A Rabbit Model for the Evaluation of Drugs for Treating the Chronic Phase of Botulism
Abstract
:1. Introduction
2. Results
2.1. Determining the Optimal Sublethal BoNT/A Dose to Induce Chronic Botulism
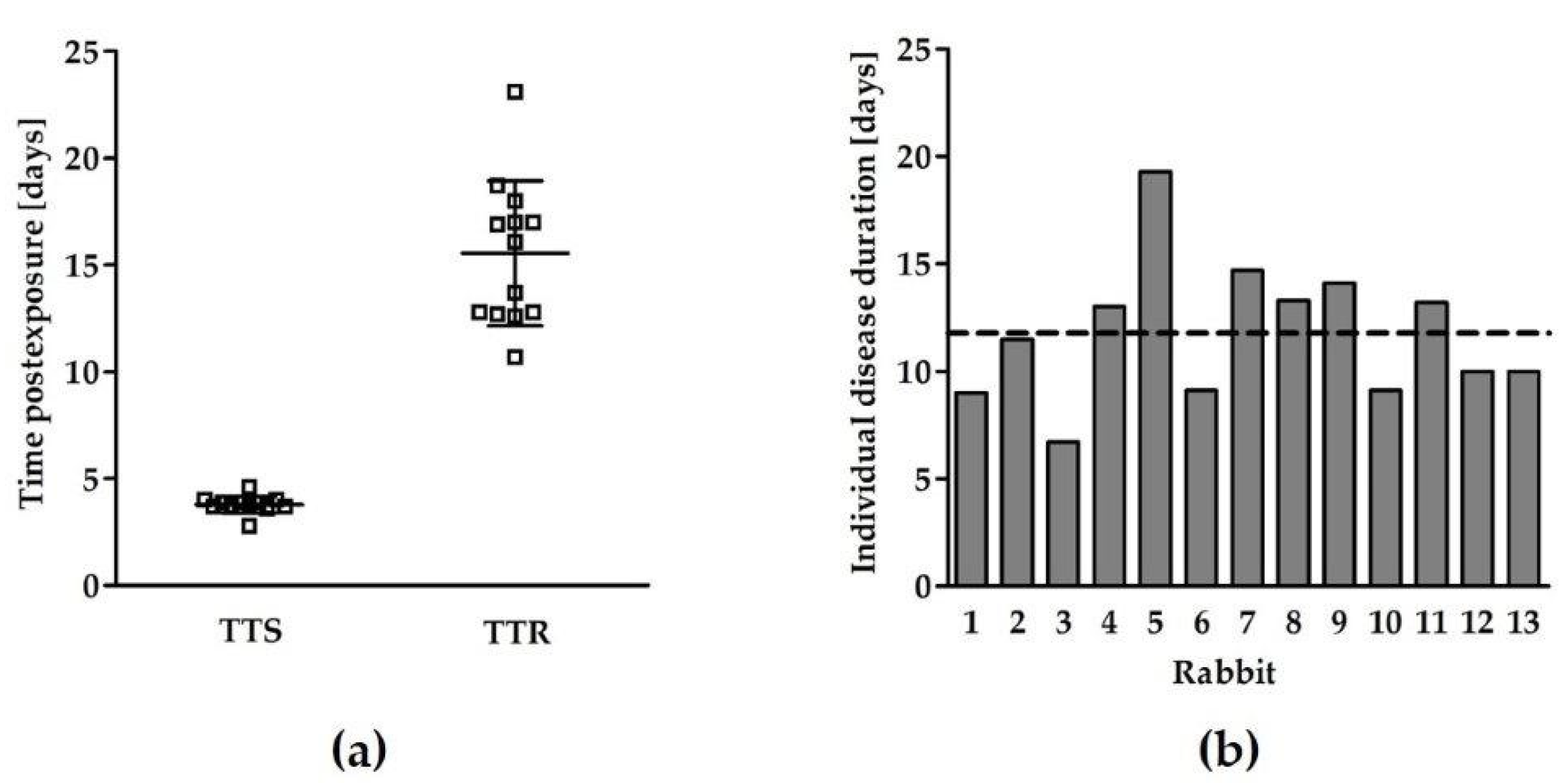
2.2. Characterization of the Chronic Phase of Botulism Induced by a Sublethal Dose of BoNT/A
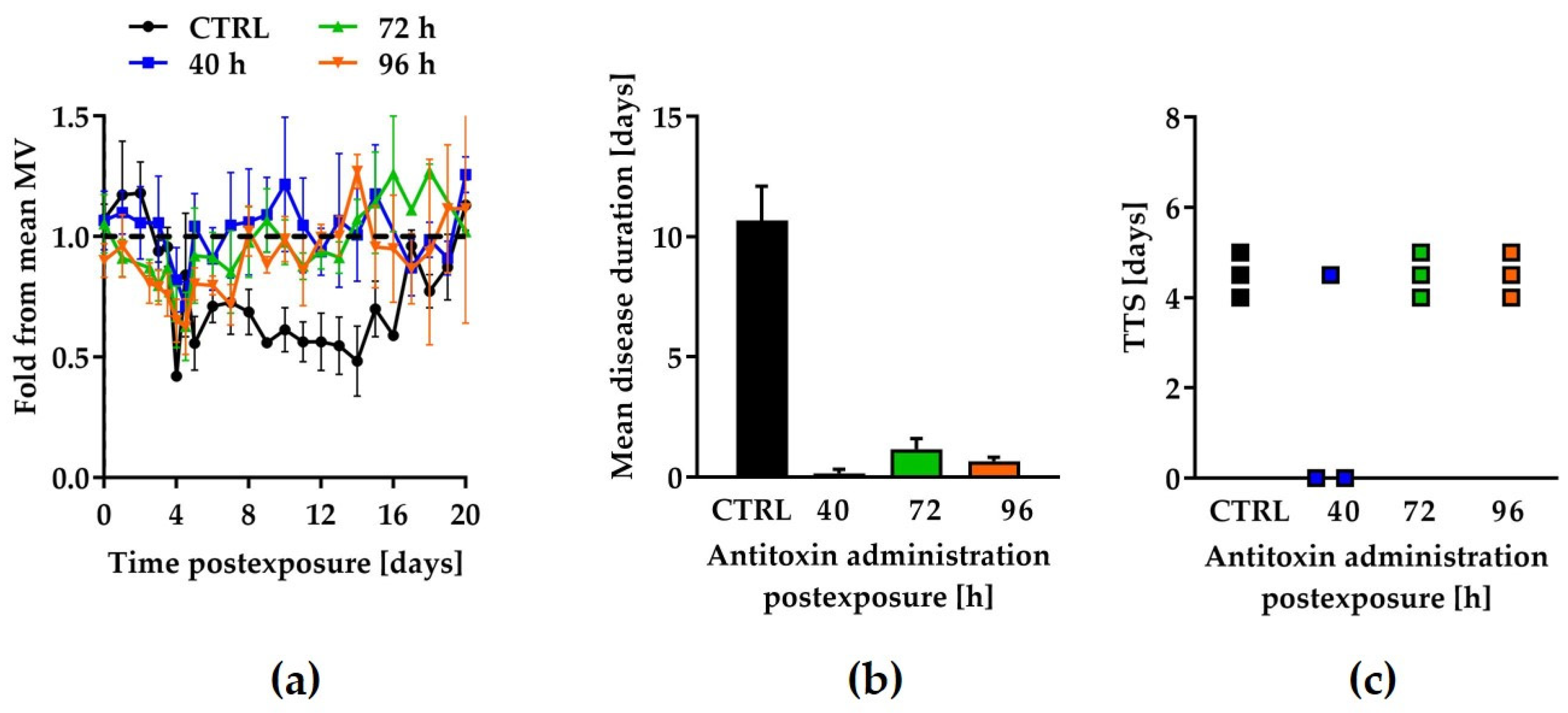
2.3. Qualification of the Model Using Botulinum Antitoxin
3. Discussion
4. Materials and Methods
4.1. Rabbits
4.2. Bacteria and Toxins
4.3. Antitoxin
4.4. Spirometry
4.5. Antitoxin Efficacy Studies
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arnon, S.S.; Schechter, R.; Inglesby, T.V.; Henderson, D.A.; Bartlett, J.G.; Ascher, M.S.; Eitzen, E.; Fine, A.D.; Hauer, J.; Layton, M.; et al. Botulinum toxin as a biological weapon: Medical and public health management. J. Am. Med. Assoc. 2001, 285, 1059–1070. [Google Scholar] [CrossRef]
- Gill, D.M. Bacterial toxins: A table of lethal amounts. Microbiol. Rev. 1982, 46, 86–94. [Google Scholar] [CrossRef]
- Atassi, M.Z.; Oshima, M. Structure, activity, and immune (T and B cell) recognition of botulinum neurotoxins. Crit. Rev. Immunol. 1999, 19, 219–260. [Google Scholar] [PubMed]
- Sugiyama, H. Clostridium botulinum neurotoxin. Microbiol. Rev. 1980, 44, 419–448. [Google Scholar] [CrossRef]
- Pirazzini, M.; Rossetto, O.; Eleopra, R.; Montecucco, C. Botulinum Neurotoxins: Biology, Pharmacology, and Toxicology. Pharmacol. Rev. 2017, 69, 200–235. [Google Scholar] [CrossRef] [PubMed]
- Lacy, D.B.; Tepp, W.; Cohen, A.C.; DasGupta, B.R.; Stevens, R.C. Crystal structure of botulinum neurotoxin type A and implications for toxicity. Nat. Struct. Biol. 1998, 5, 898–902. [Google Scholar] [CrossRef]
- Dembek, Z.F.; Smith, L.A.; Rusnak, J.M. Botulism: Cause, effects, diagnosis, clinical and laboratory identification, and treatment modalities. Disaster Med. Public Health Prep. 2007, 1, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Kongsaengdao, S.; Samintarapanya, K.; Rusmeechan, S.; Wongsa, A.; Pothirat, C.; Permpikul, C.; Pongpakdee, S.; Puavilai, W.; Kateruttanakul, P.; Phengtham, U.; et al. An outbreak of botulism in Thailand: Clinical manifestations and management of severe respiratory failure. Clin. Infect. Dis. 2006, 43, 1247–1256. [Google Scholar] [CrossRef] [PubMed]
- Weber, J.T.; Hibbs, R.G., Jr.; Darwish, A.; Mishu, B.; Corwin, A.L.; Rakha, M.; Hatheway, C.L.; El Sharkawy, S.; El-Rahim, S.A.; Al-Hamd, M.F.S.; et al. A massive outbreak of type E botulism associated with traditional salted fish in Cairo. J. Infect. Dis. 1993, 167, 451–454. [Google Scholar] [CrossRef] [PubMed]
- McCarty, C.L.; Angelo, K.; Beer, K.D.; Cibulskas-White, K.; Quinn, K.; de Fijter, S.; Bokanyi, R.; St Germain, E.; Baransi, K.; Barlow, K.; et al. Large Outbreak of Botulism Associated with a Church Potluck Meal-Ohio, 2015. MMWR Morb. Mortal. Wkly. Rep. 2015, 64, 802–803. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention Bioterrorism Agents/Diseases. Available online: https://emergency.cdc.gov/agent/agentlist-category.asp (accessed on 15 July 2021).
- Sobel, J. Botulism. Clin. Infect. Dis. 2005, 41, 1167–1173. [Google Scholar] [CrossRef]
- Iida, H.; Ono, T.; Karashimada, T.; Ando, Y. Studies on the serum therapy of type E botulism: Absorption of toxin from the gastrointestinal tract. Jpn. J. Med. Sci. Biol. 1970, 23, 282–285. [Google Scholar]
- Kodihalli, S.; Emanuel, A.; Takla, T.; Hua, Y.; Hobbs, C.; LeClaire, R.; O’Donnell, D.C. Therapeutic efficacy of equine botulism antitoxin in Rhesus macaques. PLoS ONE 2017, 12, e0186892. [Google Scholar] [CrossRef]
- Mottate, K.; Yokote, H.; Mori, S.; Horita, A.; Miyatsu, Y.; Torii, Y.; Kozaki, S.; Iwaki, M.; Takahashi, M.; Ginnaga, A. Retrospective survey to evaluate the safety and efficacy of Japanese botulinum antitoxin therapy in Japan. Toxicon 2016, 110, 12–18. [Google Scholar] [CrossRef]
- Schwartz, A.; Ben David, A.; Hotoveli, M.; Dor, E.; Diamant, E.; Vivyorka, A.; Rosen, O.; Torgeman, A.; Zichel, R. A Novel Running Wheel Mouse Model for Botulism and its use for the Evaluation of Post-Symptom Antitoxin Efficacy. Antimicrob. Agents Chemother. 2021, 65, e0042121. [Google Scholar] [CrossRef]
- Tacket, C.O.; Shandera, W.X.; Mann, J.M.; Hargrett, N.T.; Blake, P.A. Equine antitoxin use and other factors that predict outcome in type A foodborne botulism. Am. J. Med. 1984, 76, 794–798. [Google Scholar] [CrossRef]
- Sheth, A.N.; Wiersma, P.; Atrubin, D.; Dubey, V.; Zink, D.; Skinner, G.; Doerr, F.; Juliao, P.; Gonzalez, G.; Burnett, C.; et al. International outbreak of severe botulism with prolonged toxemia caused by commercial carrot juice. Clin. Infect. Dis. 2008, 47, 1245–1251. [Google Scholar] [CrossRef] [Green Version]
- Diamant, E.; Pass, A.; Rosen, O.; Ben David, A.; Torgeman, A.; Barnea, A.; Tal, A.; Rosner, A.; Zichel, R. A Novel Rabbit Spirometry Model of Type E Botulism and Its Use for the Evaluation of Postsymptom Antitoxin Efficacy. Antimicrob. Agents Chemother. 2018, 62, e02379-17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torgeman, A.; Schwartz, A.; Diamant, E.; Baruchi, T.; Dor, E.; Ben David, A.; Pass, A.; Barnea, A.; Tal, A.; Rosner, A.; et al. Studying the differential efficacy of postsymptom antitoxin treatment in type A versus type B botulism using a rabbit spirometry model. Dis. Model. Mech. 2018, 11, dmm035089. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vazquez-Cintron, E.; Machamer, J.; Ondeck, C.; Pagarigan, K.; Winner, B.; Bodner, P.; Kelly, K.; Pennington, M.R.; McNutt, P. Symptomatic treatment of botulism with a clinically approved small molecule. JCI Insight 2020, 5, e132891. [Google Scholar] [CrossRef] [PubMed]
- U.S. Food and Drug Administration. Product Development under the Animal Rule Guidance for Industry. Available online: https://www.fda.gov/media/88625/download (accessed on 15 July 2021).
- Hedenqvist, P.; Edner, A.; Fahlman, A.; Jensen-Waern, M. Continuous intravenous anaesthesia with sufentanil and midazolam in medetomidine premedicated New Zealand White rabbits. BMC Vet. Res. 2013, 9, 21. [Google Scholar] [CrossRef] [Green Version]
- Weber, K.; Mowat, V.; Hartmann, E.; Razinger, T.; Chevalier, H.J.; Blumbach, K.; Green, O.P.; Kaiser, S.; Corney, S.; Jackson, A.; et al. Pathology in Continuous Infusion Studies in Rodents and Non-Rodents and ITO (Infusion Technology Organisation)-Recommended Protocol for Tissue Sampling and Terminology for Procedure-Related Lesions. J. Toxicol. Pathol. 2011, 24, 113–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamaruzaman, N.A.; Kardia, E.; Kamaldin, N.; Latahir, A.Z.; Yahaya, B.H. The rabbit as a model for studying lung disease and stem cell therapy. BioMed Res. Int. 2013, 2013, 691830. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shiomi, M. Rabbit as a Model for the Study of Human Diseases. In Rabbit Biotechnology—Rabbit Genomics, Transgenesis, Cloning and Models; Houdebine, L.-M., Fan, J., Eds.; Springer: Dordrecht, The Netherlands, 2009; pp. 49–63. [Google Scholar]
- Jacobson, A.R.; Adler, M.; Silvaggi, N.R.; Allen, K.N.; Smith, G.M.; Fredenburg, R.A.; Stein, R.L.; Park, J.B.; Feng, X.; Shoemaker, C.B.; et al. Small molecule metalloprotease inhibitor with in vitro, ex vivo and in vivo efficacy against botulinum neurotoxin serotype A. Toxicon 2017, 137, 36–47. [Google Scholar] [CrossRef] [PubMed]
- McNutt, P.M.; Vazquez-Cintron, E.J.; Tenezaca, L.; Ondeck, C.A.; Kelly, K.E.; Mangkhalakhili, M.; Machamer, J.B.; Angeles, C.A.; Glotfelty, E.J.; Cika, J.; et al. Neuronal delivery of antibodies has therapeutic effects in animal models of botulism. Sci. Transl. Med. 2021, 13, eabd7789. [Google Scholar] [CrossRef]
- Miyashita, S.I.; Zhang, J.; Zhang, S.; Shoemaker, C.B.; Dong, M. Delivery of single-domain antibodies into neurons using a chimeric toxin-based platform is therapeutic in mouse models of botulism. Sci. Transl. Med. 2021, 13, eaaz4197. [Google Scholar] [CrossRef]
- Pang, Y.P.; Davis, J.; Wang, S.; Park, J.G.; Nambiar, M.P.; Schmidt, J.J.; Millard, C.B. Small molecules showing significant protection of mice against botulinum neurotoxin serotype A. PLoS ONE 2010, 5, e10129. [Google Scholar] [CrossRef] [Green Version]
- Burnett, J.C.; Opsenica, D.; Sriraghavan, K.; Panchal, R.G.; Ruthel, G.; Hermone, A.R.; Nguyen, T.L.; Kenny, T.A.; Lane, D.J.; McGrath, C.F.; et al. A Refined Pharmacophore Identifies Potent 4-Amino-7-chloroquinoline-Based Inhibitors of the Botulinum Neurotoxin Serotype A Metalloprotease. J. Med. Chem. 2007, 50, 2127–2136. [Google Scholar] [CrossRef] [Green Version]
- Eichhorn, T.; Dolimbek, B.Z.; Deeg, K.; Efferth, T.; Atassi, M.Z. Inhibition in vivo of the activity of botulinum neurotoxin A by small molecules selected by virtual screening. Toxicon 2012, 60, 1180–1190. [Google Scholar] [CrossRef]
- Eubanks, L.M.; Hixon, M.S.; Jin, W.; Hong, S.; Clancy, C.M.; Tepp, W.H.; Baldwin, M.R.; Malizio, C.J.; Goodnough, M.C.; Barbieri, J.T.; et al. An in vitro and in vivo disconnect uncovered through high-throughput identification of botulinum neurotoxin A antagonists. Proc. Natl. Acad. Sci. USA 2007, 104, 2602. [Google Scholar] [CrossRef] [Green Version]
- Singh, P.; Singh, M.K.; Chaudhary, D.; Chauhan, V.; Bharadwaj, P.; Pandey, A.; Upadhyay, N.; Dhaked, R.K. Small-molecule quinolinol inhibitor identified provides protection against BoNT/A in mice. PLoS ONE 2012, 7, e47110. [Google Scholar] [CrossRef] [Green Version]
- Diamant, E.; Torgeman, A.; Ozeri, E.; Zichel, R. Monoclonal Antibody Combinations that Present Synergistic Neutralizing Activity: A Platform for Next-Generation Anti-Toxin Drugs. Toxins 2015, 7, 1854–1881. [Google Scholar] [CrossRef]
- Li, B.; Peet, N.P.; Butler, M.M.; Burnett, J.C.; Moir, D.T.; Bowlin, T.L. Small molecule inhibitors as countermeasures for botulinum neurotoxin intoxication. Molecules 2010, 16, 202–220. [Google Scholar] [CrossRef] [Green Version]
- Mazuet, C.; Dano, J.; Popoff, M.R.; Creminon, C.; Volland, H. Characterization of botulinum neurotoxin type A neutralizing monoclonal antibodies and influence of their half-lives on therapeutic activity. PLoS ONE 2010, 5, e12416. [Google Scholar] [CrossRef] [Green Version]
- Nowakowski, A.; Wang, C.; Powers, D.B.; Amersdorfer, P.; Smith, T.J.; Montgomery, V.A.; Sheridan, R.; Blake, R.; Smith, L.A.; Marks, J.D. Potent neutralization of botulinum neurotoxin by recombinant oligoclonal antibody. Proc. Natl. Acad. Sci. USA 2002, 99, 11346–11350. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duplantier, A.; Kane, C.; Bavari, S. Searching for Therapeutics against Botulinum Neurotoxins: A True Challenge for Drug Discovery. Curr. Top. Med. Chem. 2016, 16, 2330–2349. [Google Scholar] [CrossRef] [PubMed]
- Dor, E.; David, T.; Dekel Jaoui, H.; Schwartz, A.; Baruchi, T.; Torgeman, A.; Ben David, A.; Rosen, O.; Tal, A.; Rosner, A.; et al. A Rabbit Model for Prolonged Continuous Intravenous Infusion via a Peripherally Inserted Central Catheter. Front. Pharmacol. 2021, 12, 637792. [Google Scholar] [CrossRef] [PubMed]
- Binz, T.; Kurazono, H.; Wille, M.; Frevert, J.; Wernars, K.; Niemann, H. The complete sequence of botulinum neurotoxin type A and comparison with other clostridial neurotoxins. J. Biol. Chem. 1990, 265, 9153–9158. [Google Scholar] [CrossRef]
- GenBank: M30196.1. C.botulinum Neurotoxin Gene, Complete Cds. Available online: https://www.ncbi.nlm.nih.gov/nuccore/M30196 (accessed on 19 September 2021).
- Diamant, E.; Lachmi, B.E.; Keren, A.; Barnea, A.; Marcus, H.; Cohen, S.; David, A.B.; Zichel, R. Evaluating the synergistic neutralizing effect of anti-botulinum oligoclonal antibody preparations. PLoS ONE 2014, 9, e87089. [Google Scholar] [CrossRef] [Green Version]
- Torgeman, A.; Mador, N.; Dorozko, M.; Lifshitz, A.; Eschar, N.; White, M.D.; Wolf, D.G.; Epstein, E. Efficacy of inactivation of viral contaminants in hyperimmune horse plasma against botulinum toxin by low pH alone and combined with pepsin digestion. Biologicals 2017, 48, 24–27. [Google Scholar] [CrossRef]
- European Directorate for the Quality of Medicines and Healthcare. European Pharmacopoeia (Botulinum antitoxin), 10th ed.; European Directorate for the Quality of Medicines and Healthcare: Strasbourg, France, 2019. [Google Scholar]

| BoNT/A Dose (RbIMLD50) 1 | % Symptomatic Rabbits (n) |
|---|---|
| 0.5 | 50 (2) |
| 0.65 | 75 (4) |
| 0.75 | 80 (5) |
| 0.85 | 100 (13) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torgeman, A.; Diamant, E.; Dor, E.; Schwartz, A.; Baruchi, T.; Ben David, A.; Zichel, R. A Rabbit Model for the Evaluation of Drugs for Treating the Chronic Phase of Botulism. Toxins 2021, 13, 679. https://doi.org/10.3390/toxins13100679
Torgeman A, Diamant E, Dor E, Schwartz A, Baruchi T, Ben David A, Zichel R. A Rabbit Model for the Evaluation of Drugs for Treating the Chronic Phase of Botulism. Toxins. 2021; 13(10):679. https://doi.org/10.3390/toxins13100679
Chicago/Turabian StyleTorgeman, Amram, Eran Diamant, Eyal Dor, Arieh Schwartz, Tzadok Baruchi, Alon Ben David, and Ran Zichel. 2021. "A Rabbit Model for the Evaluation of Drugs for Treating the Chronic Phase of Botulism" Toxins 13, no. 10: 679. https://doi.org/10.3390/toxins13100679
APA StyleTorgeman, A., Diamant, E., Dor, E., Schwartz, A., Baruchi, T., Ben David, A., & Zichel, R. (2021). A Rabbit Model for the Evaluation of Drugs for Treating the Chronic Phase of Botulism. Toxins, 13(10), 679. https://doi.org/10.3390/toxins13100679





