Skipping Breakfast and Incidence of Frequent Alcohol Drinking in University Students in Japan: A Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
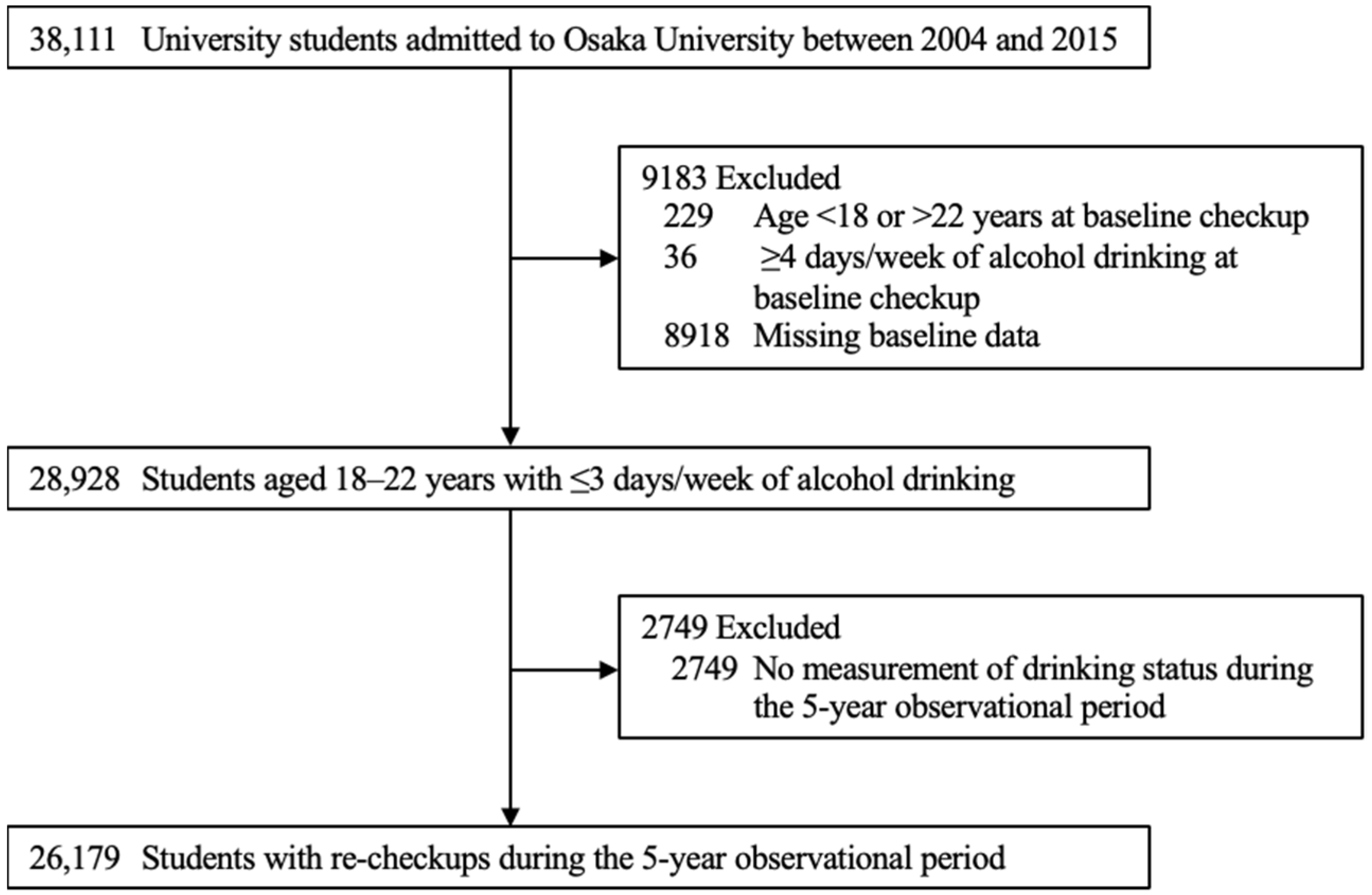
2.1. Participants
2.2. Measurements
2.3. Statistical Analysis
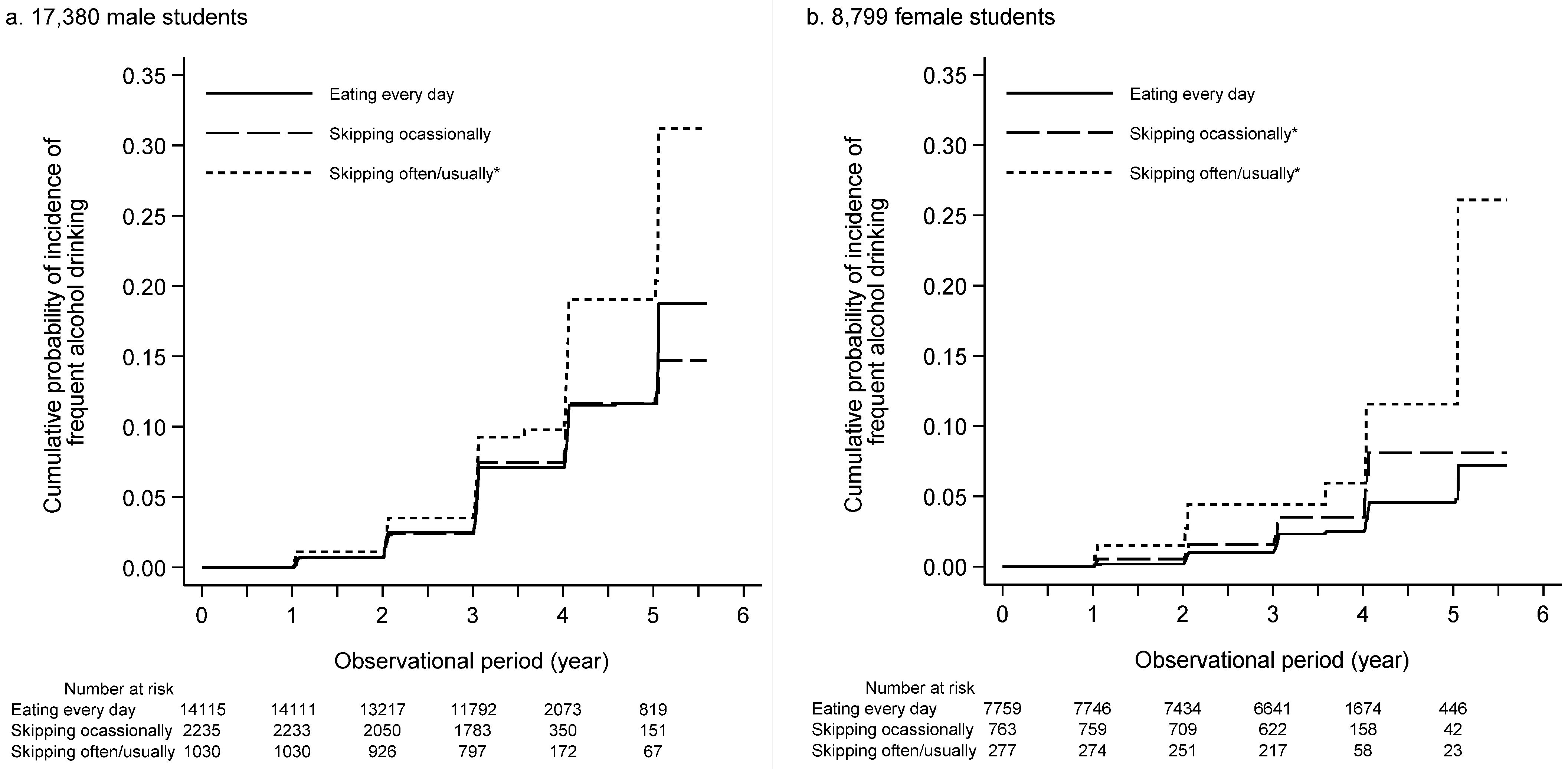
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Isaacs, J.Y.; Smith, M.M.; Sherry, S.B.; Seno, M.; Moore, M.L.; Stewart, S.H. Alcohol Use and Death by Suicide: A Meta-Analysis of 33 Studies. Suicide Life Threat. Behav. 2022. [Google Scholar] [CrossRef] [PubMed]
- Roerecke, M.; Rehm, J. Cause-Specific Mortality Risk in Alcohol Use Disorder Treatment Patients: A Systematic Review and Meta-Analysis. Int. J. Epidemiol. 2014, 43, 906–919. [Google Scholar] [CrossRef] [PubMed]
- Roerecke, M.; Vafaei, A.; Hasan, O.S.M.; Chrystoja, B.R.; Cruz, M.; Lee, R.; Neuman, M.G.; Rehm, J. Alcohol Consumption and Risk of Liver Cirrhosis: A Systematic Review and Meta-Analysis. Am. J. Gastroenterol. 2019, 114, 1574–1586. [Google Scholar] [CrossRef] [PubMed]
- Roerecke, M.; Rehm, J. Alcohol Consumption, Drinking Patterns, and Ischemic Heart Disease: A Narrative Review of Meta-Analyses and a Systematic Review and Meta-Analysis of the Impact of Heavy Drinking Occasions on Risk for Moderate Drinkers. BMC Med. 2014, 12, 182. [Google Scholar] [CrossRef] [Green Version]
- Bagnardi, V.; Rota, M.; Botteri, E.; Tramacere, I.; Islami, F.; Fedirko, V.; Scotti, L.; Jenab, M.; Turati, F.; Pasquali, E.; et al. Alcohol Consumption and Site-Specific Cancer Risk: A Comprehensive Dose–Response Meta-Analysis. Br. J. Cancer 2015, 112, 580–593. [Google Scholar] [CrossRef]
- Wechsler, H.; Davenport, A.; Dowdall, G.; Moeykens, B.; Castillo, S. Health and Behavioral Consequences of Binge Drinking in College. A National Survey of Students at 140 Campuses. JAMA 1994, 272, 1672–1677. [Google Scholar] [CrossRef]
- Wechsler, H.; Lee, J.E.; Kuo, M.; Seibring, M.; Nelson, T.F.; Lee, H. Trends in College Binge Drinking during a Period of Increased Prevention Efforts. Findings from 4 Harvard School of Public Health College Alcohol Study Surveys: 1993–2001. J. Am. Coll. Health 2002, 50, 203–217. [Google Scholar] [CrossRef]
- Dodd, L.J.; Al-Nakeeb, Y.; Nevill, A.; Forshaw, M.J. Lifestyle Risk Factors of Students: A Cluster Analytical Approach. Prev. Med. 2010, 51, 73–77. [Google Scholar] [CrossRef]
- Zysset, A.; Volken, T.; Amendola, S.; Von Wyl, A.; Dratva, J. Change in Alcohol Consumption and Binge Drinking in University Students During the Early COVID-19 Pandemic. Front. Public Health 2022, 10, 854350. [Google Scholar] [CrossRef]
- Ji, C.-Y.; Hu, P.-J.; Song, Y. The Epidemiology of Alcohol Consumption and Misuse among Chinese College Students. Alcohol Alcohol. 2012, 47, 464–472. [Google Scholar] [CrossRef]
- Kawaida, K.; Yoshimoto, H.; Morita, N.; Ogai, Y.; Saito, T. The Prevalence of Binge Drinking and Alcohol-Related Consequences and Their Relationship among Japanese College Students. Tohoku J. Exp. Med. 2021, 254, 41–47. [Google Scholar] [CrossRef] [PubMed]
- White, A.; Hingson, R. The Burden of Alcohol Use: Excessive Alcohol Consumption and Related Consequences among College Students. Alcohol Res. 2013, 35, 201–218. [Google Scholar]
- Gill, J.S. Reported Levels of Alcohol Consumption and Binge Drinking within the UK Undergraduate Student Population over the Last 25 Years. Alcohol Alcohol. 2002, 37, 109–120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hingson, R.W.; Zha, W.; Weitzman, E.R. Magnitude of and Trends in Alcohol-Related Mortality and Morbidity among U.S. College Students Ages 18–24, 1998–2005. J. Stud. Alcohol Drugs Suppl. 2009, s16, 12–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCabe, S.E.; Cranford, J.A.; Boyd, C.J. The Relationship between Past-Year Drinking Behaviors and Nonmedical Use of Prescription Drugs: Prevalence of Co-Occurrence in a National Sample. Drug Alcohol Depend. 2006, 84, 281–288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- White, A.M.; Jamieson-Drake, D.W.; Swartzwelder, H.S. Prevalence and Correlates of Alcohol-Induced Blackouts among College Students: Results of an e-Mail Survey. J. Am. Coll. Health 2002, 51, 117–131. [Google Scholar] [CrossRef]
- Wetherill, R.R.; Schnyer, D.M.; Fromme, K. Acute Alcohol Effects on Contextual Memory BOLD Response: Differences Based on Fragmentary Blackout History. Alcohol. Clin. Exp. Res. 2012, 36, 1108–1115. [Google Scholar] [CrossRef]
- Jia-Richards, M.; Sexton, J.N.; Dolan, S.L. Predicting Alcohol Use with Subjective and Objective Measures of Cognitive Function in Healthy College Students. J. Am. Coll. Health 2021, 6, 1–9. [Google Scholar] [CrossRef]
- Paradis, C.; Demers, A.; Picard, E.; Graham, K. The Importance of Drinking Frequency in Evaluating Individuals’ Drinking Patterns: Implications for the Development of National Drinking Guidelines. Addiction 2009, 104, 1179–1184. [Google Scholar] [CrossRef]
- Shinozaki, N.; Murakami, K.; Asakura, K.; Masayasu, S.; Sasaki, S. Identification of Dish-Based Dietary Patterns for Breakfast, Lunch, and Dinner and Their Diet Quality in Japanese Adults. Nutrients 2020, 13, 67. [Google Scholar] [CrossRef]
- Odegaard, A.O.; Jacobs, D.R.; Steffen, L.M.; Van Horn, L.; Ludwig, D.S.; Pereira, M.A. Breakfast Frequency and Development of Metabolic Risk. Diabetes Care 2013, 36, 3100–3106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cayres, S.U.; Júnior, I.F.F.; Barbosa, M.F.; Christofaro, D.G.D.; Fernandes, R.A. Breakfast Frequency, Adiposity, and Cardiovascular Risk Factors as Markers in Adolescents. Cardiol. Young 2016, 26, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Bonnet, J.P.; Cardel, M.I.; Cellini, J.; Hu, F.B.; Guasch-Ferré, M. Breakfast Skipping, Body Composition, and Cardiometabolic Risk: A Systematic Review and Meta-Analysis of Randomized Trials. Obesity 2020, 28, 1098–1109. [Google Scholar] [CrossRef]
- Ballon, A.; Neuenschwander, M.; Schlesinger, S. Breakfast Skipping Is Associated with Increased Risk of Type 2 Diabetes among Adults: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. J. Nutr. 2019, 149, 106–113. [Google Scholar] [CrossRef] [PubMed]
- Tomi, R.; Yamamoto, R.; Shinzawa, M.; Kimura, Y.; Fujii, Y.; Aoki, K.; Ozaki, S.; Yoshimura, R.; Taneike, M.; Nakanishi, K.; et al. Frequency of Breakfast, Lunch, and Dinner and Incidence of Proteinuria: A Retrospective Cohort Study. Nutrients 2020, 12, 3549. [Google Scholar] [CrossRef]
- Takagi, H.; Hari, Y.; Nakashima, K.; Kuno, T.; Ando, T. ALICE (All-Literature Investigation of Cardiovascular Evidence) Group Meta-Analysis of Relation of Skipping Breakfast With Heart Disease. Am. J. Cardiol. 2019, 124, 978–986. [Google Scholar] [CrossRef]
- Pendergast, F.J.; Livingstone, K.M.; Worsley, A.; McNaughton, S.A. Correlates of Meal Skipping in Young Adults: A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 125. [Google Scholar] [CrossRef] [Green Version]
- Malinauskas, B.M.; Raedeke, T.D.; Aeby, V.G.; Smith, J.L.; Dallas, M.B. Dieting Practices, Weight Perceptions, and Body Composition: A Comparison of Normal Weight, Overweight, and Obese College Females. Nutr. J. 2006, 5, 11. [Google Scholar] [CrossRef] [Green Version]
- Telleria-Aramburu, N.; Arroyo-Izaga, M. Risk Factors of Overweight/Obesity-Related Lifestyles in University Students: Results from the EHU12/24 Study. Br. J. Nutr. 2022, 127, 914–926. [Google Scholar] [CrossRef]
- Rodríguez-Muñoz, P.M.; Carmona-Torres, J.M.; Rivera-Picón, C.; Fabbian, F.; Manfredini, R.; Rodríguez-Borrego, M.A.; López-Soto, P.J. Associations between Chronotype, Adherence to the Mediterranean Diet and Sexual Opinion among University Students. Nutrients 2020, 12, 1900. [Google Scholar] [CrossRef]
- Lovell, G.P.; Nash, K.; Sharman, R.; Lane, B.R. A Cross-Sectional Investigation of Depressive, Anxiety, and Stress Symptoms and Health-Behavior Participation in Australian University Students. Nurs. Health Sci. 2015, 17, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Tang, L.; Chen, L.; Kaminga, A.C.; Xu, H. Prevalence and Risk Factors Associated with Primary Dysmenorrhea among Chinese Female University Students: A Cross-Sectional Study. J. Pediatr. Adolesc. Gynecol. 2020, 33, 15–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ren, Z.; Cao, J.; Cheng, P.; Shi, D.; Cao, B.; Yang, G.; Liang, S.; Du, F.; Su, N.; Yu, M.; et al. Association between Breakfast Consumption and Depressive Symptoms among Chinese College Students: A Cross-Sectional and Prospective Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 1571. [Google Scholar] [CrossRef] [Green Version]
- Yamamoto, R.; Tomi, R.; Shinzawa, M.; Yoshimura, R.; Ozaki, S.; Nakanishi, K.; Ide, S.; Nagatomo, I.; Nishida, M.; Yamauchi-Takihara, K.; et al. Associations of Skipping Breakfast, Lunch, and Dinner with Weight Gain and Overweight/Obesity in University Students: A Retrospective Cohort Study. Nutrients 2021, 13, 271. [Google Scholar] [CrossRef]
- Fujiwara, T.; Ono, M.; Iizuka, T.; Sekizuka-Kagami, N.; Maida, Y.; Adachi, Y.; Fujiwara, H.; Yoshikawa, H. Breakfast Skipping in Female College Students Is a Potential and Preventable Predictor of Gynecologic Disorders at Health Service Centers. Diagnostics 2020, 10, 476. [Google Scholar] [CrossRef] [PubMed]
- Keski-Rahkonen, A.; Kaprio, J.; Rissanen, A.; Virkkunen, M.; Rose, R.J. Breakfast Skipping and Health-Compromising Behaviors in Adolescents and Adults. Eur. J. Clin. Nutr. 2003, 57, 842–853. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rampersaud, G.C.; Pereira, M.A.; Girard, B.L.; Adams, J.; Metzl, J.D. Breakfast Habits, Nutritional Status, Body Weight, and Academic Performance in Children and Adolescents. J. Am. Diet. Assoc. 2005, 105, 743–760. [Google Scholar] [CrossRef]
- Pengpid, S.; Peltzer, K. Skipping Breakfast and Its Association with Health Risk Behaviour and Mental Health Among University Students in 28 Countries. Diabetes Metab. Syndr. Obes. 2020, 13, 2889–2897. [Google Scholar] [CrossRef]
- Wang, M.; Zhong, J.-M.; Wang, H.; Zhao, M.; Gong, W.-W.; Pan, J.; Fei, F.-R.; Wu, H.-B.; Yu, M. Breakfast Consumption and Its Associations with Health-Related Behaviors among School-Aged Adolescents: A Cross-Sectional Study in Zhejiang Province, China. Int. J. Environ. Res. Public Health 2016, 13, 761. [Google Scholar] [CrossRef] [Green Version]
- Pendergast, F.J.; Livingstone, K.M.; Worsley, A.; McNaughton, S.A. Examining the Correlates of Meal Skipping in Australian Young Adults. Nutr. J. 2019, 18, 24. [Google Scholar] [CrossRef] [Green Version]
- Woolard, R.; Liu, J.; Parsa, M.; Merriman, G.; Tarwater, P.; Alba, I.; Villalobos, S.; Ramos, R.; Bernstein, J.; Bernstein, E.; et al. Smoking Is Associated with Increased Risk of Binge Drinking in a Young Adult Hispanic Population at the US-Mexico Border. Subst. Abus. 2015, 36, 318–324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pelletier, J.E.; Lytle, L.A.; Laska, M.N. Stress, Health Risk Behaviors, and Weight Status Among Community College Students. Health Educ. Behav. 2015, 43, 139–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.; Feeley, T.H. Predicting Binge Drinking in College Students: Rational Beliefs, Stress, or Loneliness? J. Drug Educ. 2015, 45, 133–155. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Chiappe, N.; Lara-Monsalve, P.A.; Gómez, A.M.; Gómez, D.C.; González, J.C.; González, L.; Gutiérrez-Prieto, J.E.; Jaimes-Reyes, M.A.; González, L.D.; Castillo, J.S. Poor Sleep Quality and Associated Factors in University Students in Bogotá D.C., Colombia. Sleep Sci. 2020, 13, 125–130. [Google Scholar]
- Popovici, I.; French, M.T. Binge Drinking and Sleep Problems among Young Adults. Drug Alcohol Depend. 2013, 132, 207–215. [Google Scholar] [CrossRef] [Green Version]
- Bartoli, F.; Carretta, D.; Crocamo, C.; Schivalocchi, A.; Brambilla, G.; Clerici, M.; Carrà, G. Prevalence and Correlates of Binge Drinking among Young Adults Using Alcohol: A Cross-Sectional Survey. BioMed Res. Int. 2014, 2014, 930795. [Google Scholar] [CrossRef]
- Gong, W.-J.; Fong, D.Y.-T.; Wang, M.-P.; Lam, T.-H.; Chung, T.W.-H.; Ho, S.-Y. Skipping Breakfast and Eating Breakfast Away from Home Were Prospectively Associated with Emotional and Behavioral Problems in 115,217 Chinese Adolescents. J. Epidemiol. 2021. [Google Scholar] [CrossRef]
- Miki, T.; Eguchi, M.; Kuwahara, K.; Kochi, T.; Akter, S.; Kashino, I.; Hu, H.; Kurotani, K.; Kabe, I.; Kawakami, N.; et al. Breakfast Consumption and the Risk of Depressive Symptoms: The Furukawa Nutrition and Health Study. Psychiatry Res. 2019, 273, 551–558. [Google Scholar] [CrossRef]
- Sihvola, E.; Rose, R.J.; Dick, D.M.; Pulkkinen, L.; Marttunen, M.; Kaprio, J. Early-Onset Depressive Disorders Predict the Use of Addictive Substances in Adolescence: A Prospective Study of Adolescent Finnish Twins. Addiction 2008, 103, 2045–2053. [Google Scholar] [CrossRef] [Green Version]
- Huurre, T.; Lintonen, T.; Kaprio, J.; Pelkonen, M.; Marttunen, M.; Aro, H. Adolescent Risk Factors for Excessive Alcohol Use at Age 32 Years. A 16-Year Prospective Follow-up Study. Soc. Psychiatry Psychiatr. Epidemiol. 2010, 45, 125–134. [Google Scholar] [CrossRef]
- McKenzie, M.; Jorm, A.F.; Romaniuk, H.; Olsson, C.A.; Patton, G.C. Association of Adolescent Symptoms of Depression and Anxiety with Alcohol Use Disorders in Young Adulthood: Findings from the Victorian Adolescent Health Cohort Study. Med. J. Aust. 2011, 195, S27–S30. [Google Scholar] [CrossRef] [PubMed]
- Mushquash, A.R.; Stewart, S.H.; Sherry, S.B.; Sherry, D.L.; Mushquash, C.J.; Mackinnon, A.L. Depressive Symptoms Are a Vulnerability Factor for Heavy Episodic Drinking: A Short-Term, Four-Wave Longitudinal Study of Undergraduate Women. Addict. Behav. 2013, 38, 2180–2186. [Google Scholar] [CrossRef] [PubMed]
| Breakfast Frequency | All | Eating Every Day | Skipping Occasionally | Skipping Often/Usually |
|---|---|---|---|---|
| Number | 17,380 | 14,115 | 2235 | 1030 |
| Age: 18 years, n (%) | 11,280 (64.9) | 9398 (66.6) | 1312 (58.7) | 570 (55.3) |
| 19 | 5583 (32.1) | 4386 (31.1) | 808 (36.2) | 389 (37.8) |
| 20 | 378 (2.2) | 259 (1.8) | 80 (3.6) | 39 (3.8) |
| 21 | 99 (0.6) | 51 (0.4) | 24 (1.1) | 24 (2.3) |
| 22 | 40 (0.2) | 21 (0.2) | 11 (0.5) | 8 (0.8) |
| Body mass index, kg/m2 | 21.6 ± 2.9 | 21.6 ± 2.9 | 21.5 ± 2.9 | 21.2 ± 2.9 |
| Smokers, n (%) | 45 (0.3) | 20 (0.1) | 18 (0.8) | 7 (0.7) |
| Drinkers, n (%) | 1578 (9.1) | 1107 (7.8) | 304 (13.6) | 167 (16.2) |
| Sleep duration: <5 h, n (%) | 536 (3.1) | 417 (3.0) | 68 (3.0) | 51 (5.0) |
| 5–6 | 5540 (31.9) | 4519 (32.0) | 698 (31.2) | 323 (31.4) |
| 6–7 | 8401 (48.3) | 6910 (49.0) | 1058 (47.3) | 433 (42.0) |
| 7–8 | 2487 (14.3) | 1995 (14.1) | 323 (14.5) | 169 (16.4) |
| ≥8 | 416 (2.4) | 274 (1.9) | 88 (3.9) | 54 (5.2) |
| Living arrangement: | ||||
| Living with family, n (%) | 8341 (48.0) | 6939 (49.2) | 931 (41.7) | 471 (45.7) |
| Living alone | 7726 (44.5) | 6133 (43.5) | 1112 (49.8) | 481 (46.7) |
| Living in dormitory | 1083 (6.2) | 860 (6.1) | 157 (7.0) | 66 (6.4) |
| Other living arrangements | 230 (1.3) | 183 (1.3) | 35 (1.6) | 12 (1.2) |
| Stress frequency: rarely, n (%) | 4499 (25.9) | 3761 (26.6) | 495 (22.1) | 243 (23.6) |
| sometimes | 10,110 (58.2) | 8206 (58.1) | 1341 (60.0) | 563 (54.7) |
| often | 2431 (14.0) | 1899 (13.5) | 347 (15.5) | 185 (18.0) |
| always | 340 (2.0) | 249 (1.8) | 52 (2.3) | 39 (3.8) |
| Breakfast Frequency | All | Eating Every Day | Skipping Occasionally | Skipping Often/Usually |
|---|---|---|---|---|
| Number | 8799 | 7759 | 763 | 277 |
| Age: 18 years, n (%) | 6524 (74.1) | 5822 (75.0) | 534 (70.0) | 168 (60.6) |
| 19 | 2047 (23.3) | 1785 (23.0) | 187 (24.5) | 75 (27.1) |
| 20 | 157 (1.8) | 111 (1.4) | 25 (3.3) | 21 (7.6) |
| 21 | 47 (0.5) | 26 (0.3) | 11 (1.4) | 10 (3.6) |
| 22 | 24 (0.3) | 15 (0.2) | 6 (0.8) | 3 (1.1) |
| Body mass index, kg/m2 | 20.5 ± 2.4 | 20.5 ± 2.4 | 20.3 ± 2.4 | 20.4 ± 2.4 |
| Smokers, n (%) | 9 (0.1) | 6 (0.1) | 2 (0.3) | 1 (0.4) |
| Drinkers, n (%) | 393 (4.5) | 298 (3.8) | 59 (7.7) | 36 (13.0) |
| Sleep duration: <5 h, n (%) | 267 (3.0) | 214 (2.8) | 35 (4.6) | 18 (6.5) |
| 5–6 | 3144 (35.7) | 2779 (35.8) | 273 (35.8) | 92 (33.2) |
| 6–7 | 4181 (47.5) | 3734 (48.1) | 336 (44.0) | 111 (40.1) |
| 7–8 | 1090 (12.4) | 944 (12.2) | 103 (13.5) | 43 (15.5) |
| ≥8 | 117 (1.3) | 88 (1.1) | 16 (2.1) | 13 (4.7) |
| Living arrangement: | ||||
| Living with family, n (%) | 4586 (52.1) | 4103 (52.9) | 349 (45.7) | 134 (48.4) |
| Living alone | 3396 (38.6) | 2944 (37.9) | 331 (43.4) | 121 (43.7) |
| Living in dormitory | 616 (7.0) | 534 (6.9) | 66 (8.7) | 16 (5.8) |
| Other living arrangements | 201 (2.3) | 178 (2.3) | 17 (2.2) | 6 (2.2) |
| Stress frequency: rarely, n (%) | 1800 (20.5) | 1637 (21.1) | 116 (15.2) | 47 (17.0) |
| sometimes | 5350 (60.8) | 4714 (60.8) | 476 (62.4) | 160 (57.8) |
| often | 1479 (16.8) | 1274 (16.4) | 144 (18.9) | 61 (22.0) |
| always | 170 (1.9) | 134 (1.7) | 27 (3.5) | 9 (3.2) |
| Eating Every Day | Skipping Occasionally | Skipping Often/Usually | |
|---|---|---|---|
| Male students | |||
| Incidence of frequent drinking, n (%) | 686 (4.9) | 116 (5.2) | 76 (7.4) |
| Observational period, year | 3.03 (3.01–3.06) | 3.03 (3.01–3.06) | 3.03 (3.01–3.06) |
| IR per 1000 PY (95% CI) | 16.1 (14.9–17.4) | 17.4 (14.5–20.9) | 25.0 (20.0–31.4) |
| Unadjusted HR (95% CI) | 1.00 (Reference) | 1.06 (0.87–1.30) | 1.52 (1.20–1.93) |
| Adjusted HR (95% CI) * | 1.00 (Reference) | 1.02 (0.84–1.25) | 1.48 (1.17–1.88) |
| Female students | |||
| Incidence of frequent drinking, n (%) | 150 (1.9) | 23 (3.0) | 17 (6.1) |
| Observational period, year | 3.04 (3.02–3.06) | 3.04 (3.01–3.06) | 3.04 (3.01–3.06) |
| IR per 1000 PY (95% CI) | 6.17 (5.3–7.2) | 9.88 (6.6–14.9) | 20.2 (12.6–32.5) |
| Unadjusted HR (95% CI) | 1.00 (Reference) | 1.63 (1.05–2.52) | 3.15 (1.91–5.20) |
| Adjusted HR (95% CI) * | 1.00 (Reference) | 1.60 (1.03–2.49) | 3.14 (1.88–5.24) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsumura, Y.; Yamamoto, R.; Shinzawa, M.; Matsushita, T.; Yoshimura, R.; Otsuki, N.; Mizui, M.; Matsui, I.; Kaimori, J.; Sakaguchi, Y.; et al. Skipping Breakfast and Incidence of Frequent Alcohol Drinking in University Students in Japan: A Retrospective Cohort Study. Nutrients 2022, 14, 2657. https://doi.org/10.3390/nu14132657
Matsumura Y, Yamamoto R, Shinzawa M, Matsushita T, Yoshimura R, Otsuki N, Mizui M, Matsui I, Kaimori J, Sakaguchi Y, et al. Skipping Breakfast and Incidence of Frequent Alcohol Drinking in University Students in Japan: A Retrospective Cohort Study. Nutrients. 2022; 14(13):2657. https://doi.org/10.3390/nu14132657
Chicago/Turabian StyleMatsumura, Yuichiro, Ryohei Yamamoto, Maki Shinzawa, Taisuke Matsushita, Ryuichi Yoshimura, Naoko Otsuki, Masayuki Mizui, Isao Matsui, Junya Kaimori, Yusuke Sakaguchi, and et al. 2022. "Skipping Breakfast and Incidence of Frequent Alcohol Drinking in University Students in Japan: A Retrospective Cohort Study" Nutrients 14, no. 13: 2657. https://doi.org/10.3390/nu14132657
APA StyleMatsumura, Y., Yamamoto, R., Shinzawa, M., Matsushita, T., Yoshimura, R., Otsuki, N., Mizui, M., Matsui, I., Kaimori, J., Sakaguchi, Y., Ishibashi, C., Ide, S., Nakanishi, K., Nishida, M., Kudo, T., Yamauchi-Takihara, K., Nagatomo, I., & Moriyama, T. (2022). Skipping Breakfast and Incidence of Frequent Alcohol Drinking in University Students in Japan: A Retrospective Cohort Study. Nutrients, 14(13), 2657. https://doi.org/10.3390/nu14132657






