Association between Hyperglycemia at Hospital Presentation and Hospital Outcomes in COVID-19 Patients with and without Type 2 Diabetes: A Retrospective Cohort Study of Hospitalized Inner-City COVID-19 Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Study Measurements
2.3. Statistical Analysis
3. Results
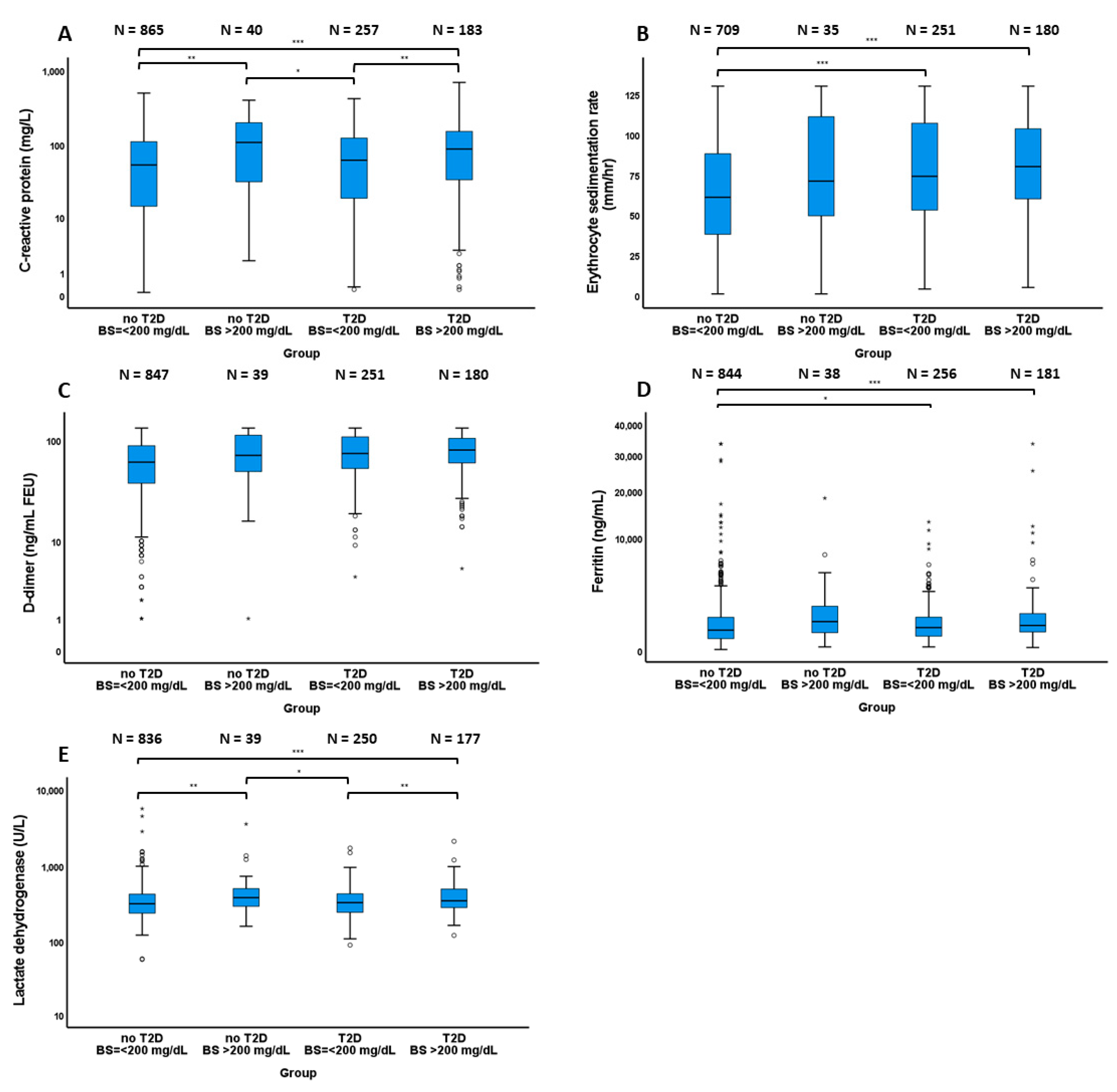
3.1. Inflammatory Marker Levels
3.2. Univariate Comparisons between Patients with and without Hyperglycemia
3.3. Multivariate Comparisons between Patients with and without Hyperglycemia
3.4. Comparisons between Hyperglycemic Patients with and without Type 2 Diabetes
3.5. Association of Long-Term Glycemic Control and Use of Anti-Diabetic Medication and Hospital Outcomes
3.6. Association between Pre-Existing Kidney Dysfunction and In-Hospital Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.-L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2020. [Google Scholar] [CrossRef]
- The Lancet Infectious Disease. COVID-19, a pandemic or not? Lancet Infect. Dis. 2020, 20, 383. [Google Scholar] [CrossRef]
- Kordzadeh-Kermani, E.; Khalili, H.; Karimzadeh, I. Pathogenesis, clinical manifestations and complications of coronavirus disease 2019 (COVID-19). Future Microbiol. 2020, 15, 1287–1305. [Google Scholar] [CrossRef] [PubMed]
- Wiersinga, W.J.; Rhodes, A.; Cheng, A.C.; Peacock, S.J.; Prescott, H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA 2020, 324, 782–793. [Google Scholar] [CrossRef]
- Palaiodimos, L.; Chamorro-Pareja, N.; Karamanis, D.; Li, W.; Zavras, P.D.; Chang, K.M.; Mathias, P.; Kokkinidis, D.G. Diabetes is associated with increased risk for in-hospital mortality in patients with COVID-19: A systematic review and meta-analysis comprising 18,506 patients. Hormones 2020, 1–10. [Google Scholar] [CrossRef]
- Roncon, L.; Zuin, M.; Rigatelli, G.; Zuliani, G. Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome. J. Clin. Virol. 2020, 127, 104354. [Google Scholar] [CrossRef] [PubMed]
- Shang, L.; Shao, M.; Guo, Q.; Shi, J.; Zhao, Y.; Xiaokereti, J.; Tang, B. Diabetes Mellitus is Associated with Severe Infection and Mortality in Patients with COVID-19: A Systematic Review and Meta-analysis. Arch. Med. Res. 2020, 51, 700–709. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.; Pritchard, A.L.; Treweeke, A.T.; Rossi, A.G.; Brace, N.; Cahill, P.; MacRury, S.M.; Wei, J.; Megson, I.L. Why Is COVID-19 More Severe in Patients with Diabetes? The Role of Angiotensin-Converting Enzyme 2, Endothelial Dysfunction and the Immunoinflammatory System. Front. Cardiovasc. Med. 2021, 7, 392. [Google Scholar] [CrossRef] [PubMed]
- Muniangi-Muhitu, H.; Akalestou, E.; Salem, V.; Misra, S.; Oliver, N.S.; Rutter, G.A. Covid-19 and Diabetes: A Complex Bidirectional Relationship. Front. Endocrinol. 2020, 11, 582936. [Google Scholar] [CrossRef]
- Kusmartseva, I.; Wu, W.; Syed, F.; Van Der Heide, V.; Jorgensen, M.; Joseph, P.; Tang, X.; Candelario-Jalil, E.; Yang, C.; Nick, H.; et al. Expression of SARS-CoV-2 Entry Factors in the Pancreas of Normal Organ Donors and Individuals with COVID-19. Cell Metab. 2020, 32, 1041–1051.e1046. [Google Scholar] [CrossRef]
- Mazori, A.Y.; Bass, I.R.; Chan, L.; Mathews, K.S.; Altman, D.R.; Saha, A.; Soh, H.; Wen, H.H.; Bose, S.; Leven, E.; et al. Hyperglycemia is Associated with Increased Mortality in Critically Ill Patients with COVID-19. Endocr. Pract. 2021, 27, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Fadini, G.P.; Morieri, M.L.; Boscari, F.; Fioretto, P.; Maran, A.; Busetto, L.; Bonora, B.M.; Selmin, E.; Arcidiacono, G.; Pinelli, S.; et al. Newly-diagnosed diabetes and admission hyperglycemia predict COVID-19 severity by aggravating respiratory deterioration. Diabetes Res. Clin. Pract. 2020, 168, 108374. [Google Scholar] [CrossRef]
- Yang, Y.; Cai, Z.; Zhang, J. Hyperglycemia at admission is a strong predictor of mortality and severe/critical complications in COVID-19 patients: A meta-analysis. Biosci. Rep. 2021, 41, BSR20203584. [Google Scholar] [CrossRef] [PubMed]
- Prattichizzo, F.; Giuliani, A.; Sabbatinelli, J.; Matacchione, G.; Ramini, D.; Bonfigli, A.R.; Rippo, M.R.; de Candia, P.; Procopio, A.D.; Olivieri, F.; et al. Prevalence of residual inflammatory risk and associated clinical variables in patients with type 2 diabetes. Diabetes Obes. Metab. 2020, 22, 1696–1700. [Google Scholar] [CrossRef]
- Sachdeva, S.; Desai, R.; Gupta, U.; Prakash, A.; Jain, A.; Aggarwal, A. Admission Hyperglycemia in Non-diabetics Predicts Mortality and Disease Severity in COVID-19: A Pooled Analysis and Meta-summary of Literature. SN Compr. Clin. Med. 2020, 1–6. [Google Scholar] [CrossRef]
- Godinjak, A.; Iglica, A.; Burekovic, A.; Jusufovic, S.; Ajanovic, A.; Tancica, I.; Kukuljac, A. Hyperglycemia in Critically Ill Patients: Management and Prognosis. Med. Arch. 2015, 69, 157–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palermo, N.E.; Gianchandani, R.Y.; McDonnell, M.E.; Alexanian, S.M. Stress Hyperglycemia During Surgery and Anesthesia: Pathogenesis and Clinical Implications. Curr. Diabetes Rep. 2016, 16, 33. [Google Scholar] [CrossRef] [PubMed]
- Dungan, K.M.; Braithwaite, S.S.; Preiser, J.-C. Stress hyperglycaemia. Lancet 2009, 373, 1798–1807. [Google Scholar] [CrossRef]
- Yu, W.-K.; Li, W.-Q.; Li, N.; Li, J.-S. Influence of acute hyperglycemia in human sepsis on inflammatory cytokine and counterregulatory hormone concentrations. World J. Gastroenterol. 2003, 9, 1824–1827. [Google Scholar] [CrossRef] [PubMed]
- Stentz, F.B.; Umpierrez, G.E.; Cuervo, R.; Kitabchi, A.E. Proinflammatory Cytokines, Markers of Cardiovascular Risks, Oxidative Stress, and Lipid Peroxidation in Patients with Hyperglycemic Crises. Diabetes 2004, 53, 2079. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boddu, S.K.; Aurangabadkar, G.; Kuchay, M.S. New onset diabetes, type 1 diabetes and COVID-19. Diabetes Metab. Syndr. 2020, 14, 2211–2217. [Google Scholar] [CrossRef]
- Nassar, M.; Nso, N.; Baraka, B.; Alfishawy, M.; Mohamed, M.; Nyabera, A.; Sachmechi, I. The association between COVID-19 and type 1 diabetes mellitus: A systematic review. Diabetes Metab. Syndr. 2021, 15, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Rubino, F.; Amiel, S.A.; Zimmet, P.; Alberti, G.; Bornstein, S.; Eckel, R.H.; Mingrone, G.; Boehm, B.; Cooper, M.E.; Chai, Z.; et al. New-Onset Diabetes in Covid-19. N. Engl. J. Med. 2020, 383, 789–790. [Google Scholar] [CrossRef] [PubMed]
- Sardu, C.; D’Onofrio, N.; Balestrieri, M.L.; Barbieri, M.; Rizzo, M.R.; Messina, V.; Maggi, P.; Coppola, N.; Paolisso, G.; Marfella, R. Outcomes in Patients with Hyperglycemia Affected by COVID-19: Can We Do More on Glycemic Control? Diabetes Care 2020, 43, 1408–1415. [Google Scholar] [CrossRef]
- Marfella, R.; Sasso, F.C.; Cacciapuoti, F.; Portoghese, M.; Rizzo, M.R.; Siniscalchi, M.; Carbonara, O.; Ferraraccio, F.; Torella, M.; Petrella, A.; et al. Tight Glycemic Control May Increase Regenerative Potential of Myocardium during Acute Infarction. J. Clin. Endocrinol. Metab. 2012, 97, 933–942. [Google Scholar] [CrossRef] [Green Version]
- Sasso, F.C.; Rinaldi, L.; Lascar, N.; Marrone, A.; Pafundi, P.C.; Adinolfi, L.E.; Marfella, R. Role of Tight Glycemic Control during Acute Coronary Syndrome on CV Outcome in Type 2 Diabetes. J. Diabetes Res. 2018, 2018, 3106056. [Google Scholar] [CrossRef] [Green Version]
- Corrao, S.; Santalucia, P.; Argano, C.; Djade, C.D.; Barone, E.; Tettamanti, M.; Pasina, L.; Franchi, C.; Kamal Eldin, T.; Marengoni, A.; et al. Gender-differences in disease distribution and outcome in hospitalized elderly: Data from the REPOSI study. Eur. J. Intern. Med. 2014, 25, 617–623. [Google Scholar] [CrossRef] [Green Version]
- Marcucci, M.; Franchi, C.; Nobili, A.; Mannucci, P.M.; Ardoino, I.; Investigators, R. Defining Aging Phenotypes and Related Outcomes: Clues to Recognize Frailty in Hospitalized Older Patients. J. Gerontol. Ser. A 2017, 72, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Prattichizzo, F.; Sabbatinelli, J.; de Candia, P.; Olivieri, F.; Ceriello, A. Tackling the pillars of ageing to fight COVID-19. Lancet Healthy Longev. 2021, 2, e191. [Google Scholar] [CrossRef]
- Pal, R.; Banerjee, M.; Mukherjee, S.; Bhogal, R.S.; Kaur, A.; Bhadada, S.K. Dipeptidyl peptidase-4 inhibitor use and mortality in COVID-19 patients with diabetes mellitus: An updated systematic review and meta-analysis. Ther. Adv. Endocrinol. Metab. 2021, 12. [Google Scholar] [CrossRef]
- Solerte, S.B.; D’Addio, F.; Trevisan, R.; Lovati, E.; Rossi, A.; Pastore, I.; Dell’Acqua, M.; Ippolito, E.; Scaranna, C.; Bellante, R.; et al. Sitagliptin Treatment at the Time of Hospitalization Was Associated with Reduced Mortality in Patients with Type 2 Diabetes and COVID-19: A Multicenter, Case-Control, Retrospective, Observational Study. Diabetes Care 2020, 43, 2999. [Google Scholar] [CrossRef] [PubMed]
- Mirabelli, M.; Chiefari, E.; Puccio, L.; Foti, D.P.; Brunetti, A. Potential Benefits and Harms of Novel Antidiabetic Drugs During COVID-19 Crisis. Int. J. Environ. Res. Public Health 2020, 17, 3664. [Google Scholar] [CrossRef] [PubMed]
- Umakanthan, S.; Chattu, V.K.; Ranade, A.V.; Das, D.; Basavarajegowda, A.; Bukelo, M. A rapid review of recent advances in diagnosis, treatment and vaccination for COVID-19. AIMS Public Health 2021, 8, 137–153. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Patients without Type 2 Diabetes | Patients with Type 2 Diabetes | ||||
|---|---|---|---|---|---|---|
| Blood Glucose > 200 mg/dL (N = 42) | Blood Glucose ≤ 200 mg/dL (N = 934) | p-Value | Blood Glucose > 200 mg/dL (N = 193) | Blood Glucose ≤ 200 mg/dL (N = 265) | p-Value | |
| Age (years old) | 57.0 (46.5–69.0) | 52.0 (38.0–64.25) | 0.055 | 63.0 (53.0–72.0) | 65.0 (57.0–74.0) | 0.065 |
| Female sex | 17 (40.5%) | 409 (43.8%) | 0.672 | 79 (40.9%) | 137 (51.7%) | 0.023 * |
| BMI (kg/m2) | 28.9 (24.1–32.7) | 28.5 (24.5–33.9) | 0.511 | 28.8 (25.1–33.0) | 29.9 (25.2–35.6) | 0.156 |
| Race | ||||||
| White | 24 (57.1%) | 506 (54.2%) | 0.439 | 81 (42.0% | 109 (41.1%) | 0.974 |
| Black | 15 (35.7%) | 393 (42.1%) | 106 (54.9%) | 147 (55.5%) | ||
| Other | 3 (7.1%) | 35 (3.7%) | 6 (3.1%) | 9 (3.4%) | ||
| History of smoking | 13 (31.0%) | 317 (33.9%) | 0.869 | 72 (37.3%) | 132 (49.8%) | 0.008 * |
| Alcohol use | 6 (14.3%) | 299 (32.0%) | 0.015* | 53 (27.5%) | 87 (32.8%) | 0.218 |
| Control of diabetes | ||||||
| HbA1C < 7% | - | - | - | 133 (68.9%) | 217 (81.9%) | 0.005 * |
| HbA1C 7– < 8% | - | - | - | 16 (8.3%) | 20 (7.5%) | |
| HbA1C 8– < 9% | - | - | - | 11 (5.7%) | 8 (3.0%) | |
| HbA1C 9– < 10% | - | - | - | 8 (4.1%) | 8 (3.0%) | |
| HbA1C ≥ 10% | - | - | - | 25 (13.0%) | 12 (4.5%) | |
| Antidiabetic medications | ||||||
| Metformin | - | - | - | 91 (47.2%) | 102 (38.5%) | 0.064 |
| DPP-4 inhibitors | - | - | - | 28 (14.5%) | 35 (13.2%) | 0.690 |
| SGLT-2 inhibitors | - | - | - | 9 (4.7%) | 9 (3.4%) | 0.491 |
| Sulfonylureas | - | - | - | 49 (25.4%) | 36 (13.6%) | 0.001 * |
| GLP-1 agonists | - | - | - | 29 (15.0%) | 29 (10.9%) | 0.195 |
| Insulin | 129 (66.8%) | 161 (60.8%) | 0.182 | |||
| Underlying diseases | ||||||
| Hypertension | 13 (31.0%) | 361 (38.7%) | 0.315 | 158 (81.9%) | 232 (87.5%) | 0.091 |
| Dyslipidemia | 7 (16.7%) | 205 (21.9%) | 0.417 | 131 (67.9%) | 178 (67.2%) | 0.874 |
| Coronary heart disease | 2 (4.8%) | 47 (5.0%) | 1.000 | 21 (10.9%) | 43 (16.2%) | 0.103 |
| Heart failure | 2 (4.8%) | 63 (6.7%) | 0.614 | 19 (9.8%) | 60 (22.6%) | <0.001 * |
| Cerebrovascular disease | 0 (0.0%) | 27 (2.9%) | 0.625 | 5 (2.6%) | 27 (10.2%) | 0.001 * |
| Asthma | 4 (9.5%) | 119 (12.7%) | 0.811 | 27 (14.0%) | 54 (20.4%) | 0.077 |
| COPD | 2 (4.8%) | 61 (6.5%) | 1.000 | 7 (3.6%) | 33 (12.5%) | 0.001 * |
| CKD | 0 (0.0%) | 76 (8.1%) | 0.069 | 46 (23.8%) | 93 (35.1%) | 0.010 * |
| ESRD | 0 (0.0%) | 27 (2.9%) | 0.264 | 5 (2.6%) | 35 (13.2%) | <0.001 * |
| Malignancy | 3 (7.1%) | 80 (8.6%) | 1.000 | 20 (10.4%) | 46 (17.4%) | 0.035 * |
| HIV infection | 2 (4.8%) | 30 (3.2%) | 0.644 | 4 (2.1%) | 6 (2.3%) | 0.890 |
| In-hospital medical therapy for COVID-19 | ||||||
| Azithromycin | 11 (26.2%) | 365 (39.1%) | 0.093 | 91 (47.2%) | 129 (48.7%) | 0.746 |
| Colchicine | 6 (14.3%) | 136 (14.6%) | 0.961 | 32 (16.6%) | 44 (16.6%) | 0.955 |
| Hydroxychloroquine | 11 (26.2%) | 425 (45.5%) | 0.014 * | 106 (54.9%) | 140 (52.8%) | 0.657 |
| Corticosteroids | 9 (21.4%) | 77 (8.2%) | 0.003 * | 23 (11.9%) | 25 (9.4%) | 0.392 |
| IL-6 antibodies | 6 (14.3%) | 172 (18.4%) | 0.498 | 50 (25.9%) | 56 (21.1%) | 0.232 |
| IL-1 receptor antagonists | 1 (2.4%) | 30 (3.2%) | 1.000 | 5 (2.6%) | 11 (4.2%) | 0.446 |
| Remdesivir | 6 (14.3%) | 49 (5.2%) | 0.013 * | 8 (4.1%) | 8 (3.0%) | 0.517 |
| Hospital Outcomes | Patients without Type 2 diabetes | Patients with Type 2 Diabetes | ||||
|---|---|---|---|---|---|---|
| Blood Glucose > 200 mg/dL (N = 42) | Blood Glucose ≤ 200 mg/dL (N = 934) | p-Value | Blood Glucose > 200 mg/dL (N = 193) | Blood Glucose ≤ 200 mg/dL (N = 265) | p-Value | |
| Death | 9 (21.4%) | 62 (6.6%) | <0.001 * | 25 (13.0%) | 36 (13.6%) | 0.844 |
| ICU admission | 16 (40.0%) | 151 (16.2%) | <0.001 * | 48 (24.9%) | 54 (20.4%) | 0.254 |
| Intubation | 15 (35.7%) | 100 (10.7%) | <0.001 * | 34 (17.6%) | 36 (13.6%) | 0.236 |
| Hospital length of stay (days) | 10.1 ± 16.8 | 7.1 ± 8.3 | 0.036 * | 9.4 ± 11.6 | 8.5 ± 9.0 | 1.000 |
| ARDS | 6 (14.3%) | 70 (7.5%) | 0.108 | 25 (13.0%) | 23 (8.7%) | 0.140 |
| Myocardial infarction | 3 (7.1%) | 42 (4.5%) | 0.437 | 17 (8.8%) | 21 (7.9%) | 0.735 |
| Acute kidney injury | 17 (40.5%) | 219 (23.4%) | 0.012 * | 104 (53.9%) | 96 (36.2%) | <0.001 * |
| Severe sepsis/septic shock | 10 (23.8%) | 73 (7.8%) | <0.001 * | 26 (13.5%) | 40 (15.1%) | 0.625 |
| Hospital Outcomes | Patients without Type 2 Diabetes | Patients with Type 2 Diabetes | ||||
|---|---|---|---|---|---|---|
| Adjusted OR | 95% CI | p-Value | Adjusted OR | 95% CI | p-Value | |
| Death | 4.46 | 1.77–11.20 | 0.001 * | 1.55 | 0.81–2.98 | 0.184 |
| ICU admission | 3.71 | 1.84–7.48 | <0.001 * | 1.69 | 1.03–2.79 | 0.039 * |
| Intubation | 4.82 | 2.39–9.72 | <0.001 * | 1.68 | 0.94–2.98 | 0.078 |
| ARDS | 1.92 | 0.75–4.91 | 0.176 | 1.81 | 0.93–3.53 | 0.081 |
| Myocardial infarction | 1.69 | 0.47–6.03 | 0.421 | 1.55 | 0.73–3.27 | 0.252 |
| Acute kidney injury | 2.29 | 1.14–4.60 | 0.020 * | 2.45 | 1.54–3.90 | <0.001 * |
| Severe sepsis/septic shock | 4.14 | 1.85–9.24 | <0.001 * | 1.05 | 0.58–1.88 | 0.882 |
| Hospital Outcomes | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| Patients with Type 2 Diabetes (N = 42) | Patients without Type 2 Diabetes (N = 193) | p-Value | Adjusted OR | 95% CI | p-Value | |
| Death | 25 (13.0%) | 9 (21.4%) | 0.157 | 5.05 | 1.34–18.99 | 0.016 * |
| ICU admission | 48 (24.9%) | 16 (40.0%) | 0.051 | 2.68 | 1.07–6.71 | 0.035 * |
| Intubation | 34 (17.6%) | 15 (35.7%) | 0.009 * | 3.78 | 1.37–10.46 | 0.010 * |
| ARDS | 25 (13.0%) | 6 (14.3%) | 0.817 | 1.44 | 0.42–4.94 | 0.567 |
| Myocardial infarction | 17 (8.8%) | 3 (7.1%) | 1.000 | 0.61 | 0.11–3.31 | 0.570 |
| Acute kidney injury | 104 (53.9%) | 17 (40.5%) | 0.115 | 1.24 | 0.49–3.15 | 0.649 |
| Severe sepsis/septic shock | 26 (13.5%) | 10 (23.8%) | 0.092 | 3.90 | 1.28–11.99 | 0.017 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Charoenngam, N.; Alexanian, S.M.; Apovian, C.M.; Holick, M.F. Association between Hyperglycemia at Hospital Presentation and Hospital Outcomes in COVID-19 Patients with and without Type 2 Diabetes: A Retrospective Cohort Study of Hospitalized Inner-City COVID-19 Patients. Nutrients 2021, 13, 2199. https://doi.org/10.3390/nu13072199
Charoenngam N, Alexanian SM, Apovian CM, Holick MF. Association between Hyperglycemia at Hospital Presentation and Hospital Outcomes in COVID-19 Patients with and without Type 2 Diabetes: A Retrospective Cohort Study of Hospitalized Inner-City COVID-19 Patients. Nutrients. 2021; 13(7):2199. https://doi.org/10.3390/nu13072199
Chicago/Turabian StyleCharoenngam, Nipith, Sara M. Alexanian, Caroline M. Apovian, and Michael F. Holick. 2021. "Association between Hyperglycemia at Hospital Presentation and Hospital Outcomes in COVID-19 Patients with and without Type 2 Diabetes: A Retrospective Cohort Study of Hospitalized Inner-City COVID-19 Patients" Nutrients 13, no. 7: 2199. https://doi.org/10.3390/nu13072199
APA StyleCharoenngam, N., Alexanian, S. M., Apovian, C. M., & Holick, M. F. (2021). Association between Hyperglycemia at Hospital Presentation and Hospital Outcomes in COVID-19 Patients with and without Type 2 Diabetes: A Retrospective Cohort Study of Hospitalized Inner-City COVID-19 Patients. Nutrients, 13(7), 2199. https://doi.org/10.3390/nu13072199







