Implications of Indirect Biomarkers of Intestinal Permeability in the Stools of Newborns and Infants with Perinatal Risk Factors for Intestinal Colonization Disorders and Infant Feeding Patterns
Abstract
1. Introduction
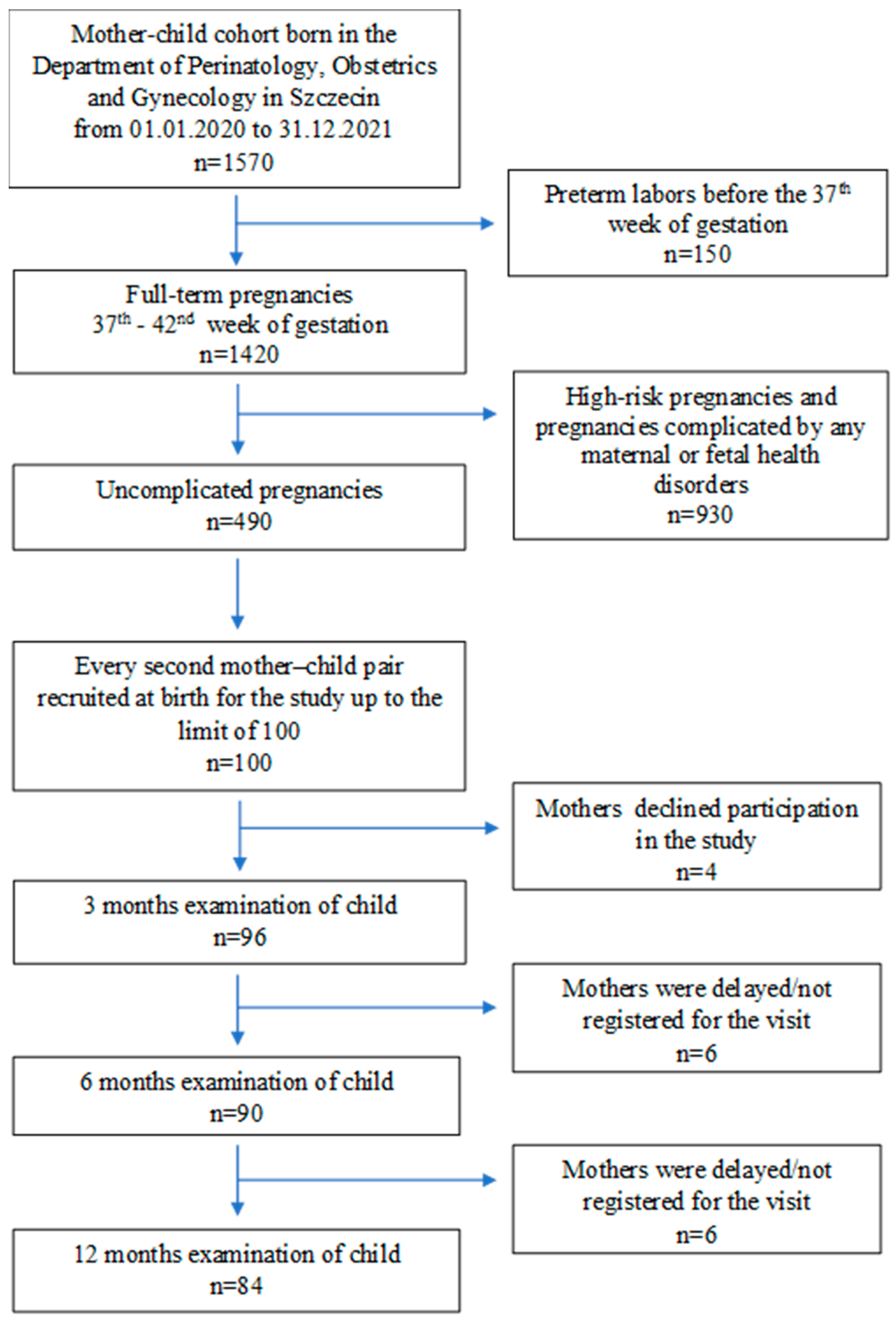
2. Materials and Methods
2.1. Study Group
2.2. Medical Assessment of Children
2.3. Analysis of Indirect Markers of Intestinal Permeability and Chronic Inflammatory Bowel Disease
2.4. Sample Preparation for the Determination of Lipopolysaccharide (LPS), Zonulin and Occludin Levels
2.5. Performance Characteristics for Assay Procedure
- Sensitivity 0.13 ng/mL; standard curve range: 0.3–90 ng/mL;
- Precision: intra-assay precision—three samples of known concentration were tested on one plate to assess intra-assay precision.
- Inter-assay precision—three samples of known concentration were tested in separate assays to assess inter-assay precision. CV(%) = SD/mean × 100
- Intra-assay: CV < 8% Inter-Assay: CV < 10%
- Specificity: this sandwich kit was for the accurate quantitative detection of human zonulin; haptoglobin (also known as HP).
- Sensitivity: the minimum detectable dose of LPS was typically less than 0.03 EU/mL. The sensitivity of this assay, or lower limit of detection (LLD) was defined as the lowest protein concentration that could be differentiated from zero. We determined the mean O.D. value of 20 replicates of the zero standard added, according to their three standard deviations.
- Detection range: 0.078–5 EU/mL. The standard curve concentrations used for the ELISAs were 5 EU/mL, 2.5 EU/mL, 1.25 EU/mL, 0.625 EU/mL, 0.312 EU/mL, 0.156 EU/mL and 0.078 EU/mL. Specificity: this assay had high sensitivity and excellent specificity for the detection of LPS. No significant cross-reactivity or interference was observed.
- Precision: Intra-assay precision (precision within an assay): three samples of known concentration were tested twenty times on one plate to assess intra-assay precision. Intra-assay CV: ≤5.3%.
2.6. Statistical Analysis
3. Results
4. Discussion
4.1. LPS, Occludin and Zonulin Stool Concentrations in Infants during the First Year of Life
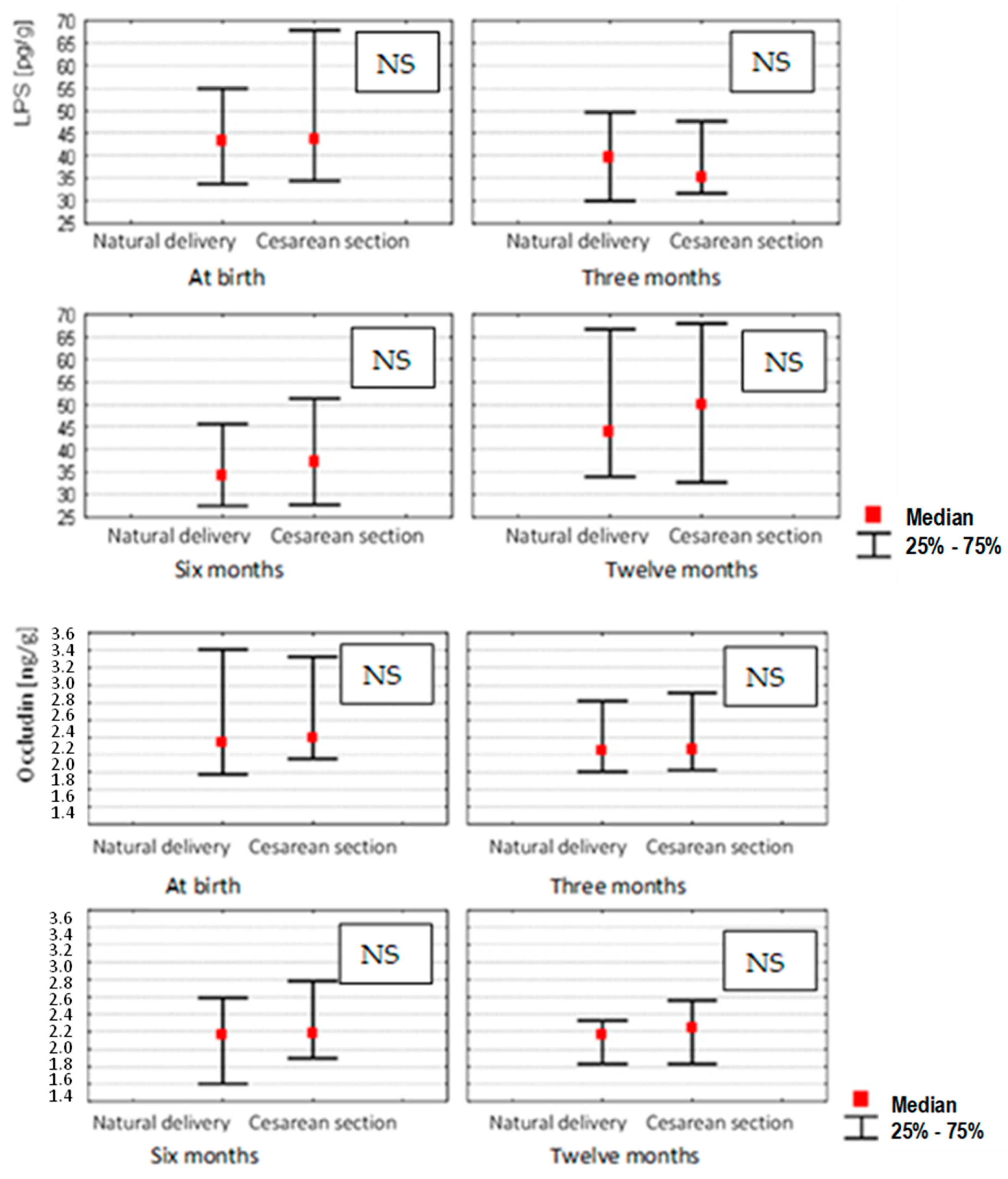
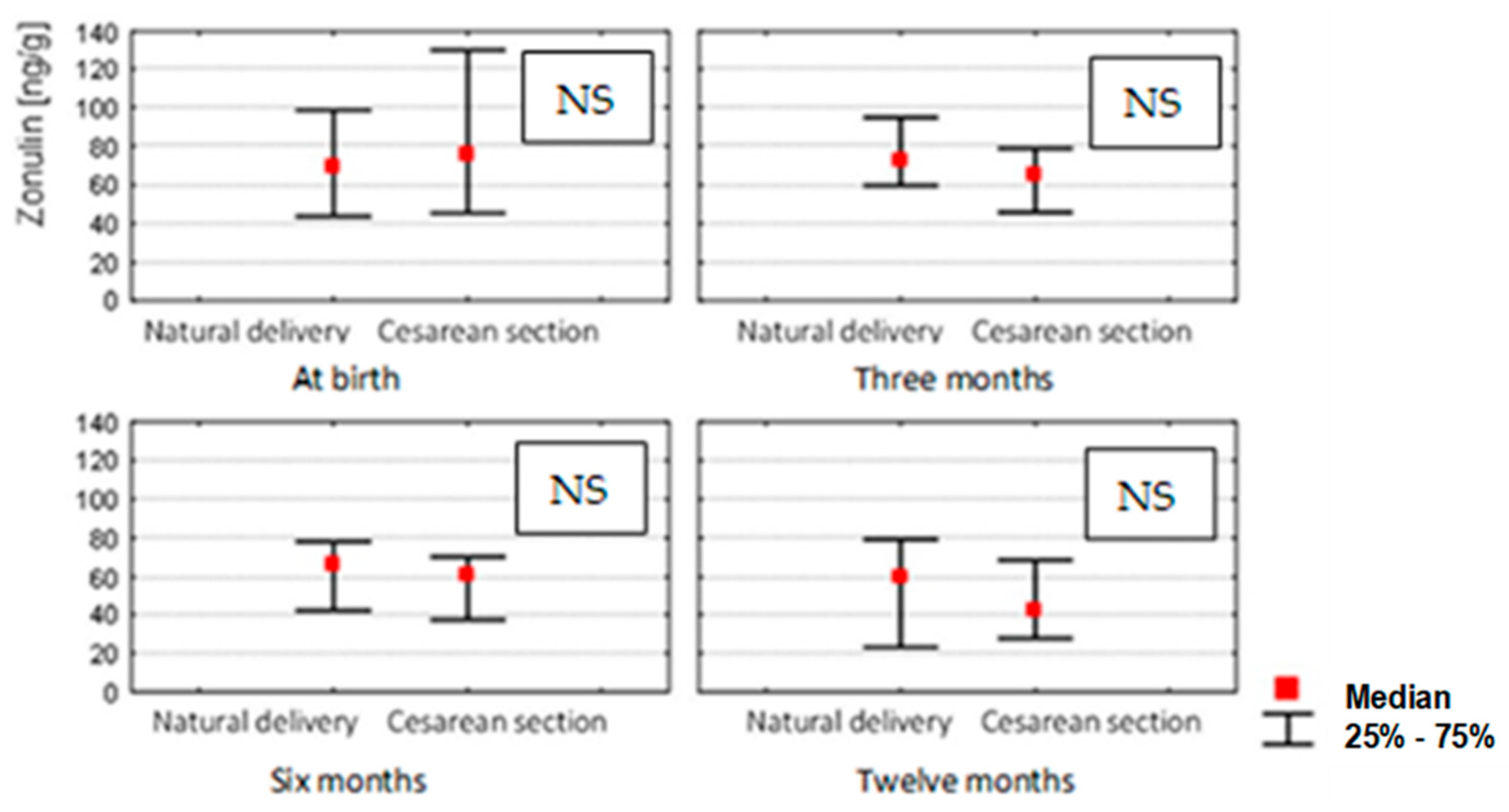
4.2. LPS, Occludin and Zonulin Stool Concentrations in Infants Depending on the Mode of Delivery
4.3. LPS, Occludin and Zonulin Stool Concentrations in Infants Depending on Other Factors
4.4. LPS, Occludin and Zonulin Stool Concentrations in Infants Depending on the Mode of Feeding
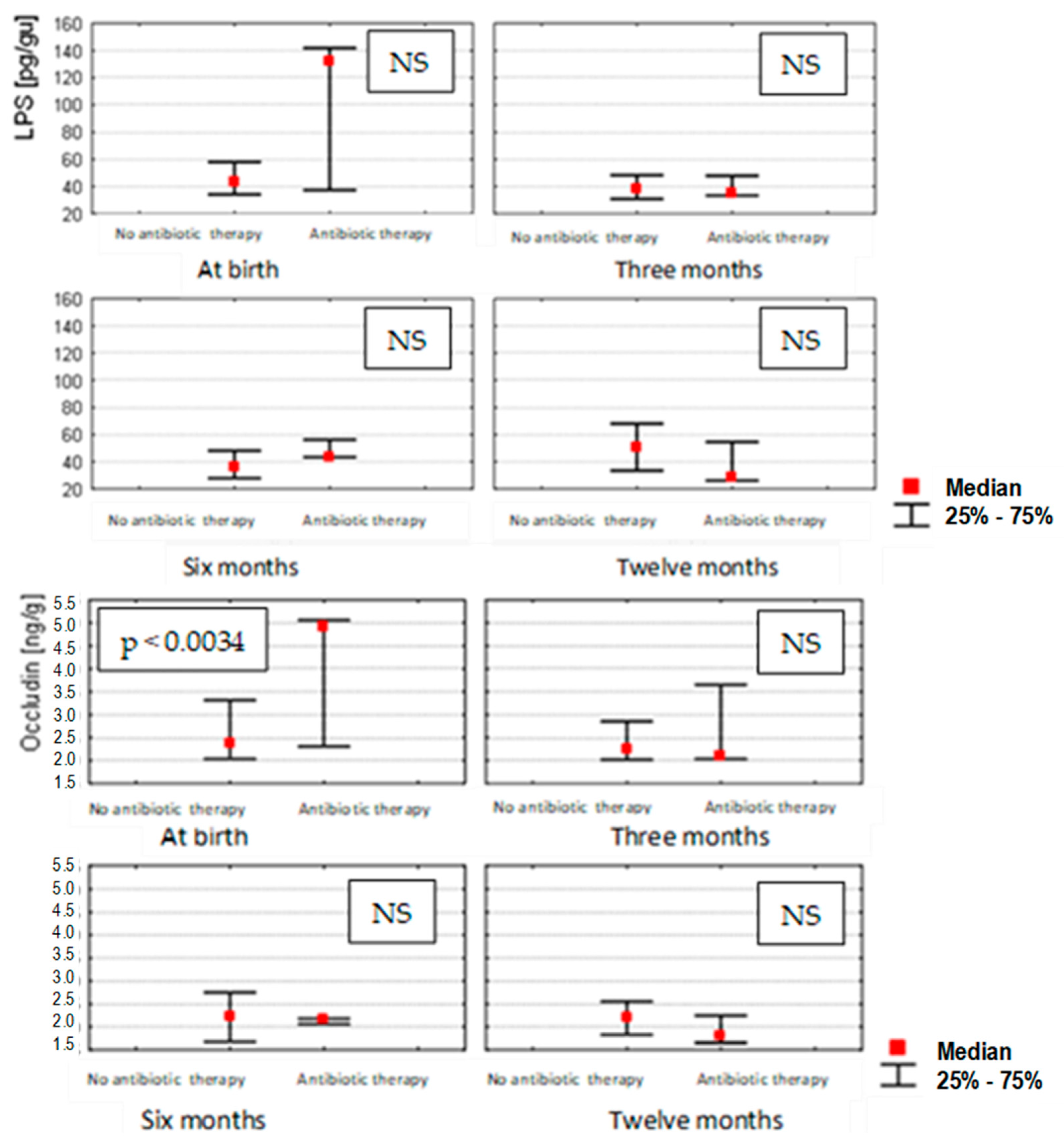
4.5. LPS, Occludin and Zonulin Stool Concentrations in Infants Depending on Antibiotic Use
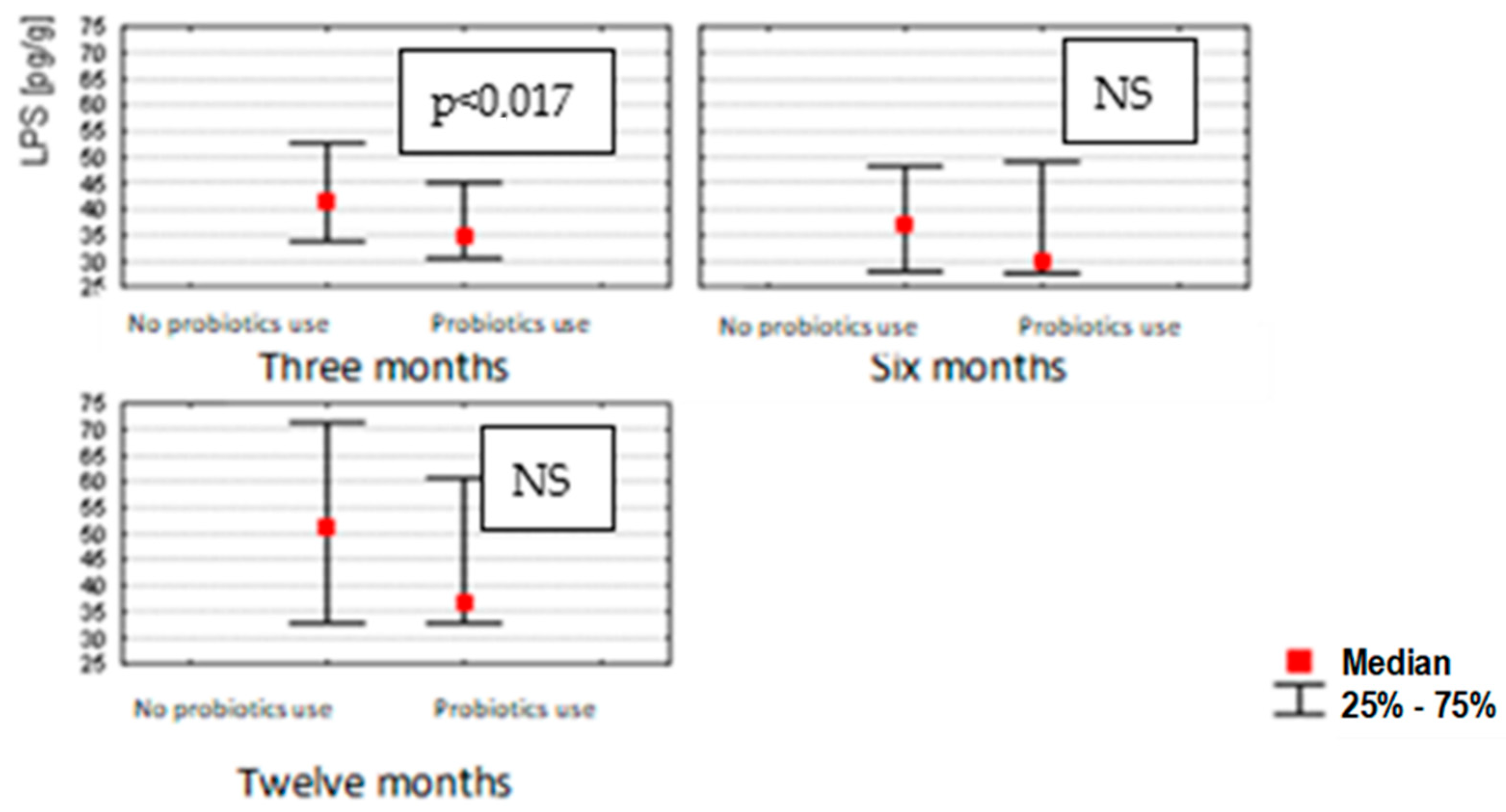
4.6. LPS, Occludin and Zonulin Stool Concentrations in Infants Depending on Probiotic Use
4.7. LPS, Occludin and Zonulin Stool Concentrations in Infants Depending on Maternal Gestational Weight Gain
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zietek, M.; Szczuko, M.; Celewicz, Z.; Kordek, A. Perinatal factors affecting the gut microbiota—Are they preventable? Ginekol. Pol. 2020, 91, 709–713. [Google Scholar] [CrossRef]
- Kapourchali, F.R.; Cresci, G.A.M. Early-Life Gut Microbiome—The Importance of Maternal and Infant Factors in Its Establishment. Nutr. Clin. Pract. 2020, 35, 386–405. [Google Scholar] [CrossRef]
- Langhendries, J.P. Colonisation bactérienne de l’intestin dans l’enfance: Pourquoi y accorder autant d’importance? Early bacterial colonisation of the intestine: Why it matters? Arch. Pediatr. 2006, 13, 1526–1534. [Google Scholar] [CrossRef]
- Tribe, R.M.; Taylor, P.D.; Kelly, N.M.; Rees, D.; Sandall, J.; Kennedy, H.P. Parturition and the perinatal period: Can mode of delivery impact on the future health of the neonate? J. Physiol. 2018, 596, 5709–5722. [Google Scholar] [CrossRef]
- Kim, S.; Kim, G.H. Roles of claudin-2, ZO-1 and occludin in leaky HK-2 cells. PLoS ONE 2017, 12, e0189221. [Google Scholar] [CrossRef]
- Vancamelbeke, M.; Vermeire, S. The intestinal barrier: A fundamental role in health and disease. Expert Rev. Gastroenterol. Hepatol. 2017, 11, 821–834. [Google Scholar] [CrossRef]
- Kinashi, Y.; Hase, K. Partners in Leaky Gut Syndrome: Intestinal Dysbiosis and Autoimmunity. Front. Immunol. 2021, 12, 673708. [Google Scholar] [CrossRef]
- Stan, T.L.; Soylu-Kucharz, R.; Burleigh, S.; Prykhodko, O.; Cao, L.; Franke, N.; Sjögren, M.; Haikal, C.; Hållenius, F.; Björkqvist, M. Increased intestinal permeability and gut dysbiosis in the R6/2 mouse model of Huntington’s disease. Sci. Rep. 2020, 10, 18270. [Google Scholar] [CrossRef]
- Lee, A.; White, N.; van der Walle, C.F. The intestinal zonula occludens toxin (ZOT) receptor recognises non-native ZOT conformers and localises to the intercellular contacts. FEBS Lett. 2003, 555, 638–642. [Google Scholar] [CrossRef]
- Bischoff, S.C.; Barbara, G.; Buurman, W.; Ockhuizen, T.; Schulzke, J.-D.; Serino, M.; Tilg, H.; Watson, A.; Wells, J.M. Intestinal permeability—A new target for disease prevention and therapy. BMC Gastroenterol. 2014, 14, 189. [Google Scholar] [CrossRef]
- Candelli, M.; Franza, L.; Pignataro, G.; Ojetti, V.; Covino, M.; Piccioni, A.; Gasbarrini, A.; Franceschi, F. Interaction between Lipopolysaccharide and Gut Microbiota in Inflammatory Bowel Diseases. Int. J. Mol. Sci. 2021, 22, 6242. [Google Scholar] [CrossRef]
- Schoultz, I.; Keita, A.V. The Intestinal Barrier and Current Techniques for the Assessment of Gut Permeability. Cells 2020, 9, 1909. [Google Scholar] [CrossRef]
- Ajamian, M.; Steer, D.; Rosella, G.; Gibson, P.R. Serum zonulin as a marker of intestinal mucosal barrier function: May not be what it seems. PLoS ONE 2019, 14, e0210728. [Google Scholar] [CrossRef]
- Vojdani, A.; Vojdani, E.; Kharrazian, D. Fluctuation of zonulin levels in blood vs stability of antibodies. World J. Gastroenterol. 2017, 23, 5669–5679. [Google Scholar] [CrossRef]
- Łoniewska, B.; Węgrzyn, D.; Adamek, K.; Kaczmarczyk, M.; Skonieczna-Żydecka, K.; Adler, G.; Jankowska, A.; Uzar, I.; Kordek, A.; Celewicz, M.; et al. The Influence of Maternal-Foetal Parameters on Concentrations of Zonulin and Calprotectin in the Blood and Stool of Healthy Newborns during the First Seven Days of Life. An Observational Prospective Cohort Study. J. Clin. Med. 2019, 8, 473. [Google Scholar] [CrossRef]
- Khasanova, S.S.; Akhmedova, D.I.; Kamilova, T.A. The Clinical Significance of Fecal Zonulin in Extremely Premature Babies. Am. J. Med. Sci. 2019, 9, 289–292. [Google Scholar] [CrossRef]
- Kaczmarczyk, M.; Löber, U.; Adamek, K.; Węgrzyn, D.; Skonieczna-Żydecka, K.; Malinowski, D.; Łoniewski, I.; Markó, L.; Ulas, T.; Forslund, S.K.; et al. The gut microbiota is associated with the small intestinal paracellular permeability and the development of the immune system in healthy children during the first two years of life. J. Transl. Med. 2021, 19, 177. [Google Scholar] [CrossRef]
- Martínez-Oca, P.; Robles-Vera, I.; Sánchez-Roncero, A.; Escrivá, F.; Pérez-Vizcaíno, F.; Duarte, J.; Álvarez, C.; Fernández-Millán, E. Gut DYSBIOSIS and altered barrier function precedes the appearance of metabolic syndrome in a rat model of nutrient-induced catch-up growth. J. Nutr. Biochem. 2020, 81, 108383. [Google Scholar] [CrossRef]
- Zak-Golab, A.; Kocelak, P.; Aptekorz, M.; Zientara, M.; Juszczyk, L.; Martirosian, G.; Chudek, J.; Olszanecka-Glinianowicz, M. Gut microbiota, microinflammation, metabolic profile, and zonulin concentration in obese and normal weight subjects. Int. J. Endocrinol. 2013, 2013, 674106. [Google Scholar] [CrossRef]
- Jian, C.; Carpén, N.; Helve, O.; de Vos, W.M.; Korpela, K.; Salonen, A. Early-life gut microbiota and its connection to metabolic health in children: Perspective on ecological drivers and need for quantitative approach. EBioMedicine 2021, 69, 103475. [Google Scholar] [CrossRef]
- Moore, R.E.; Townsend, S.D. Temporal development of the infant gut microbiome. Open Biol. 2019, 9, 190128. [Google Scholar] [CrossRef]
- Łoniewska, B.; Adamek, K.; Węgrzyn, D.; Kaczmarczyk, M.; Skonieczna-Żydecka, K.; Clark, J.; Adler, G.; Tousty, J.; Uzar, I.; Tousty, P.; et al. Analysis of Faecal Zonulin and Calprotectin Concentrations in Healthy Children During the First Two Years of Life. An Observational Prospective Cohort Study. J. Clin. Med. 2020, 9, 777. [Google Scholar] [CrossRef] [PubMed]
- Günaydın Şahin, B.S.; Keskindemirci, G.; Özden, T.A.; Durmaz, Ö.; Gökçay, G. Faecal calprotectin levels during the first year of life in healthy children. J. Paediatr. Child Health 2020, 56, 1806–1811. [Google Scholar] [CrossRef] [PubMed]
- Rutayisire, E.; Huang, K.; Liu, Y.; Tao, F. The mode of delivery affects the diversity and colonization pattern of the gut microbiota during the first year of infants’ life: A systematic review. BMC Gastroenterol. 2016, 16, 86. [Google Scholar] [CrossRef]
- Stinson, L.F.; Payne, M.S.; Keelan, J.A. A Critical Review of the Bacterial Baptism Hypothesis and the Impact of Cesarean Delivery on the Infant Microbiome. Front. Med. 2018, 5, 135. [Google Scholar] [CrossRef] [PubMed]
- Malíčková, K.; Francová, I.; Lukáš, M.; Kolář, M.; Králíková, E.; Bortlík, M.; Ďuricová, D.; Štěpánková, L.; Zvolská, K.; Pánková, A.; et al. Fecal zonulin is elevated in Crohn’s disease and in cigarette smokers. Pract. Lab. Med. 2017, 9, 39–44. [Google Scholar] [CrossRef]
- Li, F.; Ma, J.; Geng, S.; Wang, J.; Ren, F.; Sheng, X. Comparison of the different kinds of feeding on the level of fecal calprotectin. Early Hum. Dev. 2014, 90, 471–475. [Google Scholar] [CrossRef]
- Nevado, R.; Forcén, R.; Layunta, E.; Murillo, M.D.; Grasa, L. Neomycin and bacitracin reduce the intestinal permeability in mice and increase the expression of some tight-junction proteins. Rev. Esp. Enferm. Dig. 2015, 107, 672–676. [Google Scholar] [CrossRef][Green Version]
- Skonieczna-Żydecka, K.; Janda, K.; Kaczmarczyk, M.; Marlicz, W.; Łoniewski, I.; Łoniewska, B. The Effect of Probiotics on Symptoms, Gut Microbiota and Inflammatory Markers in Infantile Colic: A Systematic Review, Meta-Analysis and Meta-Regression of Randomized Controlled Trials. J. Clin. Med. 2020, 9, 999. [Google Scholar] [CrossRef]
- Ramezani Ahmadi, A.; Sadeghian, M.; Alipour, M.; Ahmadi Taheri, S.; Rahmani, S.; Abbasnezhad, A. The Effects of Probiotic/Synbiotic on Serum Level of Zonulin as a Biomarker of Intestinal Permeability: A Systematic Review and Meta-Analysis. Iran. J. Public Health 2020, 49, 1222–1231. [Google Scholar] [CrossRef]
- Han, C.; Ding, Z.; Shi, H.; Qian, W.; Hou, X.; Lin, R. The Role of Probiotics in Lipopolysaccharide-Induced Autophagy in Intestinal Epithelial Cells. Cell. Physiol. Biochem. 2016, 38, 2464–2478. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, J.; Heslehurst, N.; Hall, J.; Schoenaker, D.A.J.M.; Hutchinson, J.; Cade, J.E.; Poston, L.; Barrett, G.; Crozier, S.R.; Barker, M.; et al. Before the beginning: Nutrition and lifestyle in the preconception period and its importance for future health. Lancet 2018, 391, 1830–1841. [Google Scholar] [CrossRef]

| Variables | Median (Min–Max) |
|---|---|
| Age (years) | 31.02 (27–34) * |
| Maternal weight at visit 1 (kg) | 65.00 (57–72) * |
| Maternal BMI at visit 1 (kg/m2) | 22.74 (20.9–26.5) * |
| Maternal weight during labor (kg) | 80.00 (70.5–88.5) * |
| Maternal BMI during labor (kg/m2) | 28.53 (26–31.2) * |
| Parity | 2 (1–2) * |
| Gestation age (weeks) | 39.00 (38–39) * |
| Vaginal delivery n (%) | 44 (44) |
| Cesarean section n (%) | 56 (56) |
| Baby birth weight | 3300 (2990–3565) * |
| APGAR score at 5th min. | 10 (all 10) * |
| n | Q25 | Median | Q75 | |
|---|---|---|---|---|
| LPS (pg/g) | ||||
| 0 months (at birth) | 100 | 34.12 | 43.16 | 59.30 |
| 3 months | 96 | 31.20 | 37.61 | 48.01 |
| 6 months | 90 | 27.75 | 36.99 | 48.36 |
| 12 months | 84 | 32.90 | 48.29 | 67.86 |
| occludin (ng/g) | ||||
| 0 months (at birth) | 100 | 2.05 | 2.36 | 3.39 |
| 3 months | 96 | 2.02 | 2.25 | 2.88 |
| 6 months | 90 | 1.68 | 2.17 | 2.63 |
| 12 months | 84 | 1.83 | 2.17 | 2.53 |
| zonulin (ng/g) | ||||
| 0 months (at birth) | 100 | 45.24 | 74.14 | 106.05 |
| 3 months | 96 | 48.75 | 68.84 | 82.40 |
| 6 months | 90 | 38.50 | 63.41 | 72.27 |
| 12 months | 84 | 25.93 | 43.88 | 77.12 |
| Variable | Month | LPS | Occludin | Zonulin |
|---|---|---|---|---|
| p * | p * | p * | ||
| Mother’s education | 0 | 0.78 | 0.54 | 0.90 |
| 3 | 0.90 | 0.25 | 0.93 | |
| 6 | 0.92 | 0.87 | 0.29 | |
| 12 | 0.59 | 0.74 | 0.46 | |
| Cigarette smoking | 0 | 0.61 | 0.71 | 0.56 |
| 3 | 0.86 | 0.68 | 0.73 | |
| 6 | 0.53 | 0.68 | 0.48 | |
| 12 | 0.79 | 0.56 | 0.77 | |
| History of allergy | 0 | 0.66 | 0.28 | 0.55 |
| 3 | 0.50 | 0.10 | 0.41 | |
| 6 | 0.61 | 0.60 | 0.73 | |
| 12 | 0.73 | 0.67 | 0.43 | |
| Breastfeeding | 0 | 0.77 | 0.35 | 0.51 |
| 3 | 0.88 | 0.56 | 0.45 | |
| 6 | 0.54 | 0.28 | 0.26 | |
| 12 | 0.65 | 0.18 | 0.83 | |
| Formula feeding | 0 | 0.49 | 0.55 | 0.26 |
| 3 | 0.45 | 0.98 | 0.23 | |
| 6 | 0.47 | 0.50 | 0.74 | |
| 12 | 0.63 | 0.94 | 0.44 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sochaczewska, D.; Ziętek, M.; Dołęgowska, B.; Kordek, A.; Szczuko, M. Implications of Indirect Biomarkers of Intestinal Permeability in the Stools of Newborns and Infants with Perinatal Risk Factors for Intestinal Colonization Disorders and Infant Feeding Patterns. Nutrients 2022, 14, 2224. https://doi.org/10.3390/nu14112224
Sochaczewska D, Ziętek M, Dołęgowska B, Kordek A, Szczuko M. Implications of Indirect Biomarkers of Intestinal Permeability in the Stools of Newborns and Infants with Perinatal Risk Factors for Intestinal Colonization Disorders and Infant Feeding Patterns. Nutrients. 2022; 14(11):2224. https://doi.org/10.3390/nu14112224
Chicago/Turabian StyleSochaczewska, Diana, Maciej Ziętek, Barbara Dołęgowska, Agnieszka Kordek, and Małgorzata Szczuko. 2022. "Implications of Indirect Biomarkers of Intestinal Permeability in the Stools of Newborns and Infants with Perinatal Risk Factors for Intestinal Colonization Disorders and Infant Feeding Patterns" Nutrients 14, no. 11: 2224. https://doi.org/10.3390/nu14112224
APA StyleSochaczewska, D., Ziętek, M., Dołęgowska, B., Kordek, A., & Szczuko, M. (2022). Implications of Indirect Biomarkers of Intestinal Permeability in the Stools of Newborns and Infants with Perinatal Risk Factors for Intestinal Colonization Disorders and Infant Feeding Patterns. Nutrients, 14(11), 2224. https://doi.org/10.3390/nu14112224







