Early and Strong Leptin Reduction Is Predictive for Long-Term Weight Loss during High-Protein, Low-Glycaemic Meal Replacement—A Subanalysis of the Randomised-Controlled ACOORH Trial
Abstract
:1. Introduction
2. Materials and Methods
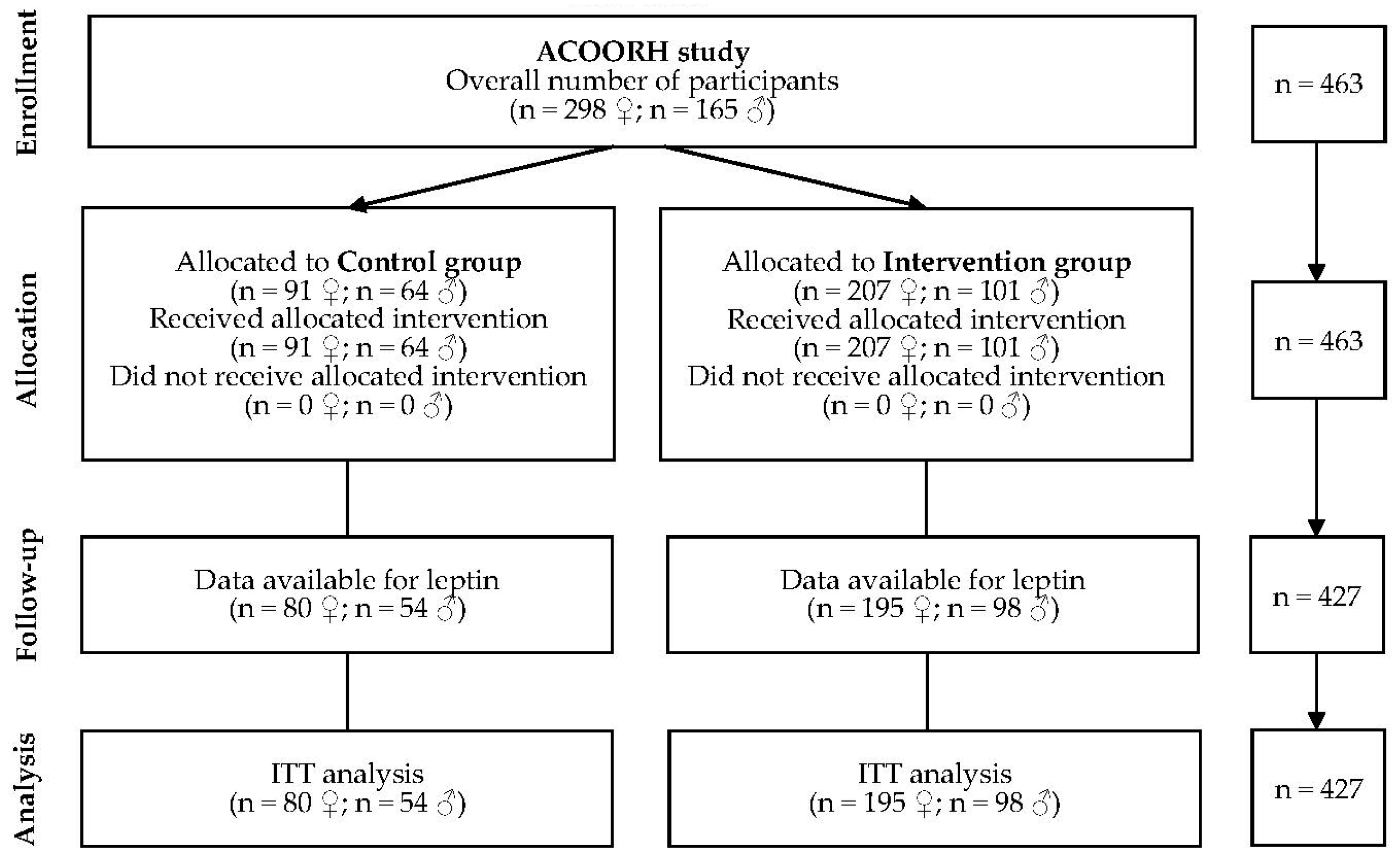
2.1. Study Design and Population
2.2. Intervention and Meal Replacement Regimen
2.3. Outcomes and Measurements
2.4. Statistics
3. Results
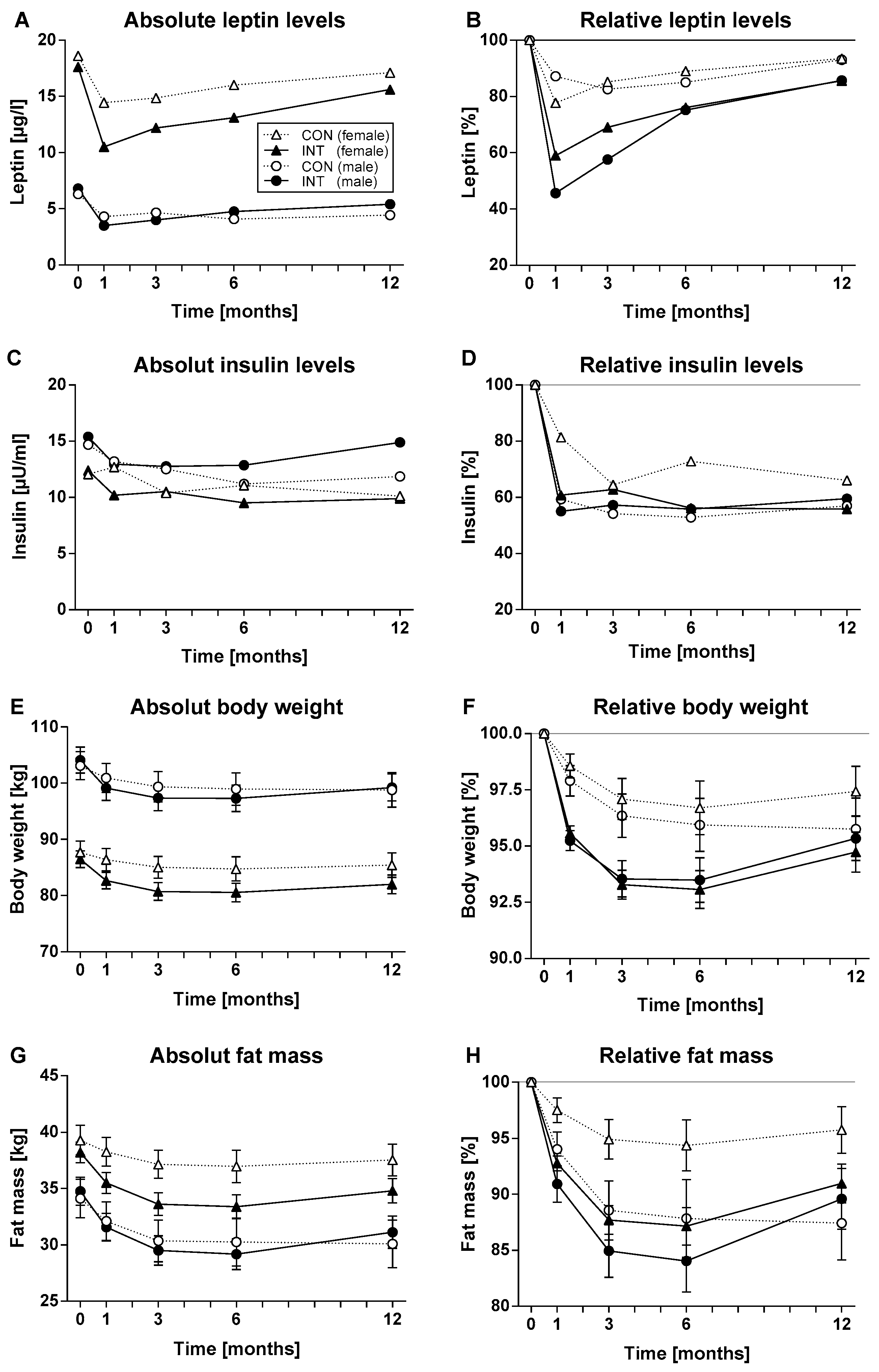
3.1. Stronger Improvement of Leptin Levels, Body Weight and Fat Mass in the Intervention Group
3.2. Baseline Leptin Values Correlate with Baseline Parameters
3.3. Leptin Reduction Is Predictive for Loss of Body Weight and Fat Mass
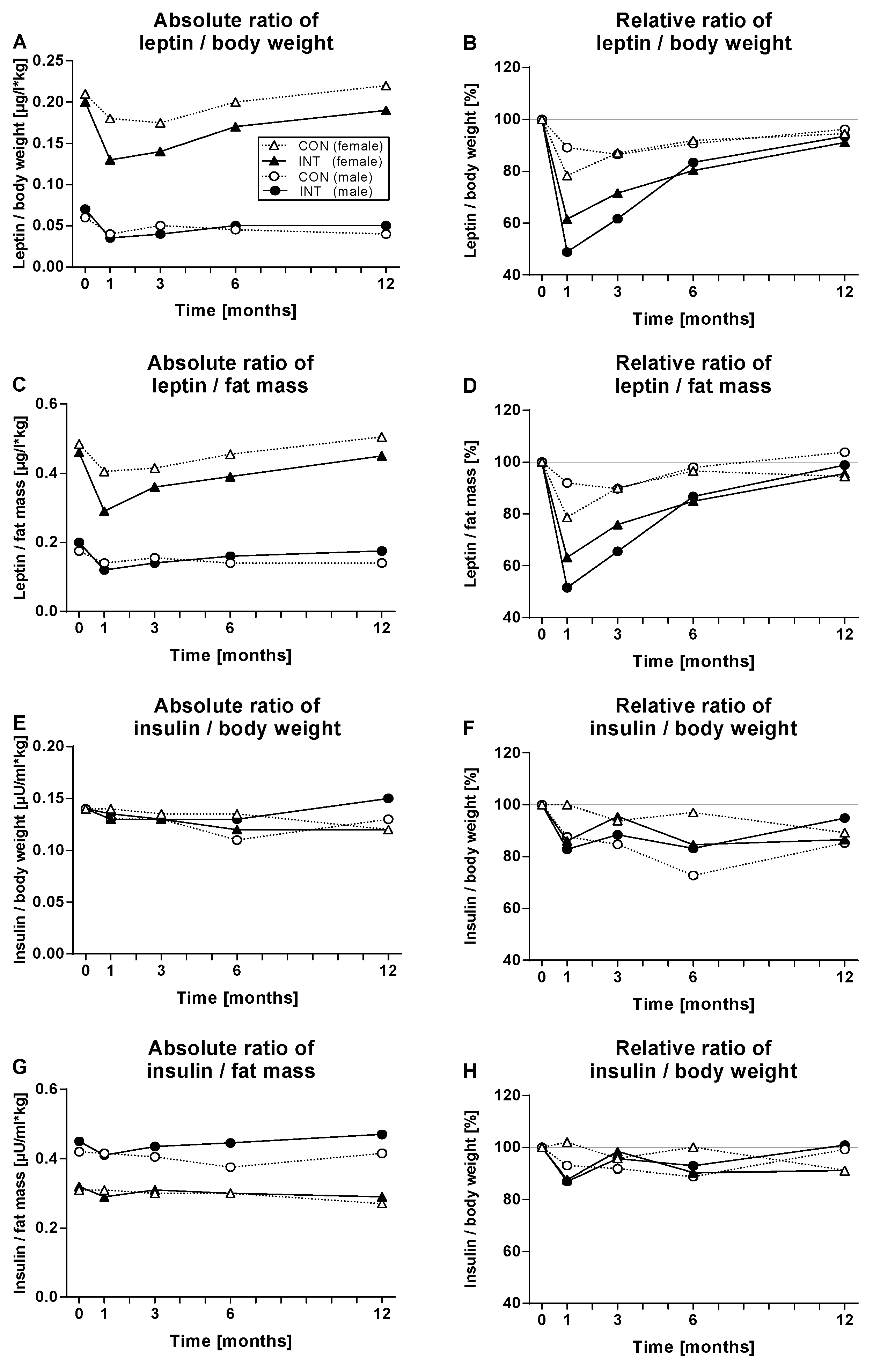
3.4. The Leptin Decrease Is Only Partially Explained by Body Weight and Fat Loss and Stronger in the Intervention Group
3.5. Leptin Reduction Accounts for Long-Term Weight Loss
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhang, Y.; Proenca, R.; Maffei, M.; Barone, M.; Leopold, L.; Friedman, J.M. Positional cloning of the mouse obese gene and its human homologue. Nature 1994, 372, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Niskanen, L.K.; Haffner, S.; Karhunen, L.J.; Turpeinen, A.K.; Miettinen, H.; Uusitupa, M.I. Serum leptin in obesity is related to gender and body fat topography but does not predict successful weight loss. Eur. J. Endocrinol. 1997, 137, 61–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campfield, L.A.; Smith, F.J.; Guisez, Y.; Devos, R.; Burn, P. Recombinant mouse OB protein: Evidence for a peripheral signal linking adiposity and central neural networks. Science 1995, 269, 546–549. [Google Scholar] [CrossRef] [PubMed]
- Halaas, J.L.; Gajiwala, K.S.; Maffei, M.; Cohen, S.L.; Chait, B.T.; Rabinowitz, D.; Lallone, R.L.; Burley, S.K.; Friedman, J.M. Weight-reducing effects of the plasma protein encoded by the obese gene. Science 1995, 269, 543–546. [Google Scholar] [CrossRef] [PubMed]
- Elias, C.F.; Aschkenasi, C.; Lee, C.; Kelly, J.; Ahima, R.S.; Bjorbaek, C.; Flier, J.S.; Saper, C.B.; Elmquist, J.K. Leptin differentially regulates NPY and POMC neurons projecting to the lateral hypothalamic area. Neuron 1999, 23, 775–786. [Google Scholar] [CrossRef] [Green Version]
- Knight, Z.A.; Hannan, K.S.; Greenberg, M.L.; Friedman, J.M. Hyperleptinemia is required for the development of leptin resistance. PLoS ONE 2010, 5, e11376. [Google Scholar] [CrossRef]
- Amitani, M.; Asakawa, A.; Amitani, H.; Inui, A. The role of leptin in the control of insulin-glucose axis. Front. Neurosci. 2013, 7, 51. [Google Scholar] [CrossRef] [Green Version]
- Tuomilehto, J.; Lindstrom, J.; Eriksson, J.G.; Valle, T.T.; Hamalainen, H.; Ilanne-Parikka, P.; Keinanen-Kiukaanniemi, S.; Laakso, M.; Louheranta, A.; Rastas, M.; et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N. Engl. J. Med. 2001, 344, 1343–1350. [Google Scholar] [CrossRef]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; Nathan, D.M. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar]
- Ramachandran, A.; Snehalatha, C.; Mary, S.; Mukesh, B.; Bhaskar, A.D.; Vijay, V. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia 2006, 49, 289–297. [Google Scholar] [CrossRef] [Green Version]
- Lim, E.L.; Hollingsworth, K.G.; Aribisala, B.S.; Chen, M.J.; Mathers, J.C.; Taylor, R. Reversal of type 2 diabetes: Normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 2011, 54, 2506–2514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lean, M.E.J.; Leslie, W.S.; Barnes, A.C.; Brosnahan, N.; Thom, G.; McCombie, L.; Peters, C.; Zhyzhneuskaya, S.; Al-Mrabeh, A.; Hollingsworth, K.G.; et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol. 2019, 7, 344–355. [Google Scholar] [CrossRef] [Green Version]
- Taheri, S.; Zaghloul, H.; Chagoury, O.; Elhadad, S.; Ahmed, S.H.; El, K.N.; Amona, R.A.; El, N.K.; Suleiman, N.; Alnaama, A.; et al. Effect of intensive lifestyle intervention on bodyweight and glycaemia in early type 2 diabetes (DIADEM-I): An open-label, parallel-group, randomised controlled trial. Lancet Diabetes Endocrinol. 2020, 8, 477–489. [Google Scholar] [CrossRef]
- Yanovski, S.Z.; Yanovski, J.A. Obesity. N. Engl. J. Med. 2002, 346, 591–602. [Google Scholar] [CrossRef]
- Halle, M.; Röhling, M.; Banzer, W.; Braumann, K.M.; Kempf, K.; McCarthy, D.; Schaller, N.; Predel, H.G.; Scholze, J.; Fuhrer-Sakel, D.; et al. Meal replacement by formula diet reduces weight more than a lifestyle intervention alone in patients with overweight or obesity and accompanied cardiovascular risk factors-the ACOORH trial. Eur. J. Clin. Nutr. 2021, 75, 661–669. [Google Scholar] [CrossRef]
- Röhling, M.; Kempf, K.; Banzer, W.; Berg, A.; Braumann, K.M.; Tan, S.; Halle, M.; McCarthy, D.; Pinget, M.; Predel, H.G.; et al. Prediabetes Conversion to Normoglycemia Is Superior Adding a Low-Carbohydrate and Energy Deficit Formula Diet to Lifestyle Intervention-A 12-Month Subanalysis of the ACOORH Trial. Nutrients 2020, 12, 2022. [Google Scholar] [CrossRef]
- Röhling, M.; Stensitzky, A.; Oliveira, C.L.P.; Beck, A.; Braumann, K.M.; Halle, M.; Fuhrer-Sakel, D.; Kempf, K.; McCarthy, D.; Predel, H.G.; et al. Effects of a Protein-Rich, Low-Glycaemic Meal Replacement on Changes in Dietary Intake and Body Weight Following a Weight-Management Intervention-The ACOORH Trial. Nutrients 2021, 13, 376. [Google Scholar] [CrossRef]
- Kempf, K.; Röhling, M.; Banzer, W.; Braumann, K.M.; Halle, M.; McCarthy, D.; Predel, H.G.; Schenkenberger, I.; Tan, S.; Toplak, H.; et al. High-Protein, Low-Glycaemic Meal Replacement Decreases Fasting Insulin and Inflammation Markers-A 12-Month Subanalysis of the ACOORH Trial. Nutrients 2021, 13, 1433. [Google Scholar] [CrossRef]
- Röhling, M.; Kempf, K.; Banzer, W.; Braumann, K.M.; Fuhrer-Sakel, D.; Halle, M.; McCarthy, D.; Martin, S.; Scholze, J.; Toplak, H.; et al. A High-Protein and Low-Glycemic Formula Diet Improves Blood Pressure and Other Hemodynamic Parameters in High-Risk Individuals. Nutrients 2022, 14, 1443. [Google Scholar] [CrossRef]
- Uzum, A.K.; Yucel, B.; Omer, B.; Issever, H.; Ozbey, N.C. Leptin concentration indexed to fat mass is increased in untreated anorexia nervosa (AN) patients. Clin. Endocrinol. 2009, 71, 33–39. [Google Scholar] [CrossRef]
- Wadden, T.A.; Considine, R.V.; Foster, G.D.; Anderson, D.A.; Sarwer, D.B.; Caro, J.S. Short- and long-term changes in serum leptin dieting obese women: Effects of caloric restriction and weight loss. J. Clin. Endocrinol. Metab. 1998, 83, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Fujita, Y.; Kouda, K.; Ohara, K.; Nakamura, H.; Iki, M. Leptin mediates the relationship between fat mass and blood pressure: The Hamamatsu School-based health study. Medicine 2019, 98, e14934. [Google Scholar] [CrossRef] [PubMed]
- Considine, R.V.; Sinha, M.K.; Heiman, M.L.; Kriauciunas, A.; Stephens, T.W.; Nyce, M.R.; Ohannesian, J.P.; Marco, C.C.; McKee, L.J.; Bauer, T.L.; et al. Serum immunoreactive-leptin concentrations in normal-weight and obese humans. N. Engl. J. Med. 1996, 334, 292–295. [Google Scholar] [CrossRef] [PubMed]
- Elmquist, J.K.; Elias, C.F.; Saper, C.B. From lesions to leptin: Hypothalamic control of food intake and body weight. Neuron 1999, 22, 221–232. [Google Scholar] [CrossRef] [Green Version]
- Heymsfield, S.B.; Greenberg, A.S.; Fujioka, K.; Dixon, R.M.; Kushner, R.; Hunt, T.; Lubina, J.A.; Patane, J.; Self, B.; Hunt, P.; et al. Recombinant leptin for weight loss in obese and lean adults: A randomized, controlled, dose-escalation trial. JAMA 1999, 282, 1568–1575. [Google Scholar] [CrossRef]
- Zelissen, P.M.; Stenlof, K.; Lean, M.E.; Fogteloo, J.; Keulen, E.T.; Wilding, J.; Finer, N.; Rossner, S.; Lawrence, E.; Fletcher, C.; et al. Effect of three treatment schedules of recombinant methionyl human leptin on body weight in obese adults: A randomized, placebo-controlled trial. Diabetes Obes. Metab. 2005, 7, 755–761. [Google Scholar] [CrossRef]
- Chaldakov, G.N.; Fiore, M.; Stankulov, I.S.; Hristova, M.; Antonelli, A.; Manni, L.; Ghenev, P.I.; Angelucci, F.; Aloe, L. NGF, BDNF, leptin, and mast cells in human coronary atherosclerosis and metabolic syndrome. Arch. Physiol. Biochem. 2001, 109, 357–360. [Google Scholar] [CrossRef]
- Bjorbak, C.; Lavery, H.J.; Bates, S.H.; Olson, R.K.; Davis, S.M.; Flier, J.S.; Myers, M.G., Jr. SOCS3 mediates feedback inhibition of the leptin receptor via Tyr985. J. Biol. Chem. 2000, 275, 40649–40657. [Google Scholar] [CrossRef] [Green Version]
- Dirlewanger, M.; di Vetta, V.; Guenat, E.; Battilana, P.; Seematter, G.; Schneiter, P.; Jequier, E.; Tappy, L. Effects of short-term carbohydrate or fat overfeeding on energy expenditure and plasma leptin concentrations in healthy female subjects. Int. J. Obes. Relat. Metab. Disord. 2000, 24, 1413–1418. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Y.; Yu, X.; Chen, H.; Sjoberg, S.; Roux, J.; Zhang, L.; Ivoulsou, A.H.; Bensaid, F.; Liu, C.L.; Liu, J.; et al. Leptin Deficiency Shifts Mast Cells toward Anti-Inflammatory Actions and Protects Mice from Obesity and Diabetes by Polarizing M2 Macrophages. Cell Metab. 2015, 22, 1045–1058. [Google Scholar] [CrossRef] [Green Version]
- Burguera, B.; Couce, M.E.; Curran, G.L.; Jensen, M.D.; Lloyd, R.V.; Cleary, M.P.; Poduslo, J.F. Obesity is associated with a decreased leptin transport across the blood-brain barrier in rats. Diabetes 2000, 49, 1219–1223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, S.; Zhu, Y.; Schultz, R.D.; Li, N.; He, Z.; Zhang, Z.; Caron, A.; Zhu, Q.; Sun, K.; Xiong, W.; et al. Partial Leptin Reduction as an Insulin Sensitization and Weight Loss Strategy. Cell Metab. 2019, 30, 706–719. [Google Scholar] [CrossRef] [PubMed]
- Crujeiras, A.B.; Goyenechea, E.; Abete, I.; Lage, M.; Carreira, M.C.; Martinez, J.A.; Casanueva, F.F. Weight regain after a diet-induced loss is predicted by higher baseline leptin and lower ghrelin plasma levels. J. Clin. Endocrinol. Metab. 2010, 95, 5037–5044. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torgerson, J.S.; Carlsson, B.; Stenlof, K.; Carlsson, L.M.; Bringman, E.; Sjostrom, L. A low serum leptin level at baseline and a large early decline in leptin predict a large 1-year weight reduction in energy-restricted obese humans. J. Clin. Endocrinol. Metab. 1999, 84, 4197–4203. [Google Scholar] [PubMed] [Green Version]
- de Luis, D.A.; Izaola, O.; Primo, D.; Ovalle, H.F.; Lopez, J.J.; Gomez, E.; Ortola, A.; Aller, R. Biochemical, Anthropometric and Lifestyle Factors Related with Weight Maintenance after Weight Loss Secondary to a Hypocaloric Mediterranean Diet. Ann. Nutr. Metab. 2017, 71, 217–223. [Google Scholar] [CrossRef]
- Seufert, J.; Kieffer, T.J.; Leech, C.A.; Holz, G.G.; Moritz, W.; Ricordi, C.; Habener, J.F. Leptin suppression of insulin secretion and gene expression in human pancreatic islets: Implications for the development of adipogenic diabetes mellitus. J. Clin. Endocrinol. Metab. 1999, 84, 670–676. [Google Scholar] [CrossRef]
- Seufert, J. Leptin effects on pancreatic beta-cell gene expression and function. Diabetes 2004, 53 (Suppl. 1), S152–S158. [Google Scholar] [CrossRef] [Green Version]
- Yip, I.; Go, V.L.; Hershman, J.M.; Wang, H.J.; Elashoff, R.; DeShields, S.; Liu, Y.; Heber, D. Insulin-leptin-visceral fat relation during weight loss. Pancreas 2001, 23, 197–203. [Google Scholar] [CrossRef]
- de Luis, D.A.; Aller, R.; Izaola, O.; Gonzalez, S.M.; Conde, R.; de la Fuente, B.; Primo, D. Effect of Lys656Asn Polymorphism of Leptin Receptor Gene on Cardiovascular Risk Factors and Serum Adipokine Levels after a High Polyunsaturated Fat Diet in Obese Patients. J. Clin. Lab. Anal. 2015, 29, 432–436. [Google Scholar] [CrossRef]
- Primo, D.; Izaola, O.; De Luis, D. Leptin gene polymorphism (rs 7799039; G2548A) is associated with changes in lipid profile during a partial meal-replacement hypocaloric diet. J. Hum. Nutr. Diet. 2021, 34, 456–463. [Google Scholar] [CrossRef]
- Xu, H.; Barnes, G.T.; Yang, Q.; Tan, G.; Yang, D.; Chou, C.J.; Sole, J.; Nichols, A.; Ross, J.S.; Tartaglia, L.A.; et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J. Clin. Investig. 2003, 112, 1821–1830. [Google Scholar] [CrossRef] [PubMed]
- Weisberg, S.P.; McCann, D.; Desai, M.; Rosenbaum, M.; Leibel, R.L.; Ferrante, A.W., Jr. Obesity is associated with macrophage accumulation in adipose tissue. J. Clin. Investig. 2003, 112, 1796–1808. [Google Scholar] [CrossRef] [PubMed]
- Kolb, H.; Mandrup-Poulsen, T. An immune origin of type 2 diabetes? Diabetologia 2005, 48, 1038–1050. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grassmann, S.; Wirsching, J.; Eichelmann, F.; Aleksandrova, K. Association Between Peripheral Adipokines and Inflammation Markers: A Systematic Review and Meta-Analysis. Obesity 2017, 25, 1776–1785. [Google Scholar] [CrossRef]
- Jequier, E. Leptin signaling, adiposity, and energy balance. Ann. N. Y. Acad. Sci. 2002, 967, 379–388. [Google Scholar] [CrossRef]
- Samtiya, M.; Aluko, R.E.; Dhewa, T.; Moreno-Rojas, J.M. Potential Health Benefits of Plant Food-Derived Bioactive Components: An Overview. Foods 2021, 10, 839. [Google Scholar] [CrossRef]

| Parameters | Female | Male | ||
|---|---|---|---|---|
| Control Group (n = 80) | Intervention Group (n = 195) | Control Group (n = 54) | Intervention Group (n = 98) | |
| Prediabetes (n) | 30 (37.5%) | 66 (33.8%) | 10 (18.5%) | 26 (26.5%) |
| Age (years) | 52 ± 9 | 51 ± 10 | 50 ± 10 | 50 ± 8 |
| Body mass index (kg/m2) | 31.7 ± 2.4 | 31.5 ± 2.5 | 31.3 ± 2.4 | 32.1 ± 2.0 |
| Weight (kg) | 87.7 ± 9.1 | 86.5 ± 10.7 | 103.1 ± 9.1 | 104.1 ± 11.5 |
| Fat mass (kg) | 39.3 ± 6.0 | 38.2 ± 6.5 | 34.1 ± 6.2 | 34.8 ± 6.2 |
| Lean body mass (kg) | 48.4 ± 5.0 | 48.3 ± 5.7 | 68.9 ± 6.8 | 69.2 ± 7.4 |
| Fasting insulin (µU/mL) | 13.6 ± 6.9 | 14.6 ± 8.9 | 18.0 ± 10.7] | 18.5 ± 11.0 |
| Leptin (µg/L) | 18.6 [13.7; 27.3] | 17.6 [12.1; 24.9] | 6.3 [3.3; 9.6] | 6.8 [4.2; 9.8] |
| Leptin/fat mass (µg/L·kg) | 0.5 [0.3; 0.7] | 0.5 [0.3; 0.6] | 0.2 [0.1; 0.3] | 0.2 [0.1; 0.3] |
| Prediabetes (n) | 30 (37.5%) | 66 (33.8%) | 10 (18.5%) | 26 (26.5%) |
| Age (years) | 52 ± 9 | 51 ± 10 | 50 ± 10 | 50 ± 8 |
| All (n = 427) | Female (n = 275) | Male (n = 152) | ||||
|---|---|---|---|---|---|---|
| Parameters | r | p | r | p | r | p |
| Sex | −0.65 | <0.001 | - | - | - | - |
| Prediabetes | 0.15 | 0.002 | 0.11 | 0.064 | 0.08 | 0.338 |
| Age | 0.02 | 0.712 | −0,02 | 0.792 | 0.03 | 0.703 |
| Body mass index | 0.24 | <0.001 | 0.38 | <0.001 | 0.29 | <0.001 |
| Body weight | −0.28 | <0.001 | 0.24 | <0.001 | 0.19 | 0.017 |
| Fat mass | 0.46 | <0.001 | 0.38 | <0.001 | 0.44 | <0.001 |
| Lean body mass | −0.54 | <0.001 | −0.01 | 0.899 | −0.09 | 0.265 |
| Fasting insulin | −0.02 | 0.685 | 0.18 | 0.003 | 0.20 | 0.015 |
| Interleukin-6 | 0.07 | 0.225 | 0.07 | 0.319 | −0.04 | 0.693 |
| C-reactive protein | 0.19 | <0.001 | 0.17 | 0.010 | −0.06 | 0.526 |
| Parameters | Control Group (n = 134) | Intervention Group (n = 293) | ||||||
|---|---|---|---|---|---|---|---|---|
| r | p | ß | p | r | p | ß | p | |
| Leptin (baseline) | ||||||||
| Body weight at baseline | −0.31 | <0.001 | −0.08 | 0.237 | −0.18 | 0.002 | −0.00 | 0.980 |
| Δ weight after 1 month | 0.09 | 0.312 | 0.00 | 0.883 | 0.12 | 0.035 | 0.01 | 0.571 |
| Δ weight after 3 months | 0.09 | 0.296 | 0.02 | 0.869 | 0.02 | 0.679 | −0.03 | 0.677 |
| Δ weight after 6 months | 0.06 | 0.470 | −0.04 | 0.724 | −0.02 | 0.774 | −0.07 | 0.351 |
| Δ weight after 12 months | 0.12 | 0.169 | 0.05 | 0.169 | −0.04 | 0.500 | −0.05 | 0.674 |
| Fat mass at baseline | 0.48 | <0.001 | 0.12 | 0.271 | 0.41 | <0.001 | 0.19 | 0.007 |
| Δ fat mass after 1 month | 0.15 | 0.075 | 0.04 | 0.605 | 0.07 | 0.243 | 0.04 | 0.445 |
| Δ fat mass after 3 months | 0.15 | 0.090 | 0.01 | 0.844 | 0.03 | 0.587 | 0.01 | 0.990 |
| Δ fat mass after 6 months | 0.11 | 0.209 | −0.01 | 0.859 | 0.01 | 0.970 | −0.03 | 0.572 |
| Δ fat mass after 12 months | 0.15 | 0.084 | −0.03 | 0.657 | −0.04 | 0.508 | −0.06 | 0.244 |
| Δ Leptin (after 1 month) | ||||||||
| Δ weight after 1 month | 0.32 | <0.001 | 0.34 | <0.001 | 0.24 | <0.001 | 0.33 | <0.001 |
| Δ weight after 3 months | 0.38 | <0.001 | 0.40 | <0.001 | 0.35 | <0.001 | 0.39 | <0.001 |
| Δ weight after 6 months | 0.41 | <0.001 | 0.44 | <0.001 | 0.36 | <0.001 | 0.39 | <0.001 |
| Δ weight after 12 months | 0.31 | <0.001 | 0.36 | <0.001 | 0.32 | <0.001 | 0.33 | <0.001 |
| Δ fat mass after 1 month | 0.20 | 0.018 | 0.27 | 0.002 | 0.22 | <0.001 | 0.25 | <0.001 |
| Δ fat mass after 3 months | 0.27 | 0.002 | 0.34 | <0.001 | 0.34 | <0.001 | 0.37 | <0.001 |
| Δ fat mass after 6 months | 0.36 | <0.001 | 0.41 | <0.001 | 0.33 | <0.001 | 0.36 | <0.001 |
| Δ fat mass after 12 months | 0.29 | 0.001 | 0.37 | <0.001 | 0.29 | <0.001 | 0.30 | <0.001 |
| Δ weight after 1 month | 0.32 | <0.001 | 0.34 | <0.001 | 0.24 | <0.001 | 0.33 | <0.001 |
| Δ weight after 3 months | 0.38 | <0.001 | 0.40 | <0.001 | 0.35 | <0.001 | 0.39 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kempf, K.; Röhling, M.; Banzer, W.; Braumann, K.M.; Halle, M.; Schaller, N.; McCarthy, D.; Predel, H.G.; Schenkenberger, I.; Tan, S.; et al. Early and Strong Leptin Reduction Is Predictive for Long-Term Weight Loss during High-Protein, Low-Glycaemic Meal Replacement—A Subanalysis of the Randomised-Controlled ACOORH Trial. Nutrients 2022, 14, 2537. https://doi.org/10.3390/nu14122537
Kempf K, Röhling M, Banzer W, Braumann KM, Halle M, Schaller N, McCarthy D, Predel HG, Schenkenberger I, Tan S, et al. Early and Strong Leptin Reduction Is Predictive for Long-Term Weight Loss during High-Protein, Low-Glycaemic Meal Replacement—A Subanalysis of the Randomised-Controlled ACOORH Trial. Nutrients. 2022; 14(12):2537. https://doi.org/10.3390/nu14122537
Chicago/Turabian StyleKempf, Kerstin, Martin Röhling, Winfried Banzer, Klaus Michael Braumann, Martin Halle, Nina Schaller, David McCarthy, Hans Georg Predel, Isabelle Schenkenberger, Susanne Tan, and et al. 2022. "Early and Strong Leptin Reduction Is Predictive for Long-Term Weight Loss during High-Protein, Low-Glycaemic Meal Replacement—A Subanalysis of the Randomised-Controlled ACOORH Trial" Nutrients 14, no. 12: 2537. https://doi.org/10.3390/nu14122537
APA StyleKempf, K., Röhling, M., Banzer, W., Braumann, K. M., Halle, M., Schaller, N., McCarthy, D., Predel, H. G., Schenkenberger, I., Tan, S., Toplak, H., Martin, S., Berg, A., & ACOORH Study Group. (2022). Early and Strong Leptin Reduction Is Predictive for Long-Term Weight Loss during High-Protein, Low-Glycaemic Meal Replacement—A Subanalysis of the Randomised-Controlled ACOORH Trial. Nutrients, 14(12), 2537. https://doi.org/10.3390/nu14122537








