Salt Intake Estimation from Urine Samples in South Asian Population: Scoping Review
Abstract
:1. Introduction
2. Methods
2.1. Stage I: Identifying the Research Question
2.2. Stage II: Identifying Relevant Studies
2.3. Stage III: Study Selection
2.4. Stage IV: Data Charting
2.5. Stage V: Reporting Results
2.6. Units
3. Results
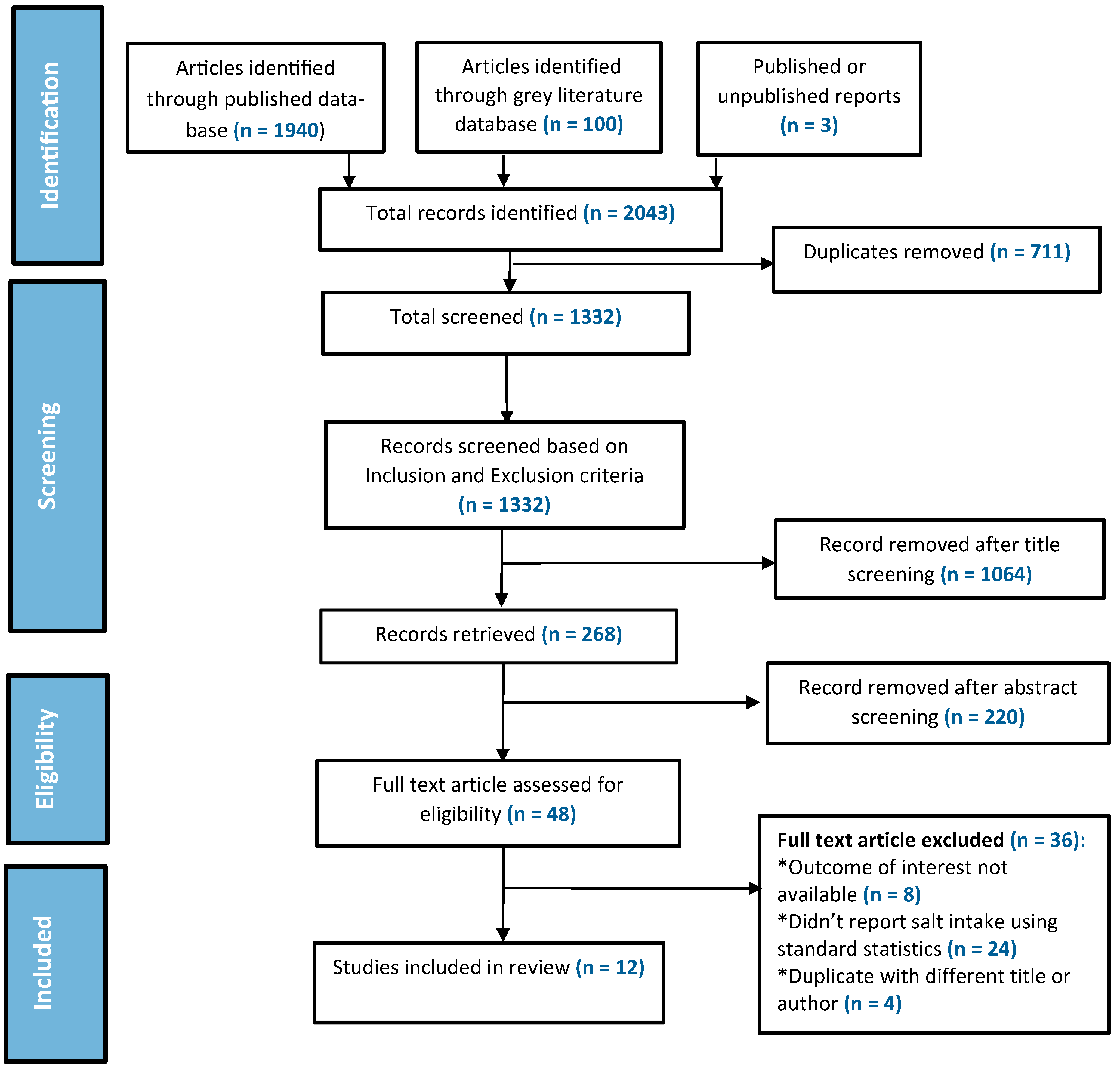
3.1. Selected Studies
3.2. Characteristics of the Included Studies
3.3. Countries with National Salt Intake Estimates
3.4. Salt Intake in Available Studies of South Asia
3.4.1. Afghanistan
3.4.2. Bangladesh
3.4.3. Bhutan
3.4.4. India
3.4.5. Nepal
3.4.6. Pakistan
3.4.7. Sri Lanka
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Noncommunicable Diseases. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 25 February 2023).
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update from the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Chen, X.; Du, J.; Wu, X.; Cao, W.; Sun, S. Global burden attributable to high sodium intake from 1990 to 2019. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 3314–3321. [Google Scholar] [CrossRef] [PubMed]
- United Nations. Political Declaration of the High-Level Meeting of the General Assembly on the Prevention and Control of Non-Communicable Diseases: Draft Resolution/Submitted by the President of the General Assembly. Available online: https://digitallibrary.un.org/record/710899/?ln=en (accessed on 13 November 2021).
- World Health Organization. Sodium Intake for Adults and Children. Available online: https://www.who.int/elena/titles/guidance_summaries/sodium_intake/en/ (accessed on 13 November 2021).
- Mohan, S.; Campbell, N.; Chockalingam, A. Time to Effectively Address Hypertension in India. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3724241/pdf/IJMR-137-627.pdf (accessed on 16 June 2022).
- World Health Organization. WHO Global Report on Sodium Intake Reduction. 2023. Available online: https://www.who.int/publications/book-orders (accessed on 13 November 2021).
- World Health Organization (WHO). Global Status Report on Noncommunicable Diseases. 2010. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 13 November 2021).
- Harnack, L.J.; Cogswell, M.E.; Shikany, J.M.; Gardner, C.D.; Gillespie, C.; Loria, C.M.; Zhou, X.; Yuan, K.; Steffen, L.M. Sources of sodium in US adults from 3 geographic regions. Circulation 2017, 135, 1775–1783. [Google Scholar] [CrossRef]
- Bishwajit, G. Nutrition transition in South Asia: The emergence of non-communicable chronic diseases. F1000Res 2015, 4, 8. [Google Scholar] [CrossRef]
- Tan, M.; Wang, C.; Song, J.; He, F.J.; MacGregor, G.A. Spot urinary sodium to monitor relative changes in population salt intake during the UK salt reduction programme. J. Hypertens. 2022, 40, 1406–1410. [Google Scholar] [CrossRef]
- Huang, L.; Crino, M.; Wu, J.H.Y.; Woodward, M.; Barzi, F.; Land, M.-A.; McLean, R.; Webster, J.; Enkhtungalag, B.; Neal, B. Mean population salt intake estimated from 24-h urine samples and spot urine samples: A systematic review and meta-analysis. Int. J. Epidemiol. 2016, 45, 239–250. [Google Scholar] [CrossRef]
- Ghimire, K.; Mishra, S.R.; Satheesh, G.; Neupane, D.; Sharma, A.; Panda, R.; Kallestrup, P.; Mclachlan, C.S. Salt intake and salt-reduction strategies in South Asia: From evidence to action. J. Clin. Hypertens. 2021, 23, 1815–1829. [Google Scholar] [CrossRef] [PubMed]
- Brown, I.J.; Tzoulaki, I.; Candeias, V.; Elliott, P. Salt intakes around the world: Implications for public health. Int. J. Epidemiol. 2009, 38, 791–813. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO STEPwise Approach to Surveillance. Available online: https://www.who.int/europe/tools-and-toolkits/who-stepwise-approach-to-surveillance#:~:text=The%20WHO%20STEPwise%20approach%20to,on%20noncommunicable%20diseases%20(NCDs) (accessed on 4 February 2023).
- Rasheed, S.; Jahan, S.; Sharmin, T.; Hoque, S.; Khanam, M.A.; Land, M.A.; Iqbal, M.; Hanifi, S.M.A.; Khatun, F.; Siddique, A.K.; et al. How much salt do adults consume in climate vulnerable coastal Bangladesh? BMC Public Health 2014, 14, 584. [Google Scholar] [CrossRef] [PubMed]
- Choudhury, S.R.; Ahmed, J.; Al Mamun, M.A. Estimation of Dietary Salt Intake by Measuring 24-Hour Urinary Sodium Excretion in Bangladeshi Population; Unpublished Report; Report of a research grant from NCDC, DGHS Grant No. DGHS/LD/NCDC/Procurement Plan/GOB(Service)/2017-2018/539/SP-09; National Heart Foundation Hospital & Research Institute: Dhaka, Bangladesh, 2018. [Google Scholar]
- Johnson, C.; Mohan, S.; Rogers, K.; Shivashankar, R.; Thout, S.R.; Gupta, P.; He, F.J.; MacGregor, G.A.; Webster, J.; Krishnan, A.; et al. Mean dietary salt intake in urban and rural areas in India: A population survey of 1395 persons. J. Am. Heart Assoc. 2017, 6, e004547. [Google Scholar] [CrossRef] [PubMed]
- Neupane, D.; Rijal, A.; Henry, M.E.; Kallestrup, P.; Koirala, B.; Mclachlan, C.S.; Ghimire, K.; Zhao, D.; Sharma, S.; Pokharel, Y.; et al. Mean dietary salt intake in Nepal: A population survey with 24-hour urine collections. J. Clin. Hypertens. 2020, 22, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Arif, M.; Saqib, N.; Rafique, I.; Ansar, M.; Rahat, T. Daily Salt Intake, its Discretionary Use and Validation of Methods for Estimation using Spot Urine-Findings from Islamabad, Pakistan. medRxiv 2020. [Google Scholar] [CrossRef]
- Jayatissa, R.; Yamori, Y.; de Silva, A.; Mori, M.; De Silva, P.C.; De Silva, K.H. Estimation of salt intake, potassium intake and sodium-to-potassium ratio by 24-hour urinary excretion: An urban rural study in Sri Lanka. medRxiv 2020. [Google Scholar] [CrossRef]
- Ministry of Public Health Afghanistan. National Non-Communicable Disease Risk Factors Survey (STEPS Survey): Country Report for Afghanistan. 2018. Available online: https://extranet.who.int/ncdsmicrodata/index.php/catalog/782 (accessed on 4 February 2023).
- Ministry of Health and Family Welfare; National Institute of Preventive and Social Medicine; World Health Organization. National STEPS Survey for Non-Communicable Diseases Risk Factors in Bangladesh. 2018. Available online: https://extranet.who.int/ncdsmicrodata/index.php/catalog/770/related-materials (accessed on 4 February 2023).
- World Health Organization, Regional Office for South-East Asia. National Survey for Noncommunicable Disease Risk Factors and Mental Health Using WHO STEPS Approach in BHUTAN. 2014. Available online: https://extranet.who.int/ncdsmicrodata/index.php/catalog/427/related-materials (accessed on 4 February 2023).
- Mathur, P.; Kulothungan, V.; Leburu, S.; Krishnan, A.; Chaturvedi, H.K.; Salve, H.R.; Amarchand, R.; Nongkynrih, B.; Kumar, P.G.; Vinay Urs, K.S.; et al. National noncommunicable disease monitoring survey (NNMS) in India: Estimating risk factor prevalence in adult population. PLoS ONE 2021, 16, e0246712. [Google Scholar] [CrossRef]
- Sarma, P.S.; Sadanandan, R.; Thulaseedharan, J.V.; Soman, B.; Srinivasan, K.; Varma, R.P.; Nair, M.R.; Pradeepkumar, A.S.; Jeemon, P.; Thankappan, K.R.; et al. Prevalence of risk factors of non-communicable diseases in Kerala, India: Results of a cross-sectional study. BMJ Open 2019, 9, e027880. [Google Scholar] [CrossRef]
- Dhimal, M.; Bista, B.; Bhattarai, S.; Dixit, L.P.; Hyder, M.K.A.; Agrawal, N.; Rani, M.; Jha, A.K. Noncommunicable Disease Risk Factors: STEPS Survey Nepal 2019. Available online: https://www.who.int/docs/default-source/nepal-documents/ncds/ncd-steps-survey-2019-compressed.pdf (accessed on 15 June 2022).
- Kwong, E.J.L.; Whiting, S.; Bunge, A.C.; Leven, Y.; Breda, J.; Rakovac, I.; Cappuccio, F.P.; Wickramasinghe, K. Population level salt intake in the WHO European Region in 2022: A systematic review. Public Health Nutr. 2022, 1–14. [Google Scholar] [CrossRef]
- Land, M.A.; Webster, J.; Christoforou, A.; Praveen, D.; Jeffery, P.; Chalmers, J.; Smith, W.; Woodward, M.; Barzi, F.; Nowson, C.; et al. Salt intake assessed by 24 h urinary sodium excretion in a random and opportunistic sample in Australia. BMJ Open 2014, 4, e003720. [Google Scholar] [CrossRef]
- Cogswell, M.E.; Loria, C.M.; Terry, A.L.; Zhao, L.; Wang, C.-Y.; Chen, T.-C.; Wright, J.D.; Pfeiffer, C.M.; Merritt, R.; Moy, C.S.; et al. Estimated 24-hour urinary sodium and potassium excretion in US Adults. JAMA-J. Am. Med. Assoc. 2018, 319, 1209–1220. [Google Scholar] [CrossRef]
- Batcagan-Abueg, A.P.M.; Lee, J.J.M.; Chan, P.; A Rebello, S.; Amarra, M.S.V. Salt intakes and salt reduction initiatives in southeast asia: A review. Asia Pac. J. Clin. Nutr. 2013, 22, 490–504. [Google Scholar]
- Zhang, J.-Y.; Yan, L.-X.; Tang, J.-L.; Ma, J.-X.; Guo, X.-L.; Zhao, W.-H.; Zhang, X.-F.; Li, J.-H.; Chu, J.; Bi, Z.-Q. Estimating daily salt intake based on 24 h urinary sodium excretion in adults aged 18–69 years in Shandong, China. BMJ Open 2014, 4, e005089. [Google Scholar] [CrossRef] [PubMed]

| For Published Article | For the Grey Literature |
|---|---|
| PubMed | Open grey |
| MEDLINE | Google Scholar |
| EMBASE | WHO official database |
| EBSCO | Key informant consultation |
| Country-specific Government website |
| Topic | Search Terms |
|---|---|
| Salt | Salt OR Sodium OR Sodium Chloride |
| Consumption | Intake OR Ingest OR Eat OR Consume OR Diet |
| Excretion | Urine OR Excrete OR 24 h urine OR Spot urine |
| South Asia | Asia OR South Asia OR Afghanistan OR Bangladesh OR India OR Nepal OR Pakistan OR Sri Lanka OR Bhutan OR Maldives |
| Search string: (Salt OR Sodium OR Sodium Chloride) AND (Intake OR Ingest OR Eat OR Consume OR Diet) AND (Urine OR Excrete OR 24 h urine OR Spot urine) AND (Asia OR South Asia OR Afghanistan OR Bangladesh OR India OR Nepal OR Pakistan OR Sri Lanka OR Bhutan). | |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| 1. Studies conducted in SAARC countries (Afghanistan, Bangladesh, India, Nepal, Pakistan, Sri Lanka, and Bhutan) | 1. If the salt intake was not reported in standard statistics (mean/median intake of salt) |
| 2. Studies estimated salt/sodium intake by measuring urinary sodium excretion | 2. Studies conducted on only special sub-populations |
| 3. Studies conducted among minimum of 100 participants | 3. Studies conducted among pregnant women or children |
| 4. Written in the English language | |
| 5. Published between January 2011 to October 2021 |
| (A) | |||||
| Country | Authors | Year | Type of Study | Sampling Technique, Study Population, Sample Size, and Sample Characteristics (Age and Sex) | |
| Bangladesh | Rasheed et al. [17] | 2014 | Cross-sectional study | 388 individuals from a community were randomly chosen for a cross-sectional household survey in Chakaria, a rural area of Bangladesh. The participants’ mean age was 44.6 years, with 50% of them being female. | |
| Bangladesh | Choudhury et al. [18] | - | Cross-sectional study | 839 community members were randomly chosen from the urban and rural areas of Khulna, Dhaka, and Rangpur, aged 30–59 years, and 49.8% were female. | |
| India | Johnson et al. [19] | 2017 | Cross-sectional study | 637 adults, the average age was 40.2 years and 48.2% were female selected from urban, rural, and slum areas in north India (Delhi and Faridabad, Haryana) and in south India (Hyderabad and West Godavari, Andhra Pradesh). | |
| Nepal | Neupane et al. [20] | 2019 | Cross-sectional study | 451 randomly selected participants, with a mean age of 49.6 years, and 65.4% were female. | |
| Pakistan | Saqib et al. [21] | 2020 | Cross-sectional study | 120 participants were chosen using a non-probability convenient sampling method; the average age was 26.5 years, and 23% were female. | |
| Sri Lanka | Jayatissa et al. [22] | 2020 | Cross-sectional study | 328 randomly selected community residents aged 30–59 years, with 53.7% being female. | |
| (B) | |||||
| Country | Authors | Year | Type of Study | Sampling Technique, Study Population, Sample Size, and Sample Characteristics (Age and Sex) | Equation Used for Estimating Sodium Intake Using Spot Urine |
| Afghanistan | WHO [23] | 2018 | Population-based national cross-sectional STEPS study | 3956 community dwellers, aged 18–69 years and 48.8% female were selected by multistage stratified random sampling technique. | INTERSALT |
| Bangladesh | WHO [24] | 2018 | Population-based national cross-sectional STEPS study | 9900 individuals aged 18–69 years and 50.7% female were selected by a multistage geographically stratified probability-based sampling process. | Tanaka |
| Bhutan | WHO [25] | 2014 | Population-based national cross-sectional STEPS study | 2816 individuals aged 18–69 years and 61.9% were female selected by multistage cluster sampling. | INTERSALT |
| India | Mathur et al. [26] | 2021 | Nationally representative cross-sectional study | 2266 participants aged 18 to 69 years and 48.2% female, were chosen using a stratified multistage selection technique. | INTERSALT |
| India | Sarma et al. [27] | 2019 | Community-based cross-sectional study | 12,012 participants were selected by the multistage cluster sampling method. Participants were aged 18–69 years, and 62.8% were female. | Modified Kawaski |
| Nepal | WHO [28] | 2019 | Population-based cross-sectional STEPS study | 5593 adults selected through multistage cluster sampling technique, aged 55–69 years, and 63.3% were female | INTERSALT |
| Country | Authors and Year | Level of Salt Intake (g/day) | ||
|---|---|---|---|---|
| Average | Male | Female | ||
| (A) | ||||
| Bangladesh | Rasheed et al. (2014) [17] | 6.7 | - | - |
| Choudhury [18] | 9.0 (9 ± 4.3) | - | - | |
| India | Johnson et al. (2017) [19] | Andhra Pradesh: 9.5 (9.1–9.9) Delhi and Haryana: 8.6 (7.9–9.5) | - | - |
| Nepal | Neupane et al. (2019) [20] | 13.3 (12.8–13.7) | 14.4 (13.6–15.2) | 12.7 (12.2–13.2) |
| Pakistan | Saqib et al. (2020) [21] | 8.7 (4.2–13.1) | 9.2 (4.7–13.8) | 8.7 (4.2–13.1) |
| Sri Lanka | Jayatissa et al. (2020) [22] | 8.4 (7.9–8.8) | 9.0 (8.3–9.8) | 7.7 (7.2–8.2) |
| (B) | ||||
| Afghanistan | WHO (2018) [23] | 12.1 (11.1–13.1) | 12.5 (10.9–14) | 11.8 (10.5–13.1) |
| Bangladesh | WHO (2018) [24] | 9 (8.9–9.1) | 12.5 (10.9–14.0) | 11.8 (10.5–13.1) |
| Bhutan | WHO (2014) [25] | 9 (8.8–9.1) | 9.6(9.4–9.8) | 8 (7.9–8.2) |
| India | Mathur et al. (2021) [26] | 8.0 (7.8–8.2) | 8.9 (8.7–9.2) | 7.1 (6.9–7.2) |
| Sarma et al. (2019) [27] | 6.7 (6.6–6.8) | 5.3 (5.2–5.4) | 7.5 (7.4–7.6) | |
| Nepal | WHO (2019) [28] | 9.1 (9.0–9.2) | 9.6 (9.4–9.8) | 8.7 (8.6–8.8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Afroza, U.; Abrar, A.K.; Nowar, A.; Akhtar, J.; Mamun, M.A.A.; Sobhan, S.M.M.; Cobb, L.; Ide, N.; Choudhury, S.R. Salt Intake Estimation from Urine Samples in South Asian Population: Scoping Review. Nutrients 2023, 15, 4358. https://doi.org/10.3390/nu15204358
Afroza U, Abrar AK, Nowar A, Akhtar J, Mamun MAA, Sobhan SMM, Cobb L, Ide N, Choudhury SR. Salt Intake Estimation from Urine Samples in South Asian Population: Scoping Review. Nutrients. 2023; 15(20):4358. https://doi.org/10.3390/nu15204358
Chicago/Turabian StyleAfroza, Ummay, Ahmad Khairul Abrar, Abira Nowar, Jubaida Akhtar, Mohammad Abdullah Al Mamun, Sheikh Mohammad Mahbubus Sobhan, Laura Cobb, Nicole Ide, and Sohel Reza Choudhury. 2023. "Salt Intake Estimation from Urine Samples in South Asian Population: Scoping Review" Nutrients 15, no. 20: 4358. https://doi.org/10.3390/nu15204358
APA StyleAfroza, U., Abrar, A. K., Nowar, A., Akhtar, J., Mamun, M. A. A., Sobhan, S. M. M., Cobb, L., Ide, N., & Choudhury, S. R. (2023). Salt Intake Estimation from Urine Samples in South Asian Population: Scoping Review. Nutrients, 15(20), 4358. https://doi.org/10.3390/nu15204358






