Calcium Intake in Elderly Australian Women Is Inadequate
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Dietary intake assessment
2.3. Anthropometry
2.4. Statistical analysis
3. Results and Discussion
3.1. Dietary energy and macronutrient intakes
| Current study | 1995 NNS | |
|---|---|---|
| (Mean ± SD) | (Mean) | |
| Age (years) | 74.2 ± 2.7 | 65 and over |
| Weight (kg) | 68.5 ± 11.3 | 66.1 |
| Height (cm) | 159.9 ± 6.0 | 156.7 |
| BMI (kg/m2) | 26.8 ± 3.9 | 26.9 |
| Current study | 1995 NNS | EAR/AMDR | |
|---|---|---|---|
| age 74.2 ± 2.7 years | for age ≥65 years | for age >70 years | |
| (Mean ± SD) | (Mean) | (Mean) | |
| Energy (kJ) | 7084 ± 1462 | 6367 | 8573 EER 1 |
| Protein (g) | 75 ± 17 | 64 | 46 |
| Protein (g/kg body weight) | 1.13 ± 0.31 | NA | 0.75 |
| Fat (g) | 62 ± 19 | 57 | NA |
| Carbohydrate (g) | 187 ± 44 | 182 | NA |
| Alcohol (g) | 7 ± 10 | 5 | NA |
| Energy contribution of macronutrients | |||
| % energy from protein | 19 ± 3 | 18 | 15–25 |
| % energy from fat | 33 ± 6 | 32 | 20–35 |
| % energy from carbohydrate | 46 ± 7 | 48 | 45–65 |
| % energy from alcohol | 3 ± 4 | 2 | NA |
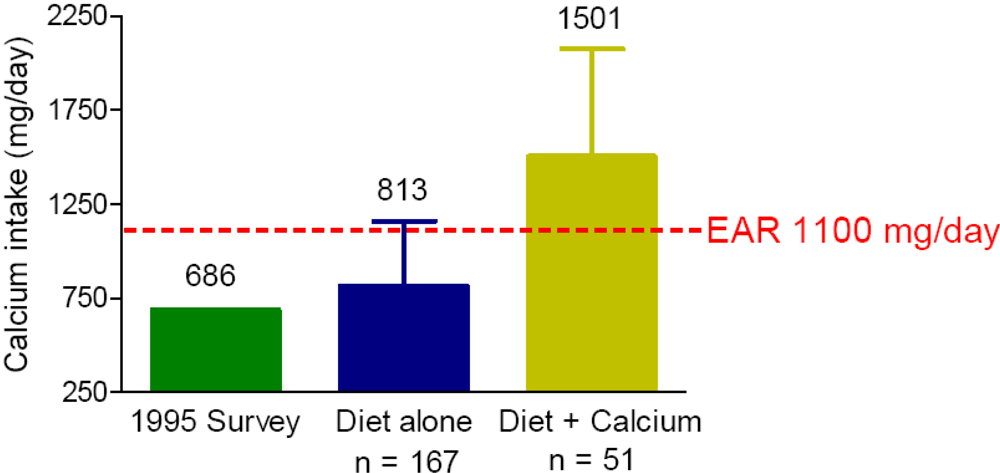
3.2. Calcium intake
| Current study | 1995 NNS | EAR | |
|---|---|---|---|
| age 74.2 ± 2.7 years | age ≥65 years | for age >70 years | |
| (Mean ± SD) | (Mean) | (Mean) | |
| Calcium (mg) | 852 ± 298 | 686 | 1100 |
| Phosphorus (mg) | 1343 ± 323 | 1132 | 580 |
| Magnesium (mg) | 299 ± 74 | 268 | 265 |
| Iron (mg) | 11 ± 3 | 11 | 5 |
| Zinc (mg) | 10 ± 2 | 9 | 6.5 |
| Potassium (mg) | 2973 ± 649 | 2626 | 2800 (AI) |
| Supplements | Number of subjects using supplements (%) |
|---|---|
| Calcium | 51 (23) |
| Vitamin D | 6 (3) |
| Fish oil | 55 (25) |
| Other vitamins or minerals | 43 (20) |
4. Conclusions
Acknowledgements
Declare
References
- Chapuy, M.C.; Arlot, M.E.; Duboeuf, F.; Brun, J.; Crouzet, B.; Arnaud, S.; Delmas, P.D.; Meunier, P.J. Vitamin D3 and calcium to prevent hip fractures in the elderly women. N. Engl. J. Med. 1992, 327, 1637–1642. [Google Scholar]
- Prince, R.L.; Devine, A.; Dhaliwal, S.S.; Dick, I.M. Effects of calcium supplementation on clinical fracture and bone structure: results of a 5-year, double-blind, placebo-controlled trial in elderly women. Arch. Intern. Med. 2006, 166, 869–875. [Google Scholar] [CrossRef] [PubMed]
- Rizzoli, R.; Bruyere, O.; Cannata-Andia, J.B.; Devogelaer, J.P.; Lyritis, G.; Ringe, J.D.; Vellas, B.; Reginster, J.Y. Management of osteoporosis in the elderly. Curr. Med. Res. Opin. 2009, 25, 2373–2387. [Google Scholar]
- Gold, D.T. Elevated calcium requirements for women and unique approaches to improving calcium adherence. J. Reprod. Med. 2005, 50, 891–895. [Google Scholar]
- Rossini, M.; Bianchi, G.; Di Munno, O.; Giannini, S.; Minisola, S.; Sinigaglia, L.; Adami, S. Determinants of adherence to osteoporosis treatment in clinical practice. Osteoporos. Int. 2006, 17, 914–921. [Google Scholar]
- McLennan, W.; Podger, A. National Nutrition Survey: Nutrient Intakes and Physical Measurements; Australian Bureau of Statistics, Commonwealth of Australia: Canberra, Australia, 1998.
- National Health and Medical Research Council, Nutrient Reference Values for Australia and New Zealand: Evidence Appendix; Commonwealth of Australia: Canberra, Australia, 2006.
- Marfell-Jones, M.; Olds, T.; Stewart, A.; Carter, L. International Standards for Anthropometric Assessment (2006); ISAK: Potchefstroom, South Africa, 2006. [Google Scholar]
- Dairy Australia: Consumption Summary. Available online: http://www.dairyaustralia.com.au/Our-Dairy-Industry/Industry-Statistics/Consumption-Summary.aspx (accessed on 10 August 2010).
- Dairy Australia: Drinking Milk Sales. Available online: http://www.dairyaustralia.com.au/Our-Dairy-Industry/Industry-Statistics/Milk/Drinking-Milk-Sales.aspx (accessed on 10 August 2010).
- Meng, X.; Zhu, K.; Devine, A.; Kerr, D.A.; Binns, C.W.; Prince, R.L. A 5-year cohort study of the effects of high protein intake on lean mass and bone mineral content in elderly postmenopausal women. J. Bone Miner. Res. 2009, 24, 1827–1834. [Google Scholar]
- Andersen, L.F.; Lande, B.; Arsky, G.H.; Trygg, K. Validation of a semi-quantitative food-frequency questionnaire used among 12-month-old Norwegian infants. Eur. J. Clin. Nutr. 2003, 57, 881–888. [Google Scholar]
- Brownie, S. Predictors of dietary and health supplement use in older Australians. Aust. J. Adv. Nurs. 2006, 23, 26–32. [Google Scholar]
© 2010 by the authors; licensee MDPI, Basel, Switzerland This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Meng, X.; Kerr, D.A.; Zhu, K.; Devine, A.; Solah, V.; Binns, C.W.; Prince, R.L. Calcium Intake in Elderly Australian Women Is Inadequate. Nutrients 2010, 2, 1036-1043. https://doi.org/10.3390/nu2091036
Meng X, Kerr DA, Zhu K, Devine A, Solah V, Binns CW, Prince RL. Calcium Intake in Elderly Australian Women Is Inadequate. Nutrients. 2010; 2(9):1036-1043. https://doi.org/10.3390/nu2091036
Chicago/Turabian StyleMeng, Xingqiong, Deborah A. Kerr, Kun Zhu, Amanda Devine, Vicky Solah, Colin W. Binns, and Richard L. Prince. 2010. "Calcium Intake in Elderly Australian Women Is Inadequate" Nutrients 2, no. 9: 1036-1043. https://doi.org/10.3390/nu2091036
APA StyleMeng, X., Kerr, D. A., Zhu, K., Devine, A., Solah, V., Binns, C. W., & Prince, R. L. (2010). Calcium Intake in Elderly Australian Women Is Inadequate. Nutrients, 2(9), 1036-1043. https://doi.org/10.3390/nu2091036






