Association between Dining with Companions and Depression among Korean Adults
Abstract
:1. Introduction
2. Methods
2.1. Study Population and Data
2.2. Measures
2.2.1. Patient Health Questionnaire-9
2.2.2. Meal Companionship Related Variables
2.2.3. Covariates
2.3. Statistical Analysis
3. Results
3.1. Participants’ General Characteristics
3.2. Association between Investigated Variables and Depression
3.3. Subgroup Analyses by Covariates
3.4. Subgroup Analyses by Levels of Depression
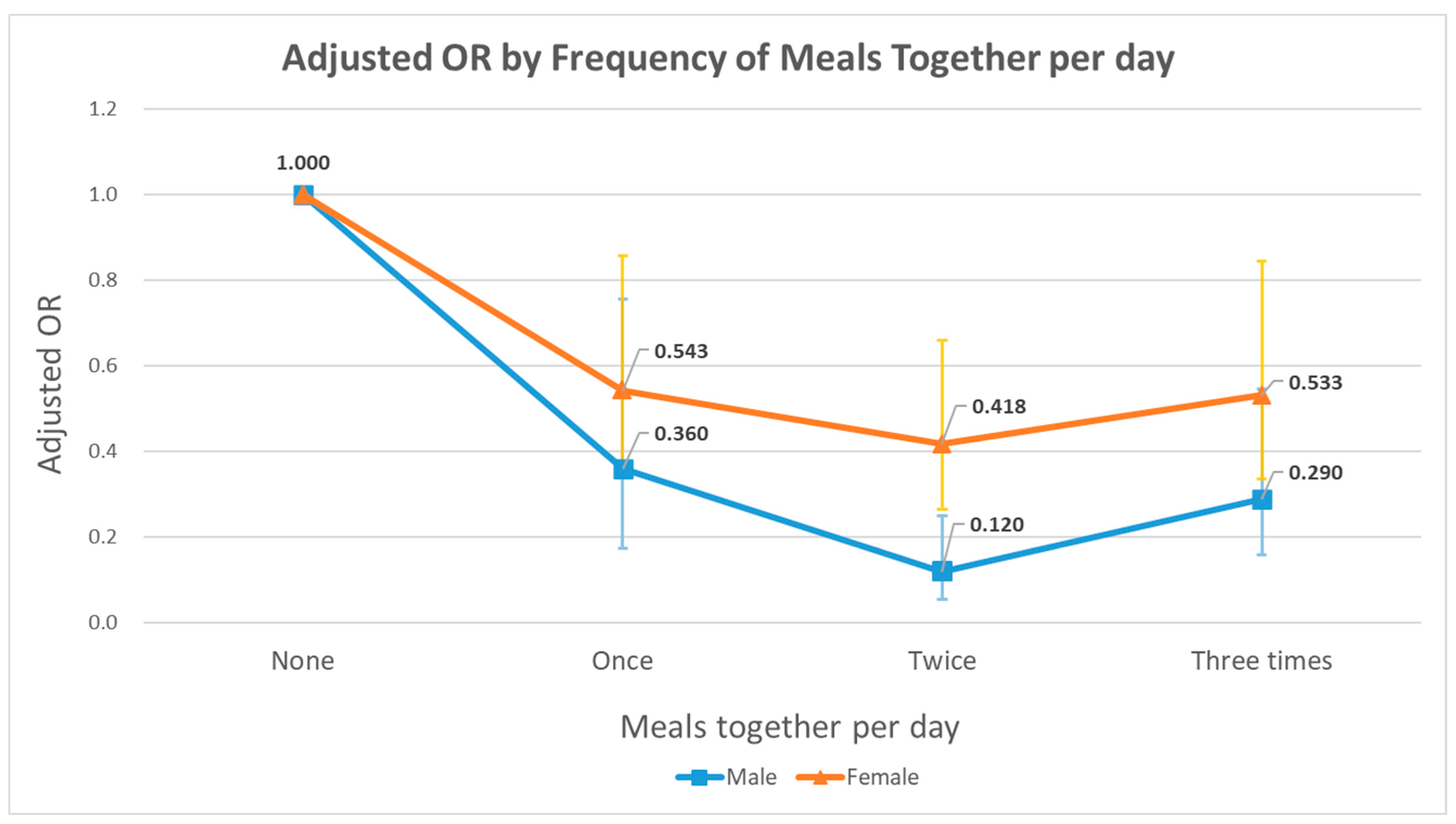
3.5. Subgroup Analyses by Various Meal Patterns
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fond, G.; Lancon, C.; Auquier, P.; Boyer, L. Prevalence of major depression in France in the general population and in specific populations from 2000 to 2018: A systematic review of the literature. Presse Med. (Paris France: 1983) 2019, 48, 365–375. [Google Scholar] [CrossRef] [PubMed]
- Weinberger, A.H.; Gbedemah, M.; Martinez, A.M.; Nash, D.; Galea, S.; Goodwin, R.D. Trends in depression prevalence in the USA from 2005 to 2015: Widening disparities in vulnerable groups. Psychol. Med. 2018, 48, 1308–1315. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Kim, K.W. A review of the epidemiology of depression in Korea. J. Korean Med. Assoc. 2011, 54, 362–369. [Google Scholar] [CrossRef] [Green Version]
- Chen, F.; Zheng, D.; Liu, J.; Gong, Y.; Guan, Z.; Lou, D. Depression and anxiety among adolescents during COVID-19: A cross-sectional study. Brain Behav. Immun. 2020, 88, 36. [Google Scholar] [CrossRef]
- Hyland, P.; Shevlin, M.; McBride, O.; Murphy, J.; Karatzias, T.; Bentall, R.P.; Martinez, A.; Vallières, F. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta Psychiatr. Scand. 2020, 142, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Mazza, M.G.; De Lorenzo, R.; Conte, C.; Poletti, S.; Vai, B.; Bollettini, I.; Melloni, E.M.T.; Furlan, R.; Ciceri, F.; Rovere-Querini, P. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav. Immun. 2020, 89, 594–600. [Google Scholar] [CrossRef]
- Obrenovic, B.; Du, J.; Godinic, D.; Baslom, M.M.M.; Tsoy, D. The threat of COVID-19 and job insecurity impact on depression and anxiety: An empirical study in the USA. Front. Psychol. 2021, 12, 648572. [Google Scholar] [CrossRef]
- Khudaykulov, A.; Changjun, Z.; Obrenovic, B.; Godinic, D.; Alsharif, H.Z.H.; Jakhongirov, I. The fear of COVID-19 and job insecurity impact on depression and anxiety: An empirical study in China in the COVID-19 pandemic aftermath. Curr. Psychol. 2022, 9, 1–14. [Google Scholar] [CrossRef]
- Henriksson, M.M.; Aro, H.M.; Marttunen, M.J.; Heikkinen, M.E.; Isometsa, E.; Kuoppasalmi, K.I.; Lonnqvist, J. Mental disorders and comorbidity in suicide. Am. J. Psychiatry 1993, 150, 935–940. [Google Scholar] [PubMed]
- Harwood, D.; Hawton, K.; Hope, T.; Jacoby, R. Psychiatric disorder and personality factors associated with suicide in older people: A descriptive and case-control study. Int. J. Geriatr. Psychiatry 2001, 16, 155–165. [Google Scholar] [CrossRef]
- Jeon, H.J. Depression and suicide. J. Korean Med. Assoc. 2011, 54, 370–375. [Google Scholar] [CrossRef] [Green Version]
- Stoudemire, A.; Frank, R.; Hedemark, N.; Kamlet, M.; Blazer, D. The economic burden of depression. Gen. Hosp. Psychiatry 1986, 8, 387–394. [Google Scholar] [CrossRef]
- Reiche, E.M.V.; Nunes, S.O.V.; Morimoto, H.K. Stress, depression, the immune system, and cancer. Lancet Oncol. 2004, 5, 617–625. [Google Scholar] [CrossRef]
- Beurel, E.; Toups, M.; Nemeroff, C.B. The bidirectional relationship of depression and inflammation: Double trouble. Neuron 2020, 107, 234–256. [Google Scholar] [CrossRef] [PubMed]
- Elliott, R.; Lythe, K.; Lee, R.; McKie, S.; Juhasz, G.; Thomas, E.J.; Downey, D.; Deakin, J.W.; Anderson, I.M. Reduced medial prefrontal responses to social interaction images in remitted depression. Arch. Gen. Psychiatry 2012, 69, 37–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nezlek, J.B.; Hampton, C.P.; Shean, G.D. Clinical depression and day-to-day social interaction in a community sample. J. Abnorm. Psychol. 2000, 109, 11. [Google Scholar] [CrossRef] [PubMed]
- Kawachi, I.; Berkman, L.F. Social ties and mental health. J. Urban Health 2001, 78, 458–467. [Google Scholar] [CrossRef] [Green Version]
- Mestdag, I.; Glorieux, I. Change and stability in commensality patterns: A comparative analysis of Belgian time-use data from 1966, 1999 and 2004. Sociol. Rev. 2009, 57, 703–726. [Google Scholar] [CrossRef]
- Choi, M.-J.; Park, Y.G.; Kim, Y.H.; Cho, K.H.; Nam, G.E. Eating together and health-related quality of life among Korean adults. J. Nutr. Educ. Behav. 2020, 52, 758–765. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Lee, E.; Lee, H. Characteristics of eating alone affecting the stress, depression, and suicidal ideation. Community Ment. Health J. 2020, 56, 1603–1609. [Google Scholar] [CrossRef] [PubMed]
- Kwak, Y.; Kim, Y. Association between mental health and meal patterns among elderly Koreans. Geriatr. Gerontol. Int. 2018, 18, 161–168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kang, Y.; Kang, S.; Kim, K.J.; Ko, H.; Shin, J.; Song, Y.-M. The association between family mealtime and depression in elderly Koreans. Korean J. Fam. Med. 2018, 39, 340. [Google Scholar] [CrossRef]
- Lee, S.A.; Park, E.-C.; Ju, Y.J.; Nam, J.Y.; Kim, T.H. Is one’s usual dinner companion associated with greater odds of depression? Using data from the 2014 Korean National Health and Nutrition Examination Survey. Int. J. Soc. Psychiatry 2016, 62, 560–568. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Patient Health Questionnaire Primary Care Study Group. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.-S.; Choi, J.-H.; Park, K.-H.; Joo, K.-J.; Ga, H.; Ko, H.-J.; Kim, S.-R. Standardization of the Korean version of Patient Health Questionnaire-9 as a screening instrument for major depressive disorder. J. Korean Acad. Fam. Med. 2007, 28, 114–119. [Google Scholar]
- An, J.Y.; Seo, E.R.; Lim, K.H.; Shin, J.H.; Kim, J.B. Standardization of the Korean version of screening tool for depression (Patient Health Questionnaire-9, PHQ-9). J. Korean Soc. Biol. Ther. Psychiatry 2013, 19, 47–56. [Google Scholar]
- Alexander, C.H. Still rolling: Leslie Kish’s “rolling samples” and the American Community Survey. Surv. Methodol. 2002, 28, 35–42. [Google Scholar]
- Son, Y.H.; Oh, S.S.; Jang, S.-I.; Park, E.-C.; Park, S.-H. Association between commensality with depression and suicidal ideation of Korean adults: The sixth and seventh Korean National Health and Nutrition Examination Survey, 2013, 2015, 2017. Nutr. J. 2020, 19, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Weissman, M.M.; Klerman, G.L. Sex differences and the epidemiology of depression. Arch. Gen. Psychiatry 1977, 34, 98–111. [Google Scholar] [CrossRef] [PubMed]
- Lynn, R.; Martin, T. Gender differences in extraversion, neuroticism, and psychoticism in 37 nations. J. Soc. Psychol. 1997, 137, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Cyranowski, J.M.; Frank, E.; Young, E.; Shear, M.K. Adolescent onset of the gender difference in lifetime rates of major depression: A theoretical model. Arch. Gen. Psychiatry 2000, 57, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Kendler, K.S.; Thornton, L.M.; Prescott, C.A. Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. Am. J. Psychiatry 2001, 158, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Belle, D. Gender Differences in the Social Moderators of Stress. In Stress and Coping: An Anthology; Columbia University Press: New York, NY, USA, 1991; pp. 258–274. [Google Scholar]
- Sobal, J.; Nelson, M.K. Commensal eating patterns: A community study. Appetite 2003, 41, 181–190. [Google Scholar] [CrossRef]
- Ferster, C.B. A functional analysis of depression. Am. Psychol. 1973, 28, 857. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coplan, R.J.; Zelenski, J.M.; Bowker, J.C. Leave Well Enough Alone? The Costs and Benefits of Solitude. In Subjective Well-Being and Life Satisfaction; Routledge: Oxfordshire, UK, 2017; pp. 129–147. [Google Scholar]
- Coplan, R.J.; Hipson, W.E.; Archbell, K.A.; Ooi, L.L.; Baldwin, D.; Bowker, J.C. Seeking more solitude: Conceptualization, assessment, and implications of aloneliness. Personal. Individ. Differ. 2019, 148, 17–26. [Google Scholar] [CrossRef]
- Vesnaver, E.; Keller, H.H. Social influences and eating behavior in later life: A review. J. Nutr. Gerontol. Geriatr. 2011, 30, 2–23. [Google Scholar] [CrossRef] [PubMed]
- Song, E.G.; Yoon, Y.S.; Yang, Y.J.; Lee, E.S.; Lee, J.H.; Lee, J.Y.; Park, W.J.; Park, S.Y. Factors associated with eating alone in Korean adults: Findings from the sixth Korea National Health and Nutrition Examination Survey, 2014. Korean J. Fam. Pract. 2017, 7, 698–706. [Google Scholar] [CrossRef]
- Dean, A.; Kolody, B.; Wood, P.; Matt, G.E. The influence of living alone on depression in elderly persons. J. Aging Health 1992, 4, 3–18. [Google Scholar] [CrossRef]
- Kessler, R.C.; Essex, M. Marital status and depression: The importance of coping resources. Soc. Forces 1982, 61, 484–507. [Google Scholar] [CrossRef]
- Ridley, M.; Rao, G.; Schilbach, F.; Patel, V. Poverty, depression, and anxiety: Causal evidence and mechanisms. Science 2020, 370, eaay0214. [Google Scholar] [CrossRef] [PubMed]
- LeMoult, J.; Gotlib, I.H. Depression: A cognitive perspective. Clin. Psychol. Rev. 2019, 69, 51–66. [Google Scholar] [CrossRef] [PubMed]
- Koster, E.H.; Hoorelbeke, K.; Onraedt, T.; Owens, M.; Derakshan, N. Cognitive control interventions for depression: A systematic review of findings from training studies. Clin. Psychol. Rev. 2017, 53, 79–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joormann, J.; Vanderlind, W.M. Emotion regulation in depression: The role of biased cognition and reduced cognitive control. Clin. Psychol. Sci. 2014, 2, 402–421. [Google Scholar] [CrossRef]
- De Jaegher, H.; Di Paolo, E.; Gallagher, S. Can social interaction constitute social cognition? Trends Cogn. Sci. 2010, 14, 441–447. [Google Scholar] [CrossRef]
- Lyketsos, C.G.; Olin, J. Depression in Alzheimer’s disease: Overview and treatment. Biol. Psychiatry 2002, 52, 243–252. [Google Scholar] [CrossRef]
- Bennett, D.A.; Schneider, J.A.; Tang, Y.; Arnold, S.E.; Wilson, R.S. The effect of social networks on the relation between Alzheimer’s disease pathology and level of cognitive function in old people: A longitudinal cohort study. Lancet Neurol. 2006, 5, 406–412. [Google Scholar] [CrossRef]
- Park, J.; Lee, G. Association of Eating Alone with Depressive Symptoms and Suicidal Ideation among Korean Adults. Korean J. Fam. Med. 2021, 42, 219. [Google Scholar] [CrossRef]
- Reijnders, J.S.; Ehrt, U.; Weber, W.E.; Aarsland, D.; Leentjens, A.F. A systematic review of prevalence studies of depression in Parkinson’s disease. Mov. Disord. 2008, 23, 183–189. [Google Scholar] [CrossRef] [Green Version]

| Variables | Male | Female | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Depression (PHQ ≥ 10) | No Depression (PHQ < 10) | p-Value | Total | Depressive (PHQ ≥ 10) | No Depression (PHQ < 10) | p-Value | |||||
| N | (%) | N | (%) | N | (%) | N | (%) | |||||
| Meals together | <0.0001 | <0.0001 | ||||||||||
| None | 426 | 46 | (10.8) | 380 | (89.2) | 818 | 98 | (12.0) | 720 | (88.0) | ||
| Once or more | 4273 | 87 | (2.0) | 4186 | (98.0) | 5538 | 236 | (4.3) | 5302 | (95.7) | ||
| Age | 0.3764 | <0.0001 | ||||||||||
| 19–29 | 462 | 10 | (2.2) | 452 | (97.8) | 463 | 27 | (5.8) | 436 | (94.2) | ||
| 30–39 | 521 | 20 | (3.8) | 501 | (96.2) | 868 | 39 | (4.5) | 829 | (95.5) | ||
| 40–49 | 758 | 18 | (2.4) | 740 | (97.6) | 1169 | 32 | (2.7) | 1137 | (97.3) | ||
| 50–59 | 898 | 22 | (2.4) | 876 | (97.6) | 1350 | 67 | (5.0) | 1283 | (95.0) | ||
| 60–69 | 1052 | 28 | (2.7) | 1024 | (97.3) | 1365 | 86 | (6.3) | 1279 | (93.7) | ||
| ≥70 | 1008 | 35 | (3.5) | 973 | (96.5) | 1141 | 83 | (7.3) | 1058 | (92.7) | ||
| Educational attainment | 0.0009 | <0.0001 | ||||||||||
| Middle school or below | 1101 | 48 | (4.4) | 1053 | (95.6) | 2275 | 182 | (8.0) | 2093 | (92.0) | ||
| High school | 1295 | 37 | (2.9) | 1258 | (97.1) | 1668 | 82 | (4.9) | 1586 | (95.1) | ||
| University or above | 2303 | 48 | (2.1) | 2255 | (97.9) | 2413 | 70 | (2.9) | 2343 | (97.1) | ||
| Equalized household income | <0.0001 | <0.0001 | ||||||||||
| Quartile 1 (low) | 810 | 61 | (7.5) | 749 | (92.5) | 1214 | 127 | (10.5) | 1087 | (89.5) | ||
| Quartile 2 | 1089 | 29 | (2.7) | 1060 | (97.3) | 1616 | 98 | (6.1) | 1518 | (93.9) | ||
| Quartile 3 | 1301 | 23 | (1.8) | 1278 | (98.2) | 1700 | 74 | (4.4) | 1626 | (95.6) | ||
| Quartile 4 (high) | 1499 | 20 | (1.3) | 1479 | (98.7) | 1826 | 35 | (1.9) | 1791 | (98.1) | ||
| Marital status | <0.0001 | <0.0001 | ||||||||||
| Married | 3653 | 82 | (2.2) | 3571 | (97.8) | 4601 | 189 | (4.1) | 4412 | (95.9) | ||
| Separated/divorced/widowed | 299 | 21 | (7.0) | 278 | (93.0) | 1158 | 109 | (9.4) | 1049 | (90.6) | ||
| Never married | 747 | 30 | (4.0) | 717 | (96.0) | 597 | 36 | (6.0) | 561 | (94.0) | ||
| Smoking status | 0.0112 | <0.0001 | ||||||||||
| Non-smoker | 1184 | 21 | (1.8) | 1163 | (98.2) | 5920 | 280 | (4.7) | 5640 | (95.3) | ||
| Smoker | 3515 | 112 | (3.2) | 3403 | (96.8) | 436 | 54 | (12.4) | 382 | (87.6) | ||
| Alcohol use status | 0.8974 | 0.2725 | ||||||||||
| No | 236 | 7 | (3.0) | 229 | (97.0) | 1151 | 68 | (5.9) | 1083 | (94.1) | ||
| Yes | 4463 | 126 | (2.8) | 4337 | (97.2) | 5205 | 266 | (5.1) | 4939 | (94.9) | ||
| Residential area | 0.7469 | 0.4644 | ||||||||||
| Urban | 2126 | 62 | (2.9) | 2064 | (97.1) | 2959 | 149 | (5.0) | 2810 | (95.0) | ||
| Rural | 2573 | 71 | (2.8) | 2502 | (97.2) | 3397 | 185 | (5.4) | 3212 | (94.6) | ||
| BMI | 0.0038 | 0.1007 | ||||||||||
| Underweight | 102 | 8 | (7.8) | 94 | (92.2) | 268 | 16 | (6.0) | 252 | (94.0) | ||
| Normal weight | 1456 | 52 | (3.6) | 1404 | (96.4) | 2829 | 141 | (5.0) | 2688 | (95.0) | ||
| Overweight | 1269 | 27 | (2.1) | 1242 | (97.9) | 1377 | 72 | (5.2) | 1305 | (94.8) | ||
| Obesity | 1649 | 41 | (2.5) | 1608 | (97.5) | 1595 | 80 | (5.0) | 1515 | (95.0) | ||
| Severe obesity | 223 | 5 | (2.2) | 218 | (97.8) | 287 | 25 | (8.7) | 262 | (91.3) | ||
| Number of household members | <0.0001 | <0.0001 | ||||||||||
| 1 | 421 | 30 | (7.1) | 391 | (92.9) | 762 | 73 | (9.6) | 689 | (90.4) | ||
| 2 | 1635 | 49 | (3.0) | 1586 | (97.0) | 1986 | 114 | (5.7) | 1872 | (94.3) | ||
| More than 2 | 2643 | 54 | (2.0) | 2589 | (98.0) | 3608 | 147 | (4.1) | 3461 | (95.9) | ||
| Physical activity | 0.2715 | 0.7956 | ||||||||||
| Low | 1812 | 56 | (3.1) | 1756 | (96.9) | 2846 | 155 | (5.4) | 2691 | (94.6) | ||
| Moderate | 2041 | 60 | (2.9) | 1981 | (97.1) | 2852 | 144 | (5.0) | 2708 | (95.0) | ||
| High | 846 | 17 | (2.0) | 829 | (98.0) | 658 | 35 | (5.3) | 623 | (94.7) | ||
| Year | 0.6128 | 0.0005 | ||||||||||
| 2014 | 1170 | 38 | (3.2) | 1132 | (96.8) | 1650 | 115 | (7.0) | 1535 | (93.0) | ||
| 2016 | 1253 | 38 | (3.0) | 1215 | (97.0) | 1737 | 94 | (5.4) | 1643 | (94.6) | ||
| 2018 | 1310 | 33 | (2.5) | 1277 | (97.5) | 1740 | 66 | (3.8) | 1674 | (96.2) | ||
| 2020 | 966 | 24 | (2.5) | 942 | (97.5) | 1229 | 59 | (4.8) | 1170 | (95.2) | ||
| Participants | 4699 | 133 | (2.8) | 4566 | (97.2) | 6356 | 334 | (5.3) | 6022 | (94.7) | ||
| Variables | Male | Female | ||
|---|---|---|---|---|
| Depression (PHQ ≥ 10) | Depression (PHQ ≥ 10) | |||
| Adjusted OR | 95% CI | Adjusted OR | 95% CI | |
| Meals together | ||||
| None | 1.00 | 1.00 | ||
| Once or more | 0.26 | (0.15–0.45) | 0.50 | (0.34–0.74) |
| Age | ||||
| 19–29 | 1.00 | 1.00 | ||
| 30–39 | 3.03 | (1.23–7.48) | 0.69 | (0.27–1.78) |
| 40–49 | 1.37 | (0.53–3.58) | 0.44 | (0.17–1.12) |
| 50–59 | 1.31 | (0.48–3.56) | 0.64 | (0.25–1.62) |
| 60-69 | 0.72 | (0.27–1.93) | 0.48 | (0.18–1.29) |
| ≥70 | 0.61 | (0.21–1.76) | 0.33 | (0.12–0.90) |
| Educational attainment | ||||
| Middle school or below | 1.00 | 1.00 | ||
| High school | 1.04 | (0.61–1.76) | 0.64 | (0.42–0.98) |
| University or above | 0.71 | (0.40–1.26) | 0.33 | (0.19–0.56) |
| Equalized household income | ||||
| Quartile 1 (low) | 1.00 | 1.00 | ||
| Quartile 2 | 0.27 | (0.15–0.49) | 0.71 | (0.48–1.04) |
| Quartile 3 | 0.21 | (0.11–0.41) | 0.51 | (0.33–0.79) |
| Quartile 4 (high) | 0.21 | (0.10–0.43) | 0.28 | (0.17–0.48) |
| Marital status | ||||
| Married | 1.00 | 1.00 | ||
| Separated/divorced/widowed | 1.25 | (0.56–2.80) | 1.47 | (1.03–2.09) |
| Never married | 1.44 | (0.73–2.81) | 1.50 | (0.69–3.31) |
| Smoking status | ||||
| Non-smoker | 1.00 | 1.00 | ||
| Smoker | 2.07 | (1.11–3.87) | 2.77 | (1.90–4.06) |
| Alcohol use status | ||||
| No | 1.00 | 1.00 | ||
| Yes | 0.88 | (0.32–2.46) | 0.95 | (0.68–1.34) |
| Residential area | ||||
| Urban | 1.00 | 1.00 | ||
| Rural | 0.71 | (0.47–1.09) | 1.06 | (0.79–1.42) |
| BMI | ||||
| Underweight | 1.97 | (0.61–6.32) | 1.32 | (0.71–2.43) |
| Normal weight | 1.00 | 1.00 | ||
| Overweight | 0.56 | (0.31–1.01) | 0.95 | (0.67–1.35) |
| Obesity | 0.81 | (0.48–1.37) | 0.88 | (0.61–1.26) |
| Severe obesity | 0.58 | (0.23–1.49) | 1.36 | (0.76–2.46) |
| Number of family members | ||||
| 1 | 1.00 | 1.00 | ||
| 2 | 0.91 | (0.42–1.95) | 1.42 | (0.91–2.22) |
| More than 2 | 1.00 | (0.47–2.13) | 1.56 | (0.96–2.54) |
| Physical activity | ||||
| Low | 1.00 | 1.00 | ||
| Moderate | 0.80 | (0.43–1.50) | 1.07 | (0.66–1.72) |
| High | 0.99 | (0.62–1.57) | 0.93 | (0.69–1.25) |
| Year | ||||
| 2014 | 1.85 | (1.05–3.25) | 1.84 | (1.21–2.80) |
| 2016 | 1.44 | (0.78–2.65) | 1.40 | (0.93–2.11) |
| 2018 | 1.00 | 1.00 | ||
| 2020 | 1.56 | (0.79–3.08) | 1.33 | (0.84–2.10) |
| Variables | Male | Female | ||||
|---|---|---|---|---|---|---|
| Meals Alone | Meals Together | Meals Alone | Meals Together | |||
| Adjusted OR | Adjusted OR | 95% CI | Adjusted OR | Adjusted OR | 95% CI | |
| Age | ||||||
| 19–29 | 1.00 | 0.07 | (0.01–0.37) | 1.00 | 0.12 | (0.02–0.70) |
| 30–39 | 1.00 | 0.41 | (0.06–2.68) | 1.00 | 0.52 | (0.13–2.17) |
| 40–49 | 1.00 | 0.42 | (0.08–2.11) | 1.00 | 0.26 | (0.08–0.89) |
| 50–59 | 1.00 | 0.29 | (0.10–0.87) | 1.00 | 0.69 | (0.28–1.69) |
| 60–69 | 1.00 | 0.10 | (0.03–0.35) | 1.00 | 0.45 | (0.23–0.87) |
| ≥70 | 1.00 | 0.18 | (0.08–0.44) | 1.00 | 0.49 | (0.25–0.97) |
| Educational attainment | ||||||
| Middle school or below | 1.00 | 0.16 | (0.07–0.39) | 1.00 | 0.51 | (0.32–0.81) |
| High school | 1.00 | 0.34 | (0.12–0.96) | 1.00 | 0.60 | (0.23–1.59) |
| University or above | 1.00 | 0.21 | (0.08–0.54) | 1.00 | 0.40 | (0.15–1.08) |
| Equalized household income | ||||||
| Quartile 1 (low) | 1.00 | 0.16 | (0.06–0.47) | 1.00 | 0.58 | (0.30–1.09) |
| Quartile 2 | 1.00 | 0.41 | (0.14–1.23) | 1.00 | 0.40 | (0.21–0.79) |
| Quartile 3 | 1.00 | 0.13 | (0.03–0.53) | 1.00 | 0.30 | (0.13–0.68) |
| Quartile 4 (high) | 1.00 | 0.27 | (0.08–0.94) | 1.00 | 0.42 | (0.08–2.15) |
| Marital status | ||||||
| Married | 1.00 | 0.37 | (0.16–0.83) | 1.00 | 0.61 | (0.34–1.10) |
| Separated/divorced/widowed | 1.00 | 0.02 | (0.00–0.30) | 1.00 | 0.44 | (0.25–0.79) |
| Never married | 1.00 | 0.20 | (0.07–0.51) | 1.00 | 0.26 | (0.06–1.13) |
| Smoking status | ||||||
| Non-smoker | 1.00 | 0.15 | (0.05–0.46) | 1.00 | 0.45 | (0.29–0.69) |
| Smoker | 1.00 | 0.30 | (0.16–0.56) | 1.00 | 0.89 | (0.35–2.26) |
| Alcohol use status | ||||||
| No | 1.00 | 0.08 | (<0.001–>999.999) | 1.00 | 0.54 | (0.25–1.18) |
| Yes | 1.00 | 0.24 | (0.13–0.43) | 1.00 | 0.50 | (0.32–0.79) |
| Residential area | ||||||
| Urban | 1.00 | 0.17 | (0.07–0.41) | 1.00 | 0.47 | (0.25–0.86) |
| Rural | 1.00 | 0.33 | (0.16–0.71) | 1.00 | 0.57 | (0.33–0.97) |
| BMI | ||||||
| Underweight | 1.00 | 220.86 | (0.98–>999.999) | 1.00 | 0.10 | (0.01–0.91) |
| Normal weight | 1.00 | 0.12 | (0.05–0.30) | 1.00 | 0.40 | (0.22–0.74) |
| Overweight | 1.00 | 0.16 | (0.05–0.52) | 1.00 | 0.90 | (0.45–1.81) |
| Obesity | 1.00 | 0.37 | (0.12–1.14) | 1.00 | 0.37 | (0.17–0.83) |
| Severe obesity | 1.00 | 0.07 | (0.01–0.73) | 1.00 | 0.77 | (0.23–2.57) |
| Number of household members | ||||||
| 1 | 1.00 | 0.13 | (0.05–0.39) | 1.00 | 0.34 | (0.15–0.79) |
| 2 | 1.00 | 0.42 | (0.14–1.30) | 1.00 | 0.59 | (0.32–1.10) |
| More than 2 | 1.00 | 0.19 | (0.08–0.43) | 1.00 | 0.48 | (0.24–0.97) |
| Physical activity | ||||||
| Low | 1.00 | 0.04 | (0.01–0.23) | 1.00 | 1.60 | (0.37–6.89) |
| Moderate | 1.00 | 0.55 | (0.22–1.38) | 1.00 | 0.33 | (0.18–0.62) |
| High | 1.00 | 0.14 | (0.05–0.38) | 1.00 | 0.65 | (0.38–1.13) |
| Year | ||||||
| 2014 | 1.00 | 0.52 | (0.14–1.90) | 1.00 | 0.43 | (0.22–0.86) |
| 2016 | 1.00 | 0.05 | (0.02–0.16) | 1.00 | 0.68 | (0.29–1.64) |
| 2018 | 1.00 | 0.77 | (0.21–2.86) | 1.00 | 0.29 | (0.14–0.61) |
| 2020 | 1.00 | 0.14 | (0.04–0.48) | 1.00 | 0.80 | (0.38–1.67) |
| Meals Together | Male | Female | |||
|---|---|---|---|---|---|
| Depression (PHQ ≥ 10) | Depression (PHQ ≥ 10) | ||||
| Adjusted OR | 95% CI | Adjusted OR | 95% CI | ||
| Breakfast together | |||||
| No | 1.00 | 1.00 | |||
| Yes | |||||
| With family | 0.87 | (0.52–1.44) | 0.91 | (0.67–1.23) | |
| With people other than family | 1.12 | (0.39–3.16) | 0.50 | (0.16–1.61) | |
| Lunch together | |||||
| No | 1.00 | 1.00 | |||
| Yes | |||||
| With family | 0.66 | (0.38–1.13) | 1.07 | (0.75–1.53) | |
| With people other than family | 0.33 | (0.20–0.55) | 0.63 | (0.42–0.94) | |
| Dinner together | |||||
| No | 1.00 | 1.00 | |||
| Yes | |||||
| With family | 0.46 | (0.27–0.79) | 0.63 | (0.43–0.90) | |
| With people other than family | 0.25 | (0.09–0.68) | 0.70 | (0.37–1.33) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, H.; Ryu, J.; Choi, J.; Kim, H.; Park, E. Association between Dining with Companions and Depression among Korean Adults. Nutrients 2022, 14, 2834. https://doi.org/10.3390/nu14142834
Jung H, Ryu J, Choi J, Kim H, Park E. Association between Dining with Companions and Depression among Korean Adults. Nutrients. 2022; 14(14):2834. https://doi.org/10.3390/nu14142834
Chicago/Turabian StyleJung, Hankyo, Jin Ryu, Junhui Choi, Hyunkyu Kim, and Euncheol Park. 2022. "Association between Dining with Companions and Depression among Korean Adults" Nutrients 14, no. 14: 2834. https://doi.org/10.3390/nu14142834
APA StyleJung, H., Ryu, J., Choi, J., Kim, H., & Park, E. (2022). Association between Dining with Companions and Depression among Korean Adults. Nutrients, 14(14), 2834. https://doi.org/10.3390/nu14142834








