2. Introduction
Spasticity is a complex neurological condition that arises from an upper motor neuron lesion, which causes a disordered sensory-motor control leading to intermittent or sustained involuntary muscle activation [
1]. It is prevalent in many neurological disorders, including stroke, multiple sclerosis, hypoxic brain damage, traumatic brain injury, tumors, and heredodegenerative diseases [
2]. The condition often leads to muscle contracture and deformity, potentially reducing function and movement, which may cause disability. Moreover, it has the capacity to affect both pediatric and adult populations. It is frequently categorized according to the distribution of the affected body regions. This classification comprises three main types: focal, regional, and generalized. Focal spasticity pertains to the involvement of a particular body part; regional spasticity refers to the impact on an entire limb, while generalized spasticity denotes the effect on multiple body areas [
3].
Spasticity can result in diverse abnormal postures in both the upper and lower limbs, including abnormal arm posture, equinovarus, knee flexion or hyperextension, spastic drop foot with hyper plantar flexion, toe flexion, contracture, pressure ulcers, and subsequent deformities [
4,
5]. These complications can have a significant impact on the mobility and quality of life of those affected. As a result, spasticity is linked to reduced physical function and diminished ability to carry out daily activities, increased pain, reduced overall health status, and ultimately, a negative effect on the quality of life [
6,
7]. Additionally, the condition negatively impacts the professional life of patients [
8]. Additionally, limb spasticity has a detrimental impact not only on patients but also on their caregivers. Fulfilling caregiving responsibilities often necessitates reduced work hours or even resignation from employment, resulting in financial difficulties [
9]. Caregivers frequently experience absenteeism and presenteeism, contributing to the overall caregiving load [
10]. This burden encompasses emotional and physical strain faced by caregivers, along with the expenses linked to medical interventions, assistive devices, and home modifications. The associated time and productivity loss related to tending to patients with spasticity can also be substantial [
11]. Both patients and their caregivers might encounter out-of-pocket costs, especially for transportation and medical treatments, which further contribute to the economic burden.
The management of the condition involves physical therapy, such as muscle stretching or range of motion exercises, and pharmacotherapy. While several anti-spasticity treatments are available, their lack of specificity and their adverse events limit their usefulness. In this context, local intramuscular injection of botulinum toxin type A (BoNT-A) has emerged as a well-tolerated, first-line treatment option for both upper and lower limb spasticity. BoNT-A injection is supported by a robust body of evidence, and guidelines recommend it as standard clinical practice [
5].
AbobotulinumtoxinA (aboBoNT-A) is a type of BoNT-A that is administered through injection. BoNT-A is produced by culturing Clostridium botulinum type A. After several isolation and purification steps, this toxin can be used as medicine and administered to patients through injection. Unlike systemic oral treatments, direct intramuscular administration of BoNT-A through injections reduces the risk of adverse effects caused by organ irritation or absorption and excretion. BoNT-A injections have been found to be effective in enhancing patient mobility and decreasing the likelihood of complications such as joint deformity, tendon shortening, deep vein thrombosis, and pressure ulcers. The evidence shows that aboBoNT-A may produce a more robust response in pediatric patients with upper limb spasticity [
12], as well as in adult patients with spasticity in their upper [
13] or lower limbs [
4], resulting in statistically significant reductions in muscle tone and overall improvement in patient function. BoNT-A offers a sustained alleviation of symptoms, resulting in extended intervals of enhanced mobility, reduced symptom-related anxieties, and heightened self-assurance for patients [
11,
14,
15].
Thus, aboBoNT-A has emerged as an established first-line therapy for upper and lower limb spasticity, providing a safe and effective treatment option for patients. However, in healthcare, it is important to consider not only the clinical effectiveness of an intervention but also its economic impact. Clinical effectiveness refers to the ability of an intervention to achieve its intended health outcomes, while economic impact refers to the costs and benefits of an intervention in relation to its clinical effectiveness.
The economic evidence of an intervention is important because healthcare resources are finite, and decisions need to be made on how to allocate them efficiently. Economic evaluation can help to identify the most cost-effective interventions, which provide the best value for money and can maximize the health benefits for patients. Additionally, it can inform decisions about resource allocation and funding, help to prioritize health interventions and support negotiations with payers and policymakers.
Therefore, it is important to consider both the clinical and economic evidence of an intervention when making decisions about its adoption and implementation. Without economic evidence, it can be difficult to make informed decisions about the use of healthcare resources and ensure that interventions are cost-effective and sustainable in the long run.
Based on the above, the study aimed to assess the cost-effectiveness and budget impact of aboBoNT-A plus BSC compared with placebo plus BSC alone for managing limb spasticity in adult patients in Greece, as well as to conduct a budget impact analysis of the introduction of aboBoNT-A in the Greek healthcare system compared to onabotulnumtoxinA (onaBoNT-A). The objectives of this study include evaluating the economic differences between aboBoNT-A and onaBoNT-A in terms of their impact on pharmaceutical costs, as both regimens can be used for these indications. We use the Greek healthcare system as a field of application of our analysis and take a third-party payer perspective to evaluate aboBoNT-A as an addition to the current treatment of upper and lower limb spasticity in adult patients. Our analysis includes cost-effectiveness and a budget impact approach in both populations.
3. Results
The cost-effectiveness analysis for the upper limb spasticity indication found that the mean total treatment cost per patient with aboBoNT-A was €34,020, while supportive therapy alone cost €28,698. The use of aboBoNT-A resulted in an increase in quality-adjusted survival per patient by 0.516 QALYs, with a cost-effectiveness ratio (ICER) of €10,313/QALY gained compared to supportive care (as shown in
Table 1).
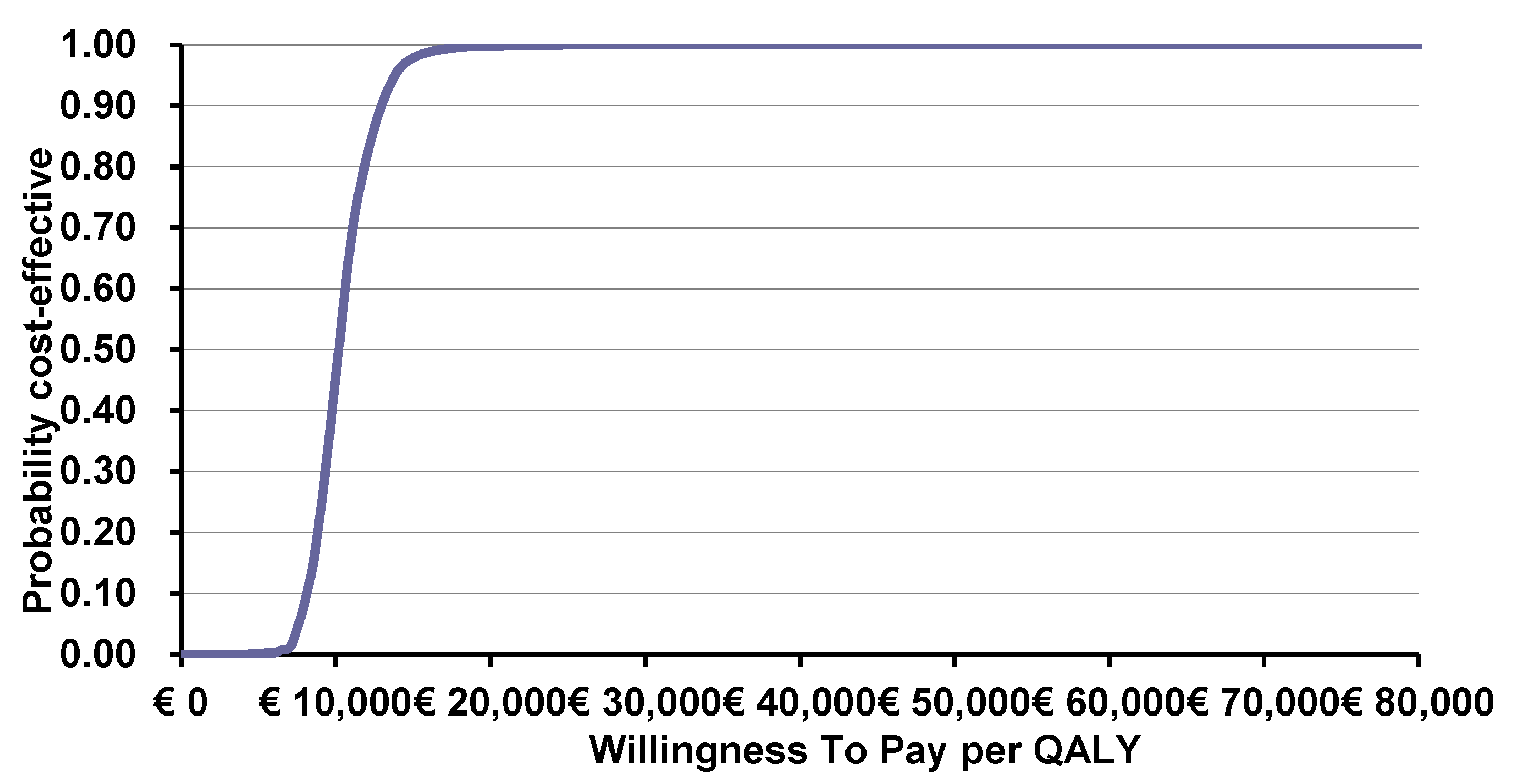
The probabilistic sensitivity analysis demonstrated that the intervention was cost-effective in all simulations, with a mean ICER of €10,132/QALY gained (as presented in
Figure 1). As demonstrated in
Figure 2, the intervention is considered 100% cost-effective for a threshold of nearly €20,000 and above.
With regards to adult lower limb spasticity, the analysis demonstrated that the mean total treatment cost per patient with aboBoNT-A was €38,853 versus €29,088 of the supportive therapy, while the QALYs gained from the intervention were 9.66 versus 9.31 of the supportive therapy, resulting in an ICER of €39,465/QALY gained (
Table 2).
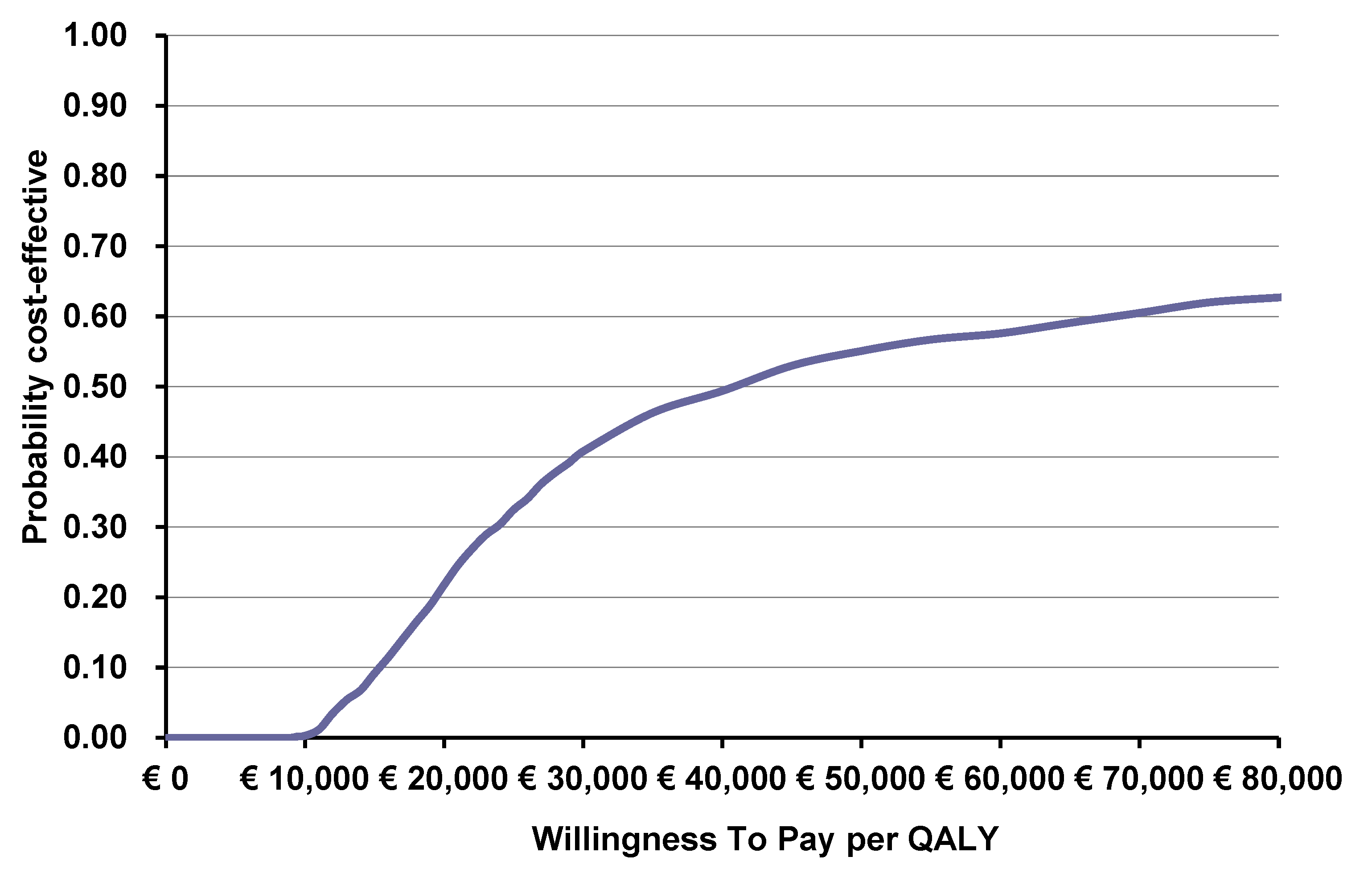
The probabilistic sensitivity analysis showed that the intervention remained cost-effective in the majority of the simulations, with a mean ICER of €39,442/QALY gained (
Figure 3). As shown in
Figure 4, the intervention has a 50% chance of being cost-effective for a threshold of €40,000, with the probability of being cost-effective increasing for higher thresholds.
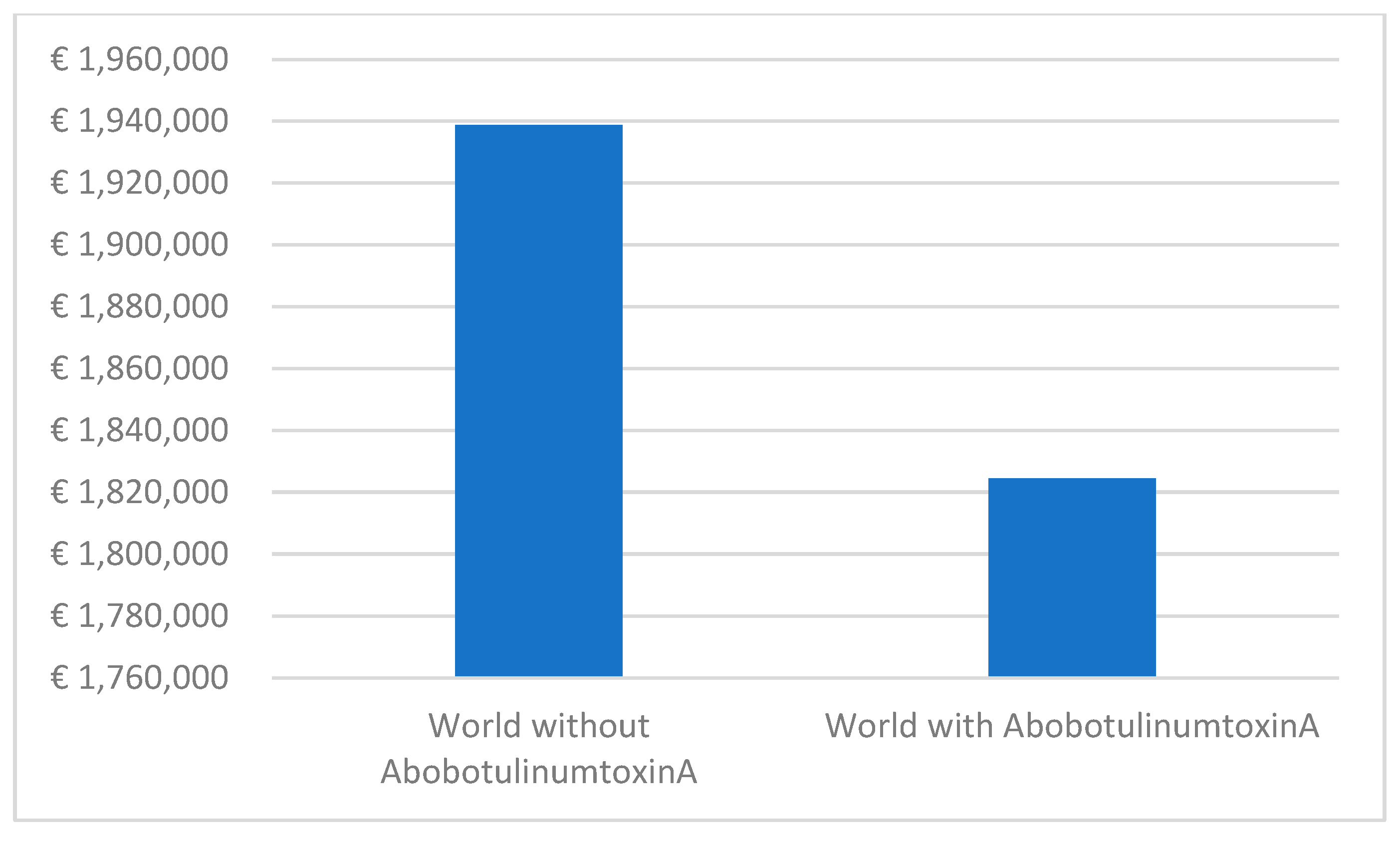
The budget impact analysis for upper limb spasticity reveals significant cost savings over a 5-year period. Comparing the two scenarios, the ‘world with aboBoNT-A’ demonstrates an estimated pharmaceutical cost of €1,824,514, while the ‘world without’ presents a higher cost of €1,938,831 (
Figure 5). This difference amounts to a total savings of 5.9% in pharmaceutical expenses for upper limb spasticity. Furthermore, the monthly cost per patient experiences a downward trend, decreasing from €122.4 in the initial year to €108.0 in the fifth year.
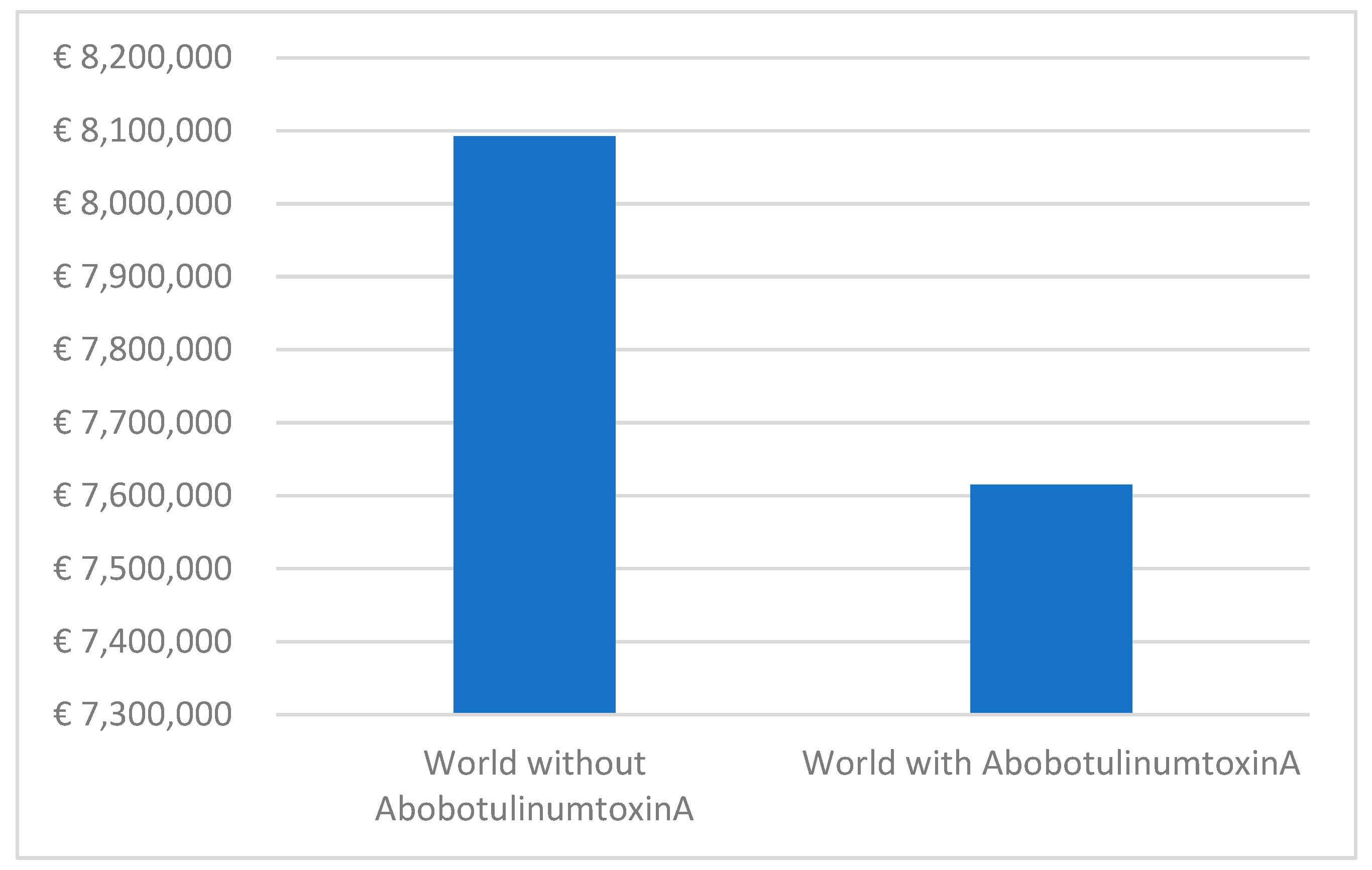
In the context of lower limb spasticity, the scenario ‘world without’ translates to pharmaceutical costs of €8,072,295, whereas the scenario ‘world with’ reflects reduced costs of €7,615,141 (
Figure 6). This demonstrates a tangible reduction in expenses over the 5-year period, with the highest savings realized in the fifth year when the utilization of aboBoNT-A therapy is at its peak for lower limb spasticity. The average monthly cost per patient consistently decreases, highlighting the cumulative financial benefits associated with aboBoNT-A therapy for both upper and lower limb spasticity.
4. Discussion
Based on the results of the CEA for the upper limb spasticity indication, it can be concluded that the use of aboBoNT-A is a cost-effective treatment option compared to supportive care alone. The ICER of €10,313/QALY gained shows that the additional cost of the treatment per QALY gained is reasonable. The probabilistic sensitivity analysis confirms that the intervention is cost-effective in all simulations, with a mean ICER of €10,132/QALY gained. This indicates that the use of aboBoNT-A is a favorable and efficient option for patients with upper limb spasticity. Similarly, the analysis for the lower limb spasticity indication also showed that aboBoNT-A is a cost-effective treatment option compared to best supportive care alone. The ICER of €39,465/QALY gained is higher than that of upper limb spasticity but still falls within the acceptable range. The probabilistic sensitivity analysis also confirmed the cost-effectiveness of the intervention in the majority of simulations, with a mean ICER of €39,442/QALY gained. This suggests that the use of aboBoNT-A is a favorable and efficient option for patients with lower limb spasticity.
The present study found aboBoNT-A to be a cost-effective option for the treatment of lower and upper limb spasticity in adults in Greece. Our study is in line with other studies in different countries, which have also reported that aboBoNT-A is a cost-effective treatment option for the treatment of lower and upper limb spasticity. For example, in Australia, aboBoNT-A was found to be a cost-effective treatment for lower limb spasticity in adults [
16]. Additionally, in the United Kingdom, aboBoNT-A was reported to dominate placebo plus BSC as a treatment option for upper limb spasticity in adults [
17] and was identified as a cost-effective approach for the management of wrist and hand disability resulting from upper-limb post-stroke spasticity in Scotland [
18]. Furthermore, studies conducted in the UK have also found that aboBoNT-A was a cost-effective strategy compared to placebo plus BSC for the treatment of post-stroke spasticity [
19] and was identified as the dominant strategy compared to onaBoNT-A for all indications [
20].
Our study examined the financial impact of aboBoNT-A treatment for upper and lower limb spasticity and found that it resulted in cost savings in pharmaceutical spending over a 5-year period. These findings are consistent with other studies, such as one conducted in the UK where aboBoNT-A was found to be less expensive per patient per year than best supportive care for upper limb spasticity, while onaBoNT-A and incobotulinumtoxinA were more expensive [
21]. However, a study in Germany showed that the use of aboBoNT-A for upper limb spasticity in adults increased costs compared to usual care but was still less expensive than its comparator. Another study in Germany suggested that increasing the use of aboBoNT-A compared to onaBoNT-A and incobotulinumtoxinA for upper limb spasticity could potentially reduce the total cost of treatment [
22].
Thus, using aboBoNT-A could lead to cost savings and potentially increase patient access to treatment while improving healthcare resource efficiency. For example, with a hypothetical annual pharmaceutical budget of €300,000 in Greece, aboBoNT-A could provide treatment for an additional 85 adult patients with upper limb spasticity each year. Similarly, with a hypothetical annual pharmaceutical budget of €1,000,000, the introduction of aboBoNT-A in the Greek market could enable 284 more patients with lower limb spasticity to receive treatment annually.