Nutrient Intake and Status in Children and Adolescents Consuming Plant-Based Diets Compared to Meat-Eaters: A Systematic Review
Abstract
:1. Introduction
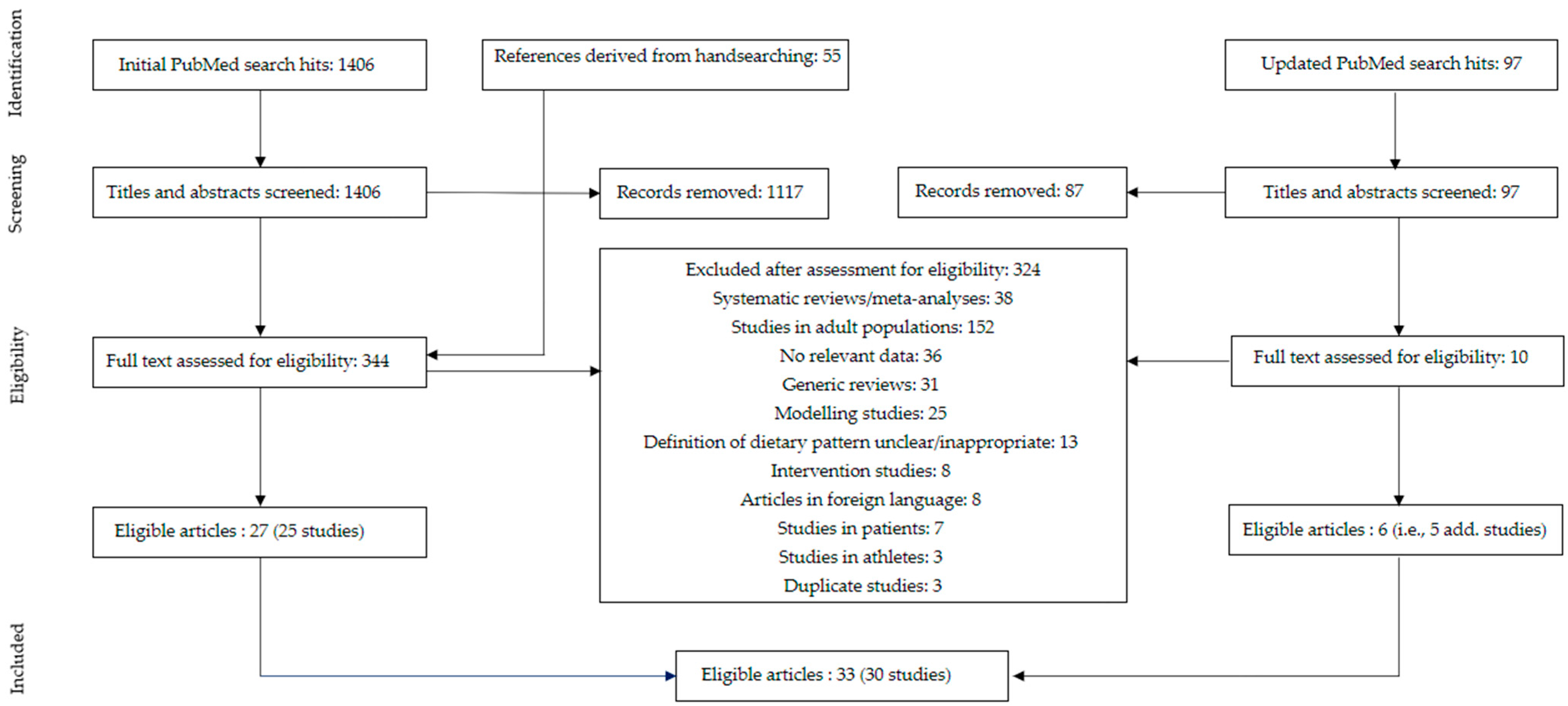
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
- Study population: Generally healthy children and/or adolescents aged 2 to 18 years. We excluded studies on infants (<2 years) because they have specific dietary needs, including breastfeeding and complementary foods. We also excluded studies conducted in populations with specific diseases.
- Type of studies: Observational studies and intervention studies (baseline data only), that compared nutrient intake and/or status of participants following a predominantly plant-based diet with participants following a conventional diet with meat were included. In addition, studies that reported only on subjects following a predominantly plant-based diet were also included. Generic reviews, case studies, and articles not published in the English language were excluded.
- Diets: To be included in our review, studies had to report on voluntary self-selected diets with a primary focus on reducing animal food intake. Studies reporting on imposed or predesigned plant-based diets (e.g., marginal plant-based staple diets in developing countries, a prescribed vegetarian diet intervention, or a modeled vegetarian diet scenario) were excluded, as well as articles on overly restrictive plant-based diets (e.g., raw food diet, macrobiotic diet) or healthy diets designed to lower non-communicable diseases (e.g., DASH diet, Mediterranean diet).
- Outcome parameters: The included studies provided data on one or more of the following parameters: dietary intake of energy, protein, saturated fatty acids (SAFA), poly-unsaturated fatty acids (PUFA), α-linolenic acid (ALA), and eicosapentanoic acid (EPA); docosahexanoic acid (DHA); dietary intake or nutritional status of micronutrients; bone markers.
2.3. Data Extraction
2.4. Data Handling
- Vegan: consuming no meat, fish, dairy, and eggs at all/not during the days of dietary assessment OR ≤ once per month OR self-defined vegans;
- Vegetarian: consuming no meat and fish at all/not during the days of dietary assessment OR ≤ once per month OR self-defined vegetarians;
- Pesco-vegetarian: consuming no meat at all/not during the days of dietary assessment OR ≤ once per month OR self-defined;
- Semi-vegetarian: consuming meat (and fish) ≤ once per week but > once per month OR consuming meat (and fish) “seldom”/“occasionally”;
- Meat eating: consuming meat > once per week OR self-defined.
2.5. Data Analysis
3. Results
3.1. Study Selection and Study Characteristics
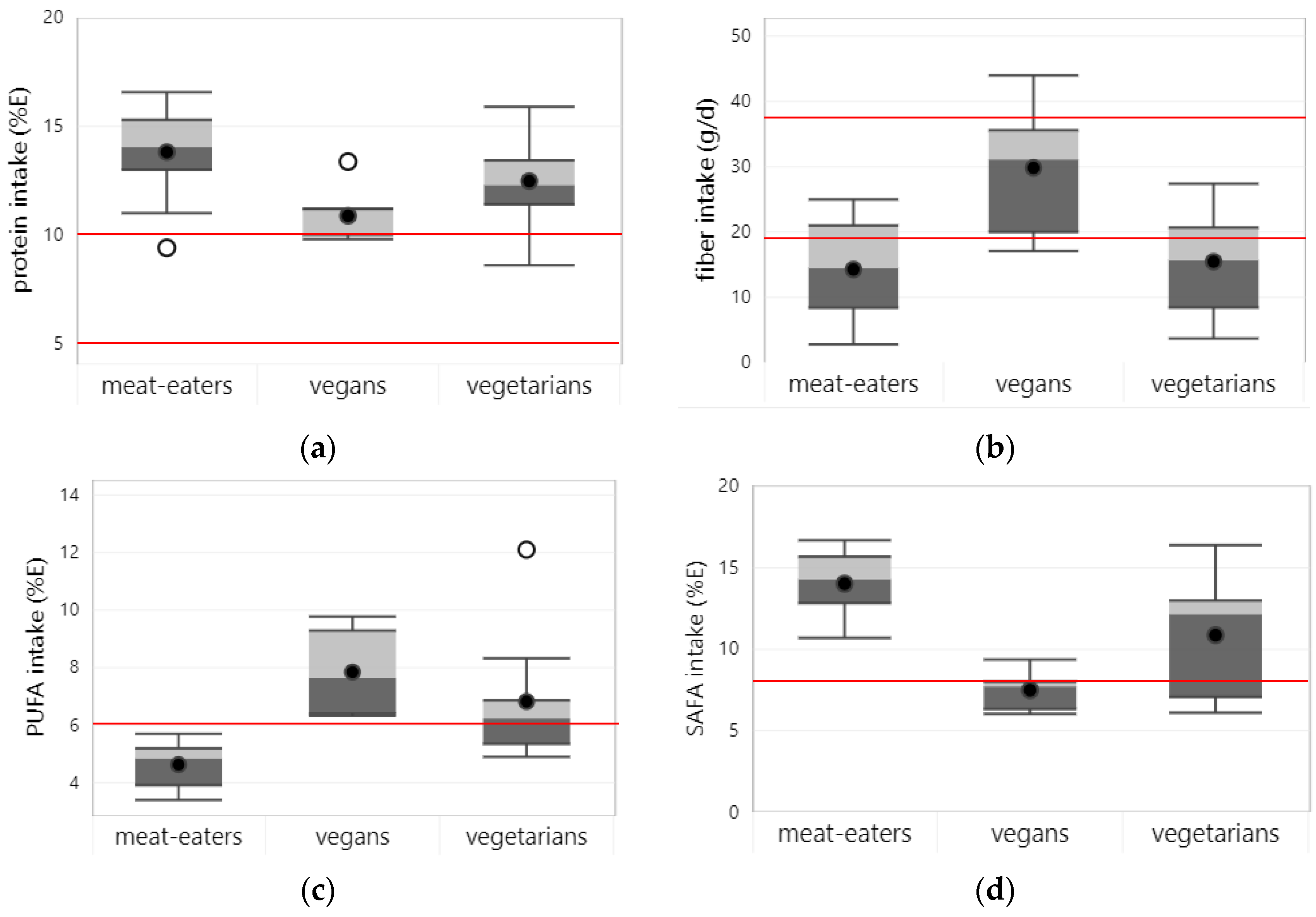
3.2. Energy, Protein, Fatty Acids, and Fiber
3.2.1. Energy
3.2.2. Protein
3.2.3. Fiber
3.2.4. Polyunsaturated Fatty Acids
3.2.5. N-3 Fatty Acids
3.2.6. Saturated Fatty Acids
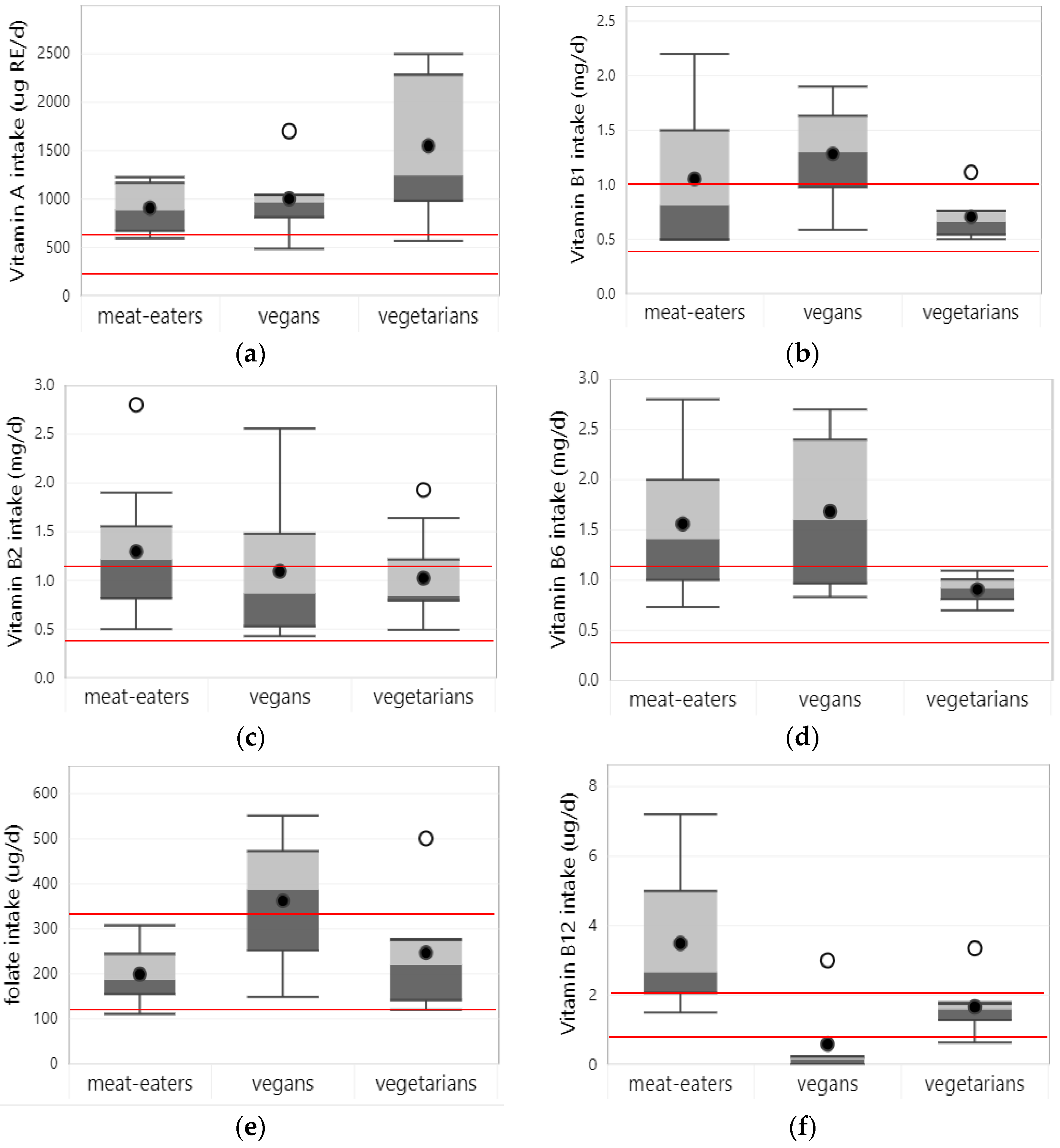
3.3. Vitamins
3.3.1. Vitamin A
3.3.2. Vitamin B1
3.3.3. Vitamin B2
3.3.4. Niacin
3.3.5. Vitamin B6
3.3.6. Folate
3.3.7. Vitamin B12
3.3.8. Vitamin C
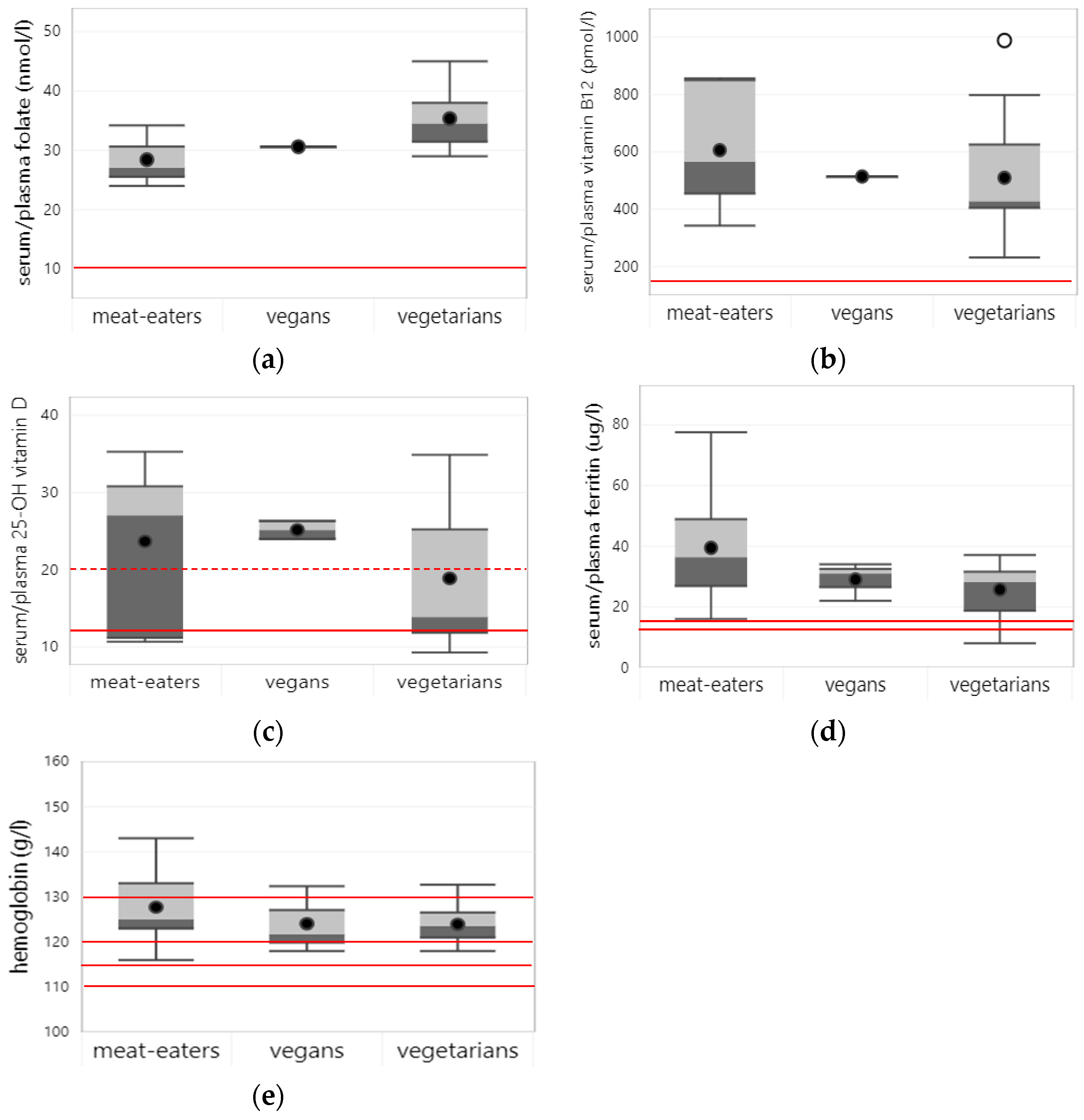
3.3.9. Vitamin D
3.3.10. Vitamin E
3.4. Minerals
3.4.1. Iron
3.4.2. Zinc
3.4.3. Iodine
3.4.4. Calcium
3.4.5. Magnesium
3.4.6. Phosphorus
4. Discussion
4.1. Main Findings and Their Significance
4.2. Strengths and Limitations of This Review
4.3. Putting Findings on Energy and Macronutrients into Perspective
4.4. Putting Findings on Micronutrients into Perspective
4.5. Findings in Other Age Groups
4.6. Public Health Recommendations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- FAO; WHO. Sustainable Healthy Diets-Guiding Principles; Food and Agriculture Organization of the United Nations, World Health Organization: Rome, Italy, 2019.
- Barnard, N.D.; Leroy, F. Children and adults should avoid consuming animal products to reduce risk for chronic disease: YES. Am. J. Clin. Nutr. 2020, 112, 926–930. [Google Scholar] [CrossRef] [PubMed]
- Craig, W.J.; Mangels, A.R.; Fresán, U.; Marsh, K.; Miles, F.L.; Saunders, A.V.; Haddad, E.H.; Heskey, C.E.; Johnston, P.; Larson-Meyer, E.; et al. The Safe and Effective Use of Plant-Based Diets with Guidelines for Health Professionals. Nutrients 2021, 13, 4144. [Google Scholar] [CrossRef] [PubMed]
- Leroy, F.; Barnard, N.D. Children and adults should avoid consuming animal products to reduce risk for chronic disease: NO. Am. J. Clin. Nutr. 2020, 112, 931–936. [Google Scholar] [CrossRef]
- Kiely, M.E. Risks and benefits of vegan and vegetarian diets in children. Proc. Nutr. Soc. 2021, 80, 159–164. [Google Scholar] [CrossRef] [PubMed]
- FAO. Protein Quality Evaluation. Report of Joint FAO/WHO Expert Consultation; FAO: Rome, Italy, 1991. [Google Scholar]
- WHO; FAO; UNU. Protein and Amino Acid Requirements in Human Nutrition. Report of a Joint WHO/FAO/UNU Expert Consultation; WHO: Geneva, Switzerland, 2007.
- FAO. Fats and Fatty Acids in Human Nutrition. Report of an Expert Consultation; Food and Agriculture Organization: Rome, Italy, 2010. [Google Scholar]
- IOM. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients); Institute of Medicine: Washington, DC, USA, 2005. [Google Scholar]
- Sutter, D.O.; Bender, N. Nutrient status and growth in vegan children. Nutr. Res. 2021, 91, 13–25. [Google Scholar] [CrossRef] [PubMed]
- Schürmann, S.; Kersting, M.; Alexy, U. Vegetarian diets in children: A systematic review. Eur. J. Nutr. 2017, 56, 1797–1817. [Google Scholar] [CrossRef] [PubMed]
- Stevens, G.A.; Beal, T.; Mbuya, M.N.N.; Luo, H.; Neufeld, L.M.; Global Micronutrient Deficiencies Research, G. Micronutrient deficiencies among preschool-aged children and women of reproductive age worldwide: A pooled analysis of individual-level data from population-representative surveys. Lancet Glob. Health 2022, 10, e1590–e1599. [Google Scholar] [CrossRef] [PubMed]
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2022; FAO: Rome, Italy, 2022; p. 260. [Google Scholar]
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 4 May 2023).
- Sabate, J.; Wien, M. Vegetarian diets and childhood obesity prevention. Am. J. Clin. Nutr. 2010, 91, 1525S–1529S. [Google Scholar] [CrossRef] [PubMed]
- Neufingerl, N.; Eilander, A. Nutrient Intake and Status in Adults Consuming Plant-Based Diets Compared to Meat-Eaters: A Systematic Review. Nutrients 2021, 14, 29. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Li, T.; Deeks, J.J. Obtaining standard deviations from standard errors and confidence intervals for group means. In Cochrane Handbook for Systematic Reviews of Interventions, Version 6.1 (updated September 2020) ed.; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: Cochrane, AB, Canada, 2020. [Google Scholar]
- Wan, X.; Wang, W.; Jiming, L.; Tiejun, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Medical Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef]
- Instititute of Medicine. Dietary Reference Intakes. The Essential Guide to Nutrient Requirements; Instititute of Medicine: Washington, DC, USA, 2006. [Google Scholar]
- Instititute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D; Institute of Medicine: Washington, DC, USA, 2011. [Google Scholar]
- Drukker, M.; Weltens, I.; van Hooijdonk, C.F.M.; Vandenberk, E.; Bak, M. Development of a Methodological Quality Criteria List for Observational Studies: The Observational Study Quality Evaluation. Front. Res. Metr. Anal. 2021, 6, 675071. [Google Scholar] [CrossRef] [PubMed]
- Osei-Boadi, K.; Lartey, A.; Marquis, G.S.; Colecraft, E.K. Dietary intakes and iron status of vegetarian and nonvegetarian children in selected communities in Accra and Cape Coast, Ghana. Afr. J. Food Agric. Nutr. Dev. 2012, 12, 5822–5842. [Google Scholar]
- Pal, R.; Sagar, V. Correlates of vitamin A deficiency among Indian rural preschool-age children. Eur. J. Ophthalmol. 2007, 17, 1007–1009. [Google Scholar] [CrossRef]
- Weder, S.; Hoffmann, M.; Becker, K.; Alexy, U.; Keller, M. Energy, Macronutrient Intake, and Anthropometrics of Vegetarian, Vegan, and Omnivorous Children (1–3 Years) in Germany (VeChi Diet Study). Nutrients 2019, 11, 832. [Google Scholar] [CrossRef] [PubMed]
- Thane, C.W.; Bates, C.J. Dietary intakes and nutrient status of vegetarian preschool children from a British national survey. J. Hum. Nutr. Diet. 2000, 13, 149–162. [Google Scholar] [CrossRef]
- Hovinen, T.; Korkalo, L.; Freese, R.; Skaffari, E.; Isohanni, P.; Niemi, M.; Nevalainen, J.; Gylling, H.; Zamboni, N.; Erkkola, M.; et al. Vegan diet in young children remodels metabolism and challenges the statuses of essential nutrients. EMBO Mol. Med. 2021, 13, e13492. [Google Scholar] [CrossRef] [PubMed]
- Elliott, L.J.; Keown-Stoneman, C.D.G.; Birken, C.S.; Jenkins, D.J.A.; Borkhoff, C.M.; Maguire, J.L. Vegetarian Diet, Growth, and Nutrition in Early Childhood: A Longitudinal Cohort Study. Pediatrics 2022, 149, e2021052598. [Google Scholar] [CrossRef]
- Weder, S.; Keller, M.; Fischer, M.; Becker, K.; Alexy, U. Intake of micronutrients and fatty acids of vegetarian, vegan, and omnivorous children (1–3 years) in Germany (VeChi Diet Study). Eur. J. Nutr. 2022, 61, 1507–1520. [Google Scholar] [CrossRef] [PubMed]
- Kehoe, S.H.; Krishnaveni, G.V.; Veena, S.R.; Guntupalli, A.M.; Margetts, B.M.; Fall, C.H.D.; Robinson, S.M. Diet patterns are associated with demographic factors and nutritional status in South Indian children. Matern. Child. Nutr. 2014, 10, 145–158. [Google Scholar] [CrossRef]
- Perry, C.L.; McGuire, M.T.; Neumark-Sztainer, D.; Story, M. Adolescent vegetarians: How well do their dietary patterns meet the healthy people 2010 objectives? Arch. Pediatr. Adolesc. Med. 2002, 156, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Grant, R.; Bilgin, A.; Zeuschner, C.; Guy, T.; Pearce, R.; Hokin, B.; Ashton, J. The relative impact of a vegetable-rich diet on key markers of health in a cohort of Australian adolescents. Asia Pac. J. Clin. Nutr. 2008, 17, 107–115. [Google Scholar]
- Gorczyca, D.; Prescha, A.; Szeremeta, K. Impact of vegetarian diet on serum immunoglobulin levels in children. Clin. Pediatr. 2013, 52, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Ambroszkiewicz, J.; Klemarczyk, W.; Mazur, J.; Gajewska, J.; Rowicka, G.; Strucińska, M.; Chełchowska, M. Serum Hepcidin and Soluble Transferrin Receptor in the Assessment of Iron Metabolism in Children on a Vegetarian Diet. Biol. Trace Elem. Res. 2017, 180, 182–190. [Google Scholar] [CrossRef] [PubMed]
- Leung, S.S.; Lee, R.H.; Sung, R.Y.; Luo, H.Y.; Kam, C.W.; Yuen, M.P.; Hjelm, M.; Lee, S.H. Growth and nutrition of Chinese vegetarian children in Hong Kong. J. Paediatr. Child Health 2001, 37, 247–253. [Google Scholar] [CrossRef]
- Gorczyca, D.; Paściak, M.; Szponar, B.; Gamian, A.; Jankowski, A. An impact of the diet on serum fatty acid and lipid profiles in Polish vegetarian children and children with allergy. Eur. J. Clin. Nutr. 2011, 65, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Peddie, M.; Scott, T.; Ranasinghe, C.; Fleming, E.; Webster, K.; Brown, R.; Houghton, L.; Haszard, J. A Sample of Female Adolescent Self-Identified Vegetarians in New Zealand Consume Less Protein and Saturated Fat, but More Fiber than Their Omnivorous Peers. Nutrients 2022, 14, 711. [Google Scholar] [CrossRef] [PubMed]
- Laskowska-Klita, T.; Chełchowska, M.; Ambroszkiewicz, J.; Gajewska, J.; Klemarczyk, W. The effect of vegetarian diet on selected essential nutrients in children. Med. Wieku Rozw. 2011, 15, 318–325. [Google Scholar]
- Larsson, C.L.; Johansson, G.K. Dietary intake and nutritional status of young vegans and omnivores in Sweden. Am. J. Clin. Nutr. 2002, 76, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Yen, C.-E.; Yen, C.-H.; Huang, M.-C.; Cheng, C.-H.; Huang, Y.-C. Dietary intake and nutritional status of vegetarian and omnivorous preschool children and their parents in Taiwan. Nutr. Res. 2008, 28, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Rush, E.C.; Chhichhia, P.; Hinckson, E.; Nabiryo, C. Dietary patterns and vitamin B(12) status of migrant Indian preadolescent girls. Eur. J. Clin. Nutr. 2009, 63, 585–587. [Google Scholar] [CrossRef] [PubMed]
- Desmond, M.A.; Sobiecki, J.G.; Jaworski, M.; Płudowski, P.; Antoniewicz, J.; Shirley, M.K.; Eaton, S.; Książyk, J.; Cortina-Borja, M.; De Stavola, B.; et al. Growth, body composition, and cardiovascular and nutritional risk of 5- to 10-y-old children consuming vegetarian, vegan, or omnivore diets. Am. J. Clin. Nutr. 2021, 113, 1565–1577. [Google Scholar] [CrossRef] [PubMed]
- Ambroszkiewicz, J.; Chełchowska, M.; Szamotulska, K.; Rowicka, G.; Klemarczyk, W.; Strucińska, M.; Gajewska, J. The Assessment of Bone Regulatory Pathways, Bone Turnover, and Bone Mineral Density in Vegetarian and Omnivorous Children. Nutrients 2018, 10, 183. [Google Scholar] [CrossRef] [PubMed]
- Thane, C.W.; Walmsley, C.M.; Bates, C.J.; Prentice, A.; Cole, T.J. Risk factors for poor iron status in British toddlers: Further analysis of data from the National Diet and Nutrition Survey of children aged 1.5–4.5 years. Public Health Nutr. 2000, 3, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Skolmowska, D.; Głąbska, D. Analysis of Heme and Non-Heme Iron Intake and Iron Dietary Sources in Adolescent Menstruating Females in a National Polish Sample. Nutrients 2019, 11, 1049. [Google Scholar] [CrossRef] [PubMed]
- Thane, C.W.; Bates, C.J.; Prentice, A. Risk factors for low iron intake and poor iron status in a national sample of British young people aged 4–18 years. Public Health Nutr. 2003, 6, 485–496. [Google Scholar] [CrossRef]
- Bhatti, A.S.; Mahida, V.I.; Gupte, S.C. Iron status of Hindu brahmin, Jain and Muslim communities in Surat, Gujarat. Indian J. Hematol. Blood Transfus. 2007, 23, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Gorczyca, D.; Prescha, A.; Szeremeta, K.; Jankowski, A. Iron status and dietary iron intake of vegetarian children from Poland. Ann. Nutr. Metab. 2013, 62, 291–297. [Google Scholar] [CrossRef]
- Ambroszkiewicz, J.; Klemarczyk, W.; Gajewska, J.; Chełchowska, M.; Laskowska-Klita, T. Serum concentration of biochemical bone turnover markers in vegetarian children. Adv. Med. Sci. 2007, 52, 279–282. [Google Scholar]
- Murphy, S.P.; Poos, M.I. Dietary Reference Intakes: Summary of applications in dietary assessment. Public Health Nutr. 2002, 5, 843–849. [Google Scholar] [CrossRef]
- Willett, W.C.; Ludwig, D.S. Milk and Health. N. Engl. J. Med. 2020, 382, 644–654. [Google Scholar] [CrossRef] [PubMed]
- Grenov, B.; Larnkjær, A.; Mølgaard, C.; Michaelsen, K.F. Role of Milk and Dairy Products in Growth of the Child. Nestle Nutr. Inst. Workshop Ser. 2020, 93, 77–90. [Google Scholar] [CrossRef] [PubMed]
- Rangan, A.M.; Flood, V.M.; Denyer, G.; Webb, K.; Marks, G.B.; Gill, T.P. Dairy consumption and diet quality in a sample of Australian children. J. Am. Coll. Nutr. 2012, 31, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Iglesia, I.; Intemann, T.; De Miguel-Etayo, P.; Pala, V.; Hebestreit, A.; Wolters, M.; Russo, P.; Veidebaum, T.; Papoutsou, S.; Nagy, P.; et al. Dairy Consumption at Snack Meal Occasions and the Overall Quality of Diet during Childhood. Prospective and Cross-Sectional Analyses from the IDEFICS/I.Family Cohort. Nutrients 2020, 12, 642. [Google Scholar] [CrossRef] [PubMed]
- de Lamas, C.; de Castro, M.J.; Gil-Campos, M.; Gil, A.; Couce, M.L.; Leis, R. Effects of Dairy Product Consumption on Height and Bone Mineral Content in Children: A Systematic Review of Controlled Trials. Adv. Nutr. 2019, 10, S88–S96. [Google Scholar] [CrossRef]
- Sioen, I.; van Lieshout, L.; Eilander, A.; Fleith, M.; Lohner, S.; Szommer, A.; Petisca, C.; Eussen, S.; Forsyth, S.; Calder, P.C.; et al. Systematic Review on N-3 and N-6 Polyunsaturated Fatty Acid Intake in European Countries in Light of the Current Recommendations-Focus on Specific Population Groups. Ann. Nutr. Metab. 2017, 70, 39–50. [Google Scholar] [CrossRef]
- Simeone, G.; Bergamini, M.; Verga, M.C.; Cuomo, B.; D’Antonio, G.; Iacono, I.D.; Mauro, D.D.; Mauro, F.D.; Mauro, G.D.; Leonardi, L.; et al. Do Vegetarian Diets Provide Adequate Nutrient Intake during Complementary Feeding? A Systematic Review. Nutrients 2022, 14, 3591. [Google Scholar] [CrossRef]
- National Health Service. The Vegan Diet. Available online: https://www.nhs.uk/live-well/eat-well/how-to-eat-a-balanced-diet/the-vegan-diet/ (accessed on 14 August 2023).
- Melina, V.; Craig, W.; Levin, S. Position of the Academy of Nutrition and Dietetics: Vegetarian Diets. J. Acad. Nutr. Diet. 2016, 116, 1970–1980. [Google Scholar] [CrossRef]
- Amit, M. Vegetarian diets in children and adolescents. Paediatr. Child Health 2010, 15, 303–314. [Google Scholar]
- Council, N.H.a.M.R. Australian Dietary Guidelines; National Health and Medical Research Council Canberra: Canberra, Australia, 2013. [Google Scholar]
- National Programme for the Promotion of a Healthy Diet. Guidelines for a Healthy Vegetarian Diet; Portuguese National Program for the Promotion of a Healthy Diet Lissabon: Lisbon, Portugal, 2015. [Google Scholar]
- Richter, M.; Boeing, H.; Grunewald-Funk, D.; Heseker, H.; Kroke, A.; Leschik-Bonnet, E.; Oberritter, H.; Strohm, D.; Watzl, B. Vegan diet. Position of the German Nutrition Society (DGE). Ernahr. Umsch. 2016, 63, 92–102. [Google Scholar] [CrossRef]
- Lemale, J.; Mas, E.; Jung, C.; Bellaiche, M.; Tounian, P.; French-speaking Pediatric Hepatology, G.; Nutrition, G. Vegan diet in children and adolescents. Recommendations from the French-speaking Pediatric Hepatology, Gastroenterology and Nutrition Group (GFHGNP). Arch. Pediatr. 2019, 26, 442–450. [Google Scholar] [CrossRef]
- Redecillas-Ferreiro, S.; Moráis-López, A.; Moreno-Villares, J.M. Position paper on vegetarian diets in infants and children. Committee on Nutrition and Breastfeeding of the Spanish Paediatric Association. An. De Pediatría 2020, 95, 306.e301–306.e306. [Google Scholar] [CrossRef]
- Dutch Nutrition Center. Kan je een Kind Veganistisch Opvoeden? Available online: https://www.voedingscentrum.nl/nl/service/vraag-en-antwoord/kinderen-en-jongeren/kan-je-een-kind-veganistisch-opvoeden-.aspx (accessed on 14 August 2023).
- Alexy, U.; Fischer, M.; Weder, S.; Längler, A.; Michalsen, A.; Sputtek, A.; Keller, M. Nutrient Intake and Status of German Children and Adolescents Consuming Vegetarian, Vegan or Omnivore Diets: Results of the VeChi Youth Study. Nutrients 2021, 13, 1707. [Google Scholar] [CrossRef] [PubMed]
- Ambroszkiewicz, J.; Laskowska-Klita, T.; Klemarczyk, W. Low levels of osteocalcin and leptin in serum of vegetarian prepubertal children. Med. Wieku Rozwoj. 2003, 7 Pt 2, 587–591. [Google Scholar] [PubMed]
- Ambroszkiewicz, J.; Laskowska-Klita, T.; Klemarczyk, W. Low serum leptin concentration in vegetarian prepubertal children. Rocz. Akad. Med. Bialymst. 2004, 49, 103–105. [Google Scholar] [PubMed]
- Ambroszkiewicz, J.; Klemarczyk, W.; Chełchowska, M.; Gajewska, J.; Laskowska-Klita, T. Serum homocysteine, folate, vitamin B12 and total antioxidant status in vegetarian children. Adv. Med. Sci. 2006, 51, 265–268. [Google Scholar]
- Ambroszkiewicz, J.; Chełchowska, M.; Rowicka, G.; Klemarczyk, W.; Strucińska, M.; Gajewska, J. Anti-Inflammatory and Pro-Inflammatory Adipokine Profiles in Children on Vegetarian and Omnivorous Diets. Nutrients 2018, 10, 1241. [Google Scholar] [CrossRef]
- Světnička, M.; Sigal, A.; Selinger, E.; Heniková, M.; El-Lababidi, E.; Gojda, J. Cross-Sectional Study of the Prevalence of Cobalamin Deficiency and Vitamin B12 Supplementation Habits among Vegetarian and Vegan Children in the Czech Republic. Nutrients 2022, 14, 535. [Google Scholar] [CrossRef] [PubMed]
- Yen, C.-E.; Yen, C.-H.; Cheng, C.-H.; Huang, Y.-C. Vitamin B-12 status is not associated with plasma homocysteine in parents and their preschool children: Lacto-ovo, lacto, and ovo vegetarians and omnivores. J. Am. Coll. Nutr. 2010, 29, 7–13. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | Number of Studies (n) |
|---|---|
| Young children (2–5 y) | 15 |
| School children (6–12 y) | 24 |
| Adolescents (13–18 y) | 11 |
| Meat-eating | 27 |
| Vegetarian | 26 |
| Vegan | 7 |
| Semi-vegetarian | 3 |
| Europe | 19 (mostly Poland) |
| Asia | 5 (mostly India) |
| North America | 2 (US, Canada) |
| Oceania | 3 (New Zealand, Australia) |
| Africa | 1 (Ghana) |
| Nutrient intake, assessed from foods alone | 14 |
| Nutrient intake, assessed from foods and supplements | 8 |
| Nutrient status in users and non-users of supplements | 20 |
| Nutrient status in non-users of supplements only | 3 |
| Dietary Pattern | Nutrients at Risk of Inadequacy * | Nutrients of Favorably High Intake |
|---|---|---|
| Vegans | Vitamin B12, vitamin D | PUFA, fiber |
| Calcium, iron, zinc | Vitamin C, vitamin E, folate | |
| Vegetarians | SAFA, PUFA **, fiber | |
| Vitamin B12, vitamin D | Vitamin E, folate | |
| Calcium, iron, zinc | ||
| Meat eaters | SAFA, PUFA, fiber | Vitamin B12 |
| Vitamin D, vitamin E, folate | Zinc | |
| Calcium |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neufingerl, N.; Eilander, A. Nutrient Intake and Status in Children and Adolescents Consuming Plant-Based Diets Compared to Meat-Eaters: A Systematic Review. Nutrients 2023, 15, 4341. https://doi.org/10.3390/nu15204341
Neufingerl N, Eilander A. Nutrient Intake and Status in Children and Adolescents Consuming Plant-Based Diets Compared to Meat-Eaters: A Systematic Review. Nutrients. 2023; 15(20):4341. https://doi.org/10.3390/nu15204341
Chicago/Turabian StyleNeufingerl, Nicole, and Ans Eilander. 2023. "Nutrient Intake and Status in Children and Adolescents Consuming Plant-Based Diets Compared to Meat-Eaters: A Systematic Review" Nutrients 15, no. 20: 4341. https://doi.org/10.3390/nu15204341
APA StyleNeufingerl, N., & Eilander, A. (2023). Nutrient Intake and Status in Children and Adolescents Consuming Plant-Based Diets Compared to Meat-Eaters: A Systematic Review. Nutrients, 15(20), 4341. https://doi.org/10.3390/nu15204341






