Urethral Sphincter Botulinum Toxin A Injection for Non-Spinal Cord Injured Patients with Voiding Dysfunction without Anatomical Obstructions: Which Patients Benefit Most?
Abstract
1. Introduction
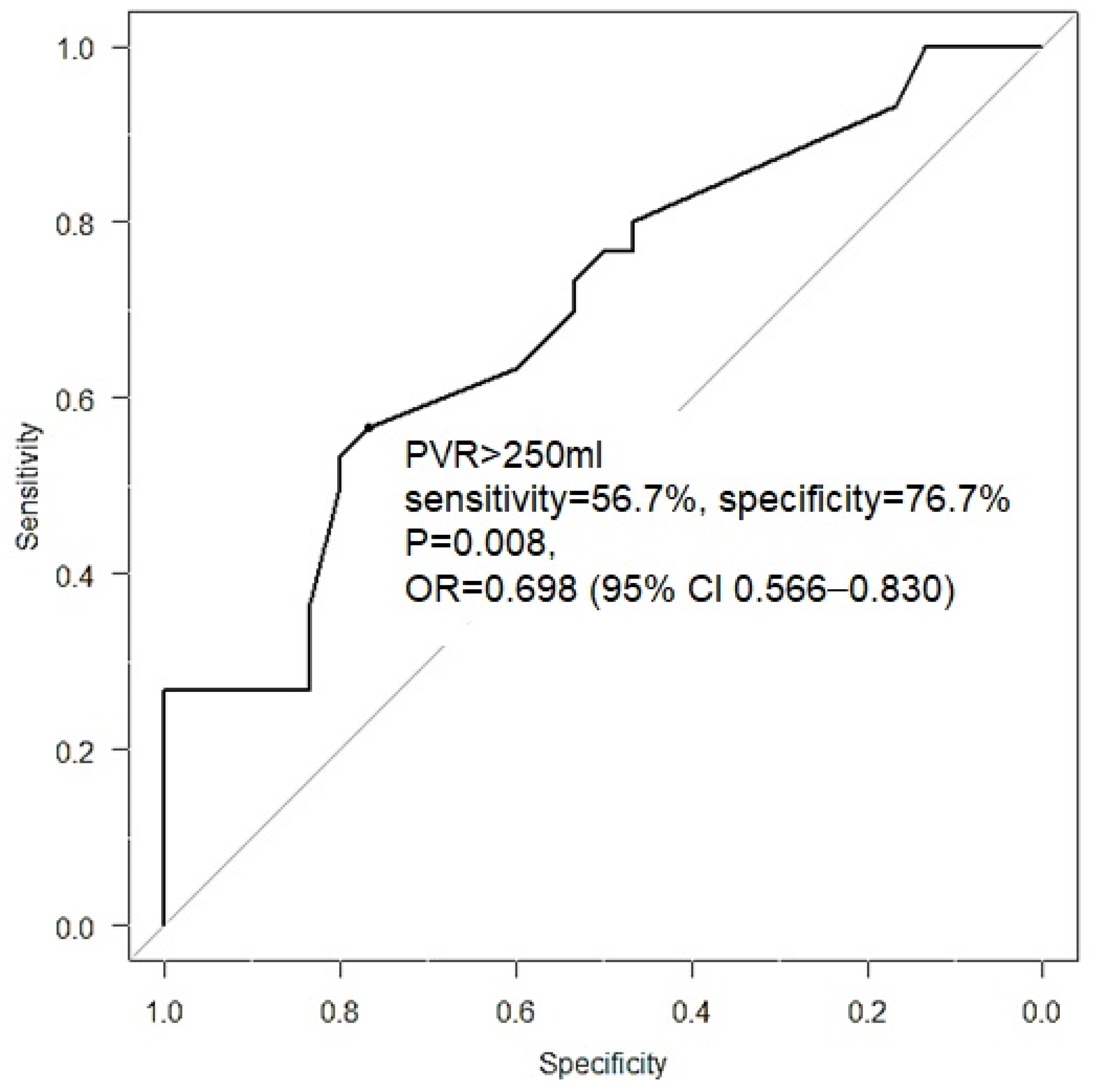
2. Results
3. Discussion
4. Conclusions
5. Materials and Methods
Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Abrams, P.; Cardozo, L.; Fall, M.; Griffiths, D.; Rosier, P.; Ulmsten, U.; Van Kerrebroeck, P.; Victor, A.; Wein, A.; Standardisation Sub-Committee of the International Continence Society. The standardisation of terminology of lower urinary tract function: Report from the Standardisation Sub-committee of the International Continence Society. Neurourol. Urodyn. 2002, 21, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Kuo, H.-C. Pathophysiology of Lower Urinary Tract Symptoms in Aged Men without Bladder Outlet Obstruction. Urol. Int. 2000, 64, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Peng, C.; Kuo, H. Will detrusor acontractility recover after medical or surgical treatment? A longitudinal long-term urodynamic follow-up. Neurourol. Urodyn. 2021, 40, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Dykstra, D.D.; Sidi, A.A.; Scott, A.B.; Pagel, J.M.; Goldish, G.D. Effects of Botulinum a Toxin on Detrusor-Sphincter Dyssynergia in Spinal Cord Injury Patients. J. Urol. 1988, 139, 919–922. [Google Scholar] [CrossRef] [PubMed]
- Phelan, M.W.; Franks, M.; Somogyi, G.T.; Yokoyama, T.; Fraser, M.O.; Lavelle, J.P.; Yoshimura, N.; Chancellor, M.B. Botulinum toxin urethral sphincter injection to restore bladder emptying in men and women with voiding dysfunction. J. Urol. 2001, 165, 1107–1110. [Google Scholar] [CrossRef] [PubMed]
- Dong, M.; Yeh, F.; Tepp, W.H.; Dean, C.; Johnson, E.A.; Janz, R.; Chapman, E.R. SV2 Is the Protein Receptor for Botulinum Neurotoxin A. Science 2006, 312, 592–596. [Google Scholar] [CrossRef]
- Kao, Y.-L.; Huang, K.-H.; Kuo, H.-C.; Ou, Y.-C. The Therapeutic Effects and Pathophysiology of Botulinum Toxin A on Voiding Dysfunction Due to Urethral Sphincter Dysfunction. Toxins 2019, 11, 728. [Google Scholar] [CrossRef]
- Jiang, Y.-H.; Jhang, J.-F.; Chen, S.-F.; Kuo, H.-C. Videourodynamic factors predictive of successful onabotulinumtoxinA urethral sphincter injection for neurogenic or non-neurogenic detrusor underactivity. LUTS Low. Urin. Tract Symptoms 2019, 11, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Jhang, J.-F.; Kuo, H.-C. Botulinum Toxin A and Lower Urinary Tract Dysfunction: Pathophysiology and Mechanisms of Action. Toxins 2016, 8, 120. [Google Scholar] [CrossRef]
- Dykstra, D.D.; Sidi, A.A. Treatment of detrusor-sphincter dyssynergia with botulinum A toxin: A double-blind study. Arch. Phys. Med. Rehabil. 1990, 71, 24–26. [Google Scholar]
- Jiang, Y.H.; Kuo, H.C. Video-urodynamic characteristics of non-neurogenic, idiopathic underactive bladder in men—A comparison of men with normal tracing and bladder outlet obstruction. PLoS ONE 2017, 12, e0174593. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.-H.; Chuang, F.-C.; Kuo, H.-C. Urodynamic characteristics of detrusor underactivity in women with voiding dysfunction. PLoS ONE 2018, 13, e0198764. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, S.-M.; Lin, H.-H.; Kuo, H.-C. Videourodynamic Studies of Women with Voiding Dysfunction. Sci. Rep. 2017, 7, 6845. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.-M.; Kuo, H.-C. Causes of Failed Urethral Botulinum Toxin A Treatment for Emptying Failure. Urology 2007, 70, 763–766. [Google Scholar] [CrossRef]
- Chen, Y.-C.; Kuo, H.-C. Clinical and video urodynamic characteristics of adult women with dysfunctional voiding. J. Formos. Med. Assoc. = Taiwan Yi Zhi 2014, 113, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-K.; Kuo, H.-C. Therapeutic Effects of Botulinum Toxin A, via Urethral Sphincter Injection on Voiding Dysfunction Due to Different Bladder and Urethral Sphincter Dysfunctions. Toxins 2019, 11, 487. [Google Scholar] [CrossRef]
- Hoeritzauer, I.; Phé, V.; Panicker, J. Urologic symptoms and functional neurologic disorders. Handb. Clin. Neurol. 2016, 139, 469–481. [Google Scholar] [CrossRef]
- Chen, S.-F.; Jhang, J.-F.; Jiang, Y.-H.; Kuo, H.-C. Treatment outcomes of detrusor underactivity in women based on clinical and videourodynamic characteristics. Int. Urol. Nephrol. 2022, 54, 1215–1223. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.-H.; Kuo, H.-C. Urothelial Barrier Deficits, Suburothelial Inflammation and Altered Sensory Protein Expression in Detrusor Underactivity. J. Urol. 2017, 197, 197–203. [Google Scholar] [CrossRef]
- Shao, I.-H.; Kuo, H.-C. Role of poor urethral sphincter relaxation in men with voiding dysfunction refractory to α-blocker therapy: Clinical characteristics and predictive factors. LUTS Low. Urin. Tract Symptoms 2019, 11, 8–13. [Google Scholar] [CrossRef]
- Kuo, H.-C. Videourodynamic Analysis of Pathophysiology of Men with Both Storage and Voiding Lower Urinary Tract Symptoms. Urology 2007, 70, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Kuo, H.-C. Recovery of Detrusor Function After Urethral Botulinum A Toxin Injection in Patients with Idiopathic Low Detrusor Contractility and Voiding Dysfunction. Urology 2007, 69, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Apostolidis, A.; Fowler, C.J. The use of botulinum neurotoxin type A (BoNTA) in urology. J. Neural Transm. 2008, 115, 593–605. [Google Scholar] [CrossRef] [PubMed]
- Kuo, H.-C. Botulinum A Toxin Urethral Injection for the Treatment of Lower Urinary Tract Dysfunction. J. Urol. 2003, 170, 1908–1912. [Google Scholar] [CrossRef] [PubMed]
- Abrams, P. Bladder outlet obstruction index, bladder contractility index and bladder voiding efficiency: Three simple indices to define bladder voiding function. BJU Int. 1999, 84, 14–15. [Google Scholar] [CrossRef] [PubMed]
| DU (n = 60) | DV (n = 77) | PRES (n = 24) | Total (n=161) | p-Value | |
|---|---|---|---|---|---|
| Age | 60.3 ± 19.4 | 54.0 ± 22.5 | 67.0 ± 11.6 | 58.1 ± 20.6 | 0.007 |
| Male | n = 19 | n = 10 | n = 14 | n = 43 | 0.000 |
| Female | n = 41 | n = 67 | n = 10 | n = 118 | |
| DM | 30.0% | 19.5% | 29.2% | 23.1% | 0.320 |
| CVA | 18.3% | 11.7% | 8.3% | 12.2% | 0.379 |
| Parkinsonism | 1.7% | 3.9% | 8.3% | 4.1% | 0.309 |
| Cervical cancer s/p radical surgery | 18.3% | 7.8% | 4.2% | 12.2% | 0.013 |
| s/p spine surgery | 13.3% | 3.9% | 8.3% | 8.2% | 0.123 |
| s/p bladder outlet surgery | 78.3% | 26.0% | 45.8% | 44.2% | 0.000 |
| Immune disease | 10.0% | 1.3% | 16.7% | 7.5% | 0.007 |
| Recurrent UTI | 33.3% | 18.2% | 4.2% | 23.8% | 0.008 |
| DU (n = 60) | DV (n = 77) | PRES (n = 24) | p-Value | ||
|---|---|---|---|---|---|
| FSF (mL) | Baseline | 172.8 ± 80.9 | 105.4 ± 53.2 | 149.5 ± 59.0 | 0.068 |
| Follow-up | 165.8 ± 88.9 | 121.7 ± 64.5 | 214.3 ± 45.8 | ||
| FS (mL) | Baseline | 241.5 ± 76.8 | 173.9 ± 79.7 | 236.8 ± 89.8 | 0.163 |
| Follow-up | 245.1 ± 127.4 | 202.9 ± 100.9 | 290.3 ± 55.1 | ||
| US (mL) | Baseline | 303.3 ± 117.1 | 209.1 ± 100.9 | 286.0 ± 113.8 | 0.151 |
| Follow-up | 286.6 ± 133.9 | 230.5 ± 105.5 | 336.4 ± 64.2 | ||
| CBC (mL) | Baseline | 402.9 ± 174.3 | 317.9 ± 135.8 | 432.0 ± 115.4 | 0.726 |
| Follow-up | 399.5 ± 168.5 | 296.7 ± 153.3 | 412.4 ± 173.3 | ||
| Compliance (mL/cmH2O) | Baseline | 63.9 ± 96.5 | 40.4 ± 62.5 | 53.8 ± 25.8 | 0.186 |
| Follow-up | 47.4 ± 36.7 | 59.6 ± 71.5 | 52.3 ± 19.5 | ||
| Pdet.Qmax (cmH2O) | Male (BL) | 10.3 ± 11.6 | 34.00 ± 15.4 | 32.0 ± 13.1 | 0.584 |
| Follow-up | 19.3 ± 25.6 | 31.1 ± 17.6 | 27.6 ± 14.6 | ||
| Female (BL) | 5.69 ± 8.09 | 60.1 ± 36.0 | 74.3 ± 90.0 | 0.000 | |
| Follow-up | 4.89 ± 8.76 | 47.6 ± 32.6 * | 13.3 ± 7.37 | ||
| Qmax (mL/s) | Baseline | 2.70 ± 4.41 | 6.54 ± 5.06 | 8.29 ± 5.96 | 0.987 |
| Follow-up | 3.44 ± 5.31 | 7.11 ± 5.58 | 8.71 ± 6.13 | ||
| Volume (mL) | Baseline | 60.5 ± 115.7 | 131.1 ± 117.3 | 219.1 ± 142.5 | 0.961 |
| Follow-up | 73.1 ± 130.6 | 139.3 ± 131.4 | 214.4 ± 163.7 | ||
| PVR (mL) | Baseline | 344.4 ± 206.8 | 183.1 ± 143.8 | 198.3 ± 160.3 | 0.680 |
| Follow-up | 326.5 ± 197.1 | 195.3 ± 147.8 | 231.0 ± 176.8 | ||
| VE | Baseline | 0.16 ± 0.29 | 0.41 ± 0.34 | 0.52 ± 0.38 | 0.811 |
| Follow-up | 0.18 ± 0.32 | 0.38 ± 0.36 | 0.58 ± 0.41 | ||
| BOOI | Male (BL) | 8.07 ± 9.21 | 16.0 ± 13.6 | 13.5 ± 19.2 | 0.580 |
| Follow-up | 15.0 ± 24.9 | 10.1 ± 14.8 | 9.75 ± 21.6 | ||
| Female (BL) | −1.51 ± 12.4 | 48.2 ± 35.8 | 53.6 ± 99.4 | 0.002 | |
| Follow-up | −2.83 ± 14.2 | 30.0 ± 33.5 * | −12.6 ± 19.0 |
| GRA = 0–1 (n = 61) | GRA = 2 (n = 69) | GRA = 3 (n = 31) | p-Value | ||
|---|---|---|---|---|---|
| Age (years) | 64.3 ± 17.1 | 54.2 ± 22.5 | 58.2 ± 18.2 | 0.016 | |
| Gender | Male | 21 (48.8%) | 13 (30.2%) | 9 (20.1%) | 0.127 |
| Female | 40 (33.9%) | 56 (47.5%) | 22 (18.6%) | ||
| Voiding dysfunction | DU | 30 (50.0%) | 25 (41.7%) | 5 (8.3%) | 0.002 |
| DV | 18 (23.4%) | 38 (49.4%) | 21 (27.8%) | ||
| PRES | 13 (54.2%) | 6 (25%) | 5 (20.8%) |
| Variables | Odd Ratio (95% CI) | p-Value |
|---|---|---|
| DV | 3.630 (1.617–8.152) | 0.002 |
| Voided volume | 1.004 (1.001–1.008) | 0.014 |
| Cervical Cancer s/p radical surgery | 0.290 (0.092–0.909) | 0.034 |
| Recurrent UTI | 3.949 (1.453–10.732) | 0.007 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, S.-F.; Kuo, H.-C. Urethral Sphincter Botulinum Toxin A Injection for Non-Spinal Cord Injured Patients with Voiding Dysfunction without Anatomical Obstructions: Which Patients Benefit Most? Toxins 2023, 15, 87. https://doi.org/10.3390/toxins15020087
Chen S-F, Kuo H-C. Urethral Sphincter Botulinum Toxin A Injection for Non-Spinal Cord Injured Patients with Voiding Dysfunction without Anatomical Obstructions: Which Patients Benefit Most? Toxins. 2023; 15(2):87. https://doi.org/10.3390/toxins15020087
Chicago/Turabian StyleChen, Sheng-Fu, and Hann-Chorng Kuo. 2023. "Urethral Sphincter Botulinum Toxin A Injection for Non-Spinal Cord Injured Patients with Voiding Dysfunction without Anatomical Obstructions: Which Patients Benefit Most?" Toxins 15, no. 2: 87. https://doi.org/10.3390/toxins15020087
APA StyleChen, S.-F., & Kuo, H.-C. (2023). Urethral Sphincter Botulinum Toxin A Injection for Non-Spinal Cord Injured Patients with Voiding Dysfunction without Anatomical Obstructions: Which Patients Benefit Most? Toxins, 15(2), 87. https://doi.org/10.3390/toxins15020087






