosus converge to form the pes anserinus on the medial aspect of the proximal tibia. Muscle contraction is visible during hip adduction, knee flexion, and internal rotation maneuvers.
3.6.4. Clinical Implications and Injection Strategy
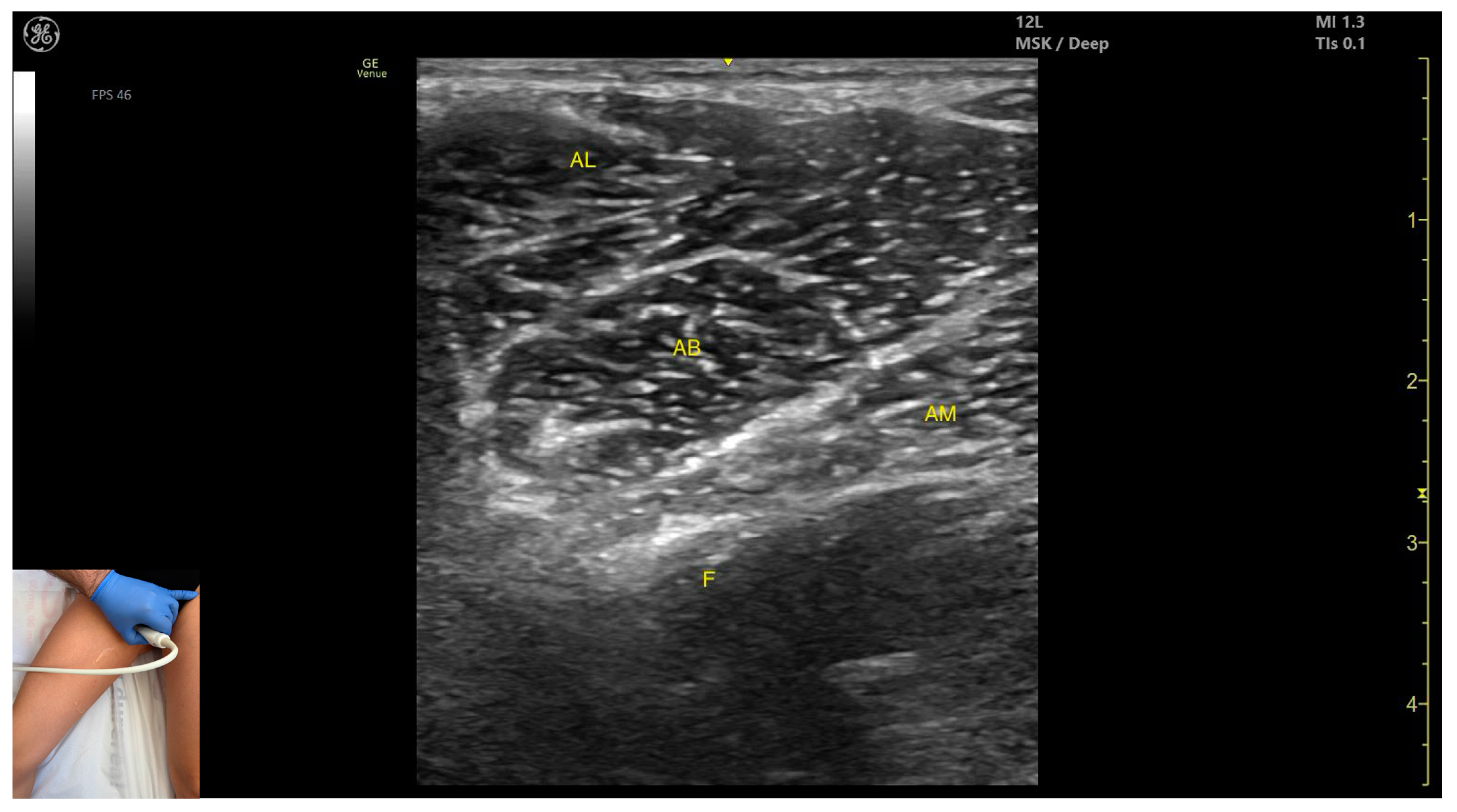
3.7. Adductor Longus (AL)
3.7.1. Overview
3.7.2. Ultrasound Identification
3.7.3. Key Ultrasound Landmarks
- Muscle position: It is the most superficial muscle mass at this level. Lateral to it lies the sartorius muscle, and medially, the gracilis muscle. The adductor canal is also visualized laterally.
- External fascia: It presents a pronounced fascia that separates it from the adductor magnus, adductor brevis, sartorius, and gracilis muscles during botulinum toxin injection.
- Dynamic evaluation: During dynamic evaluation, scanning proximally toward the hip joint, the adductor brevis, which lies deep to the adductor longus, becomes more prominent. Scanning distally toward the distal third of the medial thigh, the adductor longus gradually decreases in thickness until it disappears from view, at which point the gracilis and sartorius muscles become adjacent (Video S2). Contraction is visible during hip adduction and internal rotation maneuvers.
3.7.4. Clinical Implications and Injection Strategy
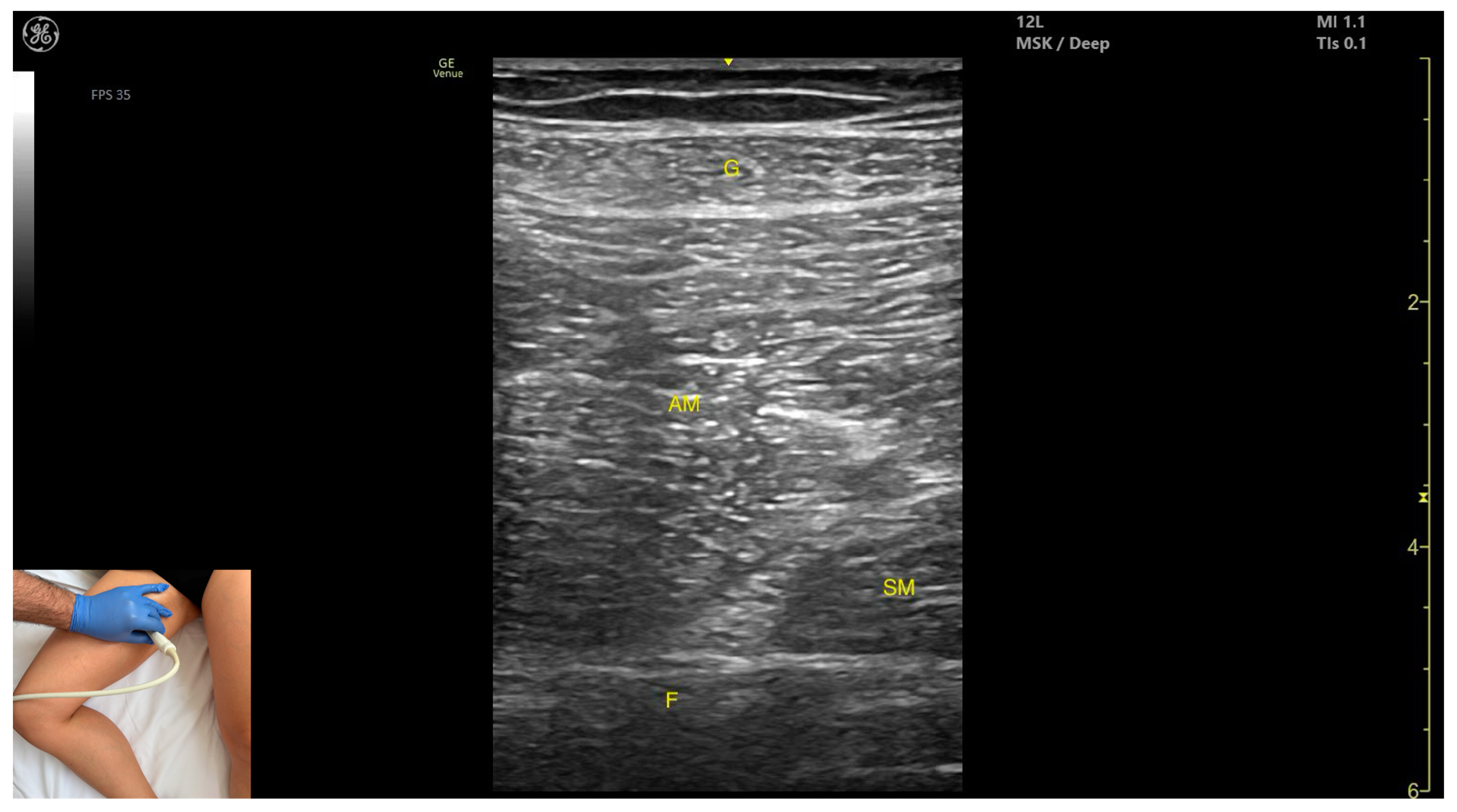
3.8. Adductor Magnus (AM)
3.8.1. Overview
3.8.2. Ultrasound Identification
3.8.3. Key Ultrasound Landmarks
- Muscle morphology: It is the largest and deepest muscle of the adductor group.
- Muscle position: It is the first muscle mass superficial to the femoral cortex at this level. It is covered superficially by the gracilis muscle; medial to it lies the semimembranosus.
- External fascia: It has a well-defined fascia separating it from the gracilis and semimembranosus, supporting safe BoNT-A injections.
- Dynamic evaluation: During dynamic evaluation, scanning distally toward the knee joint, a reduction in muscle bulk is observed in both the AM and gracilis. Muscle contraction is visible during hip adduction and hip flexion maneuvers.
3.8.4. Clinical Implications and Injection Strategy
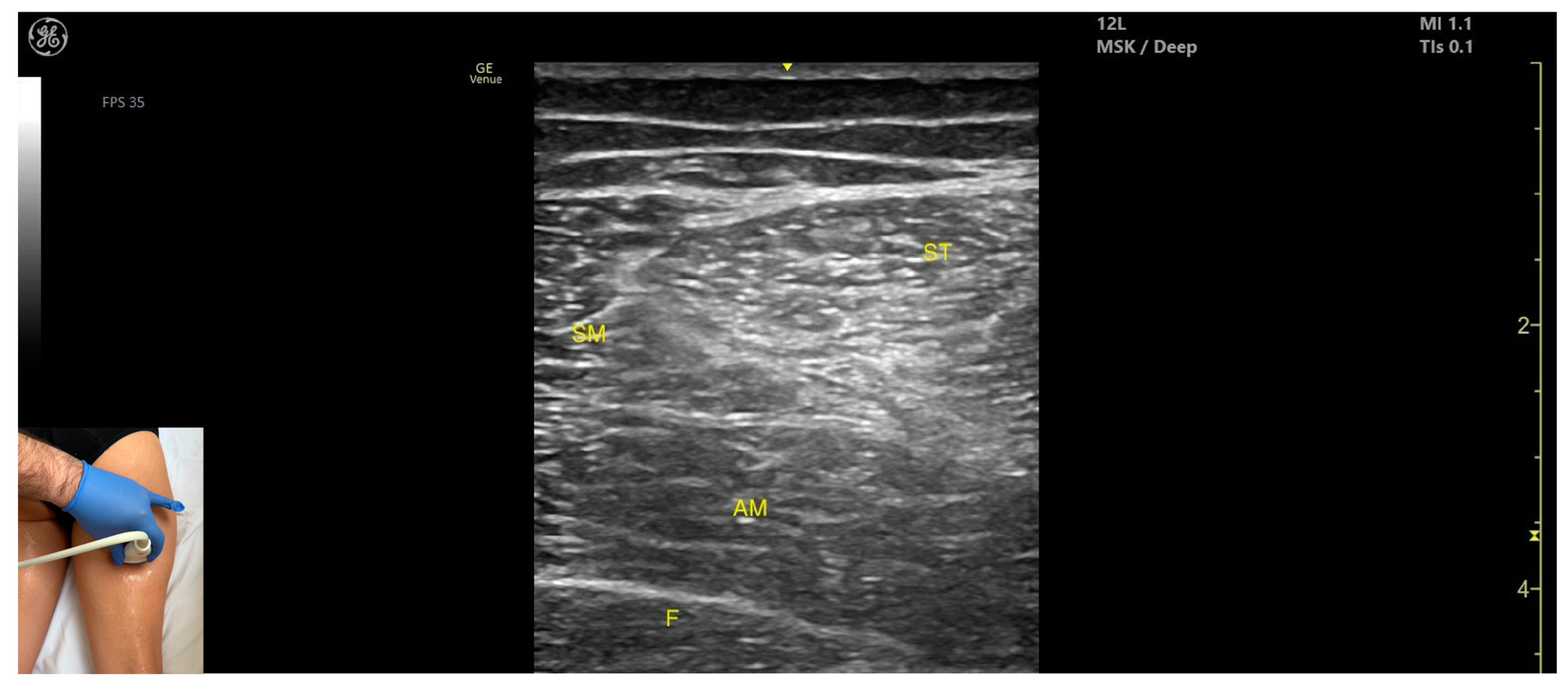
3.9. Semimembranosus (SM)
3.9.1. Overview
3.9.2. Ultrasound Identification
3.9.3. Key Ultrasound Landmarks
- Muscle position: It is a superficial muscle mass at this level. It is the first muscle seen from medial to lateral on the posterior surface of the thigh. Deep and medial to it lies the adductor magnus, while laterally to it lie the semitendinosus and biceps femoris muscles. The sciatic nerve is located deep and lateral to the SM and semitendinosus and deep to the biceps femoris. The popliteal vascular bundle is visualized deep to the muscle in the distal third of the posterior thigh.
- External fascia: It has a pronounced fascia that separates it from the subcutaneous tissue, semitendinosus, and adductor magnus, aiding in safe botulinum toxin injection.
- Dynamic evaluation: During dynamic evaluation, scanning proximally toward the hip joint, the SM decreases in thickness, while the semitendinosus increases; the sciatic nerve remains lateral and deep to the semitendinosus. Contraction is visible during hip extension, knee flexion, and the internal rotation of the leg.
3.9.4. Clinical Implications and Injection Strategy
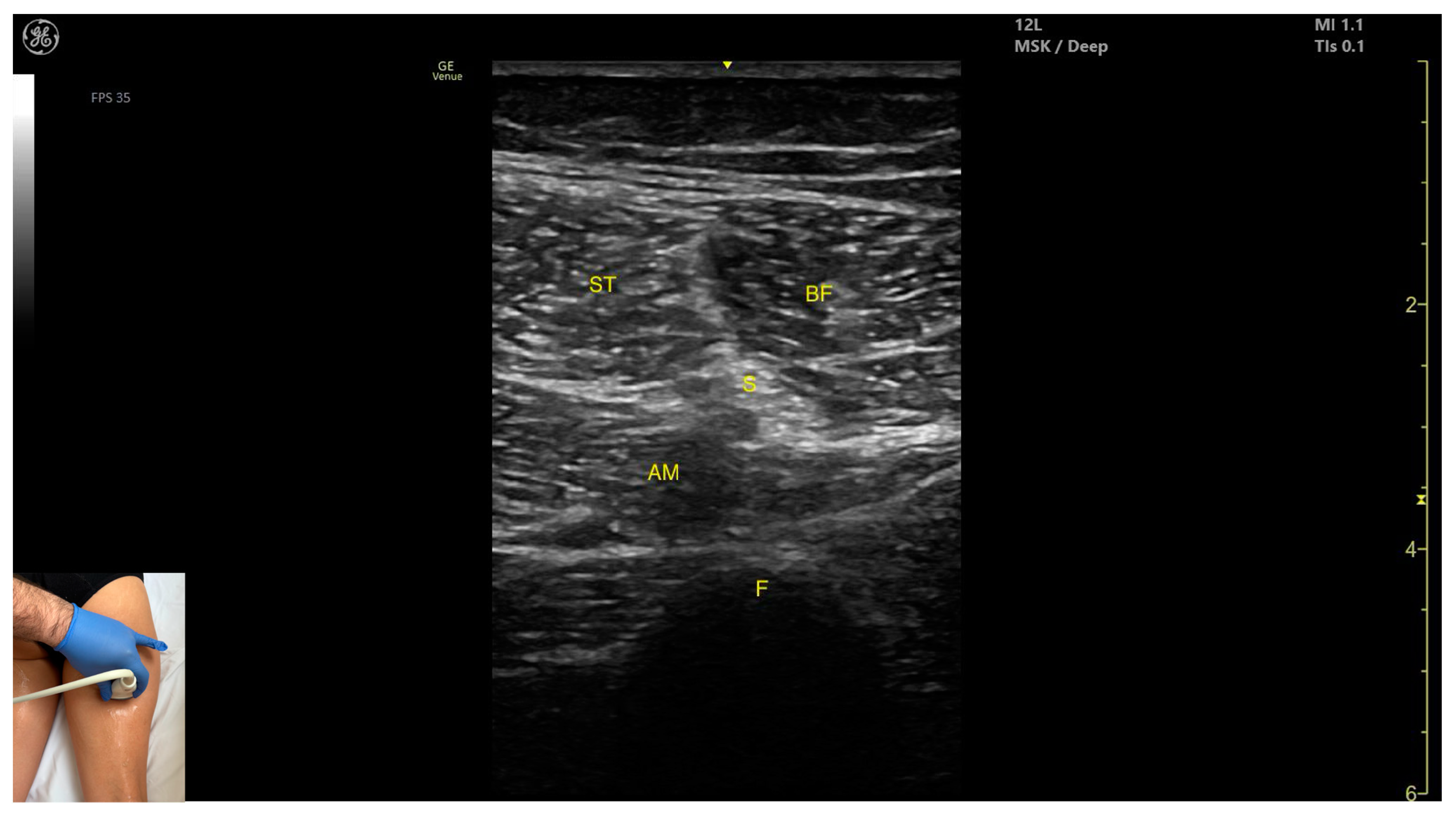
3.10. Semitendinosus (ST)
3.10.1. Overview
3.10.2. Ultrasound Identification
3.10.3. Key Ultrasound Landmarks
- Muscle position: It appears as a superficial muscle mass at this level. It is the second muscle from medial to lateral in the proximal third of the posterior thigh. It is bordered medially by the semimembranosus and laterally by the biceps femoris. The sciatic nerve lies deep and lateral to the ST and deep to the biceps femoris.
- Muscle morphology: The “Mercedes-Benz sign” may be seen—an ultrasound pattern created by the intersection of the fascial planes of the ST, biceps femoris, and adductor magnus, with the sciatic nerve centered between them. A characteristic “Venetian blind” appearance can be observed—this refers to the vertical intramuscular fascia traversing the muscle’s width. It appears as alternating hyperechoic and hypoechoic bands resembling the slats of a Venetian blind, resulting from the regular alignment of muscle fibers and connective septa reflecting ultrasound waves (Video S3).
- External fascia: It features a pronounced fascia that separates it from the subcutaneous layer, adductor magnus, semimembranosus, and biceps femoris, which is crucial for safe BoNT-A injection.
- Dynamic evaluation: During dynamic scanning distally toward the knee joint, the ST decreases in thickness, while the semimembranosus increases. The sciatic nerve maintains its course deep and lateral to the semitendinosus. Muscle contraction is visible during hip extension, knee flexion, and the internal rotation of the leg.
3.10.4. Clinical Implications and Injection Strategy
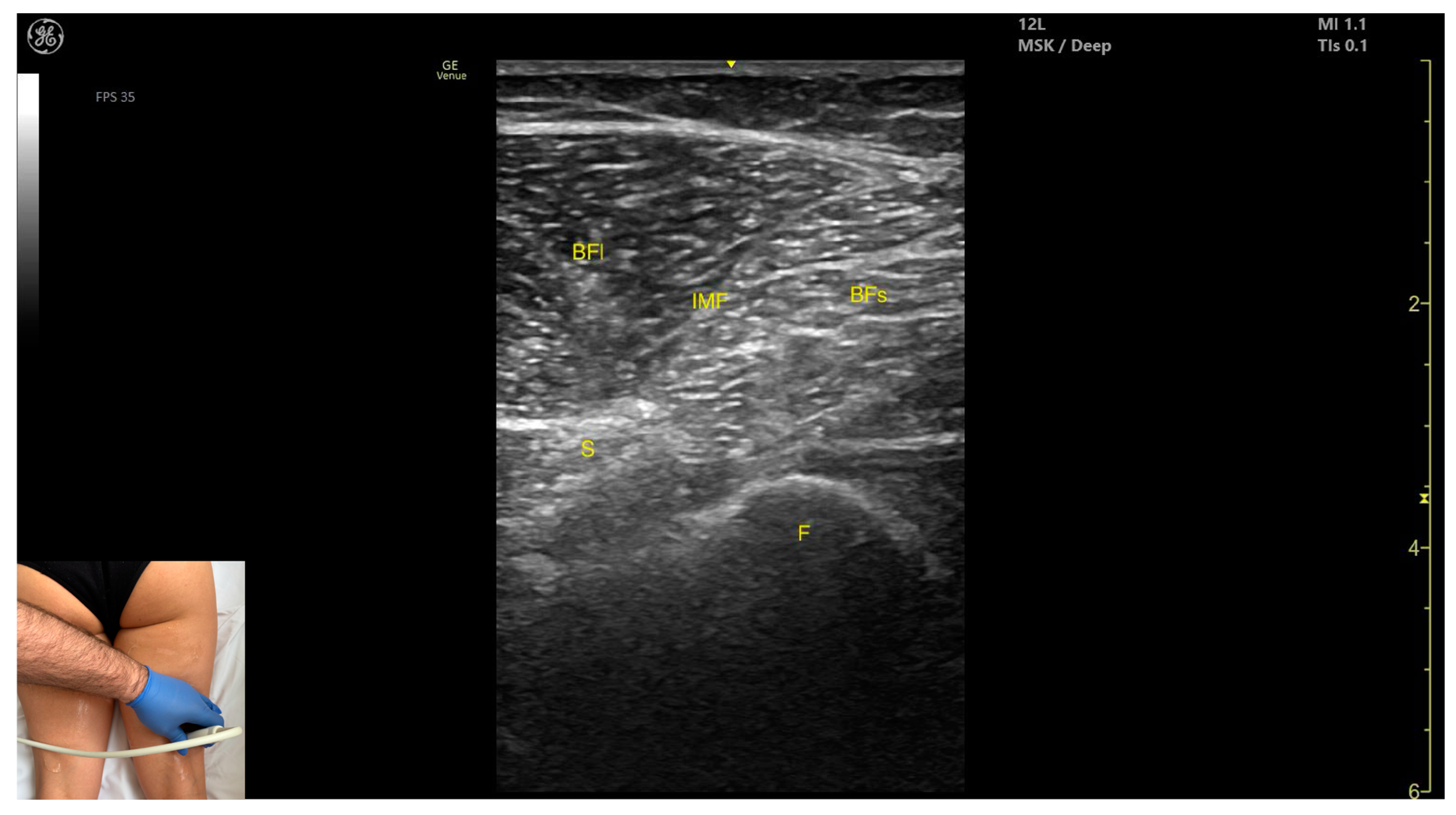
3.11. Biceps Femoris (BF)
3.11.1. Overview
3.11.2. Ultrasound Identification
3.11.3. Key Ultrasound Landmarks
- Muscle morphology: It has two heads: the long head (medial) and the short head (lateral), which can be approached individually, separated by an intramuscular fascia.
- Muscle position: It appears as a superficial muscle mass and is the most lateral muscle in the posterior (flexor) compartment of the thigh at this level. The long head lies adjacent to the sciatic nerve, which runs underneath the muscle.
- External fascia: A pronounced fascia separates the BF from the subcutaneous plane, and from the vastus lateralis and semitendinosus, which is relevant during BoNT-A injections.
- Dynamic evaluation: During dynamic evaluation, scanning proximally toward the hip joint, the long head increases in thickness while the short head decreases. At the mid-thigh, the short head disappears, and the long head reaches its maximum thickness. Scanning distally toward the knee joint, the short head increases in thickness, and the long head decreases. Muscle contraction is visible during hip extension, external rotation, knee flexion, and the external rotation of the leg.
3.11.4. Clinical Implications and Injection Strategy
- 15–30% of the reference line for the short head;
- 50–60% of the reference line for the long head.
- For the short head, the transducer is placed transversely on the distal third of the posterior-lateral thigh;
- For the long head, the transducer is placed transversely at mid-thigh level on the posterior-lateral thigh.
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Ace | Acetabulum |
| AM | Adductor magnus (muscle) |
| AB | Adductor brevis (muscle) |
| AL | Adductor longus (muscle) |
| ASIS | Anterior superior iliac spine |
| a | artery |
| BF | Biceps femoris (muscle) |
| BFs | Biceps femoris (muscle) short head |
| BFI | Biceps femoris (muscle) long head |
| BoNT-A | Botulinum toxin type-A |
| CO | Coccyx (bone) |
| EUH | Elias University Hospital |
| ES | Erector spinae (muscle) |
| FV | Femoral (vein) |
| F | Femur (bone) |
| Gmax | Gluteus maximus (muscle) |
| Gmed | Gluteus medius (muscle) |
| Gmin | Gluteus minimus (muscle) |
| G | Gracilis (muscle) |
| GT | Greater trochanter (bone) |
| I | Iliac (bone) |
| IMF | Intramuscular fascia |
| IT | Ischial tuberosity |
| NtVM | (Nerve) to vastus medialis muscle |
| PSIS | Posterior superior iliac spine |
| PM | Psoas major (muscle) |
| QL | Quadratus lumborum (muscle) |
| RF | Rectus femoris (muscle) |
| SN | Saphenous (nerve) |
| Sart | Sartorius (muscle) |
| S | Sciatic (nerve) |
| SM | Semimembranosus (muscle) |
| ST | Semitendinosus (muscle) |
| VM | Vastus medialis (muscle) |
| v | vein |
References
- Zeng, H.; Chen, J.; Guo, Y.; Tan, S. Prevalence and Risk Factors for Spasticity After Stroke: A Systematic Review and Meta-Analysis. Front. Neurol. 2021, 11, 616097. [Google Scholar] [CrossRef] [PubMed]
- Schnitzler, A.; Dince, C.; Freitag, A.; Iheanacho, I.; Fahrbach, K.; Lavoie, L.; Loze, J.-Y.; Forestier, A.; Gasq, D. Abobotulinumtoxin A Doses in Upper and Lower Limb Spasticity: A Systematic Literature Review. Toxins 2022, 14, 734. [Google Scholar] [CrossRef]
- Popescu, M.N.; Petca, R.C.; Beiu, C.; Dumitrascu, M.C.; Petca, A.; Mehedintu, C.; Farcasanu, P.D.; Sandru, F. Efficiency of Different Preparations of Botulinum Toxin Type A, Xeomin and Dysport, in the Management of Spastic Upper Limb After Stroke. Revista de Chimie 2019, 70, 3490–3494. [Google Scholar] [CrossRef]
- Popescu, M.N.; Căpeț, C.; Beiu, C.; Berteanu, M. The Elias University Hospital Approach: A Visual Guide to Ultrasound-Guided Botulinum Toxin Injection in Spasticity: Part I—Distal Upper Limb Muscles. Toxins 2025, 17, 107. [Google Scholar] [CrossRef]
- Faccioli, S.; Cavalagli, A.; Falocci, N.; Mangano, G.; Sanfilippo, I.; Sassi, S. Gait Analysis Patterns and Rehabilitative Interventions to Improve Gait in Persons with Hereditary Spastic Paraplegia: A Systematic Review and Meta-Analysis. Front. Neurol. 2023, 14, 1256392. [Google Scholar] [CrossRef] [PubMed]
- Kaymak, B.; Kara, M.; Tok, F.; Ulaşli, A.M.; Öztürk, G.T.; Chang, K.-V.; Hsiao, M.-Y.; Hung, C.-Y.; Yağiz On, A.; Özçakar, L. Sonographic Guide for Botulinum Toxin Injections of the Lower Limb: EUROMUSCULUS/USPRM Spasticity Approach. Eur. J. Phys. Rehabil. Med. 2018, 54, 486–498. [Google Scholar] [CrossRef] [PubMed]
- Sinnatamby, C.S. Last’s Anatomy: Regional and Applied, 12th ed.; Elsevier: Amsterdam, The Netherlands, 2011. [Google Scholar]
- Palastanga, N.; Soames, R. Anatomy and Human Movement Structure and Function, 7th ed.; Elsevier: Warsaw, Poland, 2019; ISBN 978-0-7020-7226-0. [Google Scholar]
- Elzanie, A.; Borger, J. Anatomy, Bony Pelvis and Lower Limb, Gluteus Maximus Muscle. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Jankovic, J.; Albanese, A.; Atassi, M.Z.; Dolly, J.O.; Hallett, M.; Mayer, N.H. Botulinum Toxin E-Book: Therapeutic Clinical Practice and Science; Elsevier: Amsterdam, The Netherlands, 2009. [Google Scholar]
- Intiso, D.; Basciani, M. Botulinum Toxin Type A in the Healing of a Chronic Buttock Ulcer in a Patient with Spastic Paraplegia after Spinal Cord Injury. J. Rehabil. Med. 2009, 41, 1100–1102. [Google Scholar] [CrossRef]
- Cigna, E.; Maruccia, M.; Fanelli, B.; Scuderi, N. Botulinum Toxin Type A in the Healing of Chronic Lesion Following Bilateral Spasticity of Gluteus Muscle. Int. Wound J. 2014, 11, 412–415. [Google Scholar] [CrossRef]
- Bhave, A.; Zywiel, M.G.; Ulrich, S.D.; McGrath, M.S.; Seyler, T.M.; Marker, D.R.; Delanois, R.E.; Mont, M.A. Botulinum Toxin Type A Injections for the Management of Muscle Tightness Following Total Hip Arthroplasty: A Case Series. J. Orthop. Surg. Res. 2009, 4, 34. [Google Scholar] [CrossRef]
- Bertoni, M.; Castagna, A.; Baricich, A.; Berti, G.; Lazzaretti, S.; Morandi, C. Administration of Type A Botulinum Toxin after Total Hip Replacement. Eur. J. Phys. Rehabil. Med. 2008, 44, 461–465. [Google Scholar]
- Yi, K.-H.; Kim, D.C.; Lee, S.; Lee, H.-J.; Lee, J.-H. Intramuscular Neural Distribution of the Gluteus Maximus Muscle: Diagnostic Electromyography and Injective Treatments. Diagnostics 2024, 14, 140. [Google Scholar] [CrossRef] [PubMed]
- Drake, R.L.; Vogl, A.W.; Mitchell, A.W.M. Gray’s Anatomy for Students; Elsevier: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Chang, C.; Jeno, S.H.; Varacallo, M.A. Anatomy, Bony Pelvis and Lower Limb: Piriformis Muscle. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Lang, A.M. Botulinum Toxin Type B in Piriformis Syndrome. Am. J. Phys. Med. Rehabil. 2004, 83, 198–202. [Google Scholar] [CrossRef]
- Yoon, S.J.; Ho, J.; Kang, H.Y.; Lee, S.H.; Kim, K.I.; Shin, W.G.; Oh, J.M. Low-Dose Botulinum Toxin Type A for the Treatment of Refractory Piriformis Syndrome. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2007, 27, 657–665. [Google Scholar] [CrossRef]
- Yan, K.; Xi, Y.; Hlis, R.; Chhabra, A. Piriformis Syndrome: Pain Response Outcomes Following CT-Guided Injection and Incremental Value of Botulinum Toxin Injection. Diagn. Interv. Radiol. 2021, 27, 126–133. [Google Scholar] [CrossRef]
- Al-Al-Shaikh, M.; Michel, F.; Parratte, B.; Kastler, B.; Vidal, C.; Aubry, S. An MRI Evaluation of Changes in Piriformis Muscle Morphology Induced by Botulinum Toxin Injections in the Treatment of Piriformis Syndrome. Diagn. Interv. Imaging 2015, 96, 37–43. [Google Scholar] [CrossRef]
- Yi, K.-H.; Lee, K.-L.; Lee, J.-H.; Hu, H.-W.; Lee, K.; Seo, K.K.; Kim, H.-J. Guidelines for Botulinum Neurotoxin Injections in Piriformis Syndrome. Clin. Anat. 2021, 34, 1028–1034. [Google Scholar] [CrossRef] [PubMed]
- Moore, K.L.; Agur, A.M.R.; Dalley, A.F. Clinically Oriented Anatomy, 8th ed.; Keith, L.M., Arthur, F.D., II, Anne, M.R.A., Eds.; Wolters Kluwer: Albany, NY, USA, 2018. [Google Scholar]
- Sconfienza, L.M.; Perrone, N.; Lacelli, F.; Lentino, C.; Serafini, G. Ultrasound-Guided Injection of Botulinum Toxin A in the Treatment of Iliopsoas Spasticity. J. Ultrasound 2008, 11, 113–117. [Google Scholar] [CrossRef]
- Campenhout, A.V.; Hubens, G.; Fagard, K.; Molenaers, G. Localization of Motor Nerve Branches of the Human Psoas Muscle. Muscle Nerve 2010, 42, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Boudarham, J.; Hameau, S.; Pradon, D.; Bensmail, D.; Roche, N.; Zory, R. Changes in Electromyographic Activity after Botulinum Toxin Injection of the Rectus Femoris in Patients with Hemiparesis Walking with a Stiff-Knee Gait. J. Electromyogr. Kinesiol. 2013, 23, 1036–1043. [Google Scholar] [CrossRef]
- Santamato, A.; Cinone, N.; Panza, F.; Letizia, S.; Santoro, L.; Lozupone, M.; Daniele, A.; Picelli, A.; Baricich, A.; Intiso, D.; et al. Botulinum Toxin Type A for the Treatment of Lower Limb Spasticity after Stroke. Drugs 2019, 79, 143–160. [Google Scholar] [CrossRef]
- Stoquart, G.G.; Detrembleur, C.; Palumbo, S.; Deltombe, T.; Lejeune, T.M. Effect of Botulinum Toxin Injection in the Rectus Femoris on Stiff-Knee Gait in People With Stroke: A Prospective Observational Study. Arch. Phys. Med. Rehabil. 2008, 89, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Robertson, J.V.G.; Pradon, D.; Bensmail, D.; Fermanian, C.; Bussel, B.; Roche, N. Relevance of Botulinum Toxin Injection and Nerve Block of Rectus Femoris to Kinematic and Functional Parameters of Stiff Knee Gait in Hemiplegic Adults. Gait Posture 2009, 29, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Tok, F.; Balaban, B.; Yaşar, E.; Alaca, R.; Tan, A.K. The Effects of Onabotulinum Toxin A Injection into Rectus Femoris Muscle in Hemiplegic Stroke Patients with Stiff-Knee Gait. Am. J. Phys. Med. Rehabil. 2012, 91, 321–326. [Google Scholar] [CrossRef]
- Lampire, N.; Roche, N.; Carne, P.; Cheze, L.; Pradon, D. Effect of Botulinum Toxin Injection on Length and Lengthening Velocity of Rectus Femoris during Gait in Hemiparetic Patients. Clin. Biomech. 2013, 28, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Supiot, A.; Geiger, M.; Bensmail, D.; Aegerter, P.; Pradon, D.; Roche, N. Effect of Botulinum Toxin Injection on Length and Force of the Rectus Femoris and Triceps Surae Muscles during Locomotion in Patients with Chronic Hemiparesis (FOLOTOX). BMC Neurol. 2018, 18, 104. [Google Scholar] [CrossRef]
- Botter, A.; Oprandi, G.; Lanfranco, F.; Allasia, S.; Maffiuletti, N.A.; Minetto, M.A. Atlas of the Muscle Motor Points for the Lower Limb: Implications for Electrical Stimulation Procedures and Electrode Positioning. Eur. J. Appl. Physiol. 2011, 111, 2461–2471. [Google Scholar] [CrossRef]
- Andersen, H.L.; Andersen, S.L.; Tranum-Jensen, J. The Spread of Injectate during Saphenous Nerve Block at the Adductor Canal: A Cadaver Study. Acta Anaesthesiol. Scand. 2015, 59, 238–245. [Google Scholar] [CrossRef]
- Netter, F.H. Atlas of Human Anatomy, 6th ed.; Elsevier: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Yi, K.-H.; Lee, J.-H.; Lee, D.K.; Hu, H.-W.; Seo, K.K.; Kim, H.-J. Anatomical Locations of the Motor Endplates of Sartorius Muscle for Botulinum Toxin Injections in Treatment of Muscle Spasticity. Surg. Radiol. Anat. 2021, 43, 2025–2030. [Google Scholar] [CrossRef]
- Campenhout, A.V.; Bar-On, L.; Desloovere, K.; Huenaerts, C.; Molenaers, G. Motor Endplate-targeted Botulinum Toxin Injections of the Gracilis Muscle in Children with Cerebral Palsy. Dev. Med. Child Neurol. 2015, 57, 476–483. [Google Scholar] [CrossRef]
- Won, S.-Y.; Rha, D.-W.; Kim, H.-S.; Jung, S.-H.; Park, E.S.; Hu, K.-S.; Kim, H.-J. Intramuscular Nerve Distribution Pattern of the Adductor Longus and Gracilis Muscles Demonstrated with Sihler Staining: Guidance for Botulinum Toxin Injection. Muscle Nerve 2012, 46, 80–85. [Google Scholar] [CrossRef]
- Albert, A.M.; Magimairaj, H.P.; Lakshmanan, J.; Holla, S.J.; Prithishkumar, I.J. Localizing Motor Entry Points of Adductor Muscles of Thigh for Motor Point Procedures in the Treatment of Adductor Spasticity. Anat. Cell Biol. 2024, 57, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Lee, S.; Jang, J.; Lim, J.; Ryu, J.S. Effect of Botulinum Toxin Injection on the Progression of Hip Dislocation in Patients with Spastic Cerebral Palsy: A Pilot Study. Toxins 2021, 13, 872. [Google Scholar] [CrossRef]
- Santamato, A.; Ranieri, M.; Panza, F.; Solfrizzi, V.; Frisardi, V.; Lapenna, L.M.; Moretti, B.; Fiore, P. Botulinum Toxin Type a in the Treatment of Painful Adductor Muscle Contracture After Total Hip Arthroplasty. Orthopedics 2009, 32, 774–776. [Google Scholar] [CrossRef]
- Campenhout, A.V.; Molenaers, G. Localization of the Motor Endplate Zone in Human Skeletal Muscles of the Lower Limb: Anatomical Guidelines for Injection with Botulinum Toxin. Dev. Med. Child Neurol. 2011, 53, 108–119. [Google Scholar] [CrossRef]
- Giuffre, B.A.; Black, A.C.; Jeanmonod, R. Anatomy, Sciatic Nerve; StatPearls: Treasure Island, FL, USA, 2025. [Google Scholar]
- Kim, S.K.; Rha, D.W.; Park, E.S. Botulinum Toxin Type A Injections Impact Hamstring Muscles and Gait Parameters in Children with Flexed Knee Gait. Toxins 2020, 12, 145. [Google Scholar] [CrossRef]
- Rha, D.-W.; Yi, K.-H.; Park, E.S.; Park, C.; Kim, H.-J. Intramuscular Nerve Distribution of the Hamstring Muscles: Application to Treating Spasticity. Clin. Anat. 2016, 29, 746–751. [Google Scholar] [CrossRef] [PubMed]
- Jačisko, J.; Mezian, K.; Güvener, O.; Ricci, V.; Kobesová, A.; Özçakar, L. Mnemonics and Metaphorical Videos for Teaching/Learning Musculoskeletal Sonoanatomy. Am. J. Phys. Med. Rehabil. 2022, 101, e189–e193. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.-T.; Chang, K.-V. A 42-Year-Old Man with Posterior Thigh Pain: Injury of the Long Head of the Biceps Femoris Muscle. J. Med. Ultrasound 2023, 31, 256–257. [Google Scholar] [CrossRef]
- Oremuš, K. Ultrasound Skills in Lower Extremity Traumatology and Orthopedics—Regional Anesthesia and Beyond. Acta Clin. Croat. 2019, 58 (Suppl. S1), 74–80. [Google Scholar] [CrossRef]
- Mezian, K.; Ricci, V.; Güvener, O.; Jačisko, J.; Novotný, T.; Kara, M.; Chang, K.-V.; Naňka, O.; Pirri, C.; Stecco, C.; et al. EURO-MUSCULUS/USPRM Dynamic Ultrasound Protocols for (Adult) Hip. Am. J. Phys. Med. Rehabil. 2022, 101, e162–e168. [Google Scholar] [CrossRef]
- Saladin, K.S. Anatomy Physiology: The Unity of Form and Function, 9th ed.; McGraw Hill: New York, NY, USA, 2021. [Google Scholar]

| Muscle | Key Anatomical Landmarks | Nearby Structures at Risk | Ultrasound Technique Tip | Injection Precautions |
|---|---|---|---|---|
| Gluteus Maximus | Upper gluteal region; 8 cm lateral to sacrum | Gluteus medius and minimus (deep); sciatic nerve (potentially) | Scan angled at 45° toward the sacrum | Avoid sciatic nerve injury |
| Piriformis | 8 cm lateral to sacrum; 10 cm proximal to the ischial tuberosity | Gluteus maximus (superficial); sciatic nerve (deep to muscle) | Transverse scan angled ~20° laterally toward the sacrum | Visualize piriformis and sciatic nerve; avoid nerve injury |
| Psoas Major | 2 cm lateral to L4 spinous process; 1 cm proximal to the iliac crest | Erector spinae muscles; quadratus lumborum (superficial); intraperitoneal space (deep to the muscle) | Transverse or longitudinal scan on posterior trunk | Avoid intraperitoneal space; inject only when muscle is clearly visualized |
| Rectus Femoris | Proximal third of anterior thigh; midline | Vastus intermedius (deep) | Transverse scan on anterior thigh | Avoid central tendon |
| Sartorius | Middle third of medial thigh | Adductor canal (deep)—femoral artery, vein, saphenous nerve, and nerve to vastus medialis; vastus medialis (deep and lateral) and adductor longus (deep and medial) | Transverse scan on medial thigh | Avoid structures in adductor canal |
| Gracilis | Proximal third of medial thigh | Adductor longus (deep and lateral), adductor magnus (deep), and semimembranosus (deep and medial) | Transverse scan with the hip abducted, externally rotated, and semi-flexed and the knee in semi-flexion | Visualize gracilis as most superficial medial muscle |
| Adductor Longus | Proximal third of medial thigh | Gracilis (medial), sartorius (lateral), adductor canal (lateral), and adductor brevis (deep) | Transverse scan on upper medial thigh | Confirm muscle position and relations, avoid structures in adductor canal |
| Adductor Magnus | Proximal third of medial thigh | Gracilis (superficial) and semimembranosus (medial) | Transverse scan with the hip abducted, externally rotated, and semi-flexed and the knee in semi-flexion | Identify deep muscle mass below gracilis |
| Semimembranosus | Distal third of posterior medial thigh | Semitendinosus (lateral), adductor magnus (deep and medial), sciatic nerve (deep and lateral), and popliteal bundle (deep) | Transverse scan on posterior medial thigh | Avoid neurovascular structures in distal thigh |
| Semitendinosus | Proximal third of posterior medial thigh | Semimembranosus (medial), biceps femoris (lateral), adductor magnus (deep), and sciatic nerve (deep and lateral) | Transverse scan on posterior thigh | Visualize characteristic ’Mercedes-Benz’ and ’Venetian blind’ signs, avoid nerve injury |
| Biceps Femoris | Distal third of posterior-lateral thigh (short head); mid-thigh for long head | Sciatic nerve (under long head) | Transverse scan at two levels on posterior thigh | Identify and differentiate long and short heads and avoid nerve injury |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Popescu, M.N.; Căpeț, C.; Beiu, C.; Berteanu, M. The Elias University Hospital Approach: A Visual Guide to Ultrasound-Guided Botulinum Toxin Injection in Spasticity: Part III—Proximal Lower Limb Muscles. Toxins 2025, 17, 240. https://doi.org/10.3390/toxins17050240
Popescu MN, Căpeț C, Beiu C, Berteanu M. The Elias University Hospital Approach: A Visual Guide to Ultrasound-Guided Botulinum Toxin Injection in Spasticity: Part III—Proximal Lower Limb Muscles. Toxins. 2025; 17(5):240. https://doi.org/10.3390/toxins17050240
Chicago/Turabian StylePopescu, Marius Nicolae, Claudiu Căpeț, Cristina Beiu, and Mihai Berteanu. 2025. "The Elias University Hospital Approach: A Visual Guide to Ultrasound-Guided Botulinum Toxin Injection in Spasticity: Part III—Proximal Lower Limb Muscles" Toxins 17, no. 5: 240. https://doi.org/10.3390/toxins17050240
APA StylePopescu, M. N., Căpeț, C., Beiu, C., & Berteanu, M. (2025). The Elias University Hospital Approach: A Visual Guide to Ultrasound-Guided Botulinum Toxin Injection in Spasticity: Part III—Proximal Lower Limb Muscles. Toxins, 17(5), 240. https://doi.org/10.3390/toxins17050240







