Anatomical Injection Guidelines for Glabellar Frown Lines Based on Ultrasonographic Evaluation
Abstract
:1. Introduction
2. Results
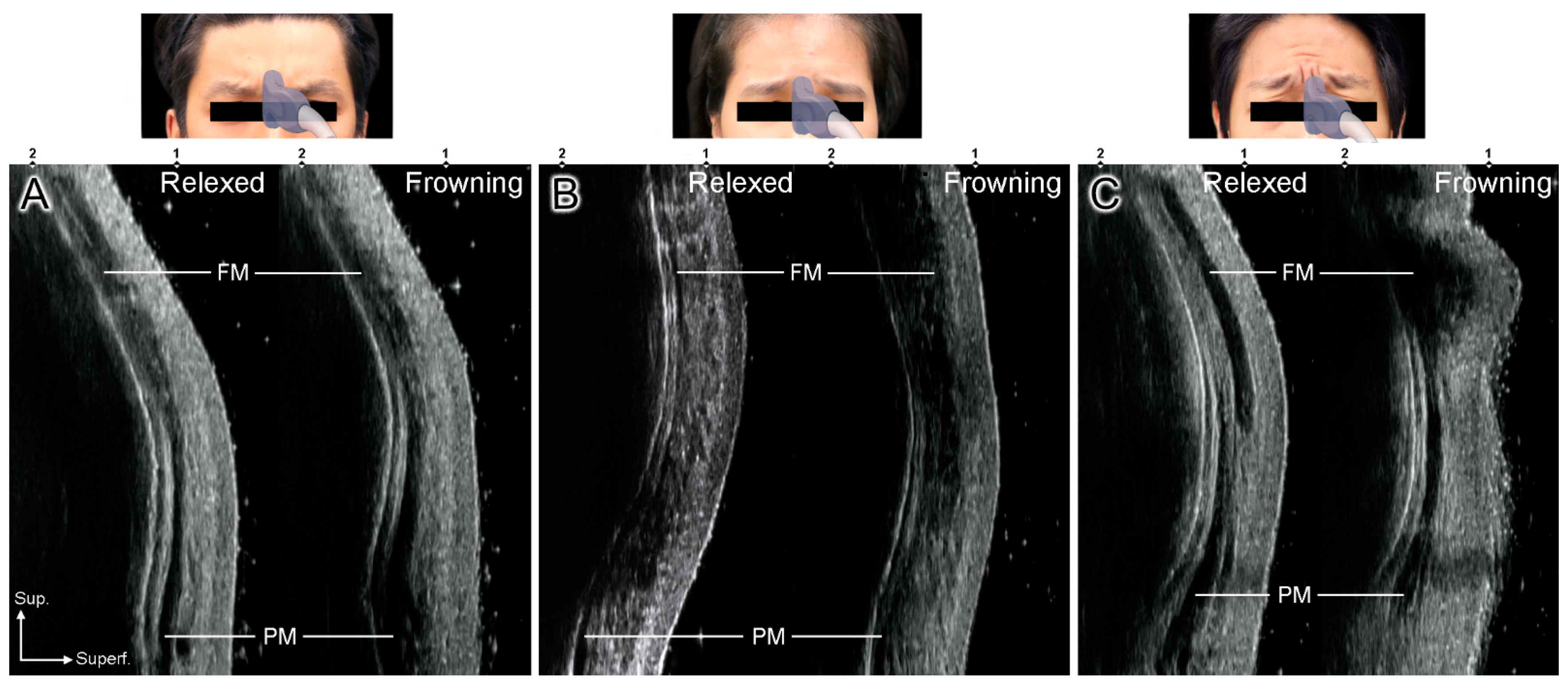
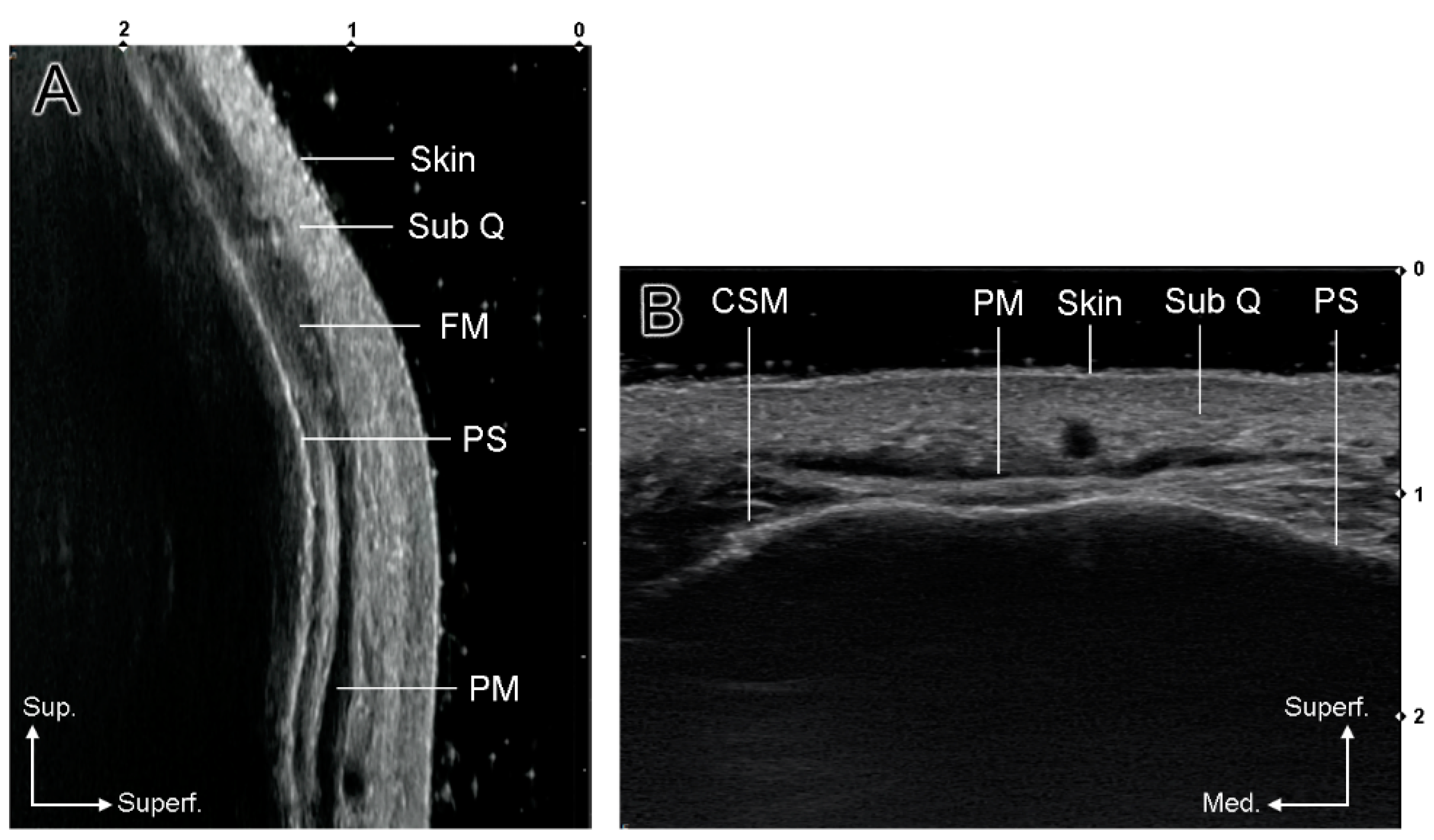
2.1. US-Based Analysis of the Glabellar Frowning Patterns
2.2. Clinical Application
2.2.1. Cases 1 and 2 (Conventional Injection)
2.2.2. Case 3 (Modified Injection)
3. Discussion
4. Materials and Methods
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lewis, M.B.; Bowler, P.J. Botulinum toxin cosmetic therapy correlates with a more positive mood. J. Cosmet. Dermatol. 2009, 8, 24–26. [Google Scholar] [CrossRef]
- Kim, H.-J.; Seo, K.K.; Lee, H.-K.; Kim, J. Clinical Anatomy for Botulinum Toxin Injection. In Clinical Anatomy of the Face for Filler and Botulinum Toxin Injection; Springer: Berlin/Heidelberg, Germany, 2016; pp. 63–68. [Google Scholar]
- Carruthers, J.A.; Lowe, N.J.; Menter, M.A.; Gibson, J.; Nordquist, M.; Mordaunt, J.; Walker, P.; Eadie, N.; BOTOX Glabellar Lines I Study Group. A multicenter, double-blind, randomized, placebo-controlled study of the efficacy and safety of botulinum toxin type A in the treatment of glabellar lines. J. Am. Acad. Dermatol. 2002, 46, 840–849. [Google Scholar] [CrossRef] [PubMed]
- Fagien, S.; Raspaldo, H. Facial rejuvenation with botulinum neurotoxin: An anatomical and experiential perspective. J. Cosmet. Laser Ther. 2007, 9, 23–31. [Google Scholar] [CrossRef]
- de Sanctis Pecora, C.; Pinheiro, M.V.B.; Ventura Ferreira, K.; Jacobino de Barros Nunes, G.; Miot, H.A. The One21 technique: An individualized treatment for glabellar lines based on clinical and anatomical landmarks. Clin. Cosmet. Investig. Dermatol. 2021, 14, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Tansatit, T.; Phumyoo, T.; Jitaree, B.; Sawatwong, W.; Rungsawang, C.; Jiirasutat, N.; Sahraoui, Y.M.E.; Lee, J.H. Ultrasound evaluation of arterial anastomosis of the forehead. J. Cosmet. Dermatol. 2018, 17, 1031–1036. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Lee, K.W.; Tansatit, T.; Kim, H.J. Three-dimensional territory and depth of the corrugator supercilii: Application to botulinum neurotoxin injection. Clin. Anat. 2020, 33, 795–803. [Google Scholar] [CrossRef]
- Rzany, B.; Ascher, B.; Fratila, A.; Monheit, G.D.; Talarico, S.; Sterry, W. Efficacy and safety of 3- and 5-injection patterns (30 and 50 U) of botulinum toxin A (Dysport) for the treatment of wrinkles in the glabella and the central forehead region. Arch. Dermatol. 2006, 142, 320–326. [Google Scholar] [CrossRef] [Green Version]
- Carruthers, A.; Carruthers, J. Prospective, double-blind, randomized, parallel-group, dose-ranging study of botulinum toxin type A in men with glabellar rhytids. Dermatol. Surg. 2005, 31, 1297–1303. [Google Scholar] [CrossRef]
- de Almeida, A.R.T.; da Costa Marques, E.R.; Banegas, R.; Kadunc, B.V. Glabellar contraction patterns: A tool to optimize botulinum toxin treatment. Dermatol. Surg. 2012, 38, 1506–1515. [Google Scholar] [CrossRef] [PubMed]
- De Boulle, K.; Fagien, S.; Sommer, B.; Glogau, R. Treating glabellar lines with botulinum toxin type A-hemagglutinin complex: A review of the science, the clinical data, and patient satisfaction. Clin. Intervig. Aging 2010, 5, 101–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schulze, J.; Neumann, I.; Magid, M.; Finzi, E.; Sinke, C.; Wollmer, M.A.; Krüger, T.H.C. Botulinum toxin for the management of depression: An updated review of the evidence and meta-analysis. J. Psychiatr. Res. 2021, 135, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Carruthers, A.; Kiene, K.; Carruthers, J. Botulinum A exotoxin use in clinical dermatology. J. Am. Acad. Dermatol. 1996, 34, 788–797. [Google Scholar] [CrossRef]
- Imhof, M.; Kühne, U. A phase III study of incobotulinumtoxinA in the treatment of glabellar frown lines. J. Clin. Aesthetic Dermatol. 2011, 4, 28–34. [Google Scholar]
- Seo, K.K. Botulinum Toxin for Asians; Springer: Singapore, 2017; p. 72. [Google Scholar]
- Cho, Y.; Lee, H.-J.; Lee, K.-W.; Lee, K.-L.; Kang, J.S.; Kim, H.-J. Ultrasonographic and three-dimensional analyses at the glabella and radix of the nose for botulinum neurotoxin injection procedures into the procerus muscle. Toxins 2019, 11, 560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, H.J.; Lee, K.L.; Gil, Y.C.; Lee, J.H.; Hu, K.S.; Kim, H.J. Sonographic analysis of the upper labial orbicularis oris and its clinical implications. Aesthetic Surg. J. 2020, 40, 778–783. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.; Moon, H.J.; Kim, J.S.; Yang, E.J. Safe glabellar wrinkle correction with soft tissue filler using doppler ultrasound. Aesthetic Surg. J. 2021, 41, 1081–1089. [Google Scholar] [CrossRef]
- Choi, Y.J.; Lee, K.W.; Gil, Y.C.; Hu, K.S.; Kim, H.J. Ultrasonographic analyses of the forehead region for injectable treatments. Ultrasound Med. Biol. 2019, 45, 2641–2648. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bae, H.; Kim, J.; Seo, K.K.; Hu, K.S.; Kim, S.T.; Kim, H.J. Comparison between conventional blind injections and ultrasound-guided injections of botulinum toxin type A into the masseter: A clinical trial. Toxins 2020, 12, 588. [Google Scholar] [CrossRef]
- Lee, K.L.; Choi, Y.J.; Gil, Y.C.; Hu, K.S.; Tansatit, T.; Kim, H.J. Locational relationship between the lateral border of the frontalis muscle and the superior temporal line. Plast. Reconstr. Surg. 2019, 143, 293e–298e. [Google Scholar] [CrossRef]
- Klein, A.W. Complications and adverse reactions with the use of botulinum toxin. Dis.-A-Mon. 2002, 48, 336–356. [Google Scholar] [CrossRef] [PubMed]
- Yoelin, S.G.; Dhawan, S.S.; Vitarella, D.; Ahmad, W.; Hasan, F.; Abushakra, S. Safety and efficacy of EB-001, a novel type E botulinum toxin, in subjects with glabellar frown lines: Results of a phase 2, randomized, placebo-controlled, ascending-dose study. Plast. Reconstr. Surg. 2018, 142, 847e–855e. [Google Scholar] [CrossRef] [PubMed]
- Carruthers, J.D.; Lowe, N.J.; Menter, M.A.; Gibson, J.; Eadie, N.; Botox Glabellar Lines II Study Group. Double-blind, placebo-controlled study of the safety and efficacy of botulinum toxin type A for patients with glabellar lines. Plast. Reconstr. Surg. 2003, 112, 21S–30S. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.K.; Lee, M.H.; Kim, H.S.; Park, J.T.; Kim, H.J.; Kim, H.J. Histomorphologic approach for the modiolus with reference to reconstructive and aesthetic surgery. J. Craniofac Surg 2013, 24, 1414–1417. [Google Scholar] [CrossRef] [PubMed]
- Flynn, T.C.; Carruthers, A.; Carruthers, J.; Geister, T.L.; Gortelmeyer, R.; Hardas, B.; Himmrich, S.; Kerscher, M.; de Maio, M.; Mohrmann, C.; et al. Validated assessment scales for the upper face. Dermatol. Surg. Off. Publ. Am. Soc. Dermatol. Surg. 2012, 38, 309–319. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-B.; Kim, H.-M.; Ahn, H.; Choi, Y.-J.; Hu, K.-S.; Oh, W.; Kim, H.-J. Anatomical Injection Guidelines for Glabellar Frown Lines Based on Ultrasonographic Evaluation. Toxins 2022, 14, 17. https://doi.org/10.3390/toxins14010017
Kim S-B, Kim H-M, Ahn H, Choi Y-J, Hu K-S, Oh W, Kim H-J. Anatomical Injection Guidelines for Glabellar Frown Lines Based on Ultrasonographic Evaluation. Toxins. 2022; 14(1):17. https://doi.org/10.3390/toxins14010017
Chicago/Turabian StyleKim, Soo-Bin, Hyoung-Moon Kim, Haeryun Ahn, You-Jin Choi, Kyung-Seok Hu, Wook Oh, and Hee-Jin Kim. 2022. "Anatomical Injection Guidelines for Glabellar Frown Lines Based on Ultrasonographic Evaluation" Toxins 14, no. 1: 17. https://doi.org/10.3390/toxins14010017
APA StyleKim, S.-B., Kim, H.-M., Ahn, H., Choi, Y.-J., Hu, K.-S., Oh, W., & Kim, H.-J. (2022). Anatomical Injection Guidelines for Glabellar Frown Lines Based on Ultrasonographic Evaluation. Toxins, 14(1), 17. https://doi.org/10.3390/toxins14010017






