PLGA Nanoparticle-Based Dissolving Microneedle Vaccine of Clostridium perfringens ε Toxin
Abstract
1. Introduction
2. Results
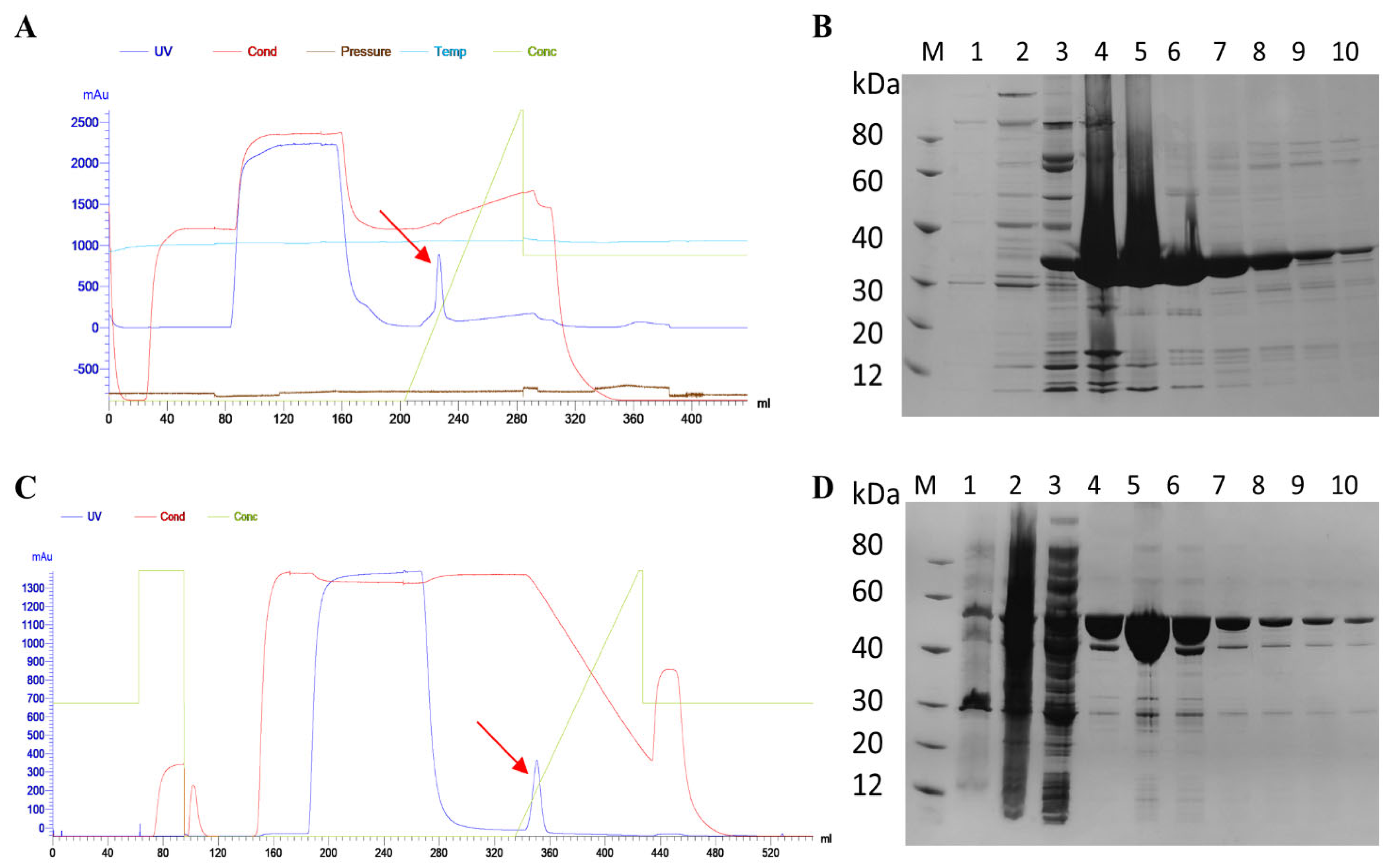
2.1. Preparation of Vaccine Antigens and Toxin Proteins
2.2. Characterization of PLGA-DDAB Nanoparticles
2.3. Analysis of the Performance of PLGA-DDAB dMN
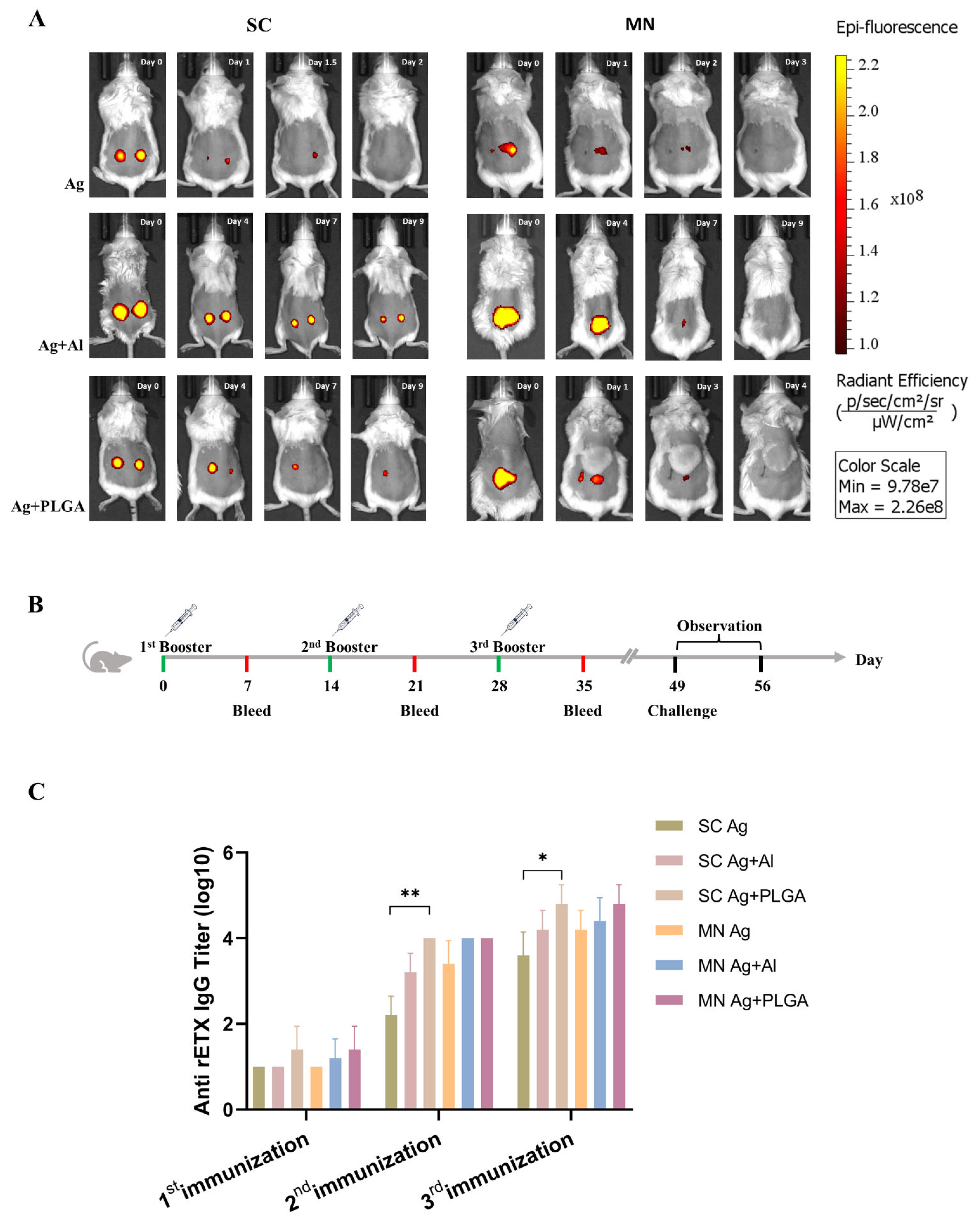
2.4. In Vivo Release Time and Antibody Titer Analysis of MN Vaccines
2.5. Analysis of Immune Response Types
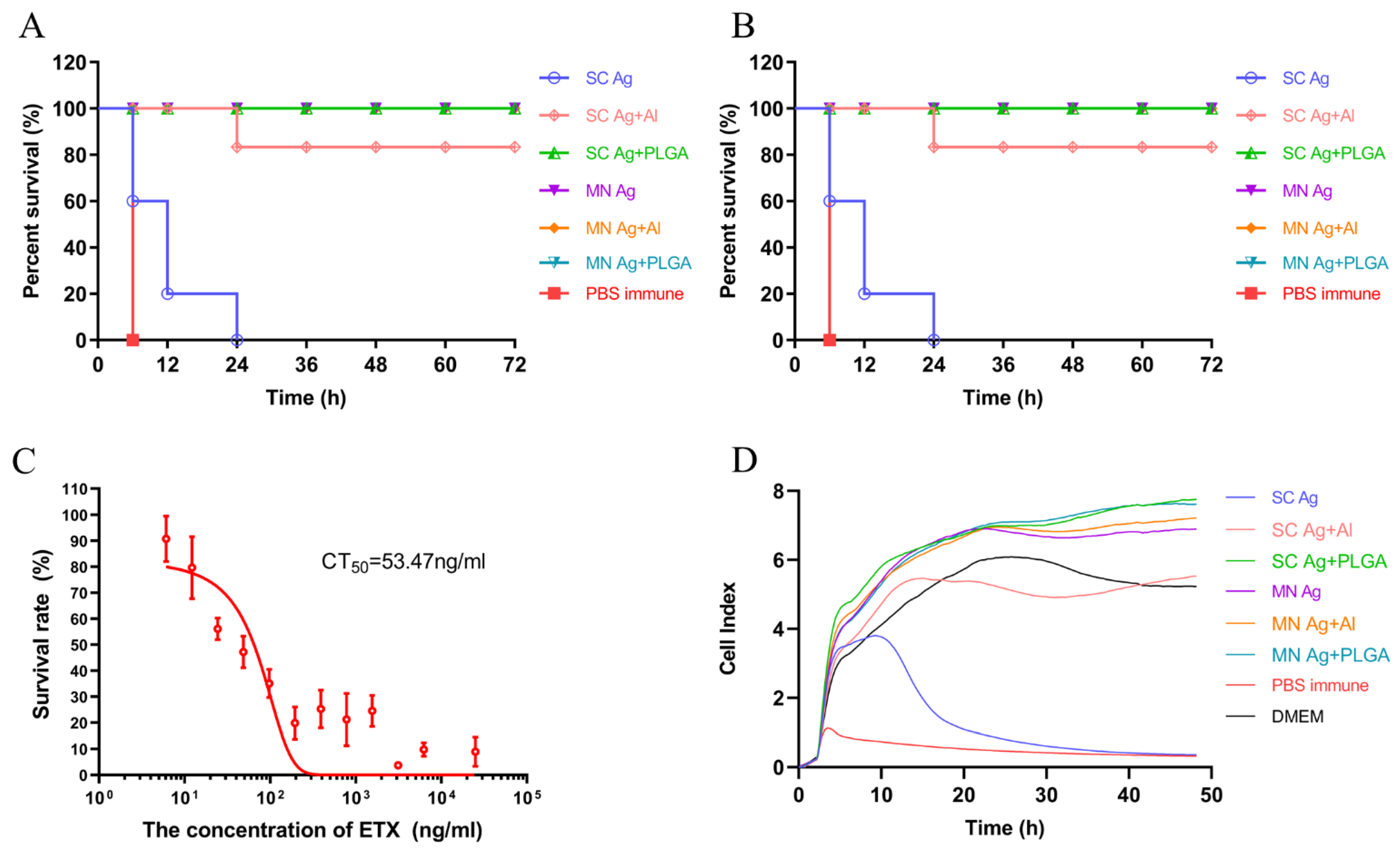
2.6. Protective Effect of Ag + PLGA dMN Vaccine
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. Animals
5.2. Preparation of Vaccine Antigens and Toxin Proteins
5.3. Preparation and Characterization of PLGA-DDAB Nanoparticles
5.4. Adsorption Rate Testing
5.5. Cell Viability Assay for PLGA-DDAB Nanoparticles
5.6. Preparation and Characterization of PLGA-DDAB dMN
5.7. MN Performance Assessment
5.8. In Vivo Release Time Determination
5.9. PLGA-DDAB-rETXY196E-C dMN Immunization in Mice
5.10. Mouse Challenge Experiment
5.11. ELISA Detection of Antibody Levels in Immune Sera and the Content of MN Vaccine
5.12. In Vitro Neutralization Assay
5.13. Cytokine Detection of Splenocytes Stimulated by rETXY196E-C In Vitro
5.14. Pathological Damage in rETXY196E-C Immunized Mice
5.15. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lewis, M.; Weaver, C.D.; McClain, M.S. Identification of Small Molecule Inhibitors of Clostridium perfringens ε-Toxin Cytotoxicity Using a Cell-Based High-Throughput Screen. Toxins 2010, 2, 1825–1847. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kumar, S.A.; Jhan, Y.Y.; Bishop, C.J. Engineering DNA vaccines against infectious diseases. Acta Biomater. 2018, 80, 31–47. [Google Scholar] [PubMed]
- Shah, R.R.; Hassett, K.J.; Brito, L.A. Overview of Vaccine Adjuvants: Introduction, History, and Current Status. Methods Mol. Biol. 2017, 1494, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Smith, D.; Zhao, Z.; Harmon, T.; Pentel, P.R.; Ehrich, M.; Zhang, C. Alum as an adjuvant for nanoparticle based vaccines: A case study with a hybrid nanoparticle-based nicotine vaccine. Nanomedicine 2019, 20, 102023. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Wang, L.; Liu, Y.; Chen, X.; Li, J.; Yang, T.; An, W.; Ma, X.; Pan, R.; Ma, G. Comparison of PLA microparticles and alum as adjuvants for H5N1 influenza split vaccine: Adjuvanticity evaluation and preliminary action mode analysis. Pharm. Res. 2014, 31, 1015–1031. [Google Scholar] [CrossRef]
- Danhier, F.; Ansorena, E.; Silva, J.M.; Coco, R.; Le Breton, A.; Préat, V. PLGA-based nanoparticles: An overview of biomedical applications. J. Control. Release 2012, 161, 505–522. [Google Scholar] [CrossRef]
- Han, S.; Ma, W.; Jiang, D.; Sutherlin, L.; Zhang, J.; Lu, Y.; Huo, N.; Chen, Z.; Engle, J.W.; Wang, Y.; et al. Intracellular signaling pathway in dendritic cells and antigen transport pathway in vivo mediated by an OVA@DDAB/PLGA nano-vaccine. J. Nanobiotechnol. 2021, 19, 394. [Google Scholar] [CrossRef]
- Mönkäre, J.; Pontier, M.; van Kampen, E.E.M.; Du, G.; Leone, M.; Romeijn, S.; Nejadnik, M.R.; O’Mahony, C.; Slütter, B.; Jiskoot, W.; et al. Development of PLGA nanoparticle loaded dissolving microneedles and comparison with hollow microneedles in intradermal vaccine delivery. Eur. J. Pharm. Biopharm. 2018, 129, 111–121. [Google Scholar] [CrossRef]
- Thomas, C.; Rawat, A.; Hope-Weeks, L.; Ahsan, F. Aerosolized PLA and PLGA nanoparticles enhance humoral, mucosal and cytokine responses to hepatitis B vaccine. Mol. Pharm. 2011, 8, 405–415. [Google Scholar] [CrossRef]
- Zheng, X.; Zhu, J.; Zheng, C.; Tan, Z.; Ji, Z.; Tao, J.; Zhao, Y.; Ji, Z.; Hu, Y. Dissolving Microneedle Arrays as a Hepatitis B Vaccine Delivery System Adjuvanted by APC-Targeted Poly (Lactic-co-Glycolic Acid) (PLGA) Nanoparticles. AAPS PharmSciTech 2023, 24, 42. [Google Scholar] [CrossRef]
- Rosas, J.E.; Hernández, R.M.; Gascón, A.R.; Igartua, M.; Guzman, F.; Patarroyo, M.E.; Pedraz, J.L. Biodegradable PLGA microspheres as a delivery system for malaria synthetic peptide SPf66. Vaccine 2001, 19, 4445–4451. [Google Scholar] [CrossRef]
- Carcaboso, A.M.; Hernández, R.M.; Igartua, M.; Rosas, J.E.; Patarroyo, M.E.; Pedraz, J.L. Potent, long lasting systemic antibody levels and mixed Th1/Th2 immune response after nasal immunization with malaria antigen loaded PLGA microparticles. Vaccine 2004, 22, 1423–1432. [Google Scholar] [CrossRef]
- Fairley, S.J.; Singh, S.R.; Yilma, A.N.; Waffo, A.B.; Subbarayan, P.; Dixit, S.; Taha, M.A.; Cambridge, C.D.; Dennis, V.A. Chlamydia trachomatis recombinant MOMP encapsulated in PLGA nanoparticles triggers primarily T helper 1 cellular and antibody immune responses in mice: A desirable candidate nanovaccine. Int. J. Nanomed. 2013, 8, 2085–2099. [Google Scholar] [CrossRef]
- Taha, M.A.; Singh, S.R.; Dennis, V.A. Biodegradable PLGA85/15 nanoparticles as a delivery vehicle for Chlamydia trachomatis recombinant MOMP-187 peptide. Nanotechnology 2012, 23, 325101. [Google Scholar] [CrossRef] [PubMed]
- Boopathy, A.V.; Mandal, A.; Kulp, D.W.; Menis, S.; Bennett, N.R.; Watkins, H.C.; Wang, W.; Martin, J.T.; Thai, N.T.; He, Y.; et al. Enhancing humoral immunity via sustained-release implantable microneedle patch vaccination. Proc. Natl. Acad. Sci. USA 2019, 116, 16473–16478. [Google Scholar] [CrossRef] [PubMed]
- Luo, Z.; Sun, W.; Fang, J.; Lee, K.; Li, S.; Gu, Z.; Dokmeci, M.R.; Khademhosseini, A. Biodegradable Gelatin Methacryloyl Microneedles for Transdermal Drug Delivery. Adv. Healthc. Mater. 2019, 8, e1801054. [Google Scholar] [CrossRef]
- Chu, L.Y.; Ye, L.; Dong, K.; Compans, R.W.; Yang, C.; Prausnitz, M.R. Enhanced Stability of Inactivated Influenza Vaccine Encapsulated in Dissolving Microneedle Patches. Pharm. Res. 2016, 33, 868–878. [Google Scholar] [CrossRef]
- Edens, C.; Collins, M.L.; Goodson, J.L.; Rota, P.A.; Prausnitz, M.R. A microneedle patch containing measles vaccine is immunogenic in non-human primates. Vaccine 2015, 33, 4712–4718. [Google Scholar] [CrossRef]
- Kolluru, C.; Gomaa, Y.; Prausnitz, M.R. Development of a thermostable microneedle patch for polio vaccination. Drug Deliv. Transl. Res. 2019, 9, 192–203. [Google Scholar] [CrossRef]
- Larrañeta, E.; McCrudden, M.T.; Courtenay, A.J.; Donnelly, R.F. Microneedles: A New Frontier in Nanomedicine Delivery. Pharm. Res. 2016, 33, 1055–1073. [Google Scholar] [CrossRef]
- Braz Gomes, K.; D’Souza, B.; Vijayanand, S.; Menon, I.; D’Souza, M.J. A dual-delivery platform for vaccination using antigen-loaded nanoparticles in dissolving microneedles. Int. J. Pharm. 2022, 613, 121393. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Liu, Y.; Wang, L.; Liu, Y.; Zhang, W.; Fan, B.; Ma, X.; Yuan, Q.; Ma, G.; Su, Z. Enhanced humoral and cell-mediated immune responses generated by cationic polymer-coated PLA microspheres with adsorbed HBsAg. Mol. Pharm. 2014, 11, 1772–1784. [Google Scholar] [CrossRef]
- Maughan, C.N.; Preston, S.G.; Williams, G.R. Particulate inorganic adjuvants: Recent developments and future outlook. J. Pharm. Pharmacol. 2015, 67, 426–449. [Google Scholar] [CrossRef] [PubMed]
- Koerner, J.; Horvath, D.; Herrmann, V.L.; MacKerracher, A.; Gander, B.; Yagita, H.; Rohayem, J.; Groettrup, M. PLGA-particle vaccine carrying TLR3/RIG-I ligand Riboxxim synergizes with immune checkpoint blockade for effective anti-cancer immunotherapy. Nat. Commun. 2021, 12, 2935. [Google Scholar] [CrossRef] [PubMed]
- Vassilieva, E.V.; Kalluri, H.; McAllister, D.; Taherbhai, M.T.; Esser, E.S.; Pewin, W.P.; Pulit-Penaloza, J.A.; Prausnitz, M.R.; Compans, R.W.; Skountzou, I. Improved immunogenicity of individual influenza vaccine components delivered with a novel dissolving microneedle patch stable at room temperature. Drug Deliv. Transl. Res. 2015, 5, 360–371. [Google Scholar] [CrossRef]
- Chen, M.C.; Lai, K.Y.; Ling, M.H.; Lin, C.W. Enhancing immunogenicity of antigens through sustained intradermal delivery using chitosan microneedles with a patch-dissolvable design. Acta Biomater. 2018, 65, 66–75. [Google Scholar] [CrossRef]
- Caudill, C.; Perry, J.L.; Iliadis, K.; Tessema, A.T.; Lee, B.J.; Mecham, B.S.; Tian, S.; DeSimone, J.M. Transdermal vaccination via 3D-printed microneedles induces potent humoral and cellular immunity. Proc. Natl. Acad. Sci. USA 2021, 118, e2102595118. [Google Scholar] [CrossRef]
- Li, S.; Xia, D.; Prausnitz, M.R. Efficient Drug Delivery into Skin Using a Biphasic Dissolvable Microneedle Patch with Water-Insoluble Backing. Adv. Funct. Mater. 2021, 31, 2103359. [Google Scholar] [CrossRef]
- Yang, Y.; Chu, H.; Zhang, Y.; Xu, L.; Luo, R.; Zheng, H.; Yin, T.; Li, Z. Rapidly separable bubble microneedle patch for effective local anesthesia. Nano Res. 2022, 15, 8336–8344. [Google Scholar] [CrossRef]
- Zhu, L.; Zhuang, J.; Zhao, Z.; Huang, Y.; Sun, J.; Liu, F.; Xue, Q.; Wu, D. Preparation and transdermal effect of a tip-loaded bubble-soluble microneedle. Sheng Wu Gong Cheng Xue Bao 2022, 38, 2281–2291. [Google Scholar] [CrossRef]
- Ning, X.; Chen, S.; Yang, Y.; Hwang, J.; Wiraja, C.; Zhang, C.; Liu, W.; Liu, L.; Xu, C. Photodynamic Bubble-Generating Microneedles for Enhanced Transdermal Cancer Therapy. ACS Appl. Polym. Mater. 2021, 3, 6502–6512. [Google Scholar] [CrossRef]
- Wang, Q.L.; Zhu, D.D.; Liu, X.B.; Chen, B.Z.; Guo, X.D. Microneedles with Controlled Bubble Sizes and Drug Distributions for Efficient Transdermal Drug Delivery. Sci. Rep. 2016, 6, 38755. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Kang, L.; Gao, S.; Zhou, Y.; Su, L.; Xin, W.; Su, Y.; Wang, J. Expression and purification of functional Clostridium perfringens alpha and epsilon toxins in Escherichia coli. Protein Expr. Purif. 2011, 77, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Yao, W.; Kang, L.; Gao, S.; Zhuang, X.; Zhang, T.; Yang, H.; Ji, B.; Xin, W.; Wang, J. Amino acid residue Y196E substitution and C-terminal peptide synergistically alleviate the toxicity of Clostridium perfringens epsilon toxin. Toxicon 2015, 100, 46–52. [Google Scholar] [CrossRef]
- Gossmann, R.; Langer, K.; Mulac, D. New Perspective in the Formulation and Characterization of Didodecyldimethylammonium Bromide (DMAB) Stabilized Poly(Lactic-co-Glycolic Acid) (PLGA) Nanoparticles. PLoS ONE 2015, 10, e0127532. [Google Scholar] [CrossRef]
- Li, W.; Terry, R.N.; Tang, J.; Feng, M.R.; Schwendeman, S.P.; Prausnitz, M.R. Rapidly separable microneedle patch for the sustained release of a contraceptive. Nat. Biomed. Eng. 2019, 3, 220–229. [Google Scholar] [CrossRef]
- Zhao, B.; Jin, Z.; Yu, Y.; Li, Y.; Wang, J.; Wan, W.; Hu, C.; Li, X.; Li, Y.; Xin, W.; et al. A Thermostable Dissolving Microneedle Vaccine with Recombinant Protein of Botulinum Neurotoxin Serotype A. Toxins 2022, 14, 881. [Google Scholar] [CrossRef]
- Bai, X.; Hu, C.; Jin, Z.; Wan, W.; Li, Y.; Wang, J.; Li, Y.; Gao, S.; Wang, J. Establishment of a thermostable direct hemolysin DAS-ELISA detection method for Vibrio para-haemolyticus. Chin. J. Zoonoses 2022, 38, 666–672. [Google Scholar]




| Group | Size (nm) | Zeta Potential (mv) | PDI |
|---|---|---|---|
| PLGA | 164.0 ± 37.4 | −16.2 ± 1.0 | 0.157 ± 0.016 |
| PLGA-DDAB | 176.7 ± 33.4 | 39.3 ± 1.2 | 0.052 ± 0.022 |
| No. | Group (n = 5) | Dose of Antigen (µg) | NPs Content (µg) | |
|---|---|---|---|---|
| 1 | MN | Ag | 10 | - |
| 2 | Ag + Al | 10 | - | |
| 3 | Ag + PLGA | 10 | 400 | |
| 4 | PBS | - | - | |
| 5 | SC | Ag | 10 | - |
| 6 | Ag + Al | 10 | - | |
| 7 | Ag + PLGA | 10 | 400 | |
| 8 | PBS | - | - | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wan, W.; Li, Y.; Wang, J.; Jin, Z.; Xin, W.; Kang, L.; Wang, J.; Li, X.; Cao, Y.; Yang, H.; et al. PLGA Nanoparticle-Based Dissolving Microneedle Vaccine of Clostridium perfringens ε Toxin. Toxins 2023, 15, 461. https://doi.org/10.3390/toxins15070461
Wan W, Li Y, Wang J, Jin Z, Xin W, Kang L, Wang J, Li X, Cao Y, Yang H, et al. PLGA Nanoparticle-Based Dissolving Microneedle Vaccine of Clostridium perfringens ε Toxin. Toxins. 2023; 15(7):461. https://doi.org/10.3390/toxins15070461
Chicago/Turabian StyleWan, Wei, Yue Li, Jing Wang, Zhiying Jin, Wenwen Xin, Lin Kang, Junhong Wang, Xiaoyang Li, Yakun Cao, Hao Yang, and et al. 2023. "PLGA Nanoparticle-Based Dissolving Microneedle Vaccine of Clostridium perfringens ε Toxin" Toxins 15, no. 7: 461. https://doi.org/10.3390/toxins15070461
APA StyleWan, W., Li, Y., Wang, J., Jin, Z., Xin, W., Kang, L., Wang, J., Li, X., Cao, Y., Yang, H., Wang, J., & Gao, S. (2023). PLGA Nanoparticle-Based Dissolving Microneedle Vaccine of Clostridium perfringens ε Toxin. Toxins, 15(7), 461. https://doi.org/10.3390/toxins15070461





