Association of Mediterranean Diet Adherence with Sociodemographic, Anthropometric, and Lifestyle Factors during the COVID-19 Pandemic: A Cross-Sectional Study in Greece
Abstract
:1. Introduction
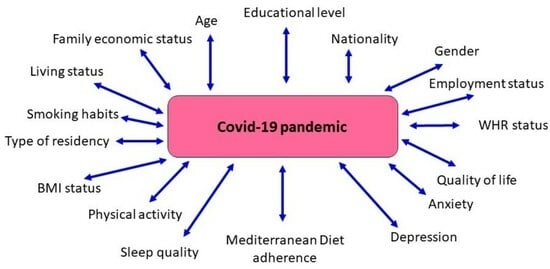
2. Materials and Methods
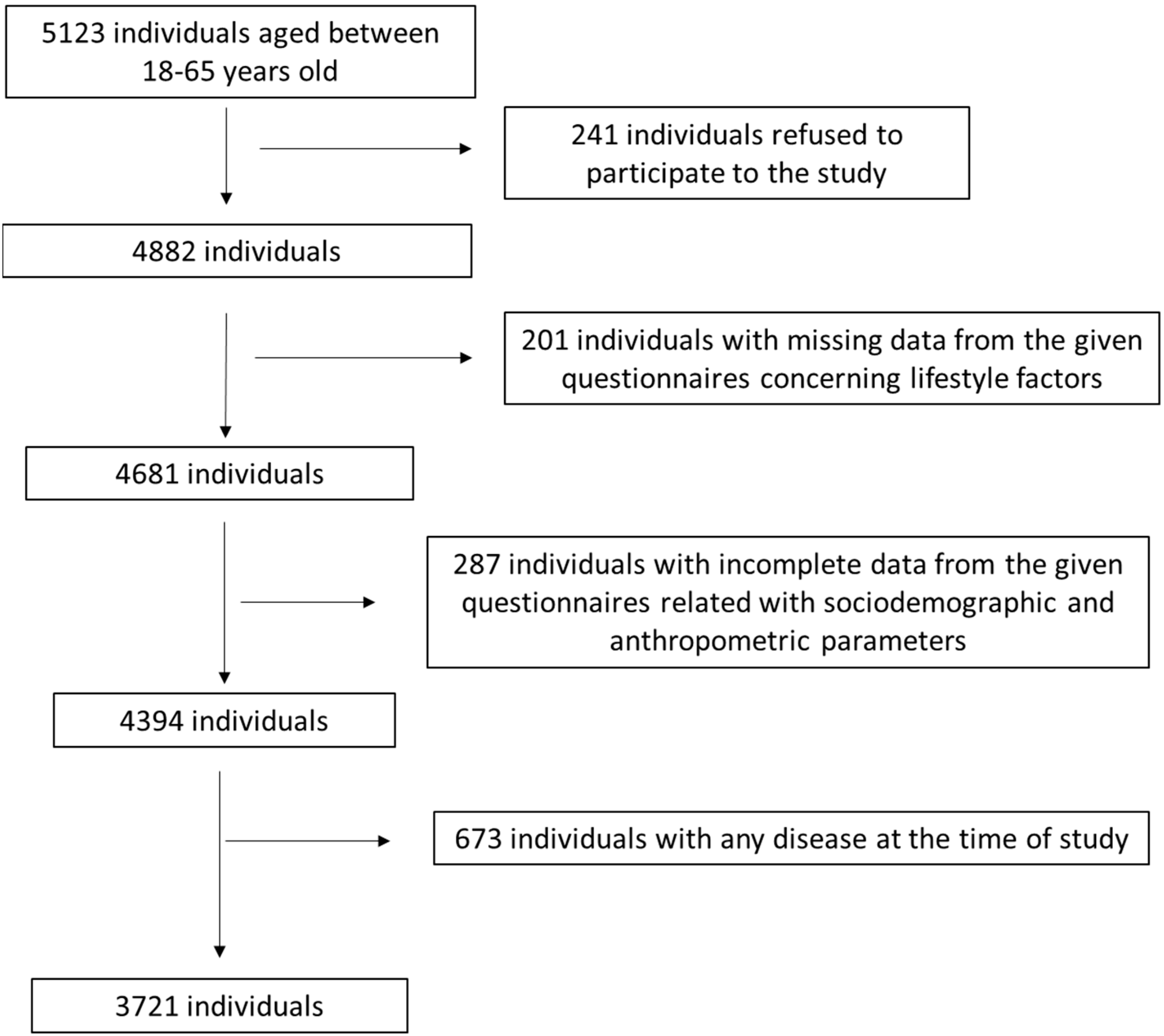
2.1. Study Population
2.2. Study Design
2.3. Statistical Analysis
3. Results
3.1. Sociodemographic and Anthropometric Characteristics of the Study Population
3.2. Lifestyle Factors of the Study Population
3.3. Association of MD Adherence with Sociodemographic and Anthropometric Characteristics of the Study Population
3.4. Association of MD Adherence with Lifestyle Factors of the Study Population
3.5. Multivariate Analysis for MD Adherence with Adjustment for Multiple Confounding Factors
3.6. Interrelationships between Sociodemographic, Anthropometric, and Lifestyle Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Almubarak, S.H.; Alsaif, A.K.; Almulla, S.J.; Alfayez, A.S.; Alnujaidi, H.Y.; Alsalman, D.M. Teleworking during COVID-19: Ex-periences from Saudi Arabia. Ind. Health 2023, 61, 291–303. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Cano, H.J.; Moreno-Murguía, M.B.; Morales-López, O.; Crow-Buchanan, O.; English, J.A.; Lozano-Alcázar, J.; Somilleda-Ventura, S.A. Anxiety, depression, and stress in response to the coronavirus disease-19 pandemic. Cir. Cir. 2020, 88, 562–568. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Aranda, F.; Casas, M.; Claes, L.; Bryan, D.C.; Favaro, A.; Granero, R.; Gudiol, C.; Jiménez-Murcia, S.; Karwautz, A.; Le Grange, D.; et al. COVID-19 and implications for eating disorders. Eur. Eat. Disord. Rev. 2020, 28, 239–245. [Google Scholar] [CrossRef]
- De Hert, M.; Mazereel, V.; Detraux, J.; Van Assche, K. Prioritizing COVID-19 vaccination for people with severe mental illness. World Psychiatry 2021, 20, 54–55. [Google Scholar] [CrossRef]
- Sideli, L.; Lo Coco, G.; Bonfanti, R.C.; Borsarini, B.; Fortunato, L.; Sechi, C.; Micali, N. Effects of COVID-19 lockdown on eating disorders and obesity: A systematic review and meta-analysis. Eur. Eat. Disord. Rev. 2021, 29, 826–841. [Google Scholar] [CrossRef]
- Wang, Y.; Di, Y.; Ye, J.; Wei, W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 2021, 26, 13–22. [Google Scholar] [CrossRef]
- Machado, P.P.P.; Pinto-Bastos, A.; Ramos, R.; Rodrigues, T.F.; Louro, E.; Gonçalves, S.; Brandão, I.; Va, A. Impact of COVID-19 lockdown measures on a cohort of eating disorders patients. J. Eat. Disord. 2020, 8, 57. [Google Scholar] [CrossRef]
- Galea, S.; Merchant, R.M.; Lurie, N. The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention. JAMA Intern. Med. 2020, 180, 817–818. [Google Scholar] [CrossRef]
- Ferrante, G.; Camussi, E.; Piccinelli, C.; Senore, C.; Armaroli, P.; Ortale, A.; Garena, F.; Giordano, L. Did social isolation during the SARS-CoV-2 epidemic have an impact on the lifestyles of citizens? Epidemiol. Prev. 2020, 44, 353–362. [Google Scholar] [CrossRef]
- Mrityunjaya, M.; Pavithra, V.; Neelam, R.; Janhavi, P.; Halami, P.M.; Ravindra, P.V. Immune-Boosting, Antioxidant and Anti-Inflammatory Food Supplements Targeting Pathogenesis of COVID-19. Front. Immunol. 2020, 11, 570122. [Google Scholar] [CrossRef]
- Lordan, R.; Rando, H.M.; Greene, C.S. Dietary Supplements and Nutraceuticals under Investigation for Covid-19 Prevention and Treatment. Msystems 2021, 6, e00122-21. [Google Scholar] [CrossRef] [PubMed]
- Mortaz, E.; Bezemer, G.; Alipoor, S.D.; Varahram, M.; Mumby, S.; Folkerts, G.; Garssen, J.; Adcock, I.M. Nutritional Impact and Its Potential Consequences on Covid-19 Severity. Front. Nutr. 2021, 8, 698617. [Google Scholar] [CrossRef] [PubMed]
- Paces, J.; Strizova, Z.; Smrz, D.; Cerny, J. COVID-19 and the Immune System. Physiol. Res. 2020, 69, 379–388. [Google Scholar] [CrossRef] [PubMed]
- Tyrovolas, S.; Giné-Vázquez, I.; Fernández, D.; Morena, M.; Koyanagi, A.; Janko, M.; Haro, J.M.; Lin, Y.; Lee, P.; Pan, W.; et al. Estimating the COVID-19 Spread through Real-Time Population Mobility Patterns: Surveillance in Low- and Middle-Income Countries. J. Med. Internet Res. 2021, 23, e22999. [Google Scholar] [CrossRef]
- Beigmohammadi, M.T.; Bitarafan, S.; Hoseindokht, A.; Abdollahi, A.; Amoozadeh, L.; Soltani, D. The effect of supplementation with vitamins A, B, C, D, and E on disease severity and inflammatory responses in patients with COVID-19: A randomized clinical trial. Trials 2021, 22, 802. [Google Scholar] [CrossRef]
- Karonova, T.L.; Chernikova, A.T.; Golovatyuk, K.A.; Bykova, E.S.; Grant, W.B.; Kalinina, O.V.; Grineva, E.N.; Shlyakhto, E.V. Vitamin D Intake May Reduce SARS-CoV-2 Infection Morbidity in Health Care Workers. Nutrients 2022, 14, 505. [Google Scholar] [CrossRef]
- Shakoor, H.; Feehan, J.; Al Dhaheri, A.S.; Ali, H.I.; Platat, C.; Ismail, L.C.; Apostolopoulos, V.; Stojanovska, L. Immune-Boosting Role of Vitamins D, C, E, Zinc, Selenium and Omega-3 Fatty Acids: Could They Help against Covid-19? Maturitas 2021, 143, 1–9. [Google Scholar] [CrossRef]
- Majidi, N.; Rabbani, F.; Gholami, S.; Gholamalizadeh, M.; BourBour, F.; Rastgoo, S.; Hajipour, A.; Shadnoosh, M.; Akbari, M.E.; Bahar, B.; et al. The Effect of Vitamin C on Pathological Pa-rameters and Survival Duration of Critically Ill Coronavirus Disease 2019 Patients: A Randomized Clinical Trial. Front. Immunol. 2021, 12, 717816. [Google Scholar] [CrossRef]
- Ghelani, D.; Alesi, S.; Mousa, A. Vitamin D and COVID-19: An Overview of Recent Evidence. Int. J. Mol. Sci. 2021, 22, 10559. [Google Scholar] [CrossRef]
- Rastogi, A.; Bhansali, A.; Khare, N.; Suri, V.; Yaddanapudi, N.; Sachdeva, N.; Puri, G.D.; Malhotra, P. Short term, high-dose vita-min D supplementation for COVID-19 disease: A randomised, placebo-controlled, study (SHADE study). Postgrad Med. J. 2022, 98, 87–90. [Google Scholar] [CrossRef]
- Cutolo, M.; Paolino, S.; Sulli, A.; Smith, V.; Pizzorni, C.; Seriolo, B. Vitamin D, steroid hormones, and autoimmunity. Ann. N. Y. Acad. Sci. 2014, 1317, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Sulli, A.; Gotelli, E.; Casabella, A.; Paolino, S.; Pizzorni, C.; Alessandri, E.; Grosso, M.; Ferone, D.; Smith, V.; Cutolo, M. Vitamin D and Lung Outcomes in Elderly COVID-19 Patients. Nutrients 2021, 13, 717. [Google Scholar] [CrossRef] [PubMed]
- Cutolo, M.; Smith, V.; Paolino, S.; Gotelli, E. Involvement of the secosteroid vitamin D in autoimmune rheumatic diseases and COVID-19. Nat. Rev. Rheumatol. 2023, 19, 265–287. [Google Scholar] [CrossRef] [PubMed]
- Sedighiyan, M.; Abdollahi, H.; Karimi, E.; Badeli, M.; Erfanian, R.; Raeesi, S.; Hashemi, R.; Vahabi, Z.; Asanjarani, B.; Mansouri, F.; et al. Omega-3 polyunsaturated fatty acid supplementation improve clinical symptoms in patients with 64 Covid-19: A randomized clinical trial. Int. J. Clin. Pract. 2021, 75, e14854. [Google Scholar] [CrossRef]
- Gutiérrez-Castrellón, P.; Gandara-Martí, T.; Abreu, A.T.Y.; Nieto-Rufino, C.D.; López-Orduña, E.; Jiménez-Escobar, I.; Jimé-nez-Gutiérrez, C.; López-Velazquez, G.; Espadaler-Mazo, J. Probiotic improves symptomatic and viral clearance in Covid19 outpa-tients: A randomized, quadruple-blinded, placebo-controlled trial. Gut Microbes 2022, 14, 2018899. [Google Scholar] [CrossRef]
- Brahma, S.; Naik, A.; Lordan, R. Probiotics: A gut response to the COVID-19 pandemic but what does the evidence show? Clin. Nutr. ESPEN 2022, 51, 17–27. [Google Scholar] [CrossRef]
- Yang, J.; Li, X.; He, T.; Ju, F.; Qiu, Y.; Tian, Z. Impact of Physical Activity on COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 14108. [Google Scholar] [CrossRef]
- Kiani, A.K.; Medori, M.C.; Bonetti, G.; Aquilanti, B.; Velluti, V.; Matera, G.; Iaconelli, A.; Stuppia, L.; Connelly, S.T.; Herbst, K.L.; et al. Modern vision of the Mediterranean diet. J. Prev. Med. Hyg. 2022, 63, E36–E43. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Morze, J.; Hoffmann, G. Mediterranean diet and health status: Active ingredients and pharmacological mechanisms. Br. J. Pharmacol. 2020, 177, 1241–1257. [Google Scholar] [CrossRef]
- Andreo-López, M.C.; Contreras-Bolívar, V.; Muñoz-Torres, M.; García-Fontana, B.; García-Fontana, C. Influence of the Mediterranean Diet on Healthy Aging. Int. J. Mol. Sci. 2023, 24, 4491. [Google Scholar] [CrossRef]
- Vetrani, C.; Piscitelli, P.; Muscogiuri, G.; Barrea, L.; Laudisio, D.; Graziadio, C.; Marino, F.; Colao, A. “Planeterranea”: An attempt to broaden the beneficial effects of the Mediterranean diet worldwide. Front. Nutr. 2022, 9, 973757. [Google Scholar] [CrossRef] [PubMed]
- Finicelli, M.; Di Salle, A.; Galderisi, U.; Peluso, G. The Mediterranean Diet: An Update of the Clinical Trials. Nutrients 2022, 14, 2956. [Google Scholar] [CrossRef] [PubMed]
- Farrugia, F.; Refalo, D.; Bonello, D.; Cuschieri, S. The impact of the COVID-19 pandemic on Mediterranean diet adherence: A narrative systematic review. Nutr. Health 2023, 2601060231187511. [Google Scholar] [CrossRef] [PubMed]
- Ferro, Y.; Pujia, R.; Maurotti, S.; Boragina, G.; Mirarchi, A.; Gnagnarella, P.; Mazza, E. Mediterranean Diet a Potential Strategy against SARS-CoV-2 Infection: A Narrative Review. Medicina 2021, 57, 1389. [Google Scholar] [CrossRef]
- Ponzo, V.; Pellegrini, M.; D’eusebio, C.; Bioletto, F.; Goitre, I.; Buscemi, S.; Bo, S. Mediterranean diet and sars-cov-2 infection: Is there any association? A proof-of-concept study. Nutrients 2021, 13, 1721. [Google Scholar] [CrossRef]
- Perez-Araluce, R.; Martinez-Gonzalez, M.A.; Fernández-Lázaro, C.I.; Bes-Rastrollo, M.; Gea, A.; Carlos, S. Mediterranean diet and the risk of COVID-19 in the ‘Seguimiento Universidad de Navarra’ cohort. Clin. Nutr. 2022, 41, 3061–3068. [Google Scholar] [CrossRef]
- Izzo, L.; Santonastaso, A.; Cotticelli, G.; Federico, A.; Pacifico, S.; Castaldo, L.; Colao, A.; Ritieni, A. An Italian Survey on Dietary Habits and Changes during the COVID-19 Lockdown. Nutrients 2021, 13, 1197. [Google Scholar] [CrossRef]
- Mantzorou, M.; Mentzelou, M.; Vasios, G.K.; Kontogiorgis, C.; Antasouras, G.; Vadikolias, K.; Psara, E.; Vorvolakos, T.; Poulios, E.; Serdari, A.; et al. Mediterranean Diet Adherence Is Associated with Favorable Health-Related Quality of Life, Physical Activity, and Sleep Quality in a Community-Dwelling Greek Older Population. Antioxidants 2023, 12, 983. [Google Scholar] [CrossRef]
- Mantzorou, M.; Vadikolias, K.; Pavlidou, E.; Tryfonos, C.; Vasios, G.; Serdari, A.; Giaginis, C. Mediterranean diet adherence is associated with better cognitive status and less depressive symptoms in a Greek elderly population. Aging Clin. Exp. Res. 2021, 33, 1033–1040. [Google Scholar] [CrossRef]
- World Health Organization. The World Health Report: 2006: Working Together for Health; World Health Organization: Geneva, Switzerland, 2006; Available online: https://apps.who.int/iris/handle/10665/43432 (accessed on 18 July 2023).
- Jamesm, W.P. WHO recognition of the global obesity epidemic. Int. J. Obes. 2008, 32, S120–S1266. [Google Scholar] [CrossRef]
- World Health Organization. Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation, Geneva, 8–11 December; World Health Organization: Geneva, Switzerland, 2011; Available online: https://apps.who.int/iris/handle/10665/44583 (accessed on 18 July 2023).
- Ahmad, N.; Adam, S.I.M.; Nawi, A.M.; Hassan, M.R.; Ghazi, H.F. Abdominal Obesity Indicators: Waist Circumference or Waist-to-hip Ratio in Malaysian Adults Population. Int. J. Prev. Med. 2016, 7, 82. [Google Scholar] [CrossRef] [PubMed]
- Bener, A.; Yousafzai, M.T.; Darwish, S.; Al-Hamaq, A.O.; Nasralla, E.A.; Abdul-Ghani, M. Obesity index that better predict met-abolic syndrome: Body mass index, waist circumference, waist hip ratio, or waist height ratio. J Obes. 2013, 2013, 269038. [Google Scholar] [CrossRef] [PubMed]
- Yanga, F.; Lv, J.H.; Lei, S.F.; Chena, X.D. Receiver-operating characteristic analyses of body mass index, waist circumference and waist-to-hip ratio for obesity: Screening in young adults in central south of China. Clin. Nut. 2006, 25, 1030–1039. [Google Scholar] [CrossRef]
- Cheng, C.H.; Ho, C.C.; Yang, C.F.; Huang, Y.C.; Lai, C.H.; Liaw, Y.P. Waist-to-hip ratio is a better anthropometric index than body mass index for predicting the risk of type 2 diabetes in Taiwanese population. Nutr. Res. 2010, 30, 585–593. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sport. Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Salahuddin, M.; Maru, T.T.; Kumalo, A.; Pandi-Perumal, S.R.; Bahammam, A.S.; Manzar, M.D. Validation of the Pittsburgh sleep quality index in community dwelling Ethiopian adults. Health Qual. Life Outcomes 2017, 15, 58. [Google Scholar] [CrossRef]
- Kalfoss, M.H.; Reidunsdatter, R.J.; Klöckner, C.A.; Nilsen, M. Validation of the WHOQOL-Bref: Psychometric properties and normative data for the Norwegian general population. Health Qual. Life Outcomes 2021, 19, 13. [Google Scholar] [CrossRef]
- Tluczek, A.; Henriques, J.B.; Brown, R.L. Support for the reliability and validity of a six-item state anxiety scale derived from the State-Trait Anxiety Inventory. J. Nurs. Meas. 2009, 17, 19–28. [Google Scholar] [CrossRef]
- Wang, Y.-P. Clarice Gorenstein. Psychometric properties of the Beck Depression Inventory-II: A comprehensive review. Rev. Bras. Psiquiatr. 2013, 35, 416–431. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Pitsavos, C.; Stefanadis, C. Dietary patterns: A Mediterranean diet score and its relation to clinical and bio-logical markers of cardiovascular disease risk. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 559–568. [Google Scholar] [CrossRef]
- Arvaniti, F.; Panagiotakos, D.B. Healthy indexes in public health practice and research: A review. Crit. Rev. Food Sci. Nutr. 2008, 48, 317–327. [Google Scholar] [CrossRef]
- Diamantis, D.V.; Karatzi, K.; Kantaras, P.; Liatis, S.; Iotova, V.; Bazdraska, T.; Tankova, T.; Greet Cardon, G.; Wikström, K.; Rurik, I.; et al. Prevalence and Socioeconomic Correlates of Adult Obesity in Europe: The Feel4Diabetes Study. Int. J. Environ. Res. Public Health 2022, 19, 12572. [Google Scholar] [CrossRef] [PubMed]
- Melpo Kapetanstrataki, M.; Anna Tzortzi, A.; Vaso Evangelopoulou, V.; Behrakis, P. Profiling smokers in Greece in 2020. Tob. Pre. Cessat. 2021, 7, 10. [Google Scholar] [CrossRef]
- Psarrou, A.; Adamakidou, T.; Apostolara, P.; Koreli, A.; Drakopoulou, M.; Plakas, S.; Mastrogiannis, D.; Mantoudi, A.; Parissopoulos, S.; Zartaloudi, A.; et al. Associations between Physical Activity and Health-Related Quality of Life among Community-Dwelling Older Adults: A Cross-Sectional Study in Urban Greece. Geriatrics 2023, 8, 61. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulou, A.; Efstathiou, V.; Yotsidi, V.; Pomini, V.; Michopoulos, I.; Markopoulou, E.; Papadopoulou, M.; Tsigkaropoulou, E.; Kalemi, G.; Tournikioti, K.; et al. Suicidal ideation during COVID-19 lockdown in Greece: Prevalence in the community, risk and protective factors. Psychiatry Res. 2021, 297, 113713. [Google Scholar] [CrossRef]
- Gournellis, R.; Efstathiou, V. The impact of the COVID-19 Pandemic on the Greek population: Suicidal ideation during the first and second lockdown. Psychiatriki 2021, 32, 267–270. [Google Scholar] [CrossRef] [PubMed]
- Health at a Glance: Europe 2020 State of Health in the EU Cycle. Available online: https://ec.europa.eu/health/system/files/2020-12/2020_healthatglance_rep_en_0.pd (accessed on 22 June 2023).
- Sikaras, C.; Zyga, S.; Tsironi, M.; Tselebis, A.; Pachi, A.; Ilias, I.; Panagiotou, A. The Mediating Role of Depression and of State Anxiety οn the Relationship between Trait Anxiety and Fatigue in Nurses during the Pandemic Crisis. Healthcare 2023, 11, 367. [Google Scholar] [CrossRef]
- Labrague, L.J. Pandemic fatigue and clinical nurses’ mental health, sleep quality and job contentment during the COVID-19 pandemic: The mediating role of resilience. J. Nurs. Manag. 2021, 29, 1992–2001. [Google Scholar] [CrossRef]
- Sasangohar, F.; Jones, S.L.; Masud, F.N.; Vahidy, F.S.; Kash, B.A. Provider Burnout and Fatigue During the COVID-19 Pandemic: Lessons Learned from a High-Volume Intensive Care Unit. Obstet. Anesthesia Dig. 2020, 131, 106–111. [Google Scholar] [CrossRef]
- Milton-Laskibar, I.; Trepiana, J.; Macarulla, M.T.; Gómez-Zorita, S.; Arellano-García, L.; Fernández-Quintela, A.; Portillo, M.P. Potential usefulness of Mediterranean diet polyphenols against COVID-19-induced inflammation: A review of the current knowledge. J. Physiol. Biochem. 2023, 79, 371–382. [Google Scholar] [CrossRef]
- Drake, I.; Sonestedt, E.; Ericson, U.; Wallström, P.; Orho-Melander, M. A western dietary pattern is prospectively associated with cardio-metabolic traits and incidence of the metabolic syndrome. Br. J. Nutr. 2018, 119, 1168–1176. [Google Scholar] [CrossRef] [PubMed]
- Port, J.R.; Adney, D.R.; Schwarz, B.; Schulz, J.E.; Sturdevant, D.E.; Smith, B.J.; Avanzato, V.A.; Holbrook, M.G.; Purushotham, J.N.; Stromberg, K.A.; et al. High-Fat high-sugar diet-induced changes in the lipid metabolism are associated with mildly increased COVID-19 severity and delayed recovery in the Syrian hamster. Viruses 2021, 13, 2506. [Google Scholar] [CrossRef] [PubMed]
- Greene, M.W.; Roberts, A.P.; Frugé, A.D. Negative association between Mediterranean diet adherence and COVID-19 cases and related deaths in Spain and 23 OECD countries: An ecological study. Front. Nutr. 2021, 8, 591964. [Google Scholar] [CrossRef] [PubMed]
- Maté-Muñoz, J.L.; Hernández-Lougedo, J.; Ruiz-Tovar, J.; Olivares-Llorente, R.; García-Fernández, P.; Zapata, I. Physical Activity Levels, Eating Habits, and Well-Being Measures in Students of Healthcare Degrees in the Second Year of the COVID-19 Pandemic. Healthcare 2023, 11, 1570. [Google Scholar] [CrossRef]
- Catucci, A.; Scognamiglio, U.; Rossi, L. Lifestyle Changes Related to Eating Habits, Physical Activity, and Weight Status During COVID-19 Quarantine in Italy and Some European Countries. Front. Nutr. 2021, 8, 718877. [Google Scholar] [CrossRef]
- Sharma, S.; Di Castelnuovo, A.; Costanzo, S.; Persichillo, M.; Panzera, T.; Ruggiero, E.; De Curtis, A.; Storto, M.; Cavallo, P.; Gianfagna, F.; et al. Habitual adherence to a traditional Mediterranean diet and risk of SARS-CoV-2 infection and Coronavirus disease 2019 (COVID-19): A longitudinal analysis. Int. J. Food Sci. Nutr. 2023, 74, 382–394. [Google Scholar] [CrossRef]
- Alhouri, A.; Shokor, M.A.; Marwa, K.; Sharabi, A.; Arrouk, D.M.N.; Al Houri, F.N.; Al Houri, H. COVID-19 and Its Impact on Healthcare Workers: Understanding Stigma, Stress, and Quality of Life. Cureus 2023, 15, e37846. [Google Scholar] [CrossRef]
- Turki, S.; Bouzekri, K.; Trabelsi, T.; El Ati, J. Assessment of Mediterranean Diet Adherence and Lifestyle Change during COVID-19 National Lockdown in Tunisian Adult Population. Nutrients 2022, 14, 4151. [Google Scholar] [CrossRef]
- Si, T.L.; Chen, P.; Zhang, L.; Sha, S.; Lam, M.I.; Lok, K.I.; Chow, I.H.I.; Li, J.X.; Wang, Y.Y.; Su, Z.; et al. Depression and quality of life among Macau residents in the 2022 COVID-19 pandemic wave from the perspective of network analysis. Front. Psychol. 2023, 14, 1164232. [Google Scholar] [CrossRef]
- Chen, P.; Zhang, L.; Sha, S.; Lam, M.I.; Lok, K.I.; Chow, I.H.I.; Si, T.L.; Su, Z.; Cheung, T.; Feng, Y.; et al. Prevalence of insomnia and its association with quality of life among Macau residents shortly after the summer 2022 COVID-19 outbreak: A network analysis perspective. Front. Psychiatry 2023, 14, 1113122. [Google Scholar] [CrossRef]
- Díaz, G.; Hernández, S.; Crespo, A.; Renghea, A.; Yébenes, H.; Iglesias-López, M.T. Macronutrient Intake, Sleep Quality, Anxiety, Adherence to a Mediterranean Diet and Emotional Eating among Female Health Science Undergraduate Students. Nutrients 2023, 15, 2882. [Google Scholar] [CrossRef] [PubMed]
- Mieziene, B.; Burkaite, G.; Emeljanovas, A.; Tilindiene, I.; Novak, D.; Kawachi, I. Adherence to Mediterranean diet among Lithuanian and Croatian students during COVID-19 pandemic and its health behavior correlates. Front. Public Health 2022, 10, 1000161. [Google Scholar] [CrossRef] [PubMed]
- Boaz, M.; Navarro, D.A.; Raz, O.; Kaufman-Shriqui, V. Dietary Changes and Anxiety during the Coronavirus Pandemic: Differences between the Sexes. Nutrients 2021, 13, 4193. [Google Scholar] [CrossRef] [PubMed]
- Bonaccio, M.; Costanzo, S.; Bracone, F.; Gialluisi, A.; Di Castelnuovo, A.; Ruggiero, E.; Esposito, S.; Olivieri, M.; Persichillo, M.; Cerletti, C.; et al. Psychological distress resulting from the COVID-19 confinement is associated with unhealthy dietary changes in two Italian population-based cohorts. Eur. J. Nutr. 2022, 61, 1491–1505. [Google Scholar] [CrossRef]
- Lorenzoni, G.; Azzolina, D.; Maresio, E.; Gallipoli, S.; Ghidina, M.; Baldas, S.; Berchialla, P.; Giron, M.C.; Silano, M.; Gregori, D.; et al. Impact of the COVID-19 lockdown on psychological health and nutritional habits in Italy: Results from the #PRESTOinsieme study. BMJ Open 2022, 12, e048916. [Google Scholar] [CrossRef]
- Kaufman-Shriqui, V.; Navarro, D.A.; Raz, O.; Boaz, M. Dietary changes and anxiety during the coronavirus pandemic: A multinational survey. Eur. J. Clin. Nutr. 2022, 76, 84–92. [Google Scholar] [CrossRef]
- Marcos-Pardo, P.J.; Abelleira-Lamela, T.; Vaquero-Cristobal, R.; González-Gálvez, N. Changes in life satisfaction, depression, general health and sleep quality of Spanish older women during COVID-19 lockdown and their relationship with lifestyle: An observational follow-up study. BMJ Open 2022, 12, e061993. [Google Scholar] [CrossRef]
- Matta, J.; Robineau, O.; Wiernik, E.; Carrat, F.; Severi, G.; Touvier, M.; Gouraud, C.; Ouazana Vedrines, C.; Pitron, V.; Ranque, B.; et al. Depression and anxiety before and at the beginning of the COVID-19 pandemic and incident persistent symptoms: A prospective population-based cohort study. Mol. Psychiatry, 2023; online ahead of print. [Google Scholar] [CrossRef]
- Roy, N.; Amin, M.B.; Mamun, M.A.; Sarker, B.; Hossain, E.; Aktarujjaman, M. Prevalence and factors associated with depression, anxiety, and stress among people with disabilities during COVID-19 pandemic in Bangladesh: A cross-sectional study. PLoS ONE 2023, 18, e0288322. [Google Scholar] [CrossRef]
- Stival, C.; Lugo, A.; Odone, A.; van den Brandt, P.A.; Fernandez, E.; Tigova, O.; Soriano, J.B.; López, M.J.; Scaglioni, S.; Gallus, S.; et al. Prevalence and Correlates of Overweight and Obesity in 12 European Countries in 2017–2018. Obes. Facts 2022, 15, 655–665. [Google Scholar] [CrossRef]
- Calina, D.; Hartung, T.; Mardare, I.; Mitroi, M.; Poulas, K.; Tsatsakis, A.; Rogoveanu, I.; Docea, A.O. COVID-19 pandemic and alcohol consumption: Impacts and interconnections. Toxicol. Rep. 2021, 8, 529–535. [Google Scholar] [CrossRef]
- Friske, M.M.; Spanagel, R. Chronic alcohol consumption and COVID-19 infection risk: A narrative review. Alcohol. Clin. Exp. Res. 2023, 47, 629–639. [Google Scholar] [CrossRef] [PubMed]
| Parameters (n = 3721) | Descriptive Statistics |
|---|---|
| Age (mean ± SD; years) | 37.6 ± 5.8 |
| Gender (n, %) | |
| Male | 1841 (49.5%) |
| Female | 1880 (50.5%) |
| Education level (mean ± SD; years) | 12.2 ± 2.8 |
| Family financial status (n, %) | |
| Low | 2664 (71.6%) |
| Medium | 693 (18.6%) |
| High | 364 (9.8%) |
| Nationality (n, %) | |
| Greek | 3189 (85.7%) |
| Other | 531 (14.3%) |
| Living status (n, %) | |
| Living with others | 2720 (73.1%) |
| Living alone | 1001 (26.9%) |
| Employment (n, %) | |
| Employed | 3006 (80.8%) |
| Unemployed | 715 (19.2%) |
| Smoking habits (n, %) | |
| Non-smokers | 2612 (70.2%) |
| Smokers | 1109 (29.8%) |
| Type of residency(n, %) | |
| Urban | 2789 (74.9%) |
| Rural | 932 (25.1%) |
| BMI status (n, %) | |
| Normal weight | 2437 (65.5%) |
| Overweight | 792 (21.3%) |
| Obese | 492 (13.2%) |
| WHR (n, %) | |
| Low | 2387 (64.2%) |
| Moderate | 854 (22.9%) |
| High | 480 (12.9%) |
| Physical activity levels (n, %) | |
| Low | 2186 (58.7%) |
| Moderate | 859 (23.1%) |
| High | 676 (18.2%) |
| Sleep quality (n, %) | |
| Adequate | 2595 (69.7%) |
| Inadequate | 1126 (30.3%) |
| Quality of life (n, %) | |
| Below mean value | 1872 (50.3%) |
| Over mean value | 1849 (49.7%) |
| Anxiety (n, %) | |
| No | 2731 (73.4%) |
| Yes | 990 (26.6%) |
| Depression (n, %) | |
| No | 2482 (66.7%) |
| Yes | 1239 (33.3%) |
| Mediterranean Diet adherence (n, %) | |
| Very low | 927 (24.9%) |
| Low | 932 (25.1%) |
| Moderate | 931 (25.0%) |
| High | 931 (25.0%) |
| Characteristics (n = 3721) | Mediterranean Diet Adherence | ||||
|---|---|---|---|---|---|
| Very Low | Low | Moderate | High | p-Value | |
| Age (mean ± SD; years) | 37.5 ± 9.1 | 37.2 ± 8.8 | 37.9 ± 8.5 | 37.6 ± 8.0 | p = 0.3857 |
| Gender (n, %) | |||||
| Male | 499 (53.8%) | 638 (68.5%) | 355 (38.1%) | 348 (37.4%) | p = 0.0001 |
| Female | 428 (46.2%) | 294 (31.5%) | 576 (61.9%) | 583 (62.6%) | |
| Education level (mean ± SD; years) | 12.8 ± 4.5 | 12.7 ± 4.3 | 13.1 ± 4.8 | 13.3 ± 5.1 | p = 0.0538 |
| Family financial status (n, %) | p = 0.0002 | ||||
| Low | 704 (75.9%) | 689 (73.9%) | 724 (77.8%) | 547 (58.7%) | |
| Medium | 187 (29.2%) | 206 (22.1%) | 168 (18.0%) | 132 (14.2%) | |
| High | 36 (3.9%) | 37 (4.0%) | 39 (4.2%) | 252 (27.1%) | |
| Nationality (n, %) | p = 0.4538 | ||||
| Greek | 794 (85.6) | 789 (84.7%) | 811 (87.2%) | 795 (85.4%) | |
| Other | 133 (14.4%) | 143 (15.3%) | 119 (12.8%) | 136 (14.6%) | |
| Living status (n, %) | p = 0.0184 | ||||
| Living with others | 657 (70.9%) | 711 (76.3%) | 643 (69.1%) | 709 (76.2%) | |
| Living alone | 270 (29.1) | 221 (23.7%) | 288 (30.9%) | 222 (23.8%) | |
| Employment (n, %) | p = 0.0894 | ||||
| Employed | 730 (78.7%) | 764 (82.0%) | 747 (80.2%) | 765 (82.2%) | |
| Unemployed | 197 (21.3%) | 168 (18.0%) | 184 (19.8%) | 166 (17.8%) | |
| Smoking habits (n, %) | p = 0.0001 | ||||
| Non-smokers | 593 (64.0%) | 528 (56.7%) | 723 (77.7%) | 768 (82.5%) | |
| Smokers | 334 (36.0%) | 404 (43.3%) | 208 (22.3%) | 163 (17.5%) | |
| Type of residency (n, %) | p = 0.0128 | ||||
| Urban | 744 (80.3%) | 692 (74.3%) | 689 (74.0%) | 664 (71.3%) | |
| Rural | 183 (19.7%) | 240 (25.7%) | 242 (26.0%) | 267 (28.7%) | |
| BMI status (n, %) | p = 0.0297 | ||||
| Normal weight | 607 (65.5%) | 575 (61.7%) | 621 (66.7%) | 634 (68.1%) | |
| Overweight | 182 (19.6%) | 225 (24.1%) | 201 (21.6%) | 184 (19.8%) | |
| Obese | 138 (14.9%) | 132 (14.2%) | 109 (11.7%) | 113 (12.1%) | |
| WHR (n, %) | p = 0.0001 | ||||
| Low | 576 (62.1%) | 544 (58.4%) | 586 (62.9%) | 681 (73.2%) | |
| Moderate | 223 (24.1%) | 260 (27.9%) | 219 (23.5%) | 152 (16.3%) | |
| High | 128 (13.8%) | 128 (13.7%) | 126 (13.5%) | 98 (10.5%) | |
| Physical activity levels (n, %) | p = 0.0021 | ||||
| Low | 750 (80.9%) | 766 (82.2%) | 334 (35.9%) | 336(36.1%) | |
| Moderate | 163 (17.6%) | 157 (16.8%) | 344 (36.9%) | 195 (20.9%) | |
| High | 14 (1.51%) | 9 (1.0%) | 253 (27.2%) | 400 (43.0%) | |
| Sleep quality (n, %) | p = 0.0001 | ||||
| Adequate | 539 (58.1%) | 525 (56.3%) | 758 (81.4%) | 773 (83.0%) | |
| Inadequate | 388 (41.9%) | 407 (43.7%) | 173 (18.6%) | 158 (17.0%) | |
| Quality of life (n, %) | p = 0.0001 | ||||
| Below mean value | 458 (49.4%) | 598 (64.2%) | 491 (52.7%) | 325 (34.9%) | |
| Over mean value | 469 (50.6%) | 334 (35.8%) | 440 (47.3%) | 606 (65.1%) | |
| Anxiety (n, %) | p = 0.0001 | ||||
| No | 610 (65.8%) | 642 (68.9%) | 700 (75.2%) | 779 (83.7%) | |
| Yes | 317 (34.2%) | 290 (31.1%) | 231 (24.8%) | 152 (16.3%) | |
| Depression (n, %) | p = 0.0001 | ||||
| No | 530 (57.2%) | 573 (61.5%) | 661 (71.0%) | 718 (77.1%) | |
| Yes | 397 (42.8%) | 359 (38.5%) | 270 (29.0%) | 213 (22.9%) | |
| Characteristics | Mediterranean Diet Adherence (Very Low + Low vs. Moderate + High) | |
|---|---|---|
| OR * (95% CI **) | p-Value | |
| Gender (Male/Female) | 1.35 (1.03–1.57) | p = 0.0087 |
| Educational status (Below/Over mean value) | 1.28 (0.77–1.82) | p = 0.2938 |
| Family financial level (Low or medium/High) | 1.32 (0.98–1.65) | p = 0.0376 |
| Nationality (Greek /Other) | 0.91 (0.23–1.67) | p = 0.8932 |
| Living status (Living alone/Living with others) | 1.42 (1.05–1.87) | p = 0.0783 |
| Employment (Unemployed/Employed) | 1.15 (0.71–1.68) | p = 0.2394 |
| Smoking habits (Yes/No) | 1.58 (1.33–1.84) | p = 0.0189 |
| Type of residency (Urban/Rural) | 1.10 (0.69–1.58) | p = 0.1947 |
| BMI status (Normal weight/Overweight + Obese) | 1.87 (1.28–2.43) | p = 0.2043 |
| WHR (Moderate + high/Low) | 1.69 (1.42–1.81) | p = 0.0184 |
| Physical activity levels (Low/Moderate + high) | 1.55 (1.18–1.89) | p = 0.0201 |
| Sleep quality (Inadequate/Adequate) | 1.96 (1.72–2.29) | p = 0.0119 |
| Quality of life (Below mean value/Over mean value) | 2.04 (1.83–2.27) | p = 0.0098 |
| Anxiety (Yes/No) | 2.18 (1.93–2.41) | p = 0.0107 |
| Depression (Yes/No) | 2.43 (2.25–2.66) | p = 0.0045 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pavlidou, E.; Papadopoulou, S.K.; Mentzelou, M.; Dakanalis, A.; Vorvolakos, T.; Antasouras, G.; Spanoudaki, M.; Pandi, A.-L.; Serdari, A.; Chrysafi, M.; et al. Association of Mediterranean Diet Adherence with Sociodemographic, Anthropometric, and Lifestyle Factors during the COVID-19 Pandemic: A Cross-Sectional Study in Greece. Nutrients 2023, 15, 4123. https://doi.org/10.3390/nu15194123
Pavlidou E, Papadopoulou SK, Mentzelou M, Dakanalis A, Vorvolakos T, Antasouras G, Spanoudaki M, Pandi A-L, Serdari A, Chrysafi M, et al. Association of Mediterranean Diet Adherence with Sociodemographic, Anthropometric, and Lifestyle Factors during the COVID-19 Pandemic: A Cross-Sectional Study in Greece. Nutrients. 2023; 15(19):4123. https://doi.org/10.3390/nu15194123
Chicago/Turabian StylePavlidou, Eleni, Sousana K. Papadopoulou, Maria Mentzelou, Antonios Dakanalis, Theofanis Vorvolakos, Georgios Antasouras, Maria Spanoudaki, Aimilia-Lynn Pandi, Aspasia Serdari, Maria Chrysafi, and et al. 2023. "Association of Mediterranean Diet Adherence with Sociodemographic, Anthropometric, and Lifestyle Factors during the COVID-19 Pandemic: A Cross-Sectional Study in Greece" Nutrients 15, no. 19: 4123. https://doi.org/10.3390/nu15194123
APA StylePavlidou, E., Papadopoulou, S. K., Mentzelou, M., Dakanalis, A., Vorvolakos, T., Antasouras, G., Spanoudaki, M., Pandi, A.-L., Serdari, A., Chrysafi, M., Dimoliani, S., & Giaginis, C. (2023). Association of Mediterranean Diet Adherence with Sociodemographic, Anthropometric, and Lifestyle Factors during the COVID-19 Pandemic: A Cross-Sectional Study in Greece. Nutrients, 15(19), 4123. https://doi.org/10.3390/nu15194123