Relationship between Fear of COVID-19, Intolerance of Uncertainty, and Coping Strategies on University Students’ Mental Health
Abstract
:1. Introduction
Objective and Hypotheses
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.3. Compliance with Ethical Standards
2.4. Statistical Analysis
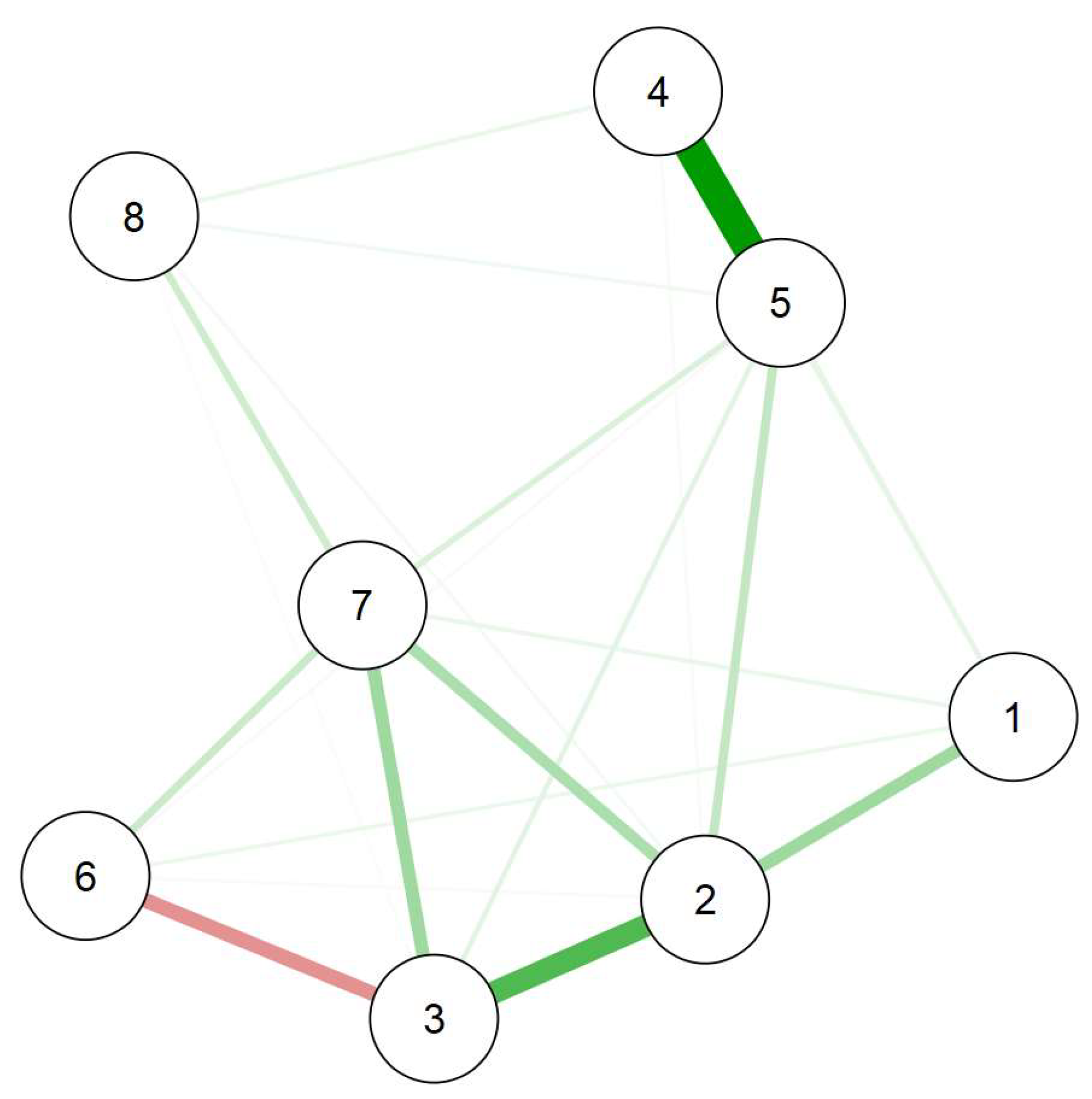
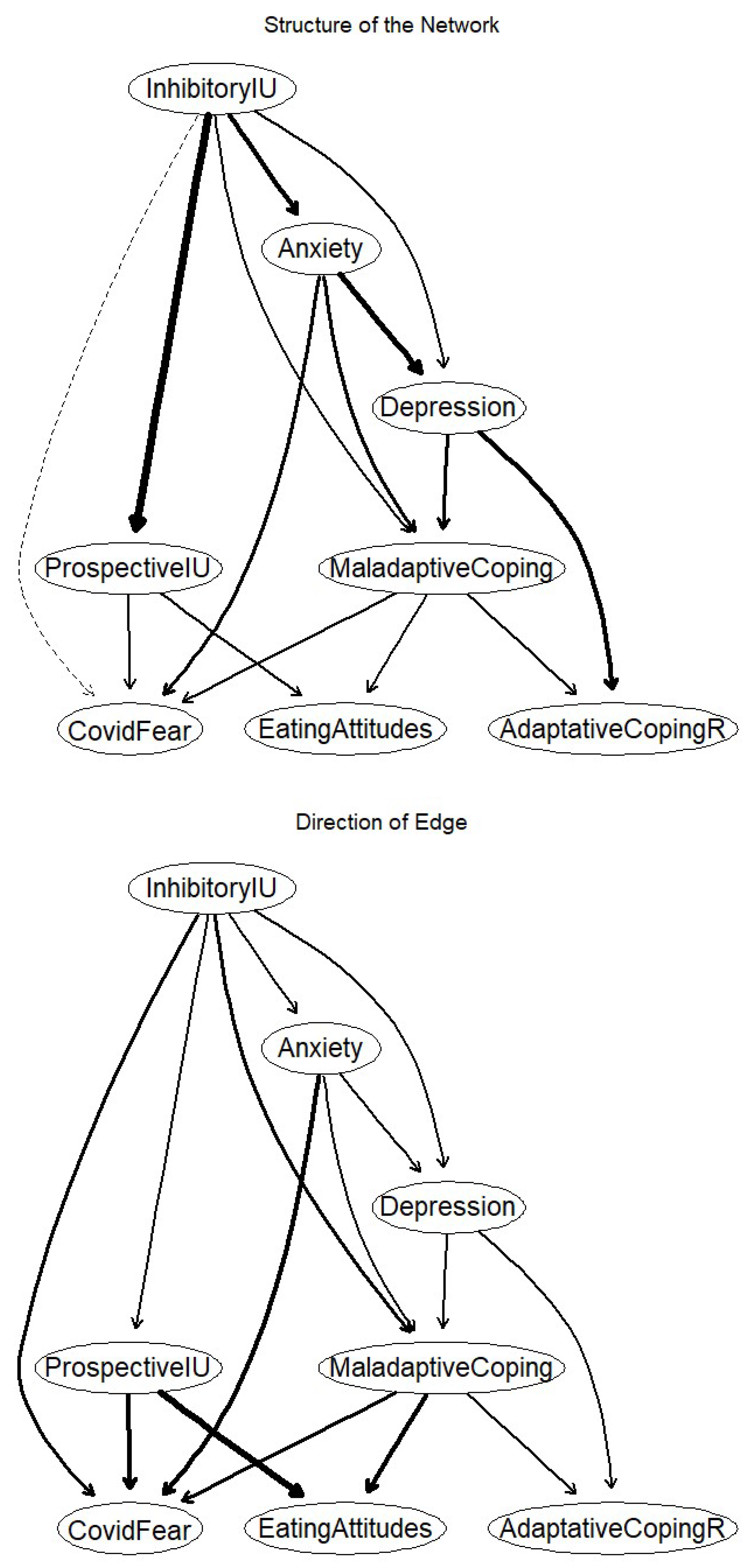
3. Results
4. Discussion
Limitations and Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Women (n = 1612) | Men (n = 506) | Nonbinary (n = 21) | ANOVA | ||||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | F | p | η2 | |
| Fear of COVID | 14.89 | 5.93 | 12.60 | 5.21 | 15.10 | 6.90 | 30.37 | <0.001 | 0.03 |
| Anxiety | 10.45 | 4.56 | 8.25 | 4.55 | 13.33 | 4.48 | 50.75 | <0.001 | 0.05 |
| Depression | 7.73 | 4.26 | 7.13 | 4.34 | 8.52 | 4.70 | 4.22 | 0.02 | 0.004 |
| Eating-related problems | 17.48 | 13.31 | 14.34 | 13.34 | 15.71 | 8.92 | 10.82 | <0.001 | 0.01 |
| Intolerance of uncertainty | 36.08 | 11.20 | 32.39 | 10.14 | 38.86 | 12.07 | 22.91 | <0.001 | 0.02 |
| Prospective IU | 21.95 | 6.84 | 20.28 | 6.29 | 22.24 | 6.20 | 12.07 | <0.001 | 0.01 |
| Inhibitory IU | 14.13 | 5.19 | 12.11 | 4.79 | 16.62 | 5.90 | 33.46 | <0.001 | 0.03 |
| Adaptive coping | 2.23 | 0.87 | 2.16 | 0.81 | 1.92 | 0.98 | 2.38 | 0.09 | 0.002 |
| Maladaptive coping | 2.04 | 0.94 | 1.77 | 0.92 | 2.32 | 0.98 | 17.98 | <0.001 | 0.02 |
References
- Vindegaard, N.; Eriksen Benros, M. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain. Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Charbonnier, E.; Goncalves, A.; Puechlong, C.; Montalescot, L.; Le Vigouroux, S. Two years and four time points: Description of emotional state and coping strategies of French university dtudents during the COVID-19 pandemic. Viruses 2022, 14, 782. [Google Scholar] [CrossRef] [PubMed]
- Dozois, D.J.A. Anxiety and depression in Canada during the COVID-19 pandemic: A national survey. Can. Psychol. 2021, 62, 136–142. [Google Scholar] [CrossRef]
- Le Vigouroux, S.; Goncalves, A.; Charbonnier, E. The psychological vulnerability of French university students to the COVID-19 confinement. Health Educ. Behav. 2021, 48, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Haddad, C.; Zakhour, M.; Bou Kheir, M.; Haddad, R.; Al Hachach, M.; Sacre, H.; Salameh, P. Association between eating behavior and quarantine/confinement stressors during the coronavirus disease 2019 outbreak. J. Eat. Disord. 2020, 8, 40. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Rackoff, G.N.; Fitzsimmons-Craft, E.E.; Shin, K.E.; Zainal, N.H.; Schwob, J.T.; Eisenberg, D.; Wilfley, D.E.; Taylor, C.B.; Newman, M.G. College mental health before and during the COVID-19 pandemic: Results from a nationwide survey. Cognit. Ther. Res. 2022, 46, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Bourion-Bédès, S.; Tarquinio, C.; Batt, M.; Tarquinio, P.; Lebreuilly, R.; Sorsana, C.; Legrand, K.; Rousseau, H.; Baumann, C. Psychological impact of the COVID-19 outbreak on students in a French region severely affected by the disease: Results of the PIMS-CoV 19 study. Psychiatry Res. 2021, 295, 113559. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Chen, T.; Lucock, M. The mental health of university students during the COVID-19 pandemic: An online survey in the UK. PLoS ONE 2022, 17, e0262562. [Google Scholar] [CrossRef]
- Kaparounaki, C.K.; Patsali, M.E.; Mousa, D.-P.V.; Papadopoulou, E.V.K.; Papadopoulou, K.K.K.; Fountoulakis, K.N. University students’ mental health amidst the COVID-19 quarantine in Greece. Psychiatry Res. 2020, 290, 113111. [Google Scholar] [CrossRef]
- Kim, H.; Jung, J. Social isolation and psychological distress during the COVID-19 pandemic: A cross-national analysis. Gerontologist 2021, 61, 103–113. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, H.; Ma, X.; Di, Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: A longitudinal study of college students in China. Int. J. Environ. Res. Public Health 2020, 17, 3722. [Google Scholar] [CrossRef]
- Charbonnier, E.; Le Vigouroux, S.; Goncalves, A. Psychological vulnerability of French university students during the COVID-19 pandemic: A four-wave longitudinal survey. Int. J. Environ. Res. Public Health 2021, 18, 9699. [Google Scholar] [CrossRef]
- Duffy, M.E.; Twenge, J.M.; Joiner, T.E. Trends in mood and anxiety symptoms and suicide-related outcomes among U.S. undergraduates, 2007–2018: Evidence from two national surveys. J. Adolesc. Health 2019, 65, 590–598. [Google Scholar] [CrossRef]
- Eisenberg, D.; Nicklett, E.J.; Roeder, K.; Kirz, N.E. Eating disorder symptoms among college students: Prevalence, persistence, correlates, and treatment-seeking. J. Am. Coll. Health 2011, 59, 700–707. [Google Scholar] [CrossRef]
- Regehr, C.; Glancy, D.; Pitts, A. Interventions to reduce stress in university students: A review and meta-analysis. J. Affect. Disord. 2013, 148, 1–11. [Google Scholar] [CrossRef]
- Bonanno, G.A.; Ho, S.M.Y.; Chan, J.C.K.; Kwong, R.S.Y.; Cheung, C.K.Y.; Wong, C.P.Y.; Wong, V.C.W. Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: A latent class approach. Health Psychol. 2008, 27, 659–667. [Google Scholar] [CrossRef]
- Lee, A.M.; Wong, J.G.; McAlonan, G.M.; Cheung, V.; Cheung, C.; Sham, P.C.; Chu, C.-M.; Wong, P.-C.; Tsang, K.W.T.; Chua, S.E. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can. J. Psychiatry 2007, 52, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Kakade, M.; Fuller, C.J.; Fan, B.; Fang, Y.; Kong, J.; Guan, Z.; Wu, P. Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Compr. Psychiatry 2012, 53, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Erbiçer, E.S.; Metin, A.; Çetinkaya, A.; Sen, S. The relationship between fear of COVID-19 and depression, anxiety, and stress: A meta-analysis. Eur. Psychol. 2021, 26, 323–333. [Google Scholar] [CrossRef]
- Matsumoto, D.; Frank, M.; Hwang, H. Nonverbal Communication: Science and Applications; SAGE Publications: Thousand Oaks, CA, USA, 2012. [Google Scholar]
- Harper, C.A.; Satchell, L.P.; Fido, D.; Latzman, R.D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Ment. Health Addict. 2021, 19, 1875–1888. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.; Ng, K.C.; Oh, J.Y.; Baeg, A.; Rajasegaran, K.; Chew, C.S.E. Caring for children and adolescents with eating disorders in the current coronavirus 19 pandemic: A Singapore perspective. J. Adolesc. Health 2020, 67, 131–134. [Google Scholar] [CrossRef] [PubMed]
- Bakioğlu, F.; Korkmaz, O.; Ercan, H. Fear of COVID-19 and positivity: Mediating role of intolerance of uncertainty, depression, anxiety, and stress. Int. J. Ment. Health Addict. 2021, 19, 2369–2382. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, K.M.; Drawve, G.; Harris, C. Facing new fears during the COVID-19 pandemic: The State of America’s mental health. J. Anxiety Disord. 2020, 75, 102291. [Google Scholar] [CrossRef]
- Rahman, M.A.; Hoque, N.; Alif, S.M.; Salehin, M.; Islam, S.M.S.; Banik, B.; Sharif, A.; Nazim, N.B.; Sultana, F.; Cross, W. Factors associated with psychological distress, fear and coping strategies during the COVID-19 pandemic in Australia. Global. Health 2020, 16, 95. [Google Scholar] [CrossRef] [PubMed]
- Baticulon, R.E.; Sy, J.J.; Alberto, N.R.I.; Baron, M.B.C.; Mabulay, R.E.C.; Rizada, L.G.T.; Tiu, C.J.S.; Clarion, C.A.; Reyes, J.C.B. Barriers to online learning in the time of COVID-19: A national survey of medical students in the Philippines. Med. Sci. Educ. 2021, 31, 615–626. [Google Scholar] [CrossRef]
- International Association of Universities. COVID-19: Higher Education Challenges and Responses. Available online: https://www.iau-aiu.net/COVID-19-Higher-Education-challenges-and-responses (accessed on 15 September 2020).
- Lazarus, R.S.; Folkman, S. Coping and adaptation. In The Handbook of Behavioral Medicine; Gentry, W.D., Ed.; Guilford: New York, NY, USA, 1984; pp. 282–325. [Google Scholar]
- Killgore, W.D.S.; Cloonan, S.A.; Taylor, E.C.; Dailey, N.S. Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Res. 2020, 290, 113117. [Google Scholar] [CrossRef]
- Garnefski, N.; Legerstee, J.; Kraaij, V.; Van Den Kommer, T.; Teerds, J. Cognitive coping strategies and symptoms of depression and anxiety: A comparison between adolescents and adults. J. Adolesc. 2002, 25, 603–611. [Google Scholar] [CrossRef]
- Whatley, S.L.; Foreman, A.C.; Richards, S. The relationship of coping style to dysphoria, anxiety, and anger. Psychol. Rep. 1998, 83, 783–791. [Google Scholar] [CrossRef]
- Mosley, T.H.; Perrin, S.G.; Neral, S.M.; Dubbert, P.M.; Grothues, C.A.; Pinto, B.M. Stress, coping, and well-being among third-year medical students. Acad. Med. 1994, 69, 765–767. [Google Scholar] [CrossRef]
- Muller, L.; Spitz, E. Évaluation multidimensionnelle du coping: Validation du Brief COPE sur une population française. Encephale 2003, 29, 507–518. [Google Scholar] [PubMed]
- Adler, A.D.; Conklin, L.R.; Strunk, D.R. Quality of coping skills predicts depressive symptom reactivity over repeated stressors. J. Clin. Psychol. 2013, 69, 1228. [Google Scholar] [CrossRef] [PubMed]
- Baenas, I.; Caravaca-Sanz, E.; Granero, R.; Sánchez, I.; Riesco, N.; Testa, G.; Vintró-Alcaraz, C.; Treasure, J.; Jiménez-Murcia, S.; Fernández-Aranda, F. COVID-19 and eating disorders during confinement: Analysis of factors associated with resilience and aggravation of symptoms. Eur. Eat. Disord. Rev. 2020, 28, 855–863. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Venanzi, L.; Dickey, L.; Green, H.; Pegg, S.; Benningfield, M.M.; Bettis, A.H.; Blackford, J.U.; Kujawa, A. Longitudinal predictors of depression, anxiety, and alcohol use following COVID-19-related stress. Stress Health 2022, 38, 679–691. [Google Scholar] [CrossRef]
- Voitsidis, P.; Nikopoulou, V.A.; Holeva, V.; Parlapani, E.; Sereslis, K.; Tsipropoulou, V.; Karamouzi, P.; Giazkoulidou, A.; Tsopaneli, N.; Diakogiannis, I. The mediating role of fear of COVID-19 in the relationship between intolerance of uncertainty and depression. Psychol. Psychother. Theory Res. Pract. 2021, 94, 884–893. [Google Scholar] [CrossRef]
- Elsharkawy, N.B.; Abdelaziz, E.M. Levels of fear and uncertainty regarding the spread of coronavirus disease (COVID-19) among university students. Perspect. Psychiatr. Care 2021, 57, 1356–1364. [Google Scholar] [CrossRef]
- Dugas, M.J.; Gosselin, P.; Ladouceur, R. Intolerance of uncertainty and worry: Investigating specificity in a nonclinical sample. Cogn. Ther. Res. 2001, 25, 551–558. [Google Scholar] [CrossRef]
- Buhr, K.; Dugas, M.J. The Intolerance of Uncertainty Scale: Psychometric properties of the English version. Behav. Res. Ther. 2002, 40, 931–945. [Google Scholar] [CrossRef]
- Dugas, M.J.; Hedayati, M.; Karavidas, A.; Buhr, K.; Francis, K.; Phillips, N.A. Intolerance of uncertainty and information processing: Evidence of biased recall and interpretations. Cogn. Ther. Res. 2005, 29, 57–70. [Google Scholar] [CrossRef]
- Dugas, M.J.; Buhr, K.; Ladouceur, R. The role of intolerance of uncertainty in etiology and maintenance. In Generalized Anxiety Disorder: Advances in Research and Practice; Heimberg, R.G., Turk, C.L., Mennin, D.S., Eds.; The Guilford Press: New York, NY, USA, 2004; pp. 143–163. [Google Scholar]
- Reilly, E.E.; Perry, T.R.; Brown, T.A.; Wierenga, C.E.; Kaye, W.H. Intolerance of uncertainty and eating disorder symptoms over the course of intensive treatment. Behav. Ther. 2021, 52, 698–708. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Y.; Hong, R.Y. Intolerance of uncertainty moderates the relation between negative life events and anxiety. Pers. Individ. Differ. 2010, 49, 49–53. [Google Scholar] [CrossRef]
- Taha, S.; Matheson, K.; Cronin, T.; Anisman, H. Intolerance of uncertainty, appraisals, coping, and anxiety: The case of the 2009 H1N1 pandemic. Br. J. Health Psychol. 2014, 19, 592–605. [Google Scholar] [CrossRef] [PubMed]
- Birrell, J.; Meares, K.; Wilkinson, A.; Freeston, M. Toward a definition of intolerance of uncertainty: A review of factor analytical studies of the Intolerance of Uncertainty Scale. Clin. Psychol. Rev. 2011, 31, 1198–1208. [Google Scholar] [CrossRef] [PubMed]
- Pawluk, E.J.; Koerner, N. A preliminary investigation of impulsivity in generalized anxiety disorder. Pers. Individ. Differ. 2013, 54, 732–737. [Google Scholar] [CrossRef]
- Stapinski, L.A.; Abbott, M.J.; Rapee, R.M. Evaluating the cognitive avoidance model of generalised anxiety disorder: Impact of worry on threat appraisal, perceived control and anxious arousal. Behav. Res. Ther. 2010, 48, 1032–1040. [Google Scholar] [CrossRef] [PubMed]
- Luhmann, C.C.; Ishida, K.; Hajcak, G. Intolerance of uncertainty and decisions about delayed, probabilistic rewards. Behav. Ther. 2011, 42, 378–386. [Google Scholar] [CrossRef]
- Berenbaum, H.; Bredemeier, K.; Thompson, R.J. Intolerance of uncertainty: Exploring its dimensionality and associations with need for cognitive closure, psychopathology, and personality. J. Anxiety Disord. 2008, 22, 117–125. [Google Scholar] [CrossRef]
- Fetzner, M.G.; Horswill, S.C.; Boelen, P.A.; Carleton, R.N. Intolerance of uncertainty and PTSD symptoms: Exploring the construct relationship in a community sample with a heterogeneous trauma history. Cognit. Ther. Res. 2013, 37, 725–734. [Google Scholar] [CrossRef]
- Helsen, K.; Van Den Bussche, E.; Vlaeyen, J.W.S.; Goubert, L. Confirmatory factor analysis of the Dutch Intolerance of Uncertainty Scale: Comparison of the full and short version. J. Behav. Ther. Exp. Psychiatry 2013, 44, 21–29. [Google Scholar] [CrossRef]
- Sexton, K.A.; Dugas, M.J. Defining distinct negative beliefs about uncertainty: Validating the factor structure of the Intolerance of Uncertainty Scale. Psychol. Assess. 2009, 21, 176–186. [Google Scholar] [CrossRef] [PubMed]
- Hong, R.Y.; Lee, S.S.M. Further clarifying prospective and inhibitory intolerance of uncertainty: Factorial and construct validity of test scores from the Intolerance of Uncertainty Scale. Psychol. Assess. 2015, 27, 605–620. [Google Scholar] [CrossRef] [PubMed]
- Champely, S.; Ekstrom, C.; Dalgaard, P.; Gill, J.; Weibelzahl, S.; Anandkumar, A.; Ford, C.; Volcic, R.; Rosario, H. De Pwr: Basic Functions for Power Analysis 2017. Available online: http://CRAN.R-project.org/package=pwr (accessed on 1 September 2022).
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and initial validation. Int. J. Ment. Health Addict. 2022, 20, 1537–1545. [Google Scholar] [CrossRef] [PubMed]
- Carleton, R.N.; Norton, M.A.P.J.; Asmundson, G.J.G. Fearing the unknown: A short version of the Intolerance of Uncertainty Scale. J. Anxiety Disord. 2007, 21, 105–117. [Google Scholar] [CrossRef] [PubMed]
- Lepine, J.P.; Godchau, M.; Brun, P. Anxiety and depression in inpatients. Lancet 1985, 326, 1425–1426. [Google Scholar] [CrossRef] [PubMed]
- Leichner, P.; Steiger, H.; Puentes-Neuman, G.; Perreault, M.; Gottheil, N. Validation d’une échelle d’attitudes alimentaires auprès d’une population québécoise francophone. Can. J. Psychiatry 1994, 39, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Scutari, M. Learning Bayesian Networks with the bnlearn R Package. J. Stat. Softw. 2010, 35, 1–22. [Google Scholar] [CrossRef]
- Scutari, M.; Nagarajan, R. Identifying significant edges in graphical models of molecular networks. Artif. Intell. Med. 2013, 57, 207–217. [Google Scholar] [CrossRef]
- McNally, R.J. Can network analysis transform psychopathology? Behav. Res. Ther. 2016, 86, 95–104. [Google Scholar] [CrossRef]
- McEvoy, P.M.; Hyett, M.P.; Shihata, S.; Price, J.E.; Strachan, L. The impact of methodological and measurement factors on transdiagnostic associations with intolerance of uncertainty: A meta-analysis. Clin. Psychol. Rev. 2019, 73, 101778. [Google Scholar] [CrossRef]
- Borkovec, T.D.; Ray, W.J.; Stöber, J. Worry: A cognitive phenomenon intimately linked to affective, physiological, and interpersonal behavioral processes. Cognit. Ther. Res. 1998, 22, 561–576. [Google Scholar] [CrossRef]
- Robichaud, M.; Koerner, N.; Dugas, M. Cognitive Behavioral Treatment for Generalized Anxiety Disorder: From Science to Practice; Routledge: London, UK, 2019. [Google Scholar]
- Einstein, D.A. Extension of the Transdiagnostic model to focus on intolerance of uncertainty: A review of the literature and implications for treatment. Clin. Psychol. 2014, 21, 280. [Google Scholar] [CrossRef] [PubMed]
- Zlomke, K.R.; Jeter, K.M. Stress and worry: Examining intolerance of uncertainty’s moderating effect. Anxiety Stress Coping 2013, 27, 202–215. [Google Scholar] [CrossRef]
- Vuillier, L.; May, L.; Greville-Harris, M.; Surman, R.; Moseley, R.L. The impact of the COVID-19 pandemic on individuals with eating disorders: The role of emotion regulation and exploration of online treatment experiences. J. Eat. Disord. 2021, 9, 10. [Google Scholar] [CrossRef] [PubMed]
- Sternheim, L.; Konstantellou, A.; Startup, H.; Schmidt, U. What does uncertainty mean to women with anorexia nervosa? An interpretative phenomenological analysis. Eur. Eat. Disord. Rev. 2011, 19, 12–24. [Google Scholar] [CrossRef] [PubMed]
- Prefit, A.B.; Cândea, D.M.; Szentagotai-Tătar, A. Emotion regulation across eating pathology: A meta-analysis. Appetite 2019, 143, 104438. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Clark, D.A. An information processing model of anxiety: Automatic and strategic processes. Behav. Res. Ther. 1997, 35, 49–58. [Google Scholar] [CrossRef]
- Richards, H.J.; Benson, V.; Donnelly, N.; Hadwin, J.A. Exploring the function of selective attention and hypervigilance for threat in anxiety. Clin. Psychol. Rev. 2014, 34, 1–13. [Google Scholar] [CrossRef]
- Ladouceur, R.; Gosselin, P.; Dugas, M.J. Experimental manipulation of intolerance of uncertainty: A study of a theoretical model of worry. Behav. Res. Ther. 2000, 38, 933–941. [Google Scholar] [CrossRef]
- Talkovsky, A.M.; Norton, P.J. Intolerance of uncertainty and transdiagnostic group cognitive behavioral therapy for anxiety. J. Anxiety Disord. 2016, 41, 108–114. [Google Scholar] [CrossRef]
- Charbonnier, E.; Le Vigouroux, S.; Puechlong, C.; Montalescot, L.; Goncalves, A.; Baussard, L.; Gisclard, B.; Philippe, A.G.; Lespiau, F. The Effect of intervention approaches of emotion regulation and learning strategies on students’ learning and mental health. Inquiry 2023, 60, 1–14. [Google Scholar] [CrossRef] [PubMed]

| Major Disciplines | n | (%) |
|---|---|---|
| Psychology | 514 | (24) |
| Sports science | 303 | (14) |
| Law | 175 | (8) |
| Languages | 148 | (7) |
| Biology | 143 | (7) |
| Computer science | 118 | (6) |
| Degree | ||
| First year | 594 | (28) |
| Second year | 531 | (25) |
| Third year | 426 | (20) |
| Professional degree | 14 | (1) |
| Fourth year | 277 | (13) |
| Fifth year | 173 | (8) |
| Doctorate | 68 | (3) |
| Other | 56 | (2) |
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 21.56 | 4.38 | — | |||||||||||||||
| 2. Fear of COVID-19 | 14.35 | 5.86 | 0.06 | ** | — | |||||||||||||
| 3. Anxiety | 9.96 | 4.66 | −0.01 | 0.41 | *** | — | ||||||||||||
| 4. Depressive symptoms | 7.60 | 4.29 | 0.02 | 0.28 | *** | 0.63 | *** | — | ||||||||||
| 5. Intolerance of uncertainty (IU) | 35.22 | 11.07 | −0.10 | *** | 0.31 | *** | 0.44 | *** | 0.35 | *** | — | |||||||
| 6. Prospective IU | 21.55 | 6.74 | −0.11 | *** | 0.27 | *** | 0.37 | *** | 0.28 | *** | 0.95 | *** | — | |||||
| 7. Inhibitory IU | 13.67 | 5.18 | −0.07 | ** | 0.31 | *** | 0.47 | *** | 0.39 | *** | 0.91 | *** | 0.72 | *** | — | |||
| 8. Eating-related problems | 16.71 | 13.33 | −0.04 | * | 0.10 | *** | 0.18 | *** | 0.16 | *** | 0.20 | *** | 0.18 | *** | 0.19 | *** | — | |
| 10. Adaptive coping | 2.21 | 0.85 | 0.06 | * | 0.003 | −0.11 | *** | −0.28 | *** | −0.09 | *** | −0.07 | *** | −0.10 | *** | −0.03 | ||
| 11. Acceptance | 3.53 | 1.66 | −0.01 | −0.24 | *** | −0.38 | *** | −0.41 | *** | −0.19 | *** | −0.15 | *** | −0.21 | *** | −0.09 | *** | |
| 12. Emotional support | 2.59 | 1.83 | −0.02 | 0.23 | *** | 0.30 | *** | 0.17 | *** | 0.14 | *** | 0.11 | *** | 0.15 | *** | 0.07 | ** | |
| 13. Humor | 1.32 | 1.51 | 0.02 | −0.28 | *** | −0.29 | *** | −0.31 | *** | −0.23 | *** | −0.21 | *** | −0.21 | *** | −0.10 | *** | |
| 14. Positive reframing | 2.83 | 1.69 | 0.03 | −0.17 | *** | −0.39 | *** | −0.46 | *** | −0.28 | *** | −0.24 | *** | −0.29 | *** | −0.11 | *** | |
| 15. Religion | 1.09 | 1.74 | 0.05 | * | 0.16 | *** | 0.09 | *** | 0.11 | *** | 0.06 | ** | 0.04 | 0.08 | *** | 0.03 | ||
| 16. Active coping | 1.84 | 1.47 | 0.09 | *** | 0.04 | −0.08 | *** | −0.24 | *** | −0.03 | 0.01 | −0.08 | *** | −0.01 | ||||
| 17. Planning | 2.27 | 1.65 | 0.06 | ** | 0.03 | −0.01 | −0.17 | *** | 0.01 | 0.05 | * | −0.03 | 0.02 | |||||
| 18. Instrumental support | 2.08 | 1.73 | 0.01 | 0.16 | *** | 0.18 | *** | 0.06 | ** | 0.09 | *** | 0.07 | ** | 0.11 | *** | 0.06 | ** | |
| 19. Venting | 2.33 | 1.65 | 0.03 | 0.02 | 0.01 | −0.12 | *** | −0.02 | −0.03 | −0.02 | −0.02 | |||||||
| 20. Maladaptive coping | 1.98 | 0.95 | −0.05 | * | 0.27 | *** | 0.49 | *** | 0.47 | *** | 0.32 | *** | 0.25 | *** | 0.36 | *** | 0.22 | *** |
| 21. Denial | 1.13 | 1.45 | −0.03 | 0.24 | *** | 0.23 | *** | 0.24 | *** | 0.20 | *** | 0.17 | *** | 0.21 | *** | 0.13 | *** | |
| 22. Self-distraction | 3.23 | 1.54 | −0.06 | ** | 0.10 | *** | 0.02 | −0.11 | *** | 0.03 | 0.04 | 0.01 | 0.03 | |||||
| 23. Substance abuse | 0.82 | 1.56 | 0.06 | ** | 0.08 | *** | 0.21 | *** | 0.24 | *** | 0.06 | ** | 0.02 | 0.10 | *** | 0.11 | *** | |
| 24. Behavioral disengagement | 2.21 | 1.68 | −0.05 | * | 0.18 | *** | 0.38 | *** | 0.47 | *** | 0.27 | *** | 0.21 | *** | 0.29 | *** | 0.15 | *** |
| 25. Self-blame | 2.53 | 1.88 | −0.07 | ** | 0.19 | *** | 0.53 | *** | 0.47 | *** | 0.34 | *** | 0.27 | *** | 0.39 | *** | 0.20 | *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Charbonnier, E.; Montalescot, L.; Puechlong, C.; Goncalves, A.; Le Vigouroux, S. Relationship between Fear of COVID-19, Intolerance of Uncertainty, and Coping Strategies on University Students’ Mental Health. Nutrients 2023, 15, 4938. https://doi.org/10.3390/nu15234938
Charbonnier E, Montalescot L, Puechlong C, Goncalves A, Le Vigouroux S. Relationship between Fear of COVID-19, Intolerance of Uncertainty, and Coping Strategies on University Students’ Mental Health. Nutrients. 2023; 15(23):4938. https://doi.org/10.3390/nu15234938
Chicago/Turabian StyleCharbonnier, Elodie, Lucile Montalescot, Cécile Puechlong, Aurélie Goncalves, and Sarah Le Vigouroux. 2023. "Relationship between Fear of COVID-19, Intolerance of Uncertainty, and Coping Strategies on University Students’ Mental Health" Nutrients 15, no. 23: 4938. https://doi.org/10.3390/nu15234938
APA StyleCharbonnier, E., Montalescot, L., Puechlong, C., Goncalves, A., & Le Vigouroux, S. (2023). Relationship between Fear of COVID-19, Intolerance of Uncertainty, and Coping Strategies on University Students’ Mental Health. Nutrients, 15(23), 4938. https://doi.org/10.3390/nu15234938








