Do Sugar-Sweetened Beverages Increase Fasting FGF21 Irrespective of the Type of Added Sugar? A Secondary Exploratory Analysis of a Randomized Controlled Trial
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Subjects
2.3. Protocol
2.4. Anthropometry
2.5. Laboratory Analysis
2.6. Dietary Assessment
2.7. Statistics
3. Results
3.1. Anthropometry
3.2. Glucose and Lipid Metabolism
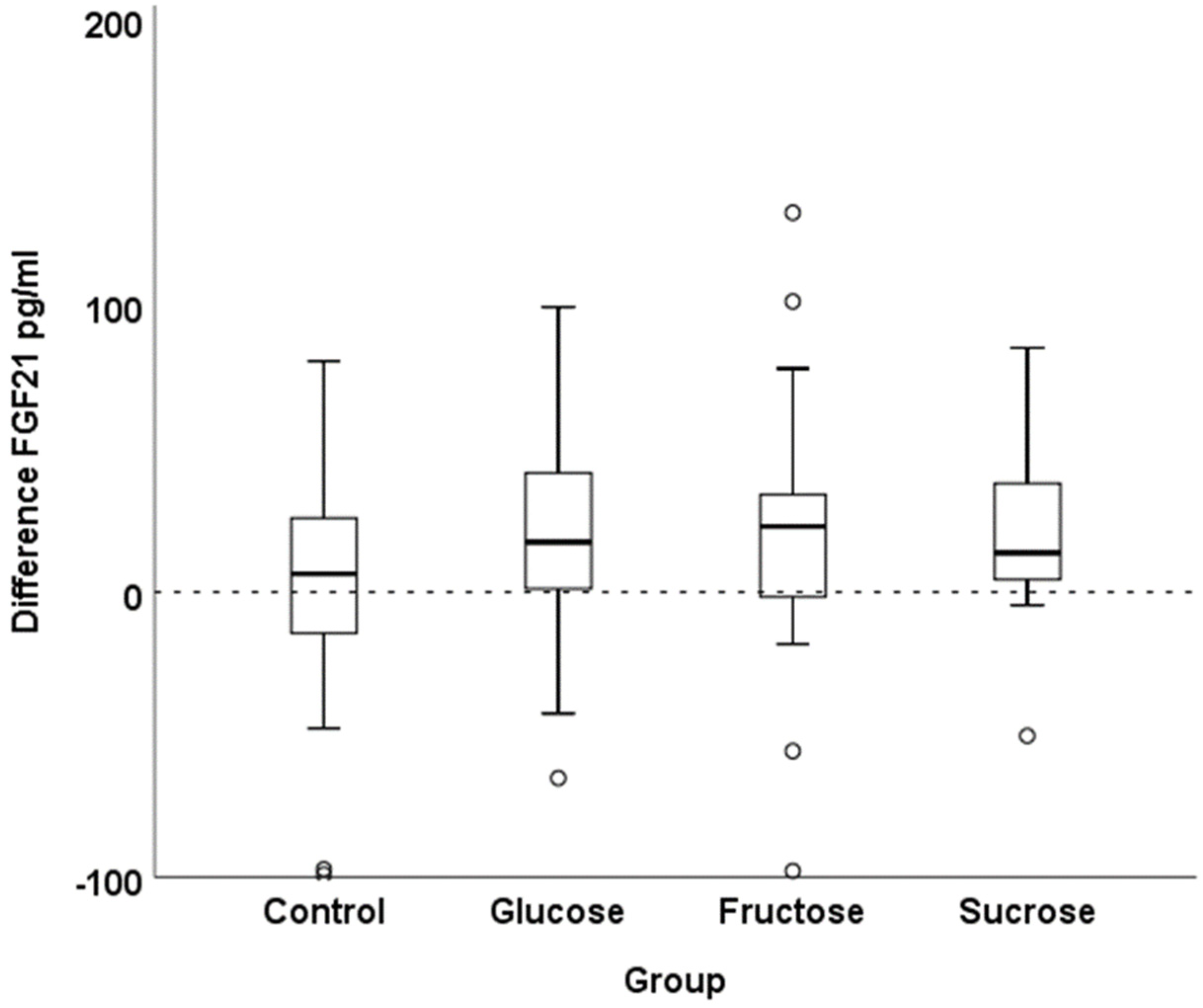
3.3. Fasting FGF21 Concentrations
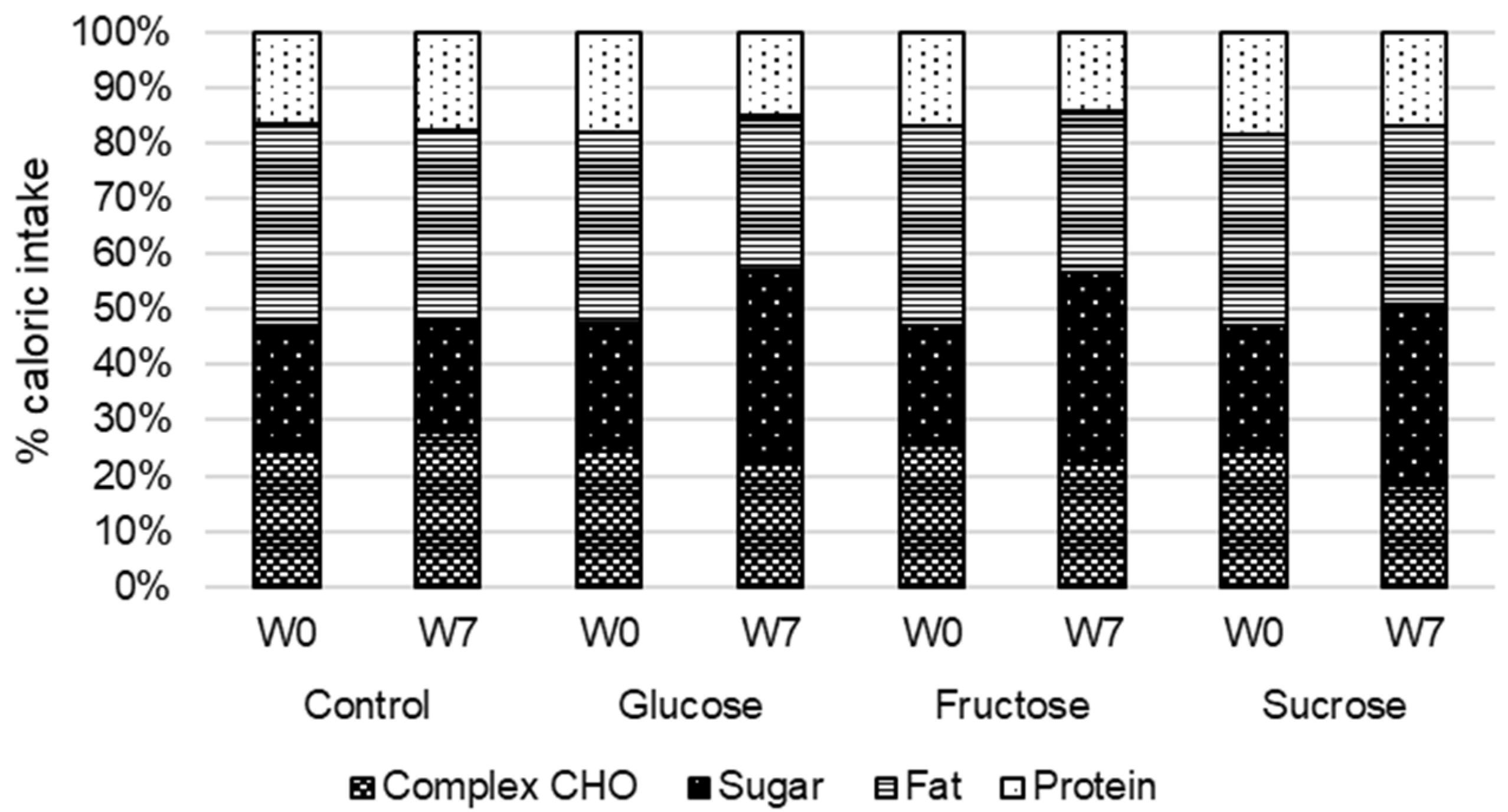
3.4. Food Intake
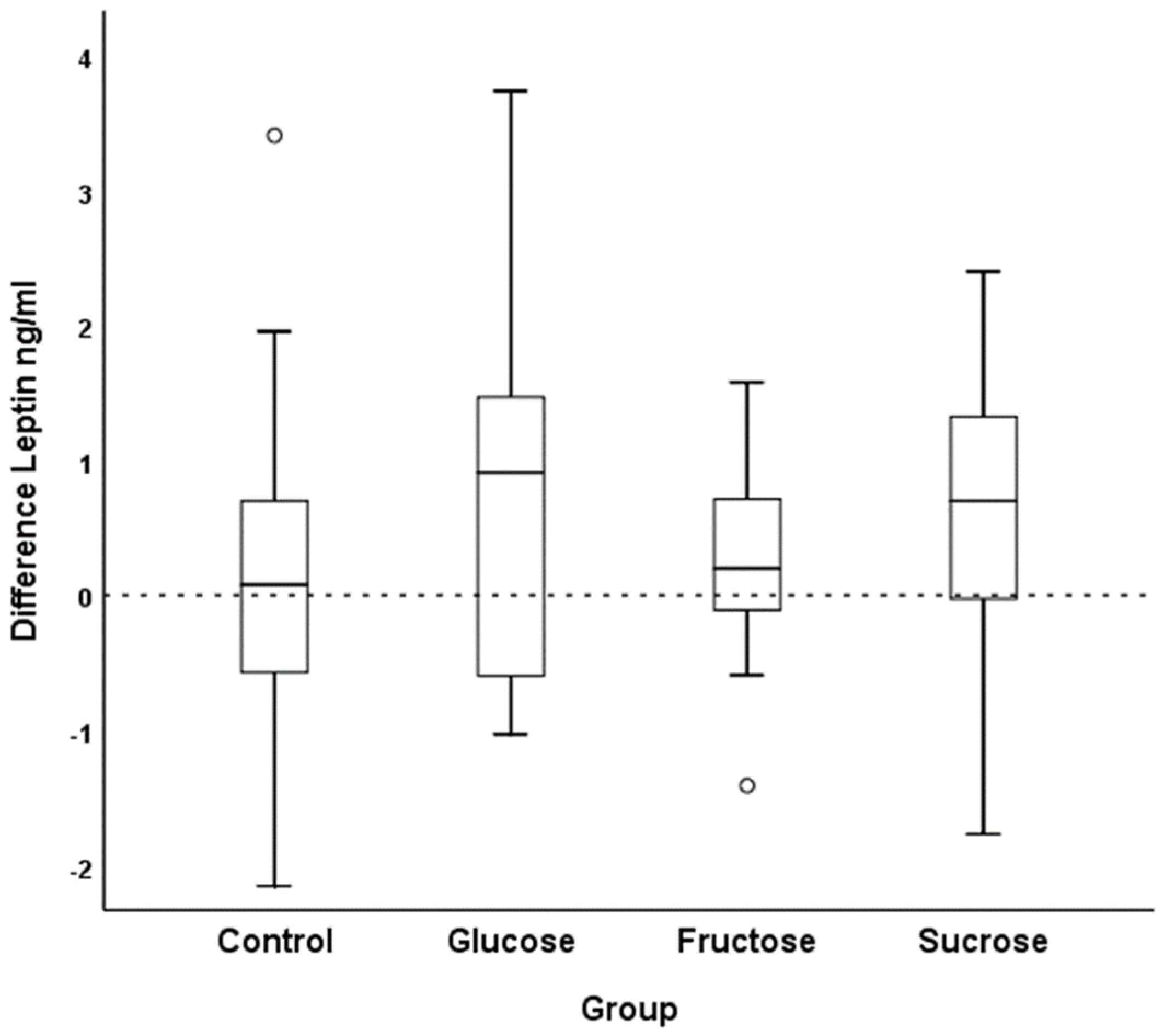
3.5. Adipokines
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Malik, V.S.; Hu, F.B. The role of sugar-sweetened beverages in the global epidemics of obesity and chronic diseases. Nat. Rev. Endocrinol. 2022, 18, 205–218. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hoffmann, G.; Lampousi, A.-M.; Knüppel, S.; Iqbal, K.; Schwedhelm, C.; Bechthold, A.; Schlesinger, S.; Boeing, H. Food groups and risk of type 2 diabetes mellitus: A systematic review and meta-analysis of prospective studies. Eur. J. Epidemiol. 2017, 32, 363–375. [Google Scholar] [CrossRef]
- Assy, N.; Nasser, G.; Kamayse, I.; Nseir, W.; Beniashvili, Z.; Djibre, A.; Grosovski, M. Soft drink consumption linked with fatty liver in the absence of traditional risk factors. Can. J. Gastroenterol. 2008, 22, 811–816. [Google Scholar] [CrossRef] [PubMed]
- Duffey, K.J.; Gordon-Larsen, P.; Steffen, L.M.; Jacobs, D.R.; Popkin, B.M. Drinking caloric beverages increases the risk of adverse cardiometabolic outcomes in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am. J. Clin. Nutr. 2010, 92, 954–959. [Google Scholar] [CrossRef]
- Aeberli, I.; Hochuli, M.; Gerber, P.A.; Sze, L.; Murer, S.B.; Tappy, L.; Spinas, G.A.; Berneis, K.; Espeland, M.A.; Bryan, R.N.; et al. Moderate amounts of fructose consumption impair insulin sensitivity in healthy young men. Diabetes Care 2012, 36, 150–156. [Google Scholar] [CrossRef]
- Geidl-Flueck, B.; Hochuli, M.; Németh, Á.; Eberl, A.; Derron, N.; Köfeler, H.C.; Tappy, L.; Berneis, K.; Spinas, G.A.; Gerber, P.A. Fructose- and sucrose- but not glucose-sweetened beverages promote hepatic de novo lipogenesis: A randomized controlled trial. J. Hepatol. 2021, 75, 46–54. [Google Scholar] [CrossRef]
- Hochuli, M.; Herter-Aeberli, I.; Weiss, A.; Hersberger, M.; Troxler, H.; Gerber, P.; Spinas, G.A.; Berneis, K. Sugar-Sweetened Beverages With Moderate Amounts of Fructose, but Not Sucrose, Induce Fatty Acid Synthesis in Healthy Young Men: A Randomized Crossover Study. J. Clin. Endocrinol. Metab. 2014, 99, 2164–2172. [Google Scholar] [CrossRef]
- Aeberli, I.; A Gerber, P.; Hochuli, M.; Kohler, S.; Haile, S.R.; Gouni-Berthold, I.; Berthold, H.K.; A Spinas, G.; Berneis, K. Low to moderate sugar-sweetened beverage consumption impairs glucose and lipid metabolism and promotes inflammation in healthy young men: A randomized controlled trial. Am. J. Clin. Nutr. 2011, 94, 479–485. [Google Scholar] [CrossRef]
- BonDurant, L.D.; Potthoff, M.J. Fibroblast Growth Factor 21: A Versatile Regulator of Metabolic Homeostasis. Annu. Rev. Nutr. 2018, 38, 173–196. [Google Scholar] [CrossRef]
- Talukdar, S.; Owen, B.M.; Song, P.; Hernandez, G.; Zhang, Y.; Zhou, Y.; Scott, W.T.; Paratala, B.; Turner, T.; Smith, A.; et al. FGF21 Regulates Sweet and Alcohol Preference. Cell Metab. 2015, 23, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Owen, B.M.; Ding, X.; Morgan, D.A.; Coate, K.C.; Bookout, A.L.; Rahmouni, K.; Kliewer, S.A.; Mangelsdorf, D.J. FGF21 acts centrally to induce sympathetic nerve activity, energy expenditure, and weight loss. Cell Metab. 2014, 20, 670–677. [Google Scholar] [CrossRef] [PubMed]
- Kharitonenkov, A.; Shiyanova, T.L.; Koester, A.; Ford, A.M.; Micanovic, R.; Galbreath, E.J.; Sandusky, G.E.; Hammond, L.J.; Moyers, J.S.; Owens, R.A.; et al. FGF-21 as a novel metabolic regulator. J. Clin. Investig. 2005, 115, 1627–1635. [Google Scholar] [CrossRef] [PubMed]
- Schlein, C.; Talukdar, S.; Heine, M.; Fischer, A.W.; Krott, L.M.; Nilsson, S.K.; Brenner, M.B.; Heeren, J.; Scheja, L. FGF21 Lowers Plasma Triglycerides by Accelerating Lipoprotein Catabolism in White and Brown Adipose Tissues. Cell Metab. 2016, 23, 441–453. [Google Scholar] [CrossRef]
- Mashili, F.L.; Austin, R.L.; Deshmukh, A.S.; Fritz, T.; Caidahl, K.; Bergdahl, K.; Zierath, J.R.; Chibalin, A.V.; Moller, D.E.; Kharitonenkov, A.; et al. Direct effects of FGF21 on glucose uptake in human skeletal muscle: Implications for type 2 diabetes and obesity. Diabetes/Metab. Res. Rev. 2011, 27, 286–297. [Google Scholar] [CrossRef] [PubMed]
- Minard, A.Y.; Tan, S.-X.; Yang, P.; Fazakerley, D.; Domanova, W.; Parker, B.L.; Humphrey, S.; Jothi, R.; Stöckli, J.; James, D.E. mTORC1 Is a Major Regulatory Node in the FGF21 Signaling Network in Adipocytes. Cell Rep. 2016, 17, 29–36. [Google Scholar] [CrossRef]
- Cuevas-Ramos, D.; Mehta, R.; Aguilar-Salinas, C.A. Fibroblast Growth Factor 21 and Browning of White Adipose Tissue. Front. Physiol. 2019, 10, 37. [Google Scholar] [CrossRef] [PubMed]
- Fisher, F.M.; Kleiner, S.; Douris, N.; Fox, E.C.; Mepani, R.J.; Verdeguer, F.; Wu, J.; Kharitonenkov, A.; Flier, J.S.; Maratos-Flier, E.; et al. FGF21 regulates PGC-1α and browning of white adipose tissues in adaptive thermogenesis. Genes Dev. 2012, 26, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Yeung, D.C.Y.; Karpisek, M.; Stejskal, D.; Zhou, Z.-G.; Liu, F.; Wong, R.L.C.; Chow, W.-S.; Tso, A.W.K.; Lam, K.S.L.; et al. Serum FGF21 Levels Are Increased in Obesity and Are Independently Associated with the Metabolic Syndrome in Humans. Diabetes 2008, 57, 1246–1253. [Google Scholar] [CrossRef] [PubMed]
- Dushay, J.; Chui, P.C.; Gopalakrishnan, G.S.; Varela–Rey, M.; Crawley, M.; Fisher, F.M.; Badman, M.K.; Chantar, M.L.M.; Maratos–Flier, E. Increased fibroblast growth factor 21 in obesity and nonalcoholic fatty liver disease. Gastroenterology 2010, 139, 456–463. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Fang, Q.; Gao, F.; Fan, J.; Zhou, J.; Wang, X.; Zhang, H.; Pan, X.; Bao, Y.; Xiang, K.; et al. Fibroblast growth factor 21 levels are increased in nonalcoholic fatty liver disease patients and are correlated with hepatic triglyceride. J. Hepatol. 2010, 53, 934–940. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Qian, L.; Zhang, L.; Zhang, J.; Zhou, J.; Li, Y.; Hou, X.; Fang, Q.; Li, H.; Jia, W. Fibroblast Growth Factor 21 is Related to Atherosclerosis Independent of Nonalcoholic Fatty Liver Disease and Predicts Atherosclerotic Cardiovascular Events. J. Am. Hear. Assoc. 2020, 9, e015226. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Lu, N.; Zheng, M. A high circulating FGF21 level as a prognostic marker in patients with acute myocardial infarction. Am. J. Transl. Res. 2018, 10, 2958–2966. [Google Scholar] [PubMed]
- Fisher, F.M.; Chui, P.C.; Antonellis, P.J.; Bina, H.A.; Kharitonenkov, A.; Flier, J.S.; Maratos-Flier, E. Obesity is a fibroblast growth factor 21 (FGF21)-resistant state. Diabetes 2010, 59, 2781–2789. [Google Scholar] [CrossRef] [PubMed]
- Gallego-Escuredo, J.M.; Gomez-Ambrosi, J.; Catalan, V.; Domingo, P.; Giralt, M.; Frühbeck, G.; Villarroya, F. Opposite alterations in FGF21 and FGF19 levels and disturbed expression of the receptor machinery for endocrine FGFs in obese patients. Int. J. Obes. 2014, 39, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Xie, T.; Leung, P.S. Fibroblast growth factor 21: A regulator of metabolic disease and health span. Am. J. Physiol. Metab. 2017, 313, E292–E302. [Google Scholar] [CrossRef]
- Inagaki, T.; Dutchak, P.; Zhao, G.; Ding, X.; Gautron, L.; Parameswara, V.; Li, Y.; Goetz, R.; Mohammadi, M.; Esser, V.; et al. Endocrine regulation of the fasting response by PPARα-mediated induction of fibroblast growth factor 21. Cell Metab. 2007, 5, 415–425. [Google Scholar] [CrossRef]
- Badman, M.K.; Pissios, P.; Kennedy, A.R.; Koukos, G.; Flier, J.S.; Maratos-Flier, E. Hepatic fibroblast growth factor 21 is regulated by PPARα and is a key mediator of hepatic lipid metabolism in ketotic states. Cell Metab. 2007, 5, 426–437. [Google Scholar] [CrossRef]
- Laeger, T.; Henagan, T.M.; Albarado, D.C.; Redman, L.M.; Bray, G.A.; Noland, R.C.; Münzberg, H.; Hutson, S.M.; Gettys, T.W.; Schwartz, M.W.; et al. FGF21 is an endocrine signal of protein restriction. J. Clin. Investig. 2014, 124, 3913–3922. [Google Scholar] [CrossRef]
- Lin, Z.; Gong, Q.; Wu, C.; Yu, J.; Lu, T.; Pan, X.; Lin, S.; Li, X. Dynamic Change of Serum FGF21 Levels in Response to Glucose Challenge in Human. J. Clin. Endocrinol. Metab. 2012, 97, E1224–E1228. [Google Scholar] [CrossRef]
- Dushay, J.R.; Toschi, E.; Mitten, E.K.; Fisher, F.M.; Herman, M.A.; Maratos-Flier, E. Fructose ingestion acutely stimulates circulating FGF21 levels in humans. Mol. Metab. 2014, 4, 51–57. [Google Scholar] [CrossRef]
- Lundsgaard, A.-M.; Fritzen, A.M.; Sjøberg, K.A.; Myrmel, L.S.; Madsen, L.; Wojtaszewski, J.F.; Richter, E.A.; Kiens, B. Circulating FGF21 in humans is potently induced by short term overfeeding of carbohydrates. Mol. Metab. 2016, 6, 22–29. [Google Scholar] [CrossRef]
- Couchepin, C.; Lê, K.-A.; Bortolotti, M.; da Encarnaҫao, J.A.; Oboni, J.-B.; Tran, C.; Schneiter, P.; Tappy, L. Markedly blunted metabolic effects of fructose in healthy young female subjects compared with male subjects. Diabetes Care 2008, 31, 1254–1256. [Google Scholar] [CrossRef] [PubMed]
- Gibson, R. Principles of Nutritional Assessment; Oxford University Press: New York, NY, USA, 2005. [Google Scholar]
- Geidl-Flueck, B.; Gerber, P.A. Insights into the Hexose Liver Metabolism—Glucose versus Fructose. Nutrients 2017, 9, 1026. [Google Scholar] [CrossRef]
- Hojman, P.; Pedersen, M.; Nielsen, A.R.; Krogh-Madsen, R.; Yfanti, C.; Åkerstrom, T.; Nielsen, S.; Pedersen, B.K. Fibroblast growth factor-21 is induced in human skeletal muscles by hyperinsulinemia. Diabetes 2009, 58, 2797–2801. [Google Scholar] [CrossRef]
- Mazuecos, L.; Pintado, C.; Rubio, B.; Guisantes-Batán, E.; Andrés, A.; Gallardo, N. Leptin, Acting at Central Level, Increases FGF21 Expression in White Adipose Tissue via PPARβ/δ. Int. J. Mol. Sci. 2021, 22, 4624. [Google Scholar] [CrossRef]
- Fisher, F.M.; Kim, M.; Doridot, L.; Cunniff, J.C.; Parker, T.S.; Levine, D.M.; Hellerstein, M.K.; Hudgins, L.C.; Maratos-Flier, E.; Herman, M.A. A critical role for ChREBP-mediated FGF21 secretion in hepatic fructose metabolism. Mol. Metab. 2016, 6, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Lin, Z.; Tian, H.; Lam, K.S.; Lin, S.; Hoo, R.C.; Konishi, M.; Itoh, N.; Wang, Y.; Bornstein, S.R.; Xu, A.; et al. Adiponectin mediates the metabolic effects of FGF21 on glucose homeostasis and insulin sensitivity in mice. Cell Metab. 2013, 17, 779–789. [Google Scholar] [CrossRef]
- Fu, Y.; Luo, N.; Klein, R.L.; Garvey, W.T. Adiponectin promotes adipocyte differentiation, insulin sensitivity, and lipid accumulation. J. Lipid Res. 2005, 46, 1369–1379. [Google Scholar] [CrossRef] [PubMed]
- Benomar, Y.; Amine, H.; Crépin, D.; Al Rifai, S.; Riffault, L.; Gertler, A.; Taouis, M. Central Resistin/TLR4 Impairs Adiponectin Signaling, Contributing to Insulin and FGF21 Resistance. Diabetes 2016, 65, 913–926. [Google Scholar] [CrossRef] [PubMed]
- Geng, L.; Liao, B.; Jin, L.; Huang, Z.; Triggle, C.; Ding, H.; Zhang, J.; Huang, Y.; Lin, Z.; Xu, A. Exercise Alleviates Obesity-Induced Metabolic Dysfunction via Enhancing FGF21 Sensitivity in Adipose Tissues. Cell Rep. 2019, 26, 2738–2752.e4. [Google Scholar] [CrossRef]
- Rodgers, M.; Heineman, B.; Dushay, J. Increased fructose consumption has sex-specific effects on fibroblast growth factor 21 levels in humans. Obes. Sci. Pract. 2019, 5, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Migdal, A.; Comte, S.; Rodgers, M.; Heineman, B.; Maratos-Flier, E.; Herman, M.; Dushay, J. Fibroblast growth factor 21 and fructose dynamics in humans. Obes. Sci. Pract. 2018, 4, 483–489. [Google Scholar] [CrossRef]
- Suez, J.; Korem, T.; Zeevi, D.; Zilberman-Schapira, G.; Thaiss, C.A.; Maza, O.; Israeli, D.; Zmora, N.; Gilad, S.; Weinberger, A.; et al. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature 2014, 514, 181–186. [Google Scholar] [CrossRef]
- Fowler, S.; Williams, K.; Resendez, R.G.; Hunt, K.J.; Hazuda, H.P.; Stern, M.P. Fueling the obesity epidemic? Artificially sweetened beverage use and long-term weight gain. Obesity 2008, 16, 1894–1900. [Google Scholar] [CrossRef]
- Rosinger, A.; Herrick, K.; Gahche, J.; Park, S. Sugar-Sweetened Beverage Consumption among U.S. Adults, 2011–2014; NCHS Data Brief; National Center for Health Statistics: Hyattsville, MD, USA, 2017; pp. 1–8. [Google Scholar]
| Variable | Control Group N = 21 | Glucose Group N = 20 | Fructose Group N = 23 | Sucrose Group N = 19 | |
|---|---|---|---|---|---|
| Age (years) | W0 | 22.5 (21.2–23.8) | 22.0 (20.8–23.1) | 23.6 (22.6–24.5) | 23.4 (22.3–24.4) |
| Body weight (kg) | W0 | 69.7 (65.8–73.7) | 71.4 (68.0–74.7) | 69.5 (65.8–73.1) | 76.2 (72.9–79.4) |
| W7 | 69.9 (66.0–73.8) | 71.9 (68.7–75.1) | 69.8 (66.2–73.4) | 76.7 (73.6–79.9) | |
| Δ | 0.0 (−0.9–1.4) 1 | 0.3 (−0.2–1.4) 1 | 0.8 (−0.7–1.2) 1 | 0.2 (−0.4–1.3) 1 | |
| Height (m) | W0 | 1.81 (1.78–1.84) | 1.81 (1.78–1.84) | 1.80 (1.77–1.83) | 1.83 (1.80–1.86) |
| W/H ratio | W0 | 0.88 (0.87–0.90) | 0.85 (0.83–0.87) | 0.87 (0.85–0.89) | 0.87 (0.85–0.89) |
| W7 | 0.88 (0.87–0.90) | 0.85 (0.83–0.87) | 0.87 (0.85–0.89) | 0.88 (0.86–0.90) | |
| Δ | 0.00 (−0.01–0.02) | 0.00 (−0.02–0.02) | 0.00 (−0.02–0.01) | 0.01 (−0.01–0.02) |
| Variable | Control Group N = 21 | Glucose Group N = 20 | Fructose Group N = 23 | Sucrose Group N = 19 | |
|---|---|---|---|---|---|
| Fasting glucose (mmol/L) | W0 | 4.33 (3.97–4.63) | 4.26 (4.09–4.42) | 4.38 (4.15–4.53) | 4.40 (4.20–4.66) |
| W7 | 4.47 (4.09–4.67) | 4.39 (4.09–4.56) | 4.44 (4.16–4.73) | 4.32 (4.24–4.57) | |
| Δ | 0.03 (−0.16–0.23) 1 | 0.05 (−0.14–0.23) 1 | 0.01 (−0.15–0.17) 1 | −0.02 (−0.14–0.10) 1 | |
| Insulin (pmol/L) | W0 | 104.1 (79.3–137.7) | 98.3 (80.6–121.8) | 103.4 (75.6–134.9) | 94.7 (45.7–123.0) |
| W7 | 90.9 (76.0–117.6) | 107.4 (83.2–143.0) | 99.3 (83.5–154.8) | 89.8 (53.9–108.9) | |
| Δ | −13.0 (−34.6–8.6) 1 | 11.5 (−12.3–35.4) 1 | −6.3 (−34.4–21.7) 1 | −8.2 (−32.0–15.5) 1 | |
| c-peptide (pmol/L) | W0 | 410.0 (360.0–445.0) | 435.0 (360.5–560.0) | 390.0 (290.0–510.0) | 350.0 (290.0–430.0) |
| W7 | 380.0 (355.0–490.0) | 480.0 (324.0–610.0) | 390.0 (310.0–510.0) | 430.0 (280.0–500.0) | |
| Δ | −13.6 (−68.8–41.6) 1 | −11.7 (−72.4–49.1) 1 | −3.7 (−38.4–31.0) 1 | 55.8 (6.0–105.6) 1 | |
| Triglycerides (mmol/L) | W0 | 0.77 (0.66–0.93) | 0.72 (0.53–0.88) | 0.84 (0.58–1.15) | 0.84 (0.61–0.92) |
| W7 | 0.74 (0.62–0.94) | 0.72 (0.53–1.12) | 0.86 (0.61–1.04) | 0.68 (0.58–0.88) | |
| Δ | −0.00 (−0.21–0.14) | 0.03 (−0.09–0.27) | −0.08 (−0.31–0.07) | −0.12 (−0.27–0.13) | |
| FFA (µmol/L) | W0 | 428 (361–700) | 531 (463–770) | 520 (340–703) | 464 (343–745) |
| W7 | 481 (393–580) | 368 (284–547) | 363 (296–472) | 441 (273–754) | |
| Δ | 30 (−269–114) | −172 (−363–51) | −117 (−263–28) | −87 (−407–187) | |
| Total cholesterol (mmol/L) | W0 | 3.80 (3.40–4.35) | 3.60 (3.30–4.30) | 3.90 (3.60–4.50) | 4.10 (3.40–4.50) |
| W7 | 3.70 (3.25–4.25) | 3.80 (3.20–4.35) | 3.80 (3.60–4.10) | 3.9 (3.58–4.35) | |
| Δ | −0.10 (−0.30–0.00) | 0.00 (−0.35–0.40) | −0.10 (−0.50–0.10) | 0.10 (−0.50–0.30) | |
| LDL cholesterol (mmol/L) | W0 | 2.00 (1.55–2.55) | 1.80 (1.50–2.30) | 2.35 (1.90–2.68) | 2.20 (1.70–2.70) |
| W7 | 2.00 (1.45–2.50) | 1.95 (1.40–2.38) | 2.00 (1.80–2.60) | 2.10 (1.65–2.53) | |
| Δ | 0.00 (−0.15- 0.10) | −0.10 (−0.20–0.30) | −0.10 (−0.50–0.20) | 0.00 (−0.40–0.20) | |
| HDL cholesterol (mmol/L) | W0 | 1.39 (1.25–1.62) | 1.45 (1.27–1.70) | 1.36 (1.09–1.55) | 1.40 0 (1.16–1.71) |
| W7 | 1.37 (1.11–1.51) | 1.48 (1.15–1.67) | 1.29 (1.13–1.62) | 1.49 (1.28–1.67) | |
| Δ | −0.07 (−0.21–−0.01) | −0.05 (−0.10–0.10) | 0.02 (−0.18–0.14) | 0.08 (−0.12–0.16) | |
| Leptin (ng/mL) | W0 | 2.1 (1.1–3.4) | 2.0 (0.8–3.1) | 2.4 (0.7–3.3) | 2.7 (1.4–3.3) |
| W7 | 2.1 (1.1–3.1) | 2.1 (1.4–4.0) | 2.6 (0.9–3.5) | 3.2 (1.7–4.3) | |
| Δ | 0.1 (−0.5–0.6) 1 | 0.6 (−0.2–1.4) 1 | 0.3 (−0.1–0.6) 1 | 0.6 (0.1–1.1) 1 | |
| Resistin (ng/mL) | W0 | 3.6 (3.0–4.3) | 3.9 (3.2–4.5) | 4.1 (3.1–5.0) | 3.7 (3.1–4.2) |
| W7 | 3.7 (2.8–4.3) | 3.8 (3.2–5.0) | 4.0 (3.2–4.5) | 3.5 (3.1–4.3) | |
| Δ | 0.1 (−0.4–0.2) | 0.0 (−0.3–0.7) | −0.3 (−0.6–0.1) | 0.1 (−0.3–0.4) | |
| Adiponectin (µg/mL) | W0 | 6.0 (4.2–9.2) | 6.0 (3.7–6.9) | 5.1 (3.7–8.7) | 4.9 (3.6–7.0) |
| W7 | 5.8 (3.9–9.1) | 6.2 (4.5–7.2) | 4.6 (3.5–7.4) | 5.6 (4.3–6.7) | |
| Δ | −0.2 (−1.0–0.7) | 0.4 (−0.6–1.6) | −0.3 (−1.1–0.3) | 0.1 (−0.7–0.8) | |
| FGF21 (pg/mL) | W0 | 49.3 (18.6–81.0) | 51.6 (42.1–65.6) | 45.0 (24.5–82.5) | 31.6 (20.4–59.0) |
| W7 | 61.4 (33.6–90.3) | 70.3 (26.6–107.1) | 53.9 (38.9–108.8) | 58.6 (32.0–102.8) | |
| Δ | 6.3 (−20.1–26.9) | 17.4 (0.4–45.8) | 22.9 (−8.6–35.1) | 13.7 (2.2–46.1) |
| Control N = 21 | Glucose N = 18 | Fructose N = 19 | Sucrose N = 18 | ||
|---|---|---|---|---|---|
| Energy (kcal/day) | W0 | 2085 (1887–2662) | 2024 (1791–2462) | 1835 (1502–2322) | 2214 (1976–2723) |
| W7 | 1898 (1687–2364) | 2389 (1876–2510) | 2131 (1707–2574) | 1894 (1640–2911) | |
| Δ | −187 (−396–−36) | 112 (−234–497) | 155 (−223–578) | −68 (−936–311) | |
| Carbohydrate, % | W0 | 47 (44–49) 2 | 47 (44–50) 2 | 47 (43–50) 2 | 47 (44–50) 2 |
| W7 | 48 (44–52) 2 | 58 (55–61) 2 | 56 (53–60) 2 | 52 (48–56) 2 | |
| Δ | 1 (−2–5) 2 | 11 (7–15) 2 | 10 (5–14) 2 | 4 (0–8) 2 | |
| Protein, % | W0 | 17 (15–18) 2 | 18 (15–20) 2 | 17 (15–19) 2 | 19 (17–21) 2 |
| W7 | 18 (16–19) 2 | 15 (14–17) 2 | 14 (13–15) 2 | 17 (15–19) 2 | |
| Δ | 1 (−1–3) 2 | −3 (−5–0) 2 | −2 (−5–0) 2 | −2 (−4–1) 2 | |
| Fat, % | W0 | 37 (35–39) 2 | 35 (32–38) 2 | 36 (32–39) 2 | 35 (32–38) 2 |
| W7 | 35 (32–38) 2 | 29 (26–32) 2 | 29 (26–32) 2 | 33 (29–37) 2 | |
| Δ | −3 (−8–2) | −4 (−11–−1) | −7 (−10–−2) | −2 (−6–0) | |
| Fructose 1, g/d | W0 | 6.9 (4.3–15.4) | 4.5 (1.2–7.9) | 5.8 (2.8–9.8) | 7.8 (1.9–12.4) |
| W7 | 5.1 (2.2–7.3) | 3.6 (1.8–6.8) | 81.8 (79.7–86.1) | 2.8 (0.6–7.3) | |
| Δ | −1.8 (−9.3–1.0) | −0.5 (−3.8–1.1) | 75.1 (63.7–80.6) | −4.4 (−8.8–0.1) | |
| Glucose 1, g/d | W0 | 4.8 (2.8–10.8) | 4.4 (1.4–8.1) | 5.3 (2.1–8.6) | 5.9 (2.1–8.9) |
| W7 | 5.0 (2.1–6.0) | 83.3 (80.6–84.2) | 3.5 (2.1–6.8) | 2.6 (0.7–5.5) | |
| Δ | −0.5 (−6.7–1.3) | 78.0 (75.6–79.7) | −2.0 (−4.9–1.8) | −0.7 (−6.7–0.6) | |
| Sucrose, g/d | W0 | 61.1 (43.1–81.9) | 50.2 (32.9–83.6) | 43.2 (32.2–82.5) | 78.6 (56.4–94.8) |
| W7 | 51.0 (33.6–70.9) | 48.9 (28.8–68.0) | 51.8 (27.7–65.4) | 118.1 (101.9–146.0) | |
| Δ | −10.8 (−23.5–2.0) 2 | −5.4 (−18.0–7.1) 2 | 1.9 (−15.1–18.9) 2 | 45.2 (25.4–65.1) 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Geidl-Flueck, B.; Hochuli, M.; Spinas, G.A.; Gerber, P.A. Do Sugar-Sweetened Beverages Increase Fasting FGF21 Irrespective of the Type of Added Sugar? A Secondary Exploratory Analysis of a Randomized Controlled Trial. Nutrients 2022, 14, 4169. https://doi.org/10.3390/nu14194169
Geidl-Flueck B, Hochuli M, Spinas GA, Gerber PA. Do Sugar-Sweetened Beverages Increase Fasting FGF21 Irrespective of the Type of Added Sugar? A Secondary Exploratory Analysis of a Randomized Controlled Trial. Nutrients. 2022; 14(19):4169. https://doi.org/10.3390/nu14194169
Chicago/Turabian StyleGeidl-Flueck, Bettina, Michel Hochuli, Giatgen A. Spinas, and Philipp A. Gerber. 2022. "Do Sugar-Sweetened Beverages Increase Fasting FGF21 Irrespective of the Type of Added Sugar? A Secondary Exploratory Analysis of a Randomized Controlled Trial" Nutrients 14, no. 19: 4169. https://doi.org/10.3390/nu14194169
APA StyleGeidl-Flueck, B., Hochuli, M., Spinas, G. A., & Gerber, P. A. (2022). Do Sugar-Sweetened Beverages Increase Fasting FGF21 Irrespective of the Type of Added Sugar? A Secondary Exploratory Analysis of a Randomized Controlled Trial. Nutrients, 14(19), 4169. https://doi.org/10.3390/nu14194169







