Complexing Protein-Free Botulinum Neurotoxin A Formulations: Implications of Excipients for Immunogenicity
Abstract
1. Introduction
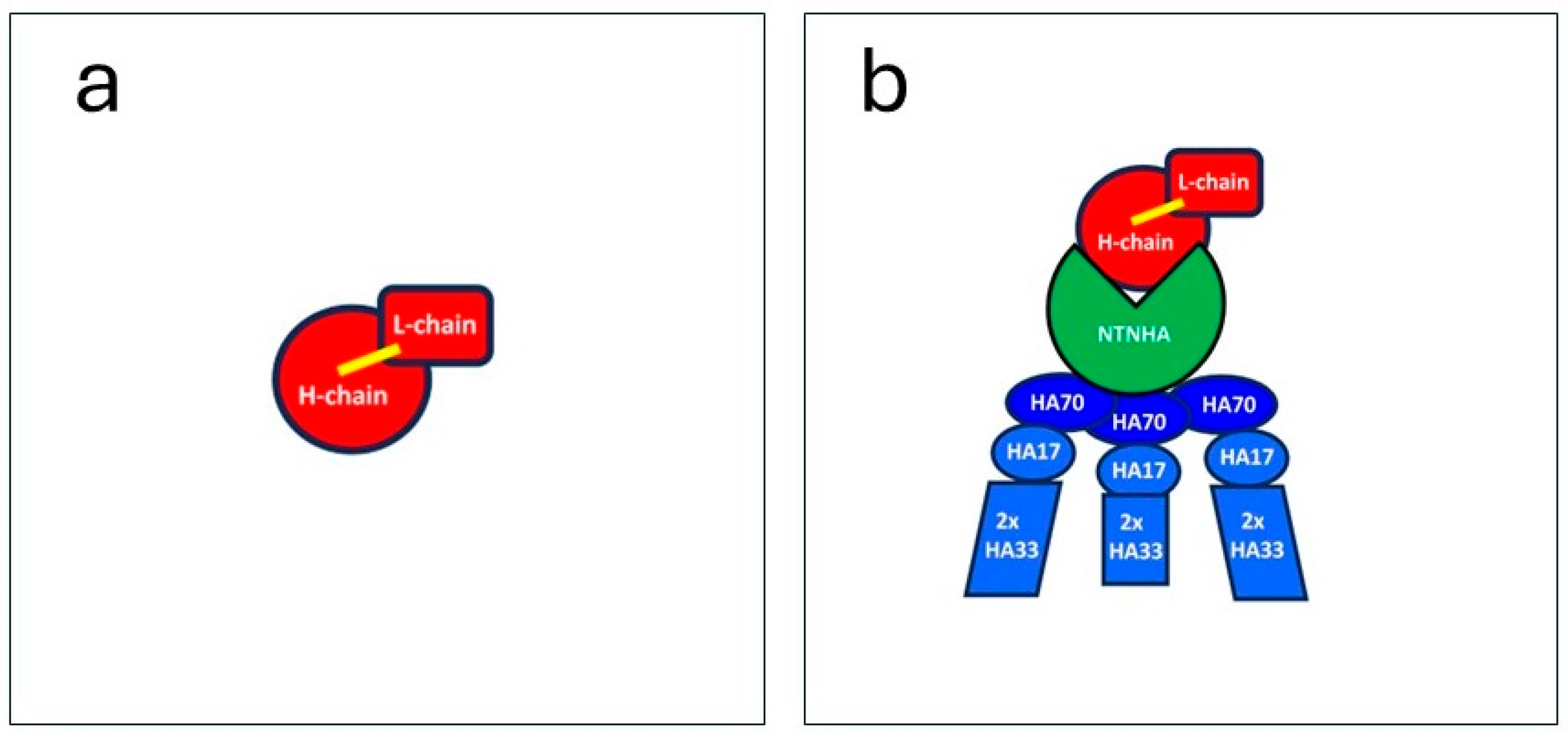
1.1. Natural Botulinum Neurotoxin A (BoNT/A) Comes as a Large Complex
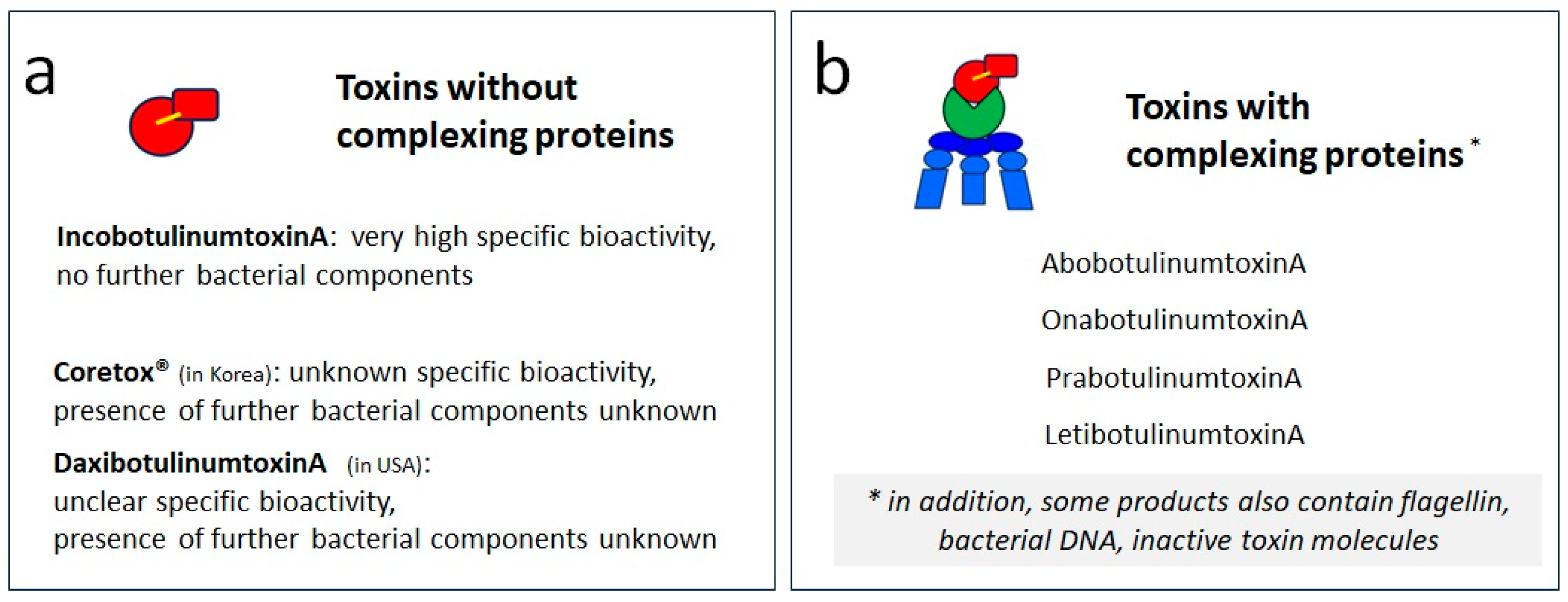
1.2. The Pharmaceutical Formulations of BoNT/A Differ in Purity and Excipients
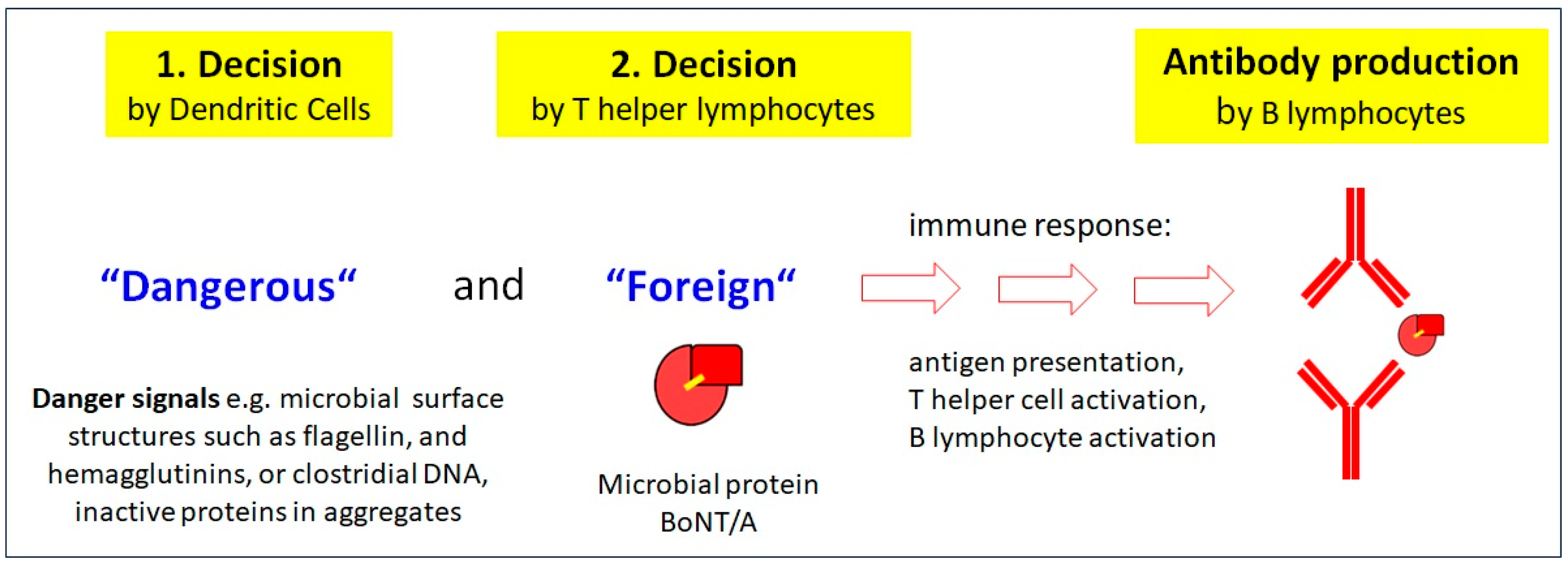
2. Immunological Consequences of Impurities in a BoNT/A Formulation
2.1. Importance of Purity for BoNT/A
2.2. Neutralizing Antibodies to BoNT/A
2.3. Why and How the Immune System Responds to Injections with BoNT/A
3. Complexing Protein-Free (CPF) BoNT/A Preparations
3.1. Three BoNT/A Formulations Are Free of Complexing Proteins but They Are Not the Same
3.2. General Considerations on Excipients in Pharma Protein Preparations
3.3. A Review of Excipients in CPF BoNT/A Formulations
3.3.1. Human Serum Albumin (HSA)
3.3.2. Sucrose
3.3.3. L-Histidine/L-Histidine-HCl
3.3.4. Trehalosedihydrate
3.3.5. Polysorbate 20 (Polyoxyethylene (20) Sorbitan Monolaurate)
3.3.6. RTP004 Peptide
Possible Effects on Immunogenicity
3.3.7. L-Methionine
3.3.8. NaCl
4. Potential Influence of Excipients on the Specific Bioactivity of BoNT/A Products and the Relevance for Immunogenicity
4.1. Specific Bioactivity of BoNT/A Formulations
4.2. Measuring Protein and the Relative Content of Active and Inactive BoNT/A Molecules
4.3. Inactive Proteins Are Not Irrelevant in a BoNT/A Formulation as They May Increase Its Immunogenicity
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rawson, A.M.; Dempster, A.W.; Humphreys, C.M.; Minton, N.P. Pathogenicity and virulence of Clostridium botulinum. Virulence 2023, 14, 2205251. [Google Scholar] [CrossRef]
- Gu, S.; Jin, R. Assembly and function of the botulinum neurotoxin progenitor complex. Curr. Top. Microbiol. Immunol. 2013, 364, 21–44. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Gu, S.; Jin, L.; Le, T.T.; Cheng, L.W.; Strotmeier, J.; Kruel, A.M.; Yao, G.; Perry, K.; Rummel, A.; et al. Structure of a bimodular botulinum neurotoxin complex provides insights into its oral toxicity. PLoS Pathog. 2013, 9, e1003690. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Zhong, X.; Gu, S.; Kruel, A.M.; Dorner, M.B.; Perry, K.; Rummel, A.; Dong, M.; Jin, R. Molecular basis for disruption of E-cadherin adhesion by botulinum neurotoxin A complex. Science 2014, 344, 1405–1410. [Google Scholar] [CrossRef]
- Matsui, T.; Gu, S.; Lam, K.H.; Carter, L.G.; Rummel, A.; Mathews, I.I.; Jin, R. Structural basis of the pH-dependent assembly of a botulinum neurotoxin complex. J. Mol. Biol. 2014, 426, 3773–3782. [Google Scholar] [CrossRef] [PubMed]
- Poulain, B. La neurotoxine botulinique [Botulinum neurotoxin]. Rev. Neurol. 2010, 166, 7–20. [Google Scholar] [CrossRef]
- Eisele, K.H.; Fink, K.; Vey, M.; Taylor, H.V. Studies on the dissociation of botulinum neurotoxin type A complexes. Toxicon 2011, 57, 555–565. [Google Scholar] [CrossRef]
- Frevert, J. Xeomin is free from complexing proteins. Toxicon 2009, 54, 697–701. [Google Scholar] [CrossRef]
- FDA Prescribing Information Xeomin/IncobotulinumtoxinA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/125360s073lbl.pdf (accessed on 6 December 2023).
- Medytox Homepage. Available online: https://www.medytox.com/page/coretox_en?site_id=en (accessed on 6 December 2023).
- Revance Aesthetics. Available online: https://hcp.daxxify.com/daxxify-difference (accessed on 1 December 2023).
- FDA Prescribing Information DAXXIFY/DaxibotulinumtoxinA-lanm. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/761127s000lbl.pdf (accessed on 6 December 2023).
- FDA Center for Evaluation and Research. “Dysport/AbobotulinumtoxinA”. 2009. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2009/125274Orig1s000MedR.pdf (accessed on 6 December 2023).
- FDA Prescribing Information Botox/OnabotulinumtoxinA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/103000s5236lbl.pdf (accessed on 6 December 2023).
- FDA Prescribing Information Jeuveau/PrabotulinumtoxinA-xvfs. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761085s000lbl.pdf (accessed on 6 December 2023).
- TGA Australian Product Information Letybo®/LetibotulinumtoxinA. Available online: https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent=&id=CP-2022-PI-02402-1&d=20231207172310101&d=20231208172310101 (accessed on 6 December 2023).
- Frevert, J.; Ahn, K.Y.; Park, M.Y.; Sunga, O. Comparison of botulinum neurotoxin type A formulations in Asia. Clin. Cosmet. Investig. Dermatol. 2018, 11, 327–331. [Google Scholar] [CrossRef]
- Park, J.Y.; Sunga, O.; Wanitphakdeedecha, R.; Frevert, J. Neurotoxin Impurities: A Review of Threats to Efficacy. Plast. Reconstr. Surg. Glob. Open 2020, 8, e2627. [Google Scholar] [CrossRef]
- Zhang, L.; Lin, W.J.; Li, S.; Aoki, K.R. Complete DNA sequences of the botulinum neurotoxin complex of Clostridium botulinum type A-Hall (Allergan) strain. Gene 2003, 315, 21–32, Erratum in Gene 2003, 322, 187. [Google Scholar] [CrossRef] [PubMed]
- Panjwani, N.; O‘Keeffe, R.; Pickett, A. Biochemical, functional and potency characteristics of type A botulinum toxin in clinical use. Botulinum J. 2008, 1, 153–166. [Google Scholar] [CrossRef]
- Frevert, J.; Grönewald, C. Presence of clostridial DNA in botulinum toxin products. Toxicon 2015, 93, S28. [Google Scholar] [CrossRef]
- Frevert, J. Pharmaceutical, biological, and clinical properties of botulinum neurotoxin type A products. Drugs R D 2015, 15, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ho, W.W.S.; Albrecht, P.; Calderon, P.E.; Corduff, N.; Loh, D.; Martin, M.U.; Park, J.Y.; Suseno, L.S.; Tseng, F.W.; Vachiramon, V.; et al. Emerging Trends in Botulinum Neurotoxin A Resistance: An International Multidisciplinary Review and Consensus. Plast. Reconstr. Surg. Glob. Open 2022, 10, e4407. [Google Scholar] [CrossRef] [PubMed]
- Wissel, J.; Bensmail, D.; Ferreira, J.J.; Molteni, F.; Satkunam, L.; Moraleda, S.; Rekand, T.; McGuire, J.; Scheschonka, A.; Flatau-Baqué, B.; et al. Safety and efficacy of incobotulinumtoxinA doses up to 800 U in limb spasticity: The TOWER study. Neurology 2017, 88, 1321–1328. [Google Scholar] [CrossRef]
- Albrecht, P.; Jansen, A.; Lee, J.I.; Moll, M.; Ringelstein, M.; Rosenthal, D.; Bigalke, H.; Aktas, O.; Hartung, H.P.; Hefter, H. High prevalence of neutralizing antibodies after long-term botulinum neurotoxin therapy. Neurology 2022, 92, e48–e54, Erratum in Neurology 2022, 98, 341. [Google Scholar] [CrossRef]
- Walter, U.; Mühlenhoff, C.; Benecke, R.; Dressler, D.; Mix, E.; Alt, J.; Wittstock, M.; Dudesek, A.; Storch, A.; Kamm, C. Frequency and risk factors of antibody-induced secondary failure of botulinum neurotoxin therapy. Neurology 2020, 94, e2109–e2120, Erratum in Neurology 2020, 95, 802. [Google Scholar] [CrossRef]
- Dressler, D.; Bigalke, H.; Frevert, J. The immunology of botulinum toxin therapy: A brief summary. Toxicology 2022, 481, 153341. [Google Scholar] [CrossRef]
- Park, J.Y.; Corduff, N.; Frevert, J.; Wanitphakdeedecha, R.; Chao, Y.Y.Y. Immunogenicity Associated with Aesthetic Botulinumtoxin A: A Survey of Asia-Pacific Physicians’ Experiences and Recommendations. Plast. Reconstr. Surg. Glob. Open 2022, 10, e4217. [Google Scholar] [CrossRef]
- Hefter, H.; Rosenthal, D.; Jansen, A.; Brauns, R.; Ürer, B.; Bigalke, H.; Hartung, H.P.; Meuth, S.G.; Lee, J.I.; Albrecht, P.; et al. Significantly lower antigenicity of incobotulinumtoxin than abo- or onabotulinumtoxin. J. Neurol. 2023, 270, 788–796. [Google Scholar] [CrossRef]
- Fabbri, M.; Leodori, G.; Fernandes, R.M.; Bhidayasiri, R.; Marti, M.J.; Colosimo, C.; Ferreira, J.J. Neutralizing Antibody and Botulinum Toxin Therapy: A Systematic Review and Meta-analysis. Neurotox. Res. 2016, 29, 105–117. [Google Scholar] [CrossRef]
- Bellows, S.; Jankovic, J. Immunogenicity Associated with Botulinum Toxin Treatment. Toxins 2019, 11, 491. [Google Scholar] [CrossRef] [PubMed]
- Carr, W.W.; Jain, N.; Sublett, J.W. Immunogenicity of Botulinum Toxin Formulations: Potential Therapeutic Implications. Adv. Ther. 2021, 38, 5046–5064. [Google Scholar] [CrossRef]
- Rho, N.K.; Han, K.H.; Kim, H.S. An Update on the Cosmetic Use of Botulinum Toxin: The Pattern of Practice among Korean Dermatologists. Toxins 2022, 14, 329. [Google Scholar] [CrossRef] [PubMed]
- Ho, W.W.S.; Chan, L.; Corduff, N.; Lau, W.T.; Martin, M.U.; Tay, C.M.; Wang, S.; Wu, R. Addressing the Real-World Challenges of Immunoresistance to Botulinum Neurotoxin A in Aesthetic Practice: Insights and Recommendations from a Panel Discussion in Hong Kong. Toxins 2023, 15, 456. [Google Scholar] [CrossRef]
- Wanitphakdeedecha, R.; Ungaksornpairote, C.; Kaewkes, A.; Sathaworawong, A.; Vanadurongwan, B.; Lektrakul, N. A pilot study comparing the efficacy of two formulations of botulinum toxin type A for muscular calves contouring. J. Cosmet. Dermatol. 2018, 17, 984–990. [Google Scholar] [CrossRef] [PubMed]
- Dressler, D.; Bigalke, H. Botulinum toxin antibody type A titres after cessation of botulinum toxin therapy. Mov. Disord. 2002, 17, 170–173. [Google Scholar] [CrossRef] [PubMed]
- Matzinger, P. Tolerance, danger, and the extended family. Annu. Rev. Immunol. 1994, 12, 991–1045. [Google Scholar] [CrossRef] [PubMed]
- Matzinger, P. The danger model: A renewed sense of self. Science 2002, 296, 301–305. [Google Scholar] [CrossRef]
- Medzhitov, R.; Janeway, C., Jr. Innate immune recognition: Mechanisms and pathways. Immunol. Rev. 2000, 173, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Oshima, M.; Deitiker, P.R.; Jankovic, J.; Duane, D.D.; Aoki, K.R.; Atassi, M.Z. Human T-cell responses to botulinum neurotoxin. Responses in vitro of lymphocytes from patients with cervical dystonia and/or other movement disorders treated with BoNT/A or BoNT/B. J. Neuroimmunol. 2011, 240–241, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Oshima, M.; Deitiker, P.R.; Jankovic, J.; Duane, D.D.; Aoki, K.R.; Atassi, M.Z. Human T-cell responses to botulinum neurotoxin: Proliferative responses in vitro of lymphocytes from botulinum neurotoxin A-treated movement disorder patients. J. Neuroimmunol. 2011, 237, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.A.; Rusnak, J.M. Botulinum neurotoxin vaccines: Past, present, and future. Crit. Rev. Immunol. 2007, 27, 303–318. [Google Scholar] [CrossRef] [PubMed]
- Sundeen, G.; Barbieri, J.T. Vaccines against Botulism. Toxins 2017, 9, 268. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Kim, J.H.; Lee, K.J.; Choi, M.M.; Kim, Y.H.; Rhie, G.E.; Yoo, C.K.; Cha, K.; Shin, N.R. Botulinum neurotoxin type A induces TLR2-mediated inflammatory responses in macrophages. PLoS ONE 2015, 10, e0120840. [Google Scholar] [CrossRef]
- Takumi, K.; Kawata, T. Chemical composition of the cell walls of Clostridium botulinum type, A. Jpn. J. Microbiol. 1970, 14, 57–63. [Google Scholar] [CrossRef]
- Takeuchi, O.; Hoshino, K.; Kawai, T.; Sanjo, H.; Takada, H.; Ogawa, T.; Takeda, K.; Akira, S. Differential roles of TLR2 and TLR4 in recognition of gram-negative and gram-positive bacterial cell wall components. Immunity 1999, 11, 443–451. [Google Scholar] [CrossRef]
- Akira, S. Toll-like receptors: Lessons from knockout mice. Biochem. Soc. Trans. 2000, 28, 551–556. [Google Scholar] [CrossRef]
- Mahmut, N.; Inoue, K.; Fujinaga, Y.; Hughes, L.; Arimitsu, H.; Sakaguchi, Y.; Ohtsuka, A.; Murakami, T.; Yokota, K.; Oguma, K. Characterisation of monoclonal antibodies against haemagglutinin associated with Clostridium botulinum type C neurotoxin. J. Med. Microbiol. 2002, 51, 286–294. [Google Scholar] [CrossRef][Green Version]
- Lee, J.C.; Yokota, K.; Arimitsu, H.; Hwang, H.J.; Sakaguchi, Y.; Cui, J.; Takeshi, K.; Watanabe, T.; Ohyama, T.; Oguma, K. Production of anti-neurotoxin antibody is enhanced by two subcomponents, HA1 and HA3b, of Clostridium botulinum type B 16S toxin-haemagglutinin. Microbiology 2005, 151 Pt 11, 3739–3747. [Google Scholar] [CrossRef] [PubMed]
- Kukreja, R.; Chang, T.W.; Cai, S.; Lindo, P.; Riding, S.; Zhou, Y.; Ravichandran, E.; Singh, B.R. Immunological characterization of the subunits of type A botulinum neurotoxin and different components of its associated proteins. Toxicon 2009, 53, 616–624. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.K.; Singh, B.R. Immunological properties of Hn-33 purified from type A Clostridium botulinum. J. Nat. Toxins 2000, 9, 357–362. [Google Scholar] [PubMed]
- Bryant, A.M.; Cai, S.; Singh, B.R. Comparative immunochemical characteristics of botulinum neurotoxin type A and its associated proteins. Toxicon 2013, 72, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Sayadmanesh, A.; Ebrahimi, F.; Hajizade, A.; Rostamian, M.; Keshavarz, H. Expression and purification of neurotoxin-associated protein HA-33/A from Clostridium botulinum and evaluation of its antigenicity. Iran. Biomed. J. 2013, 17, 165–170. [Google Scholar] [CrossRef]
- Pulendran, B.; Arunachalam, P.S.; O’Hagan, D.T. Emerging concepts in the science of vaccine adjuvants. Nat. Rev. Drug Discov. 2021, 20, 454–475. [Google Scholar] [CrossRef]
- Google Dictionary English. Available online: https://languages.oup.com/google-dictionary-en/ (accessed on 2 November 2023).
- Wikipedia English. Available online: https://en.wikipedia.org/wiki/Excipient (accessed on 6 December 2023).
- Schellekens, H. Factors influencing the immunogenicity of therapeutic proteins. Nephrol. Dial. Transplant. 2005, 20 (Suppl. S6), vi3–vi9. [Google Scholar] [CrossRef]
- Finn, T.E.; Nunez, A.C.; Sunde, M.; Easterbrook-Smith, S.B. Serum albumin prevents protein aggregation and amyloid formation and retains chaperone-like activity in the presence of physiological ligands. J. Biol. Chem. 2012, 287, 21530–21540. [Google Scholar] [CrossRef]
- Martinez Pomier, K.; Ahmed, R.; Melacini, G. Interactions of intrinsically disordered proteins with the unconventional chaperone human serum albumin: From mechanisms of amyloid inhibition to therapeutic opportunities. Biophys. Chem. 2022, 282, 106743. [Google Scholar] [CrossRef]
- Dressler, D.; Pan, L.; Su, J.; Teng, F.; Jin, L. Lantox-The Chinese Botulinum Toxin Drug-Complete English Bibliography and Comprehensive Formalised Literature Review. Toxins 2021, 13, 370. [Google Scholar] [CrossRef]
- Schellekens, H.; Jiskoot, W. Erythropoietin-Associated PRCA: Still an Unsolved Mystery. J. Immunotoxicol. 2006, 3, 123–130. [Google Scholar] [CrossRef]
- Casadevall, N. Pure red cell aplasia and anti-erythropoietin antibodies in patients treated with epoetin. Nephrol. Dial. Transplant. 2003, 18 (Suppl. S8), viii37–viii41. [Google Scholar] [CrossRef] [PubMed]
- Boven, K.; Knight, J.; Bader, F.; Rossert, J.; Eckardt, K.U.; Casadevall, N. Epoetin-associated pure red cell aplasia in patients with chronic kidney disease: Solving the mystery. Nephrol. Dial. Transplant. 2005, 20 (Suppl. S3), iii33–iii40, Erratum in Nephrol. Dial. Transplant. 2006, 21, 2678. [Google Scholar] [CrossRef][Green Version]
- Macdougall, I.C.; Casadevall, N.; Locatelli, F.; Combe, C.; London, G.M.; Di Paolo, S.; Kribben, A.; Fliser, D.; Messner, H.; McNeil, J.; et al. Incidence of erythropoietin antibody-mediated pure red cell aplasia: The Prospective Immunogenicity Surveillance Registry (PRIMS). Nephrol. Dial. Transplant. 2015, 30, 451–460. [Google Scholar] [CrossRef]
- Vincent, J.L.; Wilkes, M.M.; Navickis, R.J. Safety of human albumin—Serious adverse events reported worldwide in 1998–2000. Br. J. Anaesth. 2003, 91, 625–630. [Google Scholar] [CrossRef] [PubMed]
- Sattler, S.; Gollomp, S.; Curry, A. A Narrative Literature Review of the Established Safety of Human Serum Albumin Use as a Stabilizer in Aesthetic Botulinum Toxin Formulations Compared to Alternatives. Toxins 2023, 15, 619. [Google Scholar] [CrossRef]
- Chuang, V.T.; Otagiri, M. Recombinant human serum albumin. Drugs Today 2007, 43, 547–561. [Google Scholar] [CrossRef]
- Farrugia, A. The Evolution of the Safety of Plasma Products from Pathogen Transmission—A Continuing Narrative. Pathogens 2023, 12, 318. [Google Scholar] [CrossRef]
- Karimi, M.; Bahrami, S.; Ravari, S.B.; Zangabad, P.S.; Mirshekari, H.; Bozorgomid, M.; Shahreza, S.; Sori, M.; Hamblin, M.R. Albumin nanostructures as advanced drug delivery systems. Expert Opin. Drug Deliv. 2016, 13, 1609–1623. [Google Scholar] [CrossRef]
- Paul, M.; Itoo, A.M.; Ghosh, B.; Biswas, S. Current trends in the use of human serum albumin for drug delivery in cancer. Expert Opin. Drug Deliv. 2022, 19, 1449–1470. [Google Scholar] [CrossRef]
- Tumber, P.S.; Louis, I. Botulinum toxin type a therapy and human serum albumin. Anesthesiology 2006, 104, 104–1108; discussion 1108–1109. [Google Scholar] [CrossRef]
- Ellmerer, M.; Schaupp, L.; Brunner, G.A.; Sendlhofer, G.; Wutte, A.; Wach, P.; Pieber, T.R. Measurement of interstitial albumin in human skeletal muscle and adipose tissue by open-flow microperfusion. Am. J. Physiol. Endocrinol. Metab. 2000, 278, E352–E356. [Google Scholar] [CrossRef]
- Wang, W.; Singh, S.K.; Li, N.; Toler, M.R.; King, K.R.; Nema, S. Immunogenicity of protein aggregates—Concerns and realities. Int. J. Pharm. 2012, 431, 1–11. [Google Scholar] [CrossRef]
- Moreno Lozano, L.; Galindo Bonilla, P.; Borja Segade, J.; Extremera Ortega, A.; Gómez Torrijos, E.; García Rodríguez, R. Human Serum Albumin Induced Anaphylaxis in a Patient with Good Tolerance to Human Plasma. J Investig Allergol Clin Immunol. 2019, 29, 51–53. [Google Scholar] [CrossRef]
- Stafford, C.T.; Lobel, S.A.; Fruge, B.C.; Moffitt, J.E.; Hoff, R.G.; Fadel, H.E. Anaphylaxis to human serum albumin. Ann. Allergy 1988, 61, 85–88. [Google Scholar]
- Grammer, L.C. Hypersensitivity. Nephrol. Dial. Transplant. 1994, 9 (Suppl. S2), 29–35. [Google Scholar] [PubMed]
- Kutschenko, A.; Bigalke, H.; Wegner, F.; Wohlfarth, K. The role of human serum albumin and neurotoxin associated proteins in the formulation of BoNT/A products. Toxicon 2019, 168, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Federal Drug Administration. Search Term “Sucrose”. Available online: https://www.accessdata.fda.gov/scripts/cder/iig/index.cfm (accessed on 4 December 2023).
- Pharma Excipients. Available online: https://www.pharmaexcipients.com/stabilizer/sucrose/ (accessed on 4 December 2023).
- Federal Drug Administration. Search Term “Histidine”. Available online: https://www.accessdata.fda.gov/scripts/cder/iig/index.cfm (accessed on 4 December 2023).
- Biospectra. Available online: https://www.biospectra.us/images/TechSheets/22/L-Histidine-Monohydrochloride-Monohydrate-Bio-Excipient-LHMM-3250-V7-9-20-22.pdf (accessed on 6 December 2023).
- Saurabh, S.; Kalonia, C.; Li, Z.; Hollowell, P.; Waigh, T.; Li, P.; Webster, J.; Seddon, J.M.; Lu, J.R.; Bresme, F. Understanding the Stabilizing Effect of Histidine on mAb Aggregation: A Molecular Dynamics Study. Mol. Pharm. 2022, 19, 3288–3303. [Google Scholar] [CrossRef] [PubMed]
- Gitter, J.H.; Geidobler, R.; Presser, I.; Winter, G. A Comparison of Controlled Ice Nucleation Techniques for Freeze-Drying of a Therapeutic Antibody. J. Pharm. Sci. 2018, 107, 2748–2754. [Google Scholar] [CrossRef] [PubMed]
- Massant, J.; Fleurime, S.; Batens, M.; Vanhaerents, H.; Van den Mooter, G. Formulating monoclonal antibodies as powders for reconstitution at high concentration using spray-drying: Trehalose/amino acid combinations as reconstitution time reducing and stability improving formulations. Eur. J. Pharm. Biopharm. 2020, 156, 131–142. [Google Scholar] [CrossRef]
- Tundup, S.; Srivastava, L.; Harn, D.A., Jr. Polarization of host immune responses by helminth-expressed glycans. Ann. N. Y Acad. Sci. 2012, 1253, E1–E13. [Google Scholar] [CrossRef]
- Lynch, A.T.; Motozono, C.; Foster, A.J.; Kodar, K.; Dangerfield, E.M.; Yamasaki, S.; Wedlock, D.N.; Timmer, M.S.M.; Stocker, B.L. Trehalose diamide glycolipids augment antigen-specific antibody responses in a Mincle-dependent manner. Bioorg. Chem. 2021, 110, 104747. [Google Scholar] [CrossRef]
- Kamali Jamil, R.; Shayestehour, M.; Sadigh, Z.A.; Taqavian, M.; Shahkarami, M.K.; Esna-Ashari, F.; Shahbazi, R.; Mohammadi, A.; Foroughi, A.; Romani, B. The Effect of Various Stabilizers on Preserving Immunogenicity of Lyophilized Mumps Vaccines. J. Res. Health Sci. 2017, 17, e00393. [Google Scholar]
- Jeong, S.J.; Stitham, J.; Evans, T.D.; Zhang, X.; Rodriguez-Velez, A.; Yeh, Y.S.; Tao, J.; Takabatake, K.; Epelman, S.; Lodhi, I.J.; et al. Trehalose causes low-grade lysosomal stress to activate TFEB and the autophagy-lysosome biogenesis response. Autophagy 2021, 17, 3740–3752. [Google Scholar] [CrossRef]
- Wikipedia. Available online: https://en.wikipedia.org/wiki/Polysorbate_20 (accessed on 6 December 2023).
- Kerwin, B.A. Polysorbates 20 and 80 used in the formulation of protein biotherapeutics: Structure and degradation pathways. J. Pharm. Sci. 2008, 97, 2924–2935. [Google Scholar] [CrossRef]
- Yi, Y.; Jin, Y.; Menon, R.; Yeung, B. Polysorbate, the Good, the Bad and the Ugly. Am. Pharm. Rev. 2020. Available online: https://www.americanpharmaceuticalreview.com/Featured-Articles/569560-Polysorbate-the-Good-the-Bad-and-the-Ugly/ (accessed on 6 December 2023).
- Jones, M.T.; Mahler, H.C.; Yadav, S.; Bindra, D.; Corvari, V.; Fesinmeyer, R.M.; Gupta, K.; Harmon, A.M.; Hinds, K.D.; Koulov, A.; et al. Considerations for the Use of Polysorbates in Biopharmaceuticals. Pharm. Res. 2018, 35, 148. [Google Scholar] [CrossRef] [PubMed]
- Ko, E.J.; Kang, S.M. Immunology and efficacy of MF59-adjuvanted vaccines. Hum. Vaccin. Immunother. 2018, 14, 3041–3045. [Google Scholar] [CrossRef] [PubMed]
- Brunner, R.; Jensen-Jarolim, E.; Pali-Schöll, I. The ABC of clinical and experimental adjuvants—A brief overview. Immunol. Lett. 2010, 128, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Del Giudice, G.; Rappuoli, R.; Didierlaurent, A.M. Correlates of adjuvanticity: A review on adjuvants in licensed vaccines. Semin. Immunol. 2018, 39, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Stone, C.A., Jr.; Liu, Y.; Relling, M.V.; Krantz, M.S.; Pratt, A.L.; Abreo, A.; Hemler, J.A.; Phillips, E.J. Immediate Hypersensitivity to Polyethylene Glycols and Polysorbates: More Common than We Have Recognized. J. Allergy Clin. Immunol. Pract. 2019, 7, 1533–1540.e8. [Google Scholar] [CrossRef]
- Porter, N.A.; Caldwell, S.E.; Mills, K.A. Mechanisms of free radical oxidation of unsaturated lipids. Lipids 1995, 30, 277–290. [Google Scholar] [CrossRef]
- Yin, H.; Porter, N.A. New insights regarding the autoxidation of polyunsaturated fatty acids. Antioxid. Redox Signal. 2005, 7, 170–184. [Google Scholar] [CrossRef]
- Mittag, J.J.; Trutschel, M.L.; Kruschwitz, H.; Mäder, K.; Buske, J.; Garidel, P. Characterization of radicals in polysorbate 80 using electron paramagnetic resonance (EPR) spectroscopy and spin trapping. Int. J. Pharm. X 2022, 4, 100123. [Google Scholar] [CrossRef]
- Liu, H.; Jin, Y.; Menon, R.; Laskowich, E.; Bareford, L.; de Vilmorin, P.; Kolwyck, D.; Yeung, B.; Yi, L. Characterization of Polysorbate 80 by Liquid Chromatography-Mass Spectrometry to Understand Its Susceptibility to Degradation and Its Oxidative Degradation Pathway. J. Pharm. Sci. 2022, 111, 323–334. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, A.; Zarraga, I.E.; Demeule, B. Characterization of Polysorbate Ester Fractions and Implications in Protein Drug Product Stability. Mol. Pharm. 2020, 17, 2345–2353. [Google Scholar] [CrossRef]
- Kim, J.; Kwak, S.; Park, M.S.; Rhee, C.H.; Yang, G.H.; Lee, J.; Son, W.C.; Kang, W.H. Safety verification for polysorbate 20, pharmaceutical excipient for intramuscular administration, in Sprague-Dawley rats and New Zealand White rabbits. PLoS ONE 2021, 16, e0256869, Erratum in PLoS ONE 2022, 17, e0267238. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Yadav, S.; John Wang, Y.; Mozziconacci, O.; Schöneich, C. Dual Effect of Histidine on Polysorbate 20 Stability: Mechanistic Studies. Pharm. Res. 2018, 35, 33. [Google Scholar] [CrossRef]
- Brovč, E.V.; Mravljak, J.; Šink, R.; Pajk, S. Degradation of polysorbates 20 and 80 catalysed by histidine chloride buffer. Eur. J. Pharm. Biopharm. 2020, 154, 236–245. [Google Scholar] [CrossRef]
- AAT Bioquest Peptide and Protein Molecular Weight Calculator. Entry: RKKRRQRRRGKKKKKKKKKKKKKKKKGRKKRRQRRR. Available online: https://www.aatbio.com/tools/calculate-peptide-and-protein-molecular-weight-mw (accessed on 1 December 2023).
- Vivès, E.; Brodin, P.; Lebleu, B. A truncated HIV-1 Tat protein basic domain rapidly translocates through the plasma membrane and accumulates in the cell nucleus. J. Biol. Chem. 1997, 272, 16010–16017. [Google Scholar] [CrossRef] [PubMed]
- Rizzuti, M.; Nizzardo, M.; Zanetta, C.; Ramirez, A.; Corti, S. Therapeutic applications of the cell-penetrating HIV-1 Tat peptide. Drug Discov. Today 2015, 20, 76–85. [Google Scholar] [CrossRef]
- PCT Patent Application. Available online: https://patentimages.storage.googleapis.com/3c/34/b1/b0c64ae4b87ce0/WO2008082885A2.pdf (accessed on 1 December 2023).
- Howl, J.; Jones, S. Transport molecules using reverse sequence HIV-Tat polypeptides: Not just any old Tat? (WO200808225). Expert Opin. Ther. Pat. 2009, 19, 1329–1333. [Google Scholar] [CrossRef]
- Gallagher, C.J.; Bowsher, R.R.; Clancy, A.; Dover, J.S.; Humphrey, S.; Liu, Y.; Prawdzik, G. Clinical Immunogenicity of DaxibotulinumtoxinA for Injection in Glabellar Lines: Pooled Data from the SAKURA Phase 3 Trials. Toxins 2023, 15, 60. [Google Scholar] [CrossRef]
- Glogau, R.G.; Waugh, J.M. Preclinical Transcutaneous Flux Experiments using a Macromolecular Transport System (MTS) Peptide for Delivery of Botulinum Toxin Type A. In Proceedings of the Annual Meeting of the American Academy of Dermatology, San Antonio, TX, USA, 1–5 February 2008. [Google Scholar]
- Solish, N.; Carruthers, J.; Kaufman, J.; Rubio, R.G.; Gross, T.M.; Gallagher, C.J. Overview of DaxibotulinumtoxinA for Injection: A Novel Formulation of Botulinum Toxin Type A. Drugs 2021, 81, 2091–2101. [Google Scholar] [CrossRef]
- Ghosh, S. Sialic acid and biology of life: An introduction. In Sialic Acids and Sialoglycoconjugates in the Biology of Life, Health and Disease; Academic Press: Cambridge, MA, USA, 2020; pp. 1–61. [Google Scholar] [CrossRef]
- Humphrey, S.; Dover, J.S.; Bowsher, R.R.; Clancy, A.; Liu, Y.; Prawdzik, G.; Gallagher, C.J. Immunogenicity of DaxibotulinumtoxinA for Injection in Glabellar Lines. Aesthet Surg J. 2023, 43, 1189–1193. [Google Scholar] [CrossRef]
- Lam, X.M.; Yang, J.Y.; Cleland, J.L. Antioxidants for prevention of methionine oxidation in recombinant monoclonal antibody HER2. J. Pharm. Sci. 1997, 86, 1250–1255. [Google Scholar] [CrossRef]
- Dion, M.Z.; Leiske, D.; Sharma, V.K.; Zuch de Zafra, C.L.; Salisbury, C.M. Mitigation of Oxidation in Therapeutic Antibody Formulations: A Biochemical Efficacy and Safety Evaluation of N-Acetyl-Tryptophan and L-Methionine. Pharm. Res. 2018, 35, 222. [Google Scholar] [CrossRef]
- Hermeling, S.; Crommelin, D.J.; Schellekens, H.; Jiskoot, W. Structure-immunogenicity relationships of therapeutic proteins. Pharm. Res. 2004, 21, 897–903. [Google Scholar] [CrossRef] [PubMed]
- Lindman, S.; Xue, W.F.; Szczepankiewicz, O.; Bauer, M.C.; Nilsson, H.; Linse, S. Salting the charged surface: pH and salt dependence of protein G B1 stability. Biophys. J. 2006, 90, 2911–2921. [Google Scholar] [CrossRef] [PubMed]
- Makhatadze, G.I.; Loladze, V.V.; Ermolenko, D.N.; Chen, X.; Thomas, S.T. Contribution of surface salt bridges to protein stability: Guidelines for protein engineering. J. Mol. Biol. 2003, 327, 1135–1148. [Google Scholar] [CrossRef] [PubMed]
- Akke, M.; Forsén, S. Protein stability and electrostatic interactions between solvent exposed charged side chains. Proteins 1990, 8, 23–29. [Google Scholar] [CrossRef]
- Nail, S.L.; Jiang, S.; Chongprasert, S.; Knopp, S.A. Fundamentals of freeze-drying. Pharm. Biotechnol. 2002, 14, 281–360. [Google Scholar] [CrossRef]
- Franks, F.; Auffret, T. Freeze-Drying of Pharmaceuticals and Biopharmaceuticals Principles and Practice; Royal Society of Chemistry: London, UK, 2007. [Google Scholar]
- Matejtschuk, P.; Bird, C.; Ezeajughi, E.; MacLellan-Gibson, K.; Wadhwa, M. Impact of Formulation Choices on the Freeze-Drying of an Interleukin-6 Reference Material. Front. Mol. Biosci. 2022, 9, 868460, Erratum in Front. Mol. Biosci. 2022, 9, 1062810. [Google Scholar] [CrossRef]
- Goodnough, M.C.; Johnson, E.A. Stabilization of botulinum toxin type A during lyophilization. Appl. Environ. Microbiol. 1992, 58, 3426–3428. [Google Scholar] [CrossRef]
- Rossetto, O.; Pirazzini, M.; Montecucco, C. Botulinum neurotoxins: Genetic, structural and mechanistic insights. Nat. Rev. Microbiol. 2014, 12, 535–549. [Google Scholar] [CrossRef]
- Mire-Sluis, A.R.; Das, R.G.; Padilla, A. WHO cytokine standardization: Facilitating the development of cytokines in research, diagnosis and as therapeutic agents. J. Immunol. Methods 1998, 216, 103–116. [Google Scholar] [CrossRef]
- Frevert, J. Content of botulinum neurotoxin in Botox®/Vistabel®, Dysport®/Azzalure®, and Xeomin®/Bocouture®. Drugs R D 2010, 10, 67–73. [Google Scholar] [CrossRef]
- Patten, P.A.; Schellekens, H. The immunogenicity of biopharmaceuticals. Lessons learned and consequences for protein drug development. Dev. Biol. 2003, 112, 81–97. [Google Scholar]
- Rosenberg, A.S. Effects of protein aggregates: An immunologic perspective. AAPS J. 2006, 8, E501–E507. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.Y.; Friedman, D.F.; DaVeiga, S.P. Immediate hypersensitivity reaction to human serum albumin in a child undergoing plasmapheresis. Transfusion 2019, 59, 1921–1923. [Google Scholar] [CrossRef] [PubMed]
- Pham, N.B.; Meng, W.S. Protein aggregation and immunogenicity of biotherapeutics. Int. J. Pharm. 2020, 585, 119523. [Google Scholar] [CrossRef] [PubMed]
- Lundahl, M.L.E.; Fogli, S.; Colavita, P.E.; Scanlan, E.M. Aggregation of protein therapeutics enhances their immunogenicity: Causes and mitigation strategies. RSC Chem. Biol. 2021, 2, 1004–1020. [Google Scholar] [CrossRef] [PubMed]
- Anders, H.J.; Schlondorff, D.O. Innate immune receptors and autophagy: Implications for autoimmune kidney injury. Kidney Int. 2010, 78, 29–37. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nace, G.; Evankovich, J.; Eid, R.; Tsung, A. Dendritic cells and damage-associated molecular patterns: Endogenous danger signals linking innate and adaptive immunity. J. Innate Immun. 2012, 4, 6–15. [Google Scholar] [CrossRef]
- Rombach-Riegraf, V.; Karle, A.C.; Wolf, B.; Sordé, L.; Koepke, S.; Gottlieb, S.; Krieg, J.; Djidja, M.C.; Baban, A.; Spindeldreher, S.; et al. Aggregation of human recombinant monoclonal antibodies influences the capacity of dendritic cells to stimulate adaptive T-cell responses in vitro. PLoS ONE 2014, 9, e86322, Erratum in PLoS ONE 2014, 9, e93339. [Google Scholar] [CrossRef]
| Product Name | IncobotulinumtoxinA | MT-10107 | DaxibotulinumtoxinA-Lanm |
|---|---|---|---|
| Trade name | Xeomin® | Coretox® | Daxxify® |
| Manufacturer | Merz, Frankfurt, Germany | Medytox, Seoul, Republic of Korea | Revance, Nashville, USA |
| Dosage | 50 U, 100 U | 100 U | 50 U, 100 U |
| Toxin type | C.bot. type A (Hall) | C.bot. type A (Hall) | C.bot. type A (Hall) |
| Active ingredient (s) | Core 150 kDa toxin | Core 150 kDa toxin | Core 150 kDa toxin RTP004 peptide (11.7 µg) |
| Appearance | Lyophilizate | Lyophilizate | Lyophilizate |
| Storage | Room temperature | 2 °C to 8 °C, refrigerate | Room temperature |
| Formulation (excipients) | Human serum albumin (1 mg) Sucrose (4.7 mg) | L-Methionine (?) Polysorbate 20 (?) Sucrose (3 mg) NaCl (0.9 mg) | L-Histidine (0.14 mg) L-Histidine-HCl monohydrate (0.65 mg) Polysorbate 20 (0.1 mg) Trehalosedihydrate (36 mg) |
| “Stabilizer” | Human serum albumin | Polysorbate 20 | RTP004 peptide Polysorbate 20 |
| References | [8,9] | [10] | [11,12] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martin, M.U.; Frevert, J.; Tay, C.M. Complexing Protein-Free Botulinum Neurotoxin A Formulations: Implications of Excipients for Immunogenicity. Toxins 2024, 16, 101. https://doi.org/10.3390/toxins16020101
Martin MU, Frevert J, Tay CM. Complexing Protein-Free Botulinum Neurotoxin A Formulations: Implications of Excipients for Immunogenicity. Toxins. 2024; 16(2):101. https://doi.org/10.3390/toxins16020101
Chicago/Turabian StyleMartin, Michael Uwe, Juergen Frevert, and Clifton Ming Tay. 2024. "Complexing Protein-Free Botulinum Neurotoxin A Formulations: Implications of Excipients for Immunogenicity" Toxins 16, no. 2: 101. https://doi.org/10.3390/toxins16020101
APA StyleMartin, M. U., Frevert, J., & Tay, C. M. (2024). Complexing Protein-Free Botulinum Neurotoxin A Formulations: Implications of Excipients for Immunogenicity. Toxins, 16(2), 101. https://doi.org/10.3390/toxins16020101





