Comparison of Salt-Related Knowledge and Behaviors Status of WeChat Users between 2019 and 2020
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. WeChat-Based Survey
2.3. Salt-Related Knowledge and Behavior Scores
2.4. Statistical Analysis
3. Results
3.1. General Information
3.2. Salt-Related Knowledge
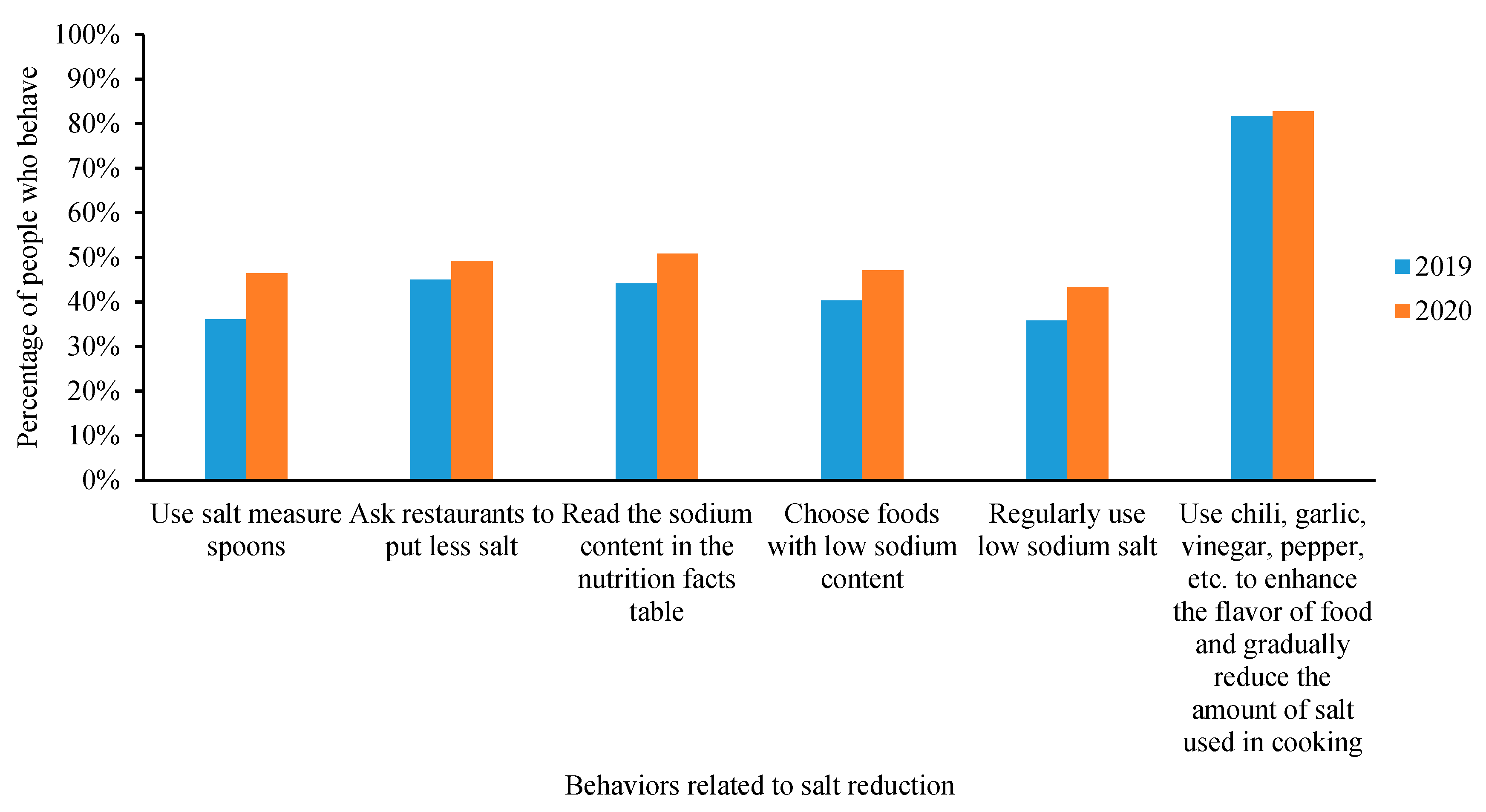
3.3. Salt-Related Behaviors
3.4. Salt-Related Knowledge and Behavior Scores
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, L.H. Non-Communicable and Chronic Diseases Control and Prevention; People’s Medical Publishing House: Beijing, China, 2018. [Google Scholar]
- Theo, V.; Stephen, S.L.; Cristiana, A.; Kaja, M.A.; Mohammad, A.; Mitra, A.; Mohsen, A.; Hedayat, A.; Foad, A.; Ahmed, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar]
- Bureau of Disease Control and Prevention of the National Health and Family Planning Commission. Report on Chinese Resident’s Chronic Diseases and Nutrition; People’s Medical Publishing House: Beijing, China, 2015. [Google Scholar]
- Hu, S.; Gao, R.; Liu, L.; Zhu, M.; Wang, W.; Wang, Y.; Wu, Z.; Li, H.; Gu, D.; Yang, Y.; et al. Summary of the 2018 report on cardiovascular diseases in China. Chin. Circ. J. 2019, 34, 209–220. [Google Scholar]
- Mozaarian, D.; Fahimi, S.; Singh, G.M.; Micha, R.; Khatibzadeh, S.; Engell, R.E.; Lim, S.; Danaei, G.; Ezzati, M.; Powles, J.; et al. Global sodium consumption and death from cardiovascular causes. N. Engl. J. Med. 2014, 371, 624–634. [Google Scholar] [CrossRef]
- Aburto, N.J.; Ziolkovska, A.; Hooper, L.; Elliott, P.; Cappuccio, F.P.; Meerpohl, J.J. Effect of lower sodium intake on health: Systematic review and meta-analyses. BMJ 2013, 346, f1326. [Google Scholar] [CrossRef]
- He, F.J.; Li, J.; Macgregor, G.A. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 2013, 346, f1325. [Google Scholar] [CrossRef]
- GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar]
- World Health Organization. Salt Reduction. Available online: https://www.who.int/news-room/fact-sheets/detail/salt-reduction (accessed on 27 April 2020).
- The State Council Information Office. The State Council Information Office (SCIO) holds Press Briefing on “Report on the Nutrition and Chronic Disease Status of Chinese Residents 2020”. Available online: http://www.gov.cn/xinwen/2020-12/24/content_5572983.htm (accessed on 27 April 2020).
- Li, Y.; Zhang, P.; Wu, J.; Ma, J.; Xu, J.; Zhang, X.; Luo, R.; Liu, M.; Sun, Y.; Li, X.; et al. Twenty-Four-Hour Urinary Sodium and Potassium Excretion and Their Associations with Blood Pressure Among Adults in China: Baseline Survey of Action on Salt China. Hypertension 2020, 76, 1580–1588. [Google Scholar] [CrossRef]
- World Health Organization. Guideline: Sodium Intake for Adults and Children; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- Chinese Nutrition Society. Dietary Guidelines for Chinese Residents 2016; People’s Medical Publishing House: Beijing, China, 2016. [Google Scholar]
- Shao, S.; Hua, Y.; Yang, Y.; Liu, X.; Fan, J.; Zhang, A.; Xiang, J.; Li, M.; Yan, L.L. Salt reduction in China: A state-of-the-art review. Risk Manag. Healthc. Policy 2017, 10, 17–28. [Google Scholar] [CrossRef]
- Xu, A.; Ma, J.; Guo, X.; Wang, L.; Wu, J.; Zhang, J.; Bai, Y.; Xu, J.; Lu, Z.; Xu, Z.; et al. Association of a Province-Wide Intervention With Salt Intake and Hypertension in Shandong Province, China, 2011–2016. JAMA Intern. Med. 2020, 180, 877–886. [Google Scholar] [CrossRef]
- He, F.; Wu, Y.; Feng, X.; Ma, J.; Ma, Y.; Wang, H.; Zhang, J.; Yuan, J.; Lin, C.; Caryl, N.; et al. School based education programme to reduce salt intake in children and their families (School-EduSalt): Cluster randomised controlled trial. BMJ 2015, 350, h770. [Google Scholar] [CrossRef]
- Li, Y.; Wang, J.; Zhang, X.; Wu, J.; Liang, X. Retrospect and Prospect of Healthy Lifestyle for All, 2007–2015. Chin. J. Health Edu. 2016, 32, 1143–1145. [Google Scholar]
- Chinese Center for Disease Control and Prevention. “All Action, Salt Control by All”, The First China Salt Reduction Conference Was Successfully Held. Available online: http://www.chinacdc.cn/yw_9324/201908/t20190828_205038.html (accessed on 27 April 2020).
- Zhang, J.; Astell-Burt, T.; Seo, D.C.; Feng, X.; Kong, L.; Zhao, W.; Li, N.; Li, Y.; Yu, S.; Feng, G.; et al. Multilevel evaluation of “China Healthy Lifestyles for All”, a nationwide initiative to promote lower intakes of salt and edible oil. Prev. Med. 2014, 67, 210–215. [Google Scholar] [CrossRef]
- Yang, Y.; He, D.; Wei, L.; Wang, S.; Chen, L.; Luo, M.; Mao, Z. Association between diet-related knowledge, attitudes, behaviors, and self-rated health in Chinese adult residents: A population-based study. BMC Public Health 2020, 20, 720. [Google Scholar] [CrossRef]
- Bhana, N.; Utter, J.; Eyles, H. Knowledge, Attitudes and Behaviours Related to Dietary Salt Intake in High-Income Countries: A Systematic Review. Curr. Nutr. Rep. 2018, 7, 183–197. [Google Scholar] [CrossRef]
- Grimes, C.A.; Khokhar, D.; Bolton, K.A.; Trieu, K.; Potter, J.; Davidson, C.; Dunford, E.K.; Jan, S.; Woodward, M.; Bolam, B.; et al. Salt-Related Knowledge, Attitudes and Behaviors (KABs) among Victorian Adults Following 22-Months of a Consumer Awareness Campaign. Nutrients 2020, 12, 1216. [Google Scholar] [CrossRef]
- Patel, D.; Cogswell, M.E.; John, K.; Creel, S.; Ayala, C. Knowledge, Attitudes, and Behaviors Related to Sodium Intake and Reduction Among Adult Consumers in the United States. Am. J. Health Promot. 2017, 31, 68–75. [Google Scholar] [CrossRef]
- Ghimire, K.; Adhikari, T.B.; Rijal, A.; Kallestrup, P.; Henry, M.E.; Neupane, D. Knowledge, attitudes, and practices related to salt consumption in Nepal: Findings from the community-based management of non-communicable diseases project in Nepal (COBIN). J. Clin. Hypertens. 2019, 21, 739–748. [Google Scholar] [CrossRef]
- Iaccarino, I.P.; D’Elia, L.; Cairella, G.; Sabino, P.; Scalfi, L.; Fabbri, A.; Galletti, F.; Garbagnati, F.; Lionetti, L.; Paolella, G.; et al. Salt and Health: Survey on Knowledge and Salt Intake Related Behaviour in Italy. Nutrients 2020, 12, 279. [Google Scholar] [CrossRef]
- Jessen, N.; Santos, A.; Damasceno, A.; Silva-Matos, C.; Severo, M.; Padrao, P.; Lunet, N. Knowledge and behaviors regarding salt intake in Mozambique. Eur. J. Clin. Nutr. 2018, 72, 1690–1699. [Google Scholar] [CrossRef]
- Hu, C.; Zhang, M.; Zhang, W.; Zhang, X.; Zhao, Z.; Huang, Z.; Li, C.; Wang, L. Salt-Related Knowledge, Behaviors, and Associated Factors Among Chinese Adults—China, 2015. China CDC Wkly. 2020, 2, 678–683. [Google Scholar] [CrossRef]
- Bureau of Disease Control and Prevention of the National Health Commission. Notice on Launching Publicity Activities for the 2019 National Healthy Lifestyle Month. Available online: http://www.jiankang121.cn/NewsDetail.aspx?id=681 (accessed on 27 April 2020).
- World Health Organization. The “5G” Era of Salt Reduction is Coming. Available online: https://baijiahao.baidu.com/s?id=1643361964880212894&wfr=spider&for=pc (accessed on 27 April 2020).
- Chinese Center for Disease Control and Prevention. Joint Initiative of Promoting the “Reduction of Salt, Oil, and Sugar” in the Food Industry. Available online: http://www.chinacdc.cn/gsywlswxx_9503/bdbs_1/201809/t20180928_194371.html (accessed on 27 April 2020).
- Sun, M.; Yang, L.; Chen, W.; Luo, H.; Zheng, K.; Zhang, Y.; Lian, T.; Yang, Y.; Ni, J. Current status of official WeChat accounts for public health education. J. Public Health 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Yu, Q.; Xu, L.; Li, L.; Zhi, M.; Gu, Y.; Wang, X.; Guo, H.; Li, Y.; Fan, Y.; Yang, B.; et al. Internet and WeChat used by patients with Crohn’s disease in China: A multi-center questionnaire survey. BMC Gastroenterol. 2019, 19, 97. [Google Scholar] [CrossRef]
- Chen, S.; Shan, L.C.; Tao, W.; Lu, T.; Regan, A.; Han, H.; Guo, L.; Deng, T.; Wall, P. A survey of Chinese consumers’ knowledge, beliefs and behavioural intentions regarding salt intake and salt reduction. Public Health Nutr. 2020, 23, 1450–1459. [Google Scholar] [CrossRef]
- Gao, C.; Wang, Z.; Liu, Y.; Lu, Y.; Zhang, X.; Yang, Y. A comprehensive analysis on the range of sodium contents of Chinese various pre-packaged foods. Acta Nutr. Sin. 2017, 39, 217–222. [Google Scholar]
- Xi, B.; Hao, Y.; Liu, F. Salt reduction strategies in China. Lancet 2014, 383, 1128. [Google Scholar] [CrossRef]
- Zhang, J.; Wu, T.; Chu, H.; Feng, X.; Shi, J.; Zhang, R.; Zhang, Y.; Zhang, J.; Li, N.; Yan, L.; et al. Salt intake belief, knowledge, and behavior: A cross-sectional study of older rural Chinese adults. Medicine 2016, 95, e4404. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.; Li, T.; Lou, P.; Chang, G.; Zhang, P.; Chen, P.; Qiao, C.; Dong, Z. Salt intake, knowledge of salt intake, and blood pressure control in Chinese hypertensive patients. J. Am. Soc. Hypertens. 2014, 8, 909–914. [Google Scholar] [CrossRef]
- Zhang, J.; Xu, A.; Shi, X.; Ma, J.; Guo, X.; Lu, Z.; Wang, H.; Li, Y.; Liang, X. The awareness of recommended limit of dietary salt and determinants in Shandong Province, China. Chin. J. Dis. Control. Prev. 2013, 17, 520–524. [Google Scholar]
- Dewey, G.; Wickramasekaran, R.N.; Kuo, T.; Robles, B. Does sodium knowledge affect dietary choices and health behaviors? Results from a survey of Los Angeles county residents. Prev. Chronic. Dis. 2017, 14, E120. [Google Scholar] [CrossRef][Green Version]
- Committee for Revision of Chinese Guidelines for the Management of Hypertension. 2018 Chinese guidelines for the management of hypertension. Chin. J. Cardiovasc. Med. 2019, 24, 1–46. [Google Scholar]
- Promotional Committee of Healthy China Initiative. Healthy China Initiative (2019–2030). 2019. Available online: http://www.nhc.gov.cn/guihuaxxs/s3585u/201907/e9275fb95d5b4295be8308415d4cd1b2.shtml (accessed on 27 April 2020).
- Chen, J.; Tian, Y.; Liao, Y.; Yang, S.; Li, Z.; He, C.; Tu, D.; Sun, X. Salt-restriction-spoon improved the salt intake among residents in China. PLoS ONE 2013, 8, e78963. [Google Scholar] [CrossRef]
- Zhang, X.; Hu, X.; Ma, J.; Zhang, P.; Li, Y.; Luo, R.; He, F.J.; MacGregor, G.A.; Wang, J.; Yin, Z. Cluster randomised controlled trial of home cook intervention to reduce salt intake in China: A protocol study. BMJ Open 2020, 10, e033842. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Yan, L.; Chen, X.; Cai, X.; Jiang, Y.; Wang, L.; Ma, J. Investigation on knowledge, attitude and behavior of salt reduction in Chinese adults, 2010. Chin. J. Prev. Med. 2014, 48, 350–354. [Google Scholar]
- Jia, P.; Liu, L.; Xie, X.; Yuan, C.; Chen, H.; Guo, B.; Zhou, J.; Yang, S. Changes in dietary patterns among youths in China during COVID-19 epidemic: The COVID-19 impact on lifestyle change survey (COINLICS). Appetite 2021, 158, 105015. [Google Scholar] [CrossRef]
- Yang, G.Y.; Lin, X.L.; Fang, A.P.; Zhu, H.L. Eating Habits and Lifestyles during the Initial Stage of the COVID-19 Lockdown in China: A Cross-Sectional Study. Nutrients 2021, 13, 970. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhao, A.; Ke, Y.; Huo, S.; Ma, Y.; Zhang, Y.; Ren, Z.; Li, Z.; Liu, K. Dietary Behaviors in the Post-Lockdown Period and Its Effects on Dietary Diversity: The Second Stage of a Nutrition Survey in a Longitudinal Chinese Study in the COVID-19 Era. Nutrients 2020, 12, 3269. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, B.; Santos, J.A.; Trieu, K.; Thout, S.R.; Johnson, C.; Arcand, J.; Webster, J.; McLean, R. The Science of Salt: A focused review on salt-related knowledge, attitudes and behaviors, and gender differences. J. Clin. Hypertens. 2018, 20, 850–866. [Google Scholar] [CrossRef] [PubMed]


| Questions | Score | Setting | |
|---|---|---|---|
| Salt-related knowledge score (total scores = 13) | Foods that contain salt | 5 | Fine dried noodles = 1, Bread = 1, Biscuit = 1, Cheese = 1, Ice cream = 1 |
| Condiments that contain salt and should be used less | 4 | Soy sauce = 1, Oyster sauce = 1, Bean paste = 1, MSG = 1 | |
| Maximum daily salt intake of healthy adults | 1 | 5 g or 6 g = 1 | |
| Diseases that related to excessive salt intake | 3 | Hypertension = 1, Heart disease = 1, Stroke = 1 | |
| Salt-reduction behavior score (total scores = 6) | Use salt measuring spoons | 1 | Have this behavior = 1 |
| Ask restaurants to use less salt | 1 | Have this behavior = 1 | |
| Read the sodium content on the nutrition facts table | 1 | Have this behavior = 1 | |
| Choose foods with low sodium content | 1 | Have this behavior = 1 | |
| Regularly use low-sodium salt | 1 | Have this behavior = 1 | |
| Use chili, garlic, vinegar, pepper, etc. to enhance the flavor of food and gradually reduce the amount of salt used in cooking | 1 | Have this behavior = 1 | |
| High salt intake behavior score (total scores = 9) | Frequency of using high-salt condiments such as oyster sauce, bean paste, MSG, etc. | 3 | Regularly = 3, Occasionally = 2, Rarely = 1, Never = 0 |
| Frequency of eating processed foods and canned foods | 3 | Regularly = 3, Occasionally = 2, Rarely = 1, Never = 0 | |
| Frequency of eating pickled mustard tubers, salted vegetables and sauce foods | 3 | Regularly = 3, Occasionally = 2, Rarely = 1, Never = 0 |
| Variables | Year 2019 (N = 2109) | Year 2020 (N = 12,732) | χ2 | p-Value | ||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Gender | 0.374 | 0.541 | ||||
| Male | 629 | 29.8 | 3714 | 29.2 | ||
| Female | 1480 | 70.2 | 9018 | 70.8 | ||
| Age | 17.036 | <0.001 | ||||
| ≤45 | 1377 | 65.3 | 7711 | 60.6 | ||
| >45 | 732 | 34.7 | 5021 | 39.4 | ||
| Education level | 251.467 | <0.001 | ||||
| Middle school and below | 170 | 8.1 | 2031 | 16.0 | ||
| High school | 556 | 26.4 | 4214 | 33.1 | ||
| College | 1177 | 55.8 | 5968 | 46.9 | ||
| Postgraduate | 206 | 9.8 | 519 | 4.1 | ||
| Region | 477.862 | <0.001 | ||||
| East | 764 | 36.2 | 5393 | 42.4 | ||
| Middle | 852 | 40.4 | 2482 | 19.5 | ||
| West | 493 | 23.4 | 4857 | 38.1 | ||
| Answering time | 61.155 | <0.001 | ||||
| ≥1–2min | 769 | 36.5 | 3714 | 29.2 | ||
| ≥2–5 min | 1263 | 59.9 | 8195 | 64.4 | ||
| ≥5 min | 77 | 3.7 | 823 | 6.5 | ||
| Self-reported health status | ||||||
| Hypertension | 237 | 11.2 | 1677 | 13.2 | 6.024 | 0.014 |
| Basic health | 1826 | 86.6 | 10790 | 84.7 | 4.776 | 0.029 |
| Salt-related taste | 2.645 | 0.266 | ||||
| Salty | 494 | 23.4 | 2781 | 21.8 | ||
| Moderate | 1113 | 52.8 | 6842 | 53.7 | ||
| Bland | 502 | 23.8 | 3109 | 24.4 | ||
| Willingness for salt reduction | 9.163 | 0.027 | ||||
| Yes | 1861 | 88.2 | 11487 | 90.2 | ||
| No | 130 | 6.2 | 694 | 5.5 | ||
| Do not care | 102 | 4.8 | 485 | 3.8 | ||
| Do not know | 16 | 0.8 | 66 | 0.5 | ||
| Variables | Salt-Related Knowledge Score | Salt Reduction Behavior Score | High-Salt Intake Behavior Score | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | Z | p-Year | 2019 | 2020 | Z | p-Year | 2019 | 2020 | Z | p-Year | |
| Total | 11(3) | 10(4) | 6.908 | <0.001 | 2(3) | 3(4) | −8.132 | <0.001 | 5(3) | 5(2) | −4.947 | <0.001 |
| Gender | ||||||||||||
| Male | 10(4) | 10(3) | 4.391 | <0.001 | 2(3) | 3(4) | −5.784 | <0.001 | 5(3) | 5(2) | −1.814 | 0.070 |
| Female | 11(3) | 10(4) | 5.431 | <0.001 | 3(3) | 3(4) | −5.917 | <0.001 | 5(3) | 5(2) | −4.761 | <0.001 |
| p-group | 0.001 | <0.001 | 0.173 | 0.137 | 0.013 | 0.001 | ||||||
| Age | ||||||||||||
| ≤45 | 11(3) | 10(4) | 6.157 | <0.001 | 2(3) | 3(4) | −5.857 | <0.001 | 5(3) | 5(2) | −4.029 | <0.001 |
| >45 | 10(4) | 10(4) | 2.730 | 0.006 | 3(3) | 4(3) | −5.035 | <0.001 | 4(3) | 5(3) | −3.458 | <0.001 |
| P-group | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
| Education level | ||||||||||||
| Middle school and below | 8(4) | 9(5) | −2.003 | 0.045 | 2(3) | 3(3) | −5.746 | <0.001 | 4(3) | 5(3) | −2.779 | 0.005 |
| High school | 9(4) | 10(3) | −1.447 | 0.148 | 3(4) | 3(3) | −5.445 | <0.001 | 5(3) | 5(3) | −2.467 | 0.014 |
| College | 11(3) | 11(3) | 4.123 | <0.001 | 2(4) | 3(4) | −3.621 | <0.001 | 5(3) | 5(2) | −4.112 | <0.001 |
| Postgraduate | 12(2) | 11(3) | 2.906 | 0.004 | 3(3) | 3(3) | 0.285 | 0.776 | 5(3) | 5(2) | −1.247 | 0.212 |
| p-group | <0.001 | <0.001 | 0.028 | <0.001 | 0.072 | <0.001 | ||||||
| Region | ||||||||||||
| East | 11(3) | 10(4) | 6.890 | <0.001 | 3(4) | 4(3) | −6.342 | <0.001 | 5(3) | 5(2) | −2.891 | 0.004 |
| Middle | 10(4) | 10(4) | −1.379 | 0.168 | 2(3) | 3(4) | −3.195 | 0.001 | 5(3) | 5(3) | −1.820 | 0.069 |
| West | 11(4) | 10(3) | 5.263 | <0.001 | 2(3) | 3(4) | −4.055 | <0.001 | 5(3) | 5(2) | −2.729 | 0.006 |
| p-group | <0.001 | <0.001 | <0.001 | <0.001 | 0.535 | <0.001 | ||||||
| Answering time | ||||||||||||
| ≥1–2min | 11(4) | 11(3) | 5.383 | <0.001 | 2(3) | 3(4) | −2.192 | 0.0284 | 5(3) | 5(2) | −3.939 | <0.001 |
| ≥2–5 min | 10(4) | 10(4) | 2.681 | 0.007 | 3(4) | 3(3) | −7.134 | <0.001 | 5(3) | 5(3) | −3.853 | <0.001 |
| ≥5 min | 9(4) | 9(4) | 2.012 | 0.044 | 2(4) | 4(3) | −2.864 | 0.004 | 5(3) | 5(3) | −0.563 | 0.574 |
| p-group | <0.001 | <0.001 | 0.736 | <0.001 | 0.051 | <0.001 | ||||||
| Hypertension | ||||||||||||
| Yes | 10(4) | 10(4) | 2.007 | 0.045 | 2(3) | 3(3) | −4.445 | <0.001 | 5(2) | 5(3) | −2.049 | 0.041 |
| No | 11(3) | 10(4) | 6.519 | <0.001 | 3(3) | 3(4) | −6.989 | <0.001 | 5(3) | 5(2) | −4.398 | <0.001 |
| p-group | 0.019 | <0.001 | 0.468 | 0.002 | 0.011 | <0.001 | ||||||
| Salt-related taste | ||||||||||||
| Salty | 11(4) | 10(4) | 3.143 | 0.002 | 2(2) | 2(3) | −3.452 | <0.001 | 6(2) | 6(2) | −2.216 | 0.027 |
| Moderate | 11(3) | 10(4) | 4.120 | <0.001 | 2(3) | 3(3) | −6.826 | <0.001 | 5(3) | 5(2) | −4.160 | <0.001 |
| Bland | 11(3) | 10(4) | 5.048 | <0.001 | 4(3) | 4(4) | −3.520 | <0.001 | 4(2) | 4(2) | −3.530 | <0.001 |
| p-group | 0.011 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
| Willingness for salt reduction | ||||||||||||
| Yes | 11(3) | 10(4) | 7.009 | <0.001 | 3(4) | 3(3) | −7.276 | <0.001 | 5(3) | 5(2) | −5.208 | <0.001 |
| No | 9(4) | 9(5) | 1.929 | 0.054 | 1(1) | 1(1) | −1.422 | 0.155 | 5(3) | 6(3) | −0.897 | 0.370 |
| p-group | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Y.; Wang, J.; Ma, J.; Shi, W.; Wu, J. Comparison of Salt-Related Knowledge and Behaviors Status of WeChat Users between 2019 and 2020. Nutrients 2021, 13, 2141. https://doi.org/10.3390/nu13072141
Yang Y, Wang J, Ma J, Shi W, Wu J. Comparison of Salt-Related Knowledge and Behaviors Status of WeChat Users between 2019 and 2020. Nutrients. 2021; 13(7):2141. https://doi.org/10.3390/nu13072141
Chicago/Turabian StyleYang, Yibing, Jinglei Wang, Jixiang Ma, Wenhui Shi, and Jing Wu. 2021. "Comparison of Salt-Related Knowledge and Behaviors Status of WeChat Users between 2019 and 2020" Nutrients 13, no. 7: 2141. https://doi.org/10.3390/nu13072141
APA StyleYang, Y., Wang, J., Ma, J., Shi, W., & Wu, J. (2021). Comparison of Salt-Related Knowledge and Behaviors Status of WeChat Users between 2019 and 2020. Nutrients, 13(7), 2141. https://doi.org/10.3390/nu13072141





