Effective Treatment of Neurological Symptoms with Normal Doses of Botulinum Neurotoxin in Wilson’s Disease: Six Cases and Literature Review
Abstract
1. Introduction
2. Report of Patients
2.1. WD and Palmar Hyperhidrosis (Patient 1)
2.2. WD and Segmental Dystonia (Patient 2)
2.3. WD and Generalized Dystonia and Hypersalivation (Patient 3)
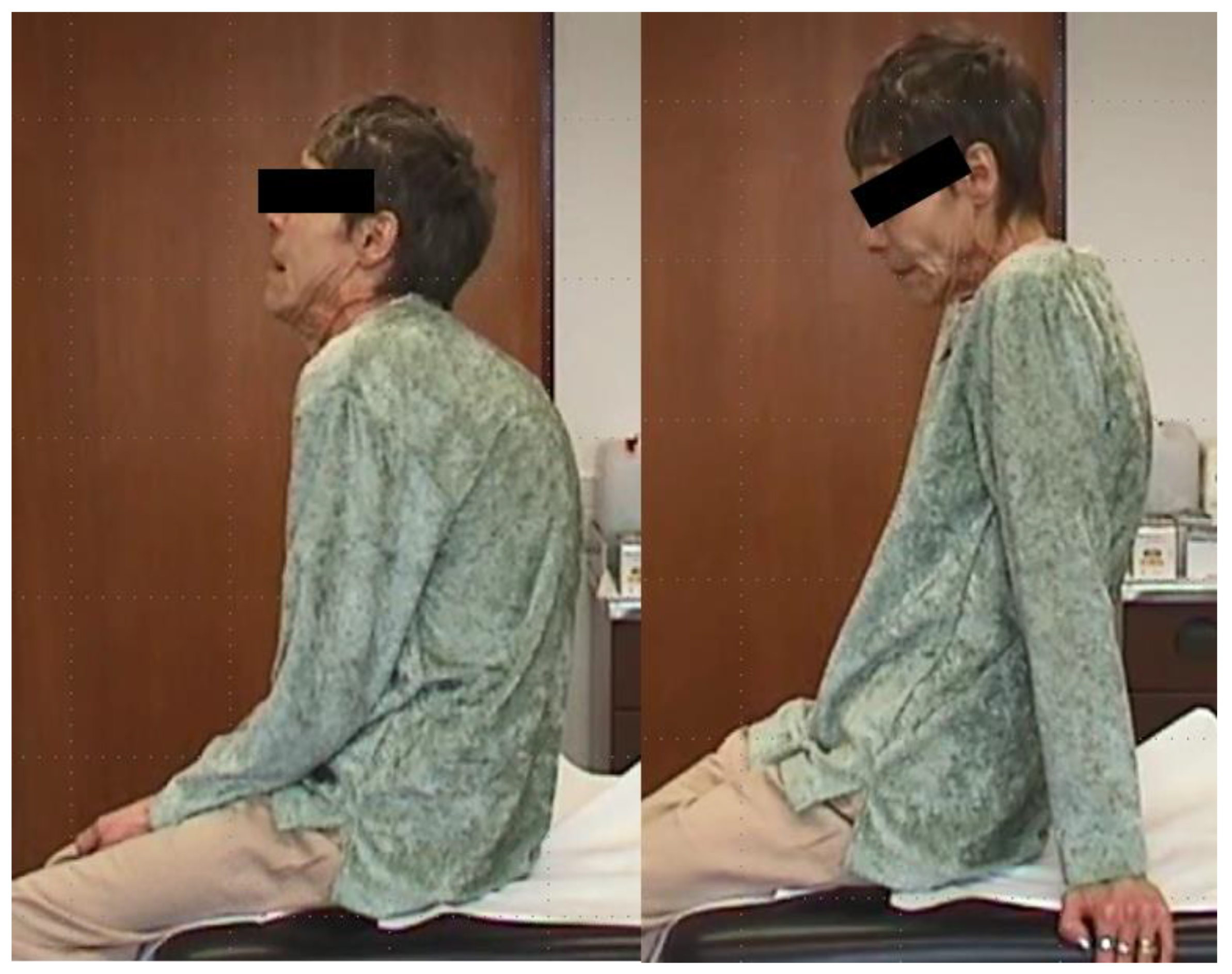
2.4. WD and Generalized Dystonia (Patient 4)
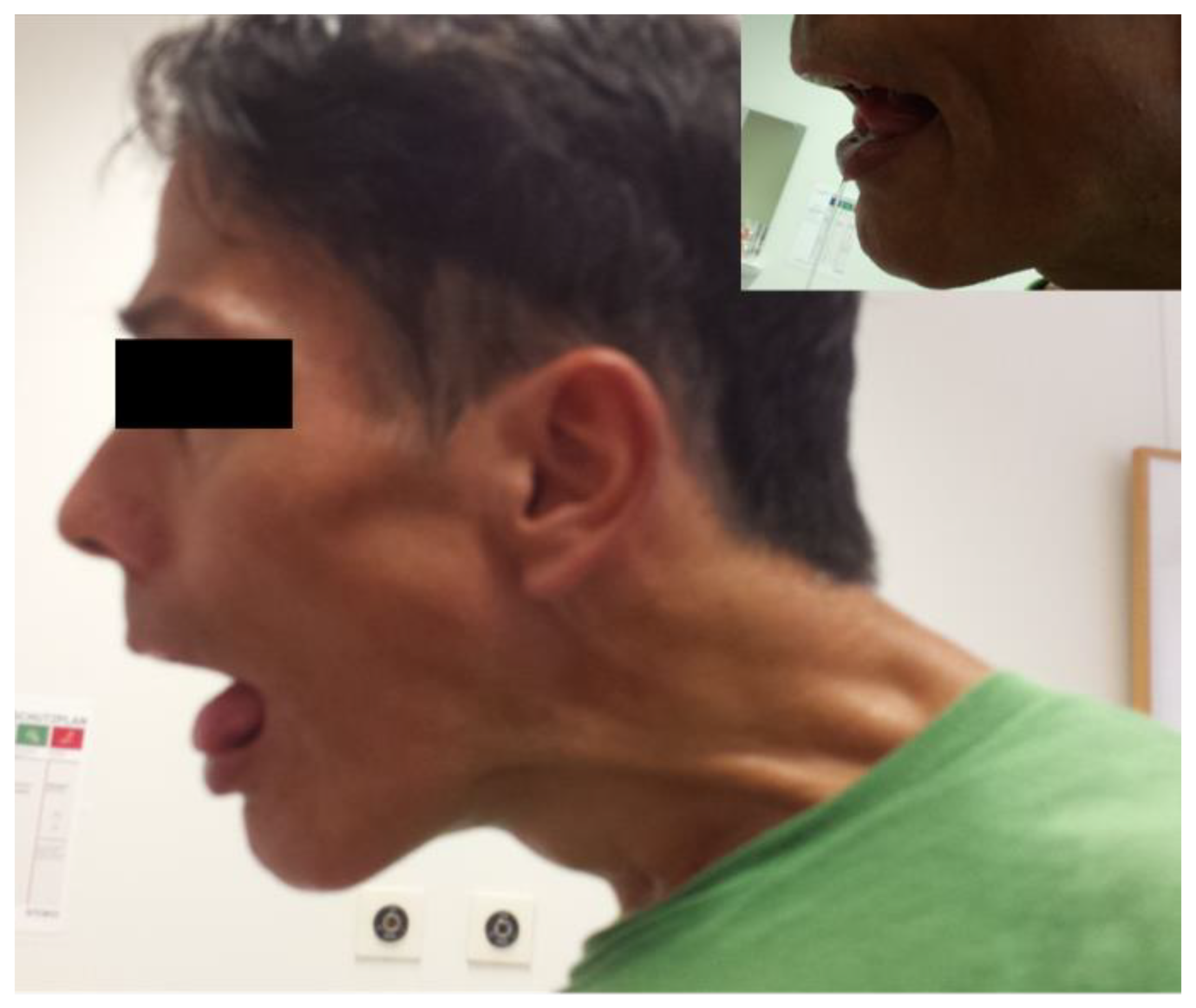
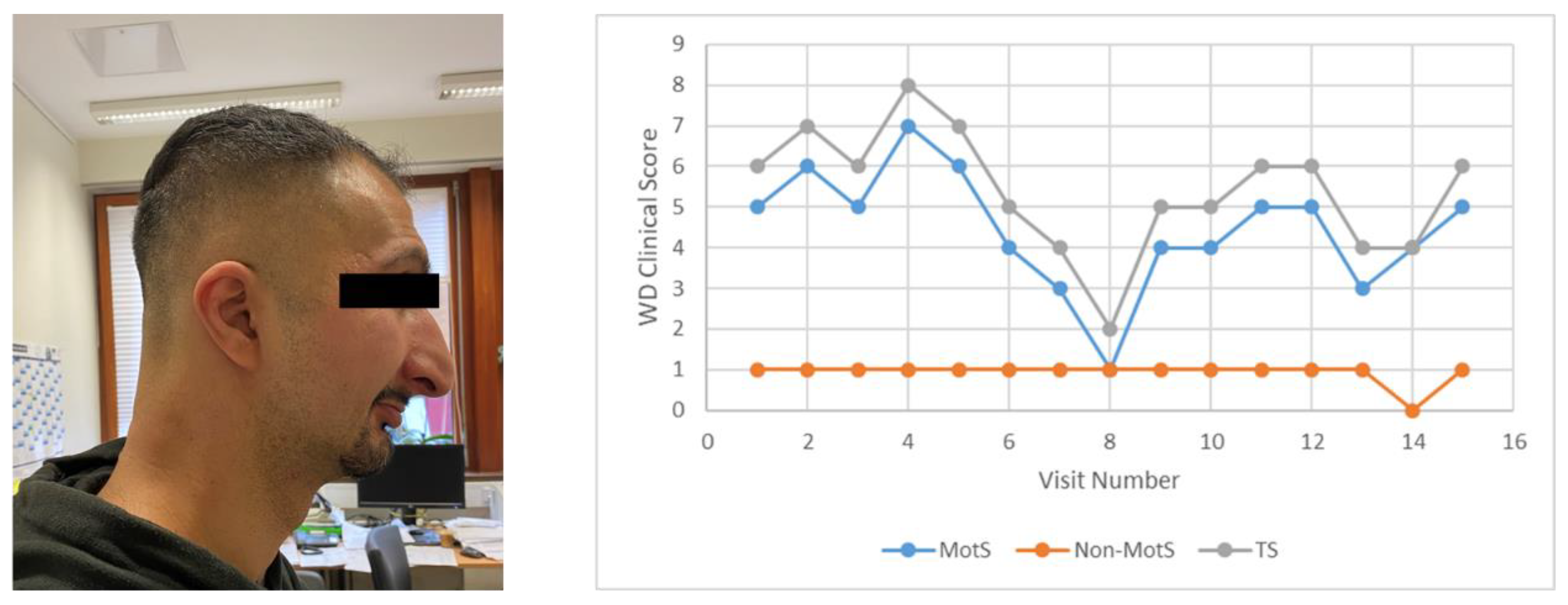
2.5. WD and Multifocal Dystonia and Hypersalivation (Patient 5)
2.6. WD and Spasmodic Dysphonia (Patient 6)
3. Cases in the Literature
4. Discussion
4.1. BoNT/A Is Effective in Normal Doses in WD
4.2. BoNT/A Is Only Used in Severely Affected Patients
4.3. In the Majority of WD Patients, There Is No Indication for BoNT/A Treatment
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Herrero, B.A.; Ecklung, A.E.; Streett, C.S.; Ford, D.F.; King, J.K. Experimental botulism in monkeys—A clinical pathological study. Exp. Mol. Pathol. 1967, 6, 84–95. [Google Scholar] [CrossRef]
- Arnon, S.S.; Schechter, R.; Inglesby, T.V.; Henderson, D.A.; Bartlett, J.G.; Ascher, M.S.; Eitzen, E.; Fine, A.D.; Hauer, J.; Working Group on Civilian Biodefense; et al. Botulinum toxin as a biological weapon: Medical and public health management. JAMA 2001, 285, 1059–1070, Erratum in 2001, 285, 2081. [Google Scholar] [CrossRef]
- McCarty, C.L.; Angelo, K.; Beer, K.D.; Cibulskas-White, K.; Quinn, K.; de Fijter, S.; Bokanyi, R.; St Germain, E.; Baransi, K.; Barlow, K.; et al. Large Outbreak of Botulism Associated with a Church Potluck Meal--Ohio, 2015. MMWR Morb. Mortal. Wkly. Rep. 2015, 64, 802–803. [Google Scholar] [CrossRef]
- Shapiro, R.L.; Hatheway, C.; Becher, J.; Swerdlow, D.L. Botulism Surveillance and Emergency Response: A Public Health Strategy for a Global Challenge. JAMA 1997, 278, 433–435. [Google Scholar] [CrossRef] [PubMed]
- Hooper, R.R. The covert use of chemical and biological warfare against United States Strategic Forces. Mil. Med. 1983, 148, 901–902. [Google Scholar] [CrossRef] [PubMed]
- Pirazzini, M.; Tehran, D.A.; Zanetti, G.; Lista, F.; Binz, T.; Shone, C.C.; Rossetto, O.; Montecucco, C. The thioredoxin reductase—Thioredoxin redox system cleaves the interchain disulphide bond of botulinum neurotoxins on the cytosolic surface of synaptic vesicles. Toxicon 2015, 107, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Pirazzini, M.; Bordin, F.; Rossetto, O.; Shone, C.C.; Binz, T.; Montecucco, C. The thioredoxin reductase-thioredoxin system is involved in the entry of tetanus and botulinum neurotoxins in the cytosol of nerve terminals. FEBS Lett. 2013, 587, 150–155. [Google Scholar] [CrossRef]
- Schiavo, G.; Rossetto, O.; Catsicas, S.; Delaureto, P.P.; Dasgupta, B.R.; Benfenati, F.; Montecucco, C.J. Identification of the nerve terminal targets of botulinum neurotoxin serotypes A, D, and E. J. Biol. Chem. 1993, 268, 23784–23787. [Google Scholar] [CrossRef]
- Bremer, P.T.; Pellett, S.; Carolan, J.P.; Tepp, W.H.; Eubanks, L.M.; Allen, K.N.; Johnson, E.A.; Janda, K.D. Metal Ions Effectively Ablate the Action of Botulinum Neurotoxin A. J. Am. Chem. Soc. 2017, 139, 7264–7272. [Google Scholar] [CrossRef]
- Bandmann, O.; Weiss, K.H.; Kaler, S.G. Wilson’s disease and other neurological copper disorders. Lancet Neurol. 2015, 14, 103–113. [Google Scholar] [CrossRef]
- Członkowska, A.; Litwin, T.; Dusek, P.; Ferenci, P.; Lutsenko, S.; Medici, V.; Rybakowski, J.K.; Weiss, K.H.; Schilsky, M.L. Wilson disease. Nat. Rev. Dis. Primers 2018, 4, 21. [Google Scholar] [CrossRef]
- Pfeiffer, R. Wilson’s disease. Semin. Neurol. 2007, 27, 123–132. [Google Scholar] [CrossRef]
- Hefter, H.; Tezayak, O.; Rosenthal, D. Long-term outcome of neurological Wilson’s disease. Park. Rel. Disord. 2019, 49, 48–53. [Google Scholar] [CrossRef]
- Burke, J.F.; Dayalu, P.; Nan, B.; Askari, F.; Brewer, G.J.; Lorincz, M.T. Prognostic significance of neurologic examination findings in Wilson’s disease. Park. Relat. Disord. 2011, 17, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Lorincz, M.T. Neurologic Wilson’s disease. Ann. N. Y. Acad. Sci. 2009, 1184, 173–187. [Google Scholar] [CrossRef]
- Członkowska, A.; Litwin, T.; Dzieżyc, K.; Karliński, M.; Bring, J.; Bjartmar, C. Characteristics of a newly diagnosed Polish cohort of patients with neurological manifestations of Wilson disease evaluated with the Unified Wilson’s Disease Rating Scale. BMC Neurol. 2018, 18, 34. [Google Scholar] [CrossRef] [PubMed]
- Litwin, T.; Dušek, P.; Członkowska, A. Symptomatic treatment of neurologic symptoms in Wilson disease. Handb. Clin. Neurol. 2017, 142, 211–223. [Google Scholar] [PubMed]
- European Association for Study of Liver. EASL Clinical Practice Guidelines: Wilson’s disease. J. Hepatol. 2012, 56, 671–685. [Google Scholar] [CrossRef] [PubMed]
- Roberts, E.A.; Schilsky, M.L. Diagnosis and treatment of Wilson disease: An update. Hepatology 2008, 47, 2089–2111. [Google Scholar] [CrossRef]
- Hölscher, S.; Leinweber, B.; Hefter, H.; Reuner, U.; Günther, P.; Weiss, K.H.; Oertel, W.H.; Möller, J.C. Evaluation of the symptomatic treatment of residual neurological symptoms in Wilson disease. Eur. Neurol. 2010, 64, 83–87. [Google Scholar] [CrossRef]
- Meyer, B.U.; Britton, T.C.; Benecke, R. Wilson’s disease: Normalisation of cortically evoked motor responses with treatment. J. Neurol. 1991, 238, 327–330. [Google Scholar] [CrossRef] [PubMed]
- Meyer, B.U.; Britton, B.C.; Bischoff, C.; Machetanz, J.; Benecke, R.; Conrad, B. Abnormal conduction in corticospinal pathways in Wilson’s disease: Investigation of nine cases with magnetic brain stimulation. Mov. Disord. 1991, 6, 320–323. [Google Scholar] [CrossRef] [PubMed]
- Teive, H.A.; Klüppel, L.E.; Munhoz, R.P.; Becker, N.; Müller, P.R.; Werneck, L.C. Jaw-opening oromandibular dystonia secondary to Wilson’s disease treated with botulinum toxin type A. Arq. Neuropsiquiatr. 2012, 70, 407–409. [Google Scholar] [CrossRef] [PubMed]
- Hassell, T.J.W.; Charles, D. Treatment of blepharospasm and oromandibular dystonia with botulinum toxins. Toxins 2020, 12, 269. [Google Scholar] [CrossRef]
- Joan, D.; Neves, C.M.; Marina, M. Importance of botulinum toxin in symptomatic treatment of Wilson’s disease. Toxicon 2008, 51, 26. [Google Scholar] [CrossRef]
- Litwin, T.; Chabik, G.; Członkowska, A. Acute focal dystonia induced by a tricyclic antidepressant in a patient with Wilson disease: A case report. Neurol. Neurochir. Pol. 2013, 47, 502–506. [Google Scholar] [CrossRef]
- Kuwert, T.; Hefter, H.; Scholz, D.; Milz, M.; Weiss, P.; Arendt, G.; Feinendegen, L.E. Regional cerebral glucose consumption measured by positron emission tomography in patients with Wilson’s disease. Eur. J. Nucl. Med. 1992, 19, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Hefter, H.; Kuwert, T.; Herzog, H.; Herzog, H.; Feinendegen, L.E.; Stremmel, W. Relationship between striatal glucose consumption and copper excretion in patients with Wilson’s disease treated with D-penicillamine. J. Neurol. 1993, 241, 49–53. [Google Scholar] [CrossRef] [PubMed]


| Parameter | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 |
|---|---|---|---|---|---|---|
| Demographical data | ||||||
| Age | 30 | 66 | 64 | 50 | 52 | 35 |
| Sex | FEMALE | FEMALE | FEMALE | MALE | MALE | MALE |
| Age at first diagnosis (years) | 10 | 12 | 15 | 18 | 18 | 5 |
| WD therapy | Trientine® | DPA | Trientine® | DPA | DPA | DPA |
| Clinical score * | ||||||
| MotS | 2 | 5 | 8 | 9 | 9 | 5 |
| Non-MotS | 0 | 0 | 3 | 0 | 2 | 1 |
| TS | 2 | 5 | 11 | 9 | 11 | 6 |
| Laboratory findings ** (of the last visit before recruitment into this study: grey windows indicate values out of the normal range) | ||||||
| Cerulo (mg/dL) | <7 | <7 | 14 | 10 | <7 | <7 |
| CU (mg/dL) | 0.02 | 0.21 | 0.49 | 0.40 | 0.60 | 0.05 |
| AST (U/L) | 25 | 21 | 41 | 34 | 52 | 15 |
| CHE (U/L) | 6079 | 5194 | 5149 | 6744 | 4290 | 3870 |
| 24 h-CU mg/d | 0.041 | 0.045 | 0.092 | 0.037 | 0.059 | 0.377 |
| BoNT/A Therapy (data of the last visit before recruitment: treatment related data and laboratory findings result from the same visit) | ||||||
| Indication | Palmar hyperhidrosis | Segmental dystonia | Hypersalivation | Generalized dystonia | Cervical dystonia hypersalivation | Spasmodic dysphonia |
| Preparation | ona BoNT/A | Abo BoNT/A | inco BoNT/A | inco BoNT/A | inco BoNT/A | ona- or inco BoNT/A |
| Dose of BoNT/A | 100 U/hand | 500–1000 U for neck | 100 U/gland | 200 U for trunk 200 U for left arm | 200 U for CD 100 U/gland | 5–10 U/ side |
| Recommended dose range | 100 U/hand | 500–1000 U for CD | 50–100/gland | Off-label | 200 U for CD 100 U/gland | 5–10 U/ side |
| Efficacy | Good | Moderate | Moderate | Good | Mild/ Moderate | Very good |
| Side effects | Pain during injection | None | None | None | None | None |
| Parameter | Demasio et al., 2008 [25] | Litwin et al., 2013 [26] | Hölscher et al., 2010 [20] | Teive et al., 2012 [23] |
|---|---|---|---|---|
| N | 4 | 1 | 3 | 5 |
| Severity of WD | Severe dystonia, 3 patients to be transplanted | Hand dystonia induced by antidepressants | 2 with dystonia, 1 with tremor | General dystonia |
| Indication | Pain Limb dystonia | Hand dystonia | Dystonia Tremor | Jaw opening dystonia |
| Preparation | n.m. | aboBoNT/A | n.m. | onaBoNT/A |
| Dose | n.m. | n.m. | n.m. | 100 U |
| Efficacy | some functional recovery | complete normalization | n.m. | Mild to moderate improvement |
| Side effects | n.m. | n.m. | n.m. | 3/5 mild dysphagia |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hefter, H.; Samadzadeh, S. Effective Treatment of Neurological Symptoms with Normal Doses of Botulinum Neurotoxin in Wilson’s Disease: Six Cases and Literature Review. Toxins 2021, 13, 241. https://doi.org/10.3390/toxins13040241
Hefter H, Samadzadeh S. Effective Treatment of Neurological Symptoms with Normal Doses of Botulinum Neurotoxin in Wilson’s Disease: Six Cases and Literature Review. Toxins. 2021; 13(4):241. https://doi.org/10.3390/toxins13040241
Chicago/Turabian StyleHefter, Harald, and Sara Samadzadeh. 2021. "Effective Treatment of Neurological Symptoms with Normal Doses of Botulinum Neurotoxin in Wilson’s Disease: Six Cases and Literature Review" Toxins 13, no. 4: 241. https://doi.org/10.3390/toxins13040241
APA StyleHefter, H., & Samadzadeh, S. (2021). Effective Treatment of Neurological Symptoms with Normal Doses of Botulinum Neurotoxin in Wilson’s Disease: Six Cases and Literature Review. Toxins, 13(4), 241. https://doi.org/10.3390/toxins13040241





