Fluid Intake Monitoring Systems for the Elderly: A Review of the Literature
Abstract
1. Introduction
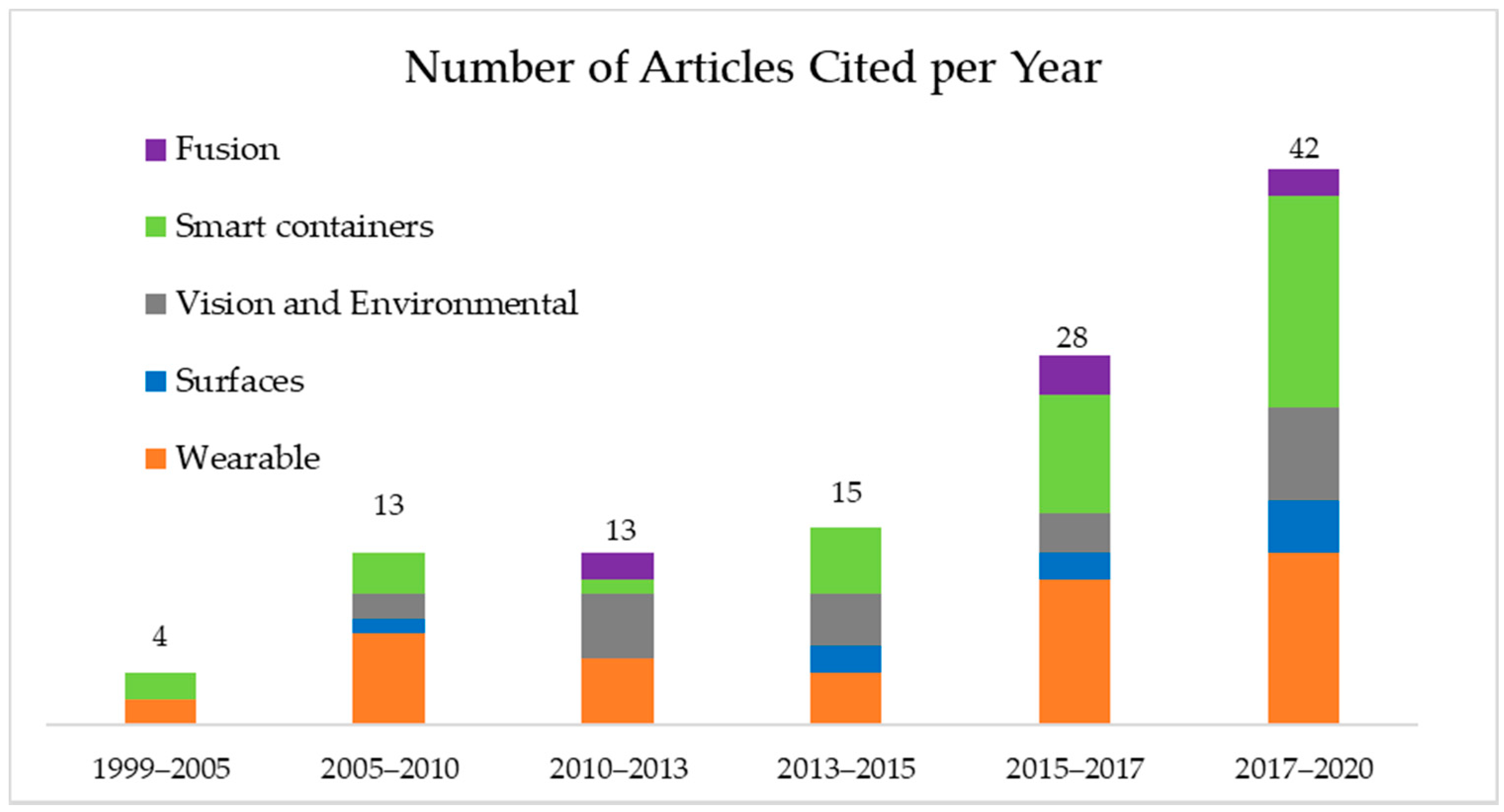
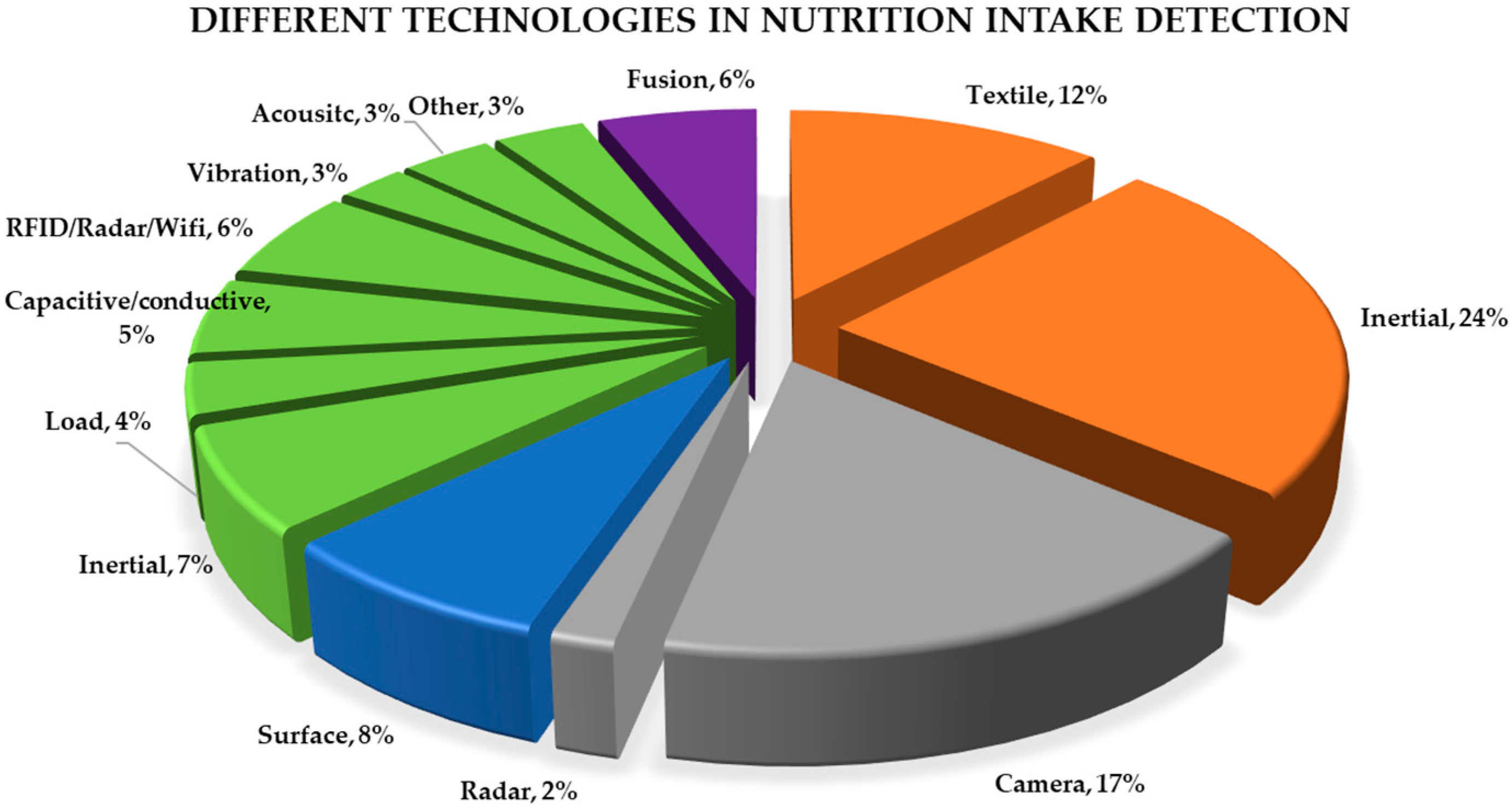
2. Methods
3. Wearable Technology
3.1. Intertial
3.2. Textile
Respiratory Inductance Plethysmography (RIP)
4. Surfaces
5. Vision- and Environmental-Based Methods
5.1. Cameras
5.2. Radar
6. Smart Containers
6.1. Inertial
6.2. Load and Pressure
6.3. Capacitance and Conductivity
6.4. RFID, Radar and Wi-Fi
6.5. Vibration
6.6. Acoustic
6.7. Other
6.8. Commercial
7. Fusion
8. Discussion and Overview
8.1. Wearables
8.2. Surfaces
8.3. Vision and Environmental Based
8.4. Smart Container
8.5. Fusion
8.6. Real-World Datasets
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- El-Sharkawy, A.M.; Sahota, O.; Maughan, R.J.; Lobo, D.N. The pathophysiology of fluid and electrolyte balance in the older adult surgical patient. Clin. Nutr. 2014, 33, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Jéquier, E.; Constant, F. Water as an essential nutrient: The physiological basis of hydration. Eur. J. Clin. Nutr. 2010, 64, 115–123. [Google Scholar] [CrossRef]
- Lavizzo-Mourey, R.J. Dehydration in the Elderly: A Short Review. J. Natl. Med. Assoc. 1987, 79, 1033–1038. [Google Scholar] [PubMed]
- Allison, S.P.; Lobo, D.N. Fluid and electrolytes in the elderly. Curr. Opin. Clin. Nutr. Metab. Care 2004, 7, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.A. Dehydration: Hazards and Benefits. Geriatr. Nurs. 2000, 21, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Phillips, P.A.; Rolls, B.J.; Ledingham, J.G.G.; Forsling, M.L.; Morton, J.J.; Crowe, M.J.; Wollner, L. Reduced Thirst after Water Deprivation in Healthy Elderly Men. N. Engl. J. Med. 1984, 311, 753–759. [Google Scholar] [CrossRef] [PubMed]
- Hooper, L.; Bunn, D. Detecting dehydration in older people: Useful tests. Nurs. Times 2015, 111, 12–16. [Google Scholar]
- Picetti, D.; Foster, S.; Pangle, A.K.; Schrader, A.; George, M.; Wei, J.Y.; Azhar, G. Hydration health literacy in the elderly. Nutr. Health Aging 2017, 4, 227–237. [Google Scholar] [CrossRef] [PubMed]
- Rowat, A.; Graham, C.; Dennis, M. Dehydration in Hospital-Admitted Stroke Patients. Stroke 2012, 43, 857–859. [Google Scholar] [CrossRef]
- Birgersson, A.-M.B.; Hammar, V.; Widerfors, G.; Hallberg, I.; Athlin, E. Elderly women’s feelings about being urinary incontinent, using napkins and being helped by nurses to change napkins. J. Clin. Nurs. 1993, 2, 165–171. [Google Scholar] [CrossRef]
- Zhang, J.; Goode, K.M.; Cuddihy, P.E.; Cleland, J.G.; on behalf of the TEN-HMS Investigators. Predicting hospitalization due to worsening heart failure using daily weight measurement: Analysis of the Trans-European Network-Home-Care Management System (TEN-HMS) study. Eur. J. Heart Fail. 2009, 11, 420–427. [Google Scholar] [CrossRef] [PubMed]
- Bernard, J.; Song, L.; Henderson, B.; Tasian, G.E. Association between Daily Water Intake and 24-hour Urine Volume Among Adolescents With Kidney Stones. Urology 2020, 140, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, L.E.; Maughan, R.J.; Senay, L.C.; Shirreffs, S.M. Limitations to the use of plasma osmolality as a hydration biomarker. Am. J. Clin. Nutr. 2013, 98, 503–504. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, L.E. Assessing Hydration Status: The Elusive Gold Standard. J. Am. Coll. Nutr. 2007, 26, 575S–584S. [Google Scholar] [CrossRef]
- Perrier, E.; Vergne, S.; Klein, A.; Poupin, M.; Rondeau, P.; Le Bellego, L.; Armstrong, L.E.; Lang, F.; Stookey, J.; Tack, I. Hydration biomarkers in free-living adults with different levels of habitual fluid consumption. Br. J. Nutr. 2012, 109, 1678–1687. [Google Scholar] [CrossRef] [PubMed]
- Garrett, D.C.; Rae, N.; Fletcher, J.R.; Zarnke, S.; Thorson, S.; Hogan, D.B.; Fear, E.C. Engineering Approaches to Assessing Hydration Status. IEEE Rev. Biomed. Eng. 2018, 11, 233–248. [Google Scholar] [CrossRef]
- Baron, S.; Courbebaisse, M.; Lepicard, E.M.; Friedlander, G. Assessment of hydration status in a large population. Br. J. Nutr. 2015, 113, 147–158. [Google Scholar] [CrossRef]
- Fortes, M.B.; Owen, J.; Raymond-Barker, P.; Bishop, C.; Elghenzai, S.; Oliver, S.J.; Walsh, N.P. Is This Elderly Patient Dehydrated? Diagnostic Accuracy of Hydration Assessment Using Physical Signs, Urine, and Saliva Markers. J. Am. Med. Dir. Assoc. 2015, 16, 221–228. [Google Scholar] [CrossRef]
- Bak, A.; Tsiami, A.; Greene, C. Methods of Assessment of Hydration Status and their Usefulness in Detecting Dehydration in the Elderly. Curr. Res. Nutr. Food Sci. J. 2017, 5, 43–54. [Google Scholar] [CrossRef]
- Hooper, L.; Bunn, D.K.; Abdelhamid, A.; Gillings, R.; Jennings, A.; Maas, K.; Millar, S.; Twomlow, E.; Hunter, P.R.; Shepstone, L.; et al. Water-loss (intracellular) dehydration assessed using urinary tests: How well do they work? Diagnostic accuracy in older people. Am. J. Clin. Nutr. 2016, 104, 121–131. [Google Scholar] [CrossRef]
- Paulis, S.J.C.; Everink, I.H.J.; Halfens, R.J.G.; Lohrmann, C.; Wirnsberger, R.R.; Gordon, A.L.; Schols, J.M.G.A. Diagnosing dehydration in the nursing home: International consensus based on a modified Delphi study. Eur. Geriatr. Med. 2020, 11, 393–402. [Google Scholar] [CrossRef]
- Bunn, D.K.; Hooper, L. Signs and Symptoms of Low-Intake Dehydration Do Not Work in Older Care Home Residents—DRIE Diagnostic Accuracy Study. J. Am. Med. Dir. Assoc. 2019, 20, 963–970. [Google Scholar] [CrossRef] [PubMed]
- Taylor, K.; Jones, E.B. Adult Dehydration. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Cheuvront, S.N.; Muñoz, C.X.; Kenefick, R.W. The void in using urine concentration to assess population fluid intake adequacy or hydration status. Am. J. Clin. Nutr. 2016, 104, 553–556. [Google Scholar] [CrossRef]
- Perrier, E.T.; Buendia-Jimenez, I.; Vecchio, M.; Armstrong, L.E.; Tack, I.; Klein, A. Twenty-Four-Hour Urine Osmolality as a Physiological Index of Adequate Water Intake. Dis. Markers 2015, 2015, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Cheuvront, S.N.; Ely, B.R.; Kenefick, R.W.; Sawka, M.N. Biological Variation and Diagnostic Accuracy of Dehydration Assessment Markers. Am. J. Clin. Nutr. 2010, 92, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, B.; Mentes, J.; Diggelmann, L.; Culp, K. Monitoring Hydration Status in Elderly Veterans. West. J. Nurs. Res. 2002, 24, 132–142. [Google Scholar] [CrossRef] [PubMed]
- Vivanti, A.; Harvey, K.; Ash, S. Developing a quick and practical screen to improve the identification of poor hydration in geriatric and rehabilitative care. Arch. Gerontol. Geriatr. 2010, 50, 156–164. [Google Scholar] [CrossRef]
- Rodrigues, S.; Silva, J.; Severo, M.; Inácio, C.; Padrão, P.; Lopes, C.; Carvalho, J.; Carmo, I.D.; Moreira, P. Validation Analysis of a Geriatric Dehydration Screening Tool in Community-Dwelling and Institutionalized Elderly People. Int. J. Environ. Res. Public Health 2015, 12, 2700–2717. [Google Scholar] [CrossRef] [PubMed]
- Hooper, L.; Abdelhamid, A.; Attreed, N.J.; Campbell, W.W.; Channell, A.M.; Chassagne, P.; Culp, K.R.; Fletcher, S.J.; Fortes, M.B.; Fuller, N.; et al. Clinical symptoms, signs and tests for identification of impending and current water-loss dehydration in older people. Cochrane Database Syst. Rev. 2015, 2015, CD009647. [Google Scholar] [CrossRef]
- Rösler, A.; Lehmann, F.; Krause, T.; Wirth, R.; von Renteln-Kruse, W. Nutritional and hydration status in elderly subjects: Clinical rating versus bioimpedance analysis. Arch. Gerontol. Geriatr. 2010, 50, e81–e85. [Google Scholar] [CrossRef]
- Liu, C.; Tsow, F.; Shao, D.; Yang, Y.; Iriya, R.; Tao, N. Skin Mechanical Properties and Hydration Measured with Mobile Phone Camera. IEEE Sens. J. 2016, 16, 924–930. [Google Scholar] [CrossRef]
- Cumming, K.; Hoyle, G.E.; Hutchison, J.D.; Soiza, R.L. Bioelectrical impedance analysis is more accurate than clinical examination in determining the volaemic status of elderly patients with fragility fracture and hyponatraemia. J. Nutr. Health Aging 2014, 18, 744–750. [Google Scholar] [CrossRef]
- Ferry, M. Strategies for Ensuring Good Hydration in the Elderly. Nutr. Rev. 2005, 63, S22–S29. [Google Scholar] [CrossRef] [PubMed]
- Tsiompanou, E.; Lucas, C.; Stroud, M. Overfeeding and overhydration in elderly medical patients: Lessons from the Liverpool Care Pathway. Clin. Med. 2013, 13, 248–251. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J. Overhydration—Hormonal and Metabolic Disorders. Available online: https://www.merckmanuals.com/home/hormonal-and-metabolic-disorders/water-balance/overhydration (accessed on 26 January 2021).
- Amft, O. Ambient, On-Body, and Implantable Monitoring Technologies to Assess Dietary Behavior. In Handbook of Behavior, Food and Nutrition; Springer: Berlin/Heidelberg, Germany, 2011; pp. 3507–3526. [Google Scholar]
- Kalantarian, H.; Alshurafa, N.; Sarrafzadeh, M. A Survey of Diet Monitoring Technology. IEEE Pervasive Comput. 2017, 16, 57–65. [Google Scholar] [CrossRef]
- Prioleau, T.; Moore, E.; Ghovanloo, M.; Ii, E.M. Unobtrusive and Wearable Systems for Automatic Dietary Monitoring. IEEE Trans. Biomed. Eng. 2017, 64, 2075–2089. [Google Scholar] [CrossRef] [PubMed]
- Vu, T.; Lin, F.; Alshurafa, N.; Xu, W. Wearable Food Intake Monitoring Technologies: A Comprehensive Review. Computers 2017, 6, 4. [Google Scholar] [CrossRef]
- Schiboni, G.; Amft, O. Automatic Dietary Monitoring Using Wearable Accessories. In Seamless Healthcare Monitoring: Advancements in Wearable, Attachable, and Invisible Devices; Tamura, T., Chen, W., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 369–412. ISBN 978-3-319-69362-0. [Google Scholar]
- Hassannejad, H.; Matrella, G.; Ciampolini, P.; De Munari, I.; Mordonini, M.; Cagnoni, S. Automatic diet monitoring: A review of computer vision and wearable sensor-based methods. Int. J. Food Sci. Nutr. 2017, 68, 656–670. [Google Scholar] [CrossRef]
- Stumbo, P.J. New technology in dietary assessment: A review of digital methods in improving food record accuracy. In Nutrition Society; Cambridge University Press (CUP): Cambridge, UK, 2013; Volume 72, pp. 70–76. [Google Scholar]
- Heydarian, H.; Adam, M.; Burrows, T.; Collins, C.; Rollo, M.E. Assessing Eating Behaviour Using Upper Limb Mounted Motion Sensors: A Systematic Review. Nutrients 2019, 11, 1168. [Google Scholar] [CrossRef]
- Amft, O.; Bannach, D.; Pirkl, G.; Kreil, M.; Lukowicz, P. Towards wearable sensing-based assessment of fluid intake. In Proceedings of the 2010 8th IEEE International Conference on Pervasive Computing and Communications Workshops (PERCOM Workshops), Mannheim, Germany, 29 March–2 April 2010; pp. 298–303. [Google Scholar]
- Wellnitz, A.; Wolff, J.-P.; Haubelt, C.; Kirste, T. Fluid intake recognition using inertial sensors. In Proceedings of the 6th International Workshop on Sensor-Based Activity Recognition and Interaction, Rostock, Germany, 16 September 2019; ACM: New York, NY, USA, 2019; pp. 1–7. [Google Scholar]
- Gomes, D.; Sousa, I. Real-Time Drink Trigger Detection in Free-living Conditions Using Inertial Sensors. Sensors 2019, 19, 2145. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Ang, J.M.H.; Xiao, W.; Tham, C.K. Detection of Activities by Wireless Sensors for Daily Life Surveillance: Eating and Drinking. Sensors 2009, 9, 1499–1517. [Google Scholar] [CrossRef]
- Fontana, J.M.; Farooq, M.; Sazonov, E. Automatic Ingestion Monitor: A Novel Wearable Device for Monitoring of Ingestive Behavior. IEEE Trans. Biomed. Eng. 2014, 61, 1772–1779. [Google Scholar] [CrossRef]
- Shen, Y.; Salley, J.; Muth, E.; Hoover, A. Assessing the Accuracy of a Wrist Motion Tracking Method for Counting Bites Across Demographic and Food Variables. IEEE J. Biomed. Health Inform. 2017, 21, 599–606. [Google Scholar] [CrossRef]
- Eskandari, S. Bite Detection and Differentiation Using Templates of Wrist Motion. Master’s Thesis, Clemson University, Clemson, SC, USA, 2013. [Google Scholar]
- Anderez, D.O.; Lotfi, A.; Langensiepen, C. A Hierarchical Approach in Food and Drink Intake Recognition Using Wearable Inertial Sensors. In Proceedings of the 11th PErvasive Technologies Related to Assistive Environments Conference, Corfu, Greece, 26–29 June 2018; ACM: New York, NY, USA, 2018; pp. 552–557. [Google Scholar]
- Lutze, R.; Baldauf, R.; Waldhör, K. Dehydration prevention and effective support for the elderly by the use of smartwatches. In Proceedings of the 2015 17th International Conference on E-health Networking, Application & Services (HealthCom), Boston, MA, USA, 14–17 October 2015; pp. 404–409. [Google Scholar]
- Anderez, D.O.; Lotfi, A.; Pourabdollah, A. Eating and drinking gesture spotting and recognition using a novel adaptive segmentation technique and a gesture discrepancy measure. Expert Syst. Appl. 2020, 140, 112888. [Google Scholar] [CrossRef]
- Krishnan, N.C.; Juillard, C.; Colbry, D.; Panchanathan, S. Recognition of hand movements using wearable accelerometers. J. Ambient. Intell. Smart Environ. 2009, 1, 143–155. [Google Scholar] [CrossRef]
- Schiboni, G.; Amft, O. Sparse natural gesture spotting in free living to monitor drinking with wrist-worn inertial sensors. In Proceedings of the 2018 ACM International Symposium on Wearable Computers, Singapour, 8–12 October 2018; ACM: New York, NY, USA, 2018; pp. 140–147. [Google Scholar]
- Weiss, G.; Timko, J.L.; Gallagher, C.M.; Yoneda, K.; Schreiber, A.J. Smartwatch-based activity recognition: A machine learning approach. In Proceedings of the 2016 IEEE-EMBS International Conference on Biomedical and Health Informatics (BHI), Las Vegas, NV, USA, 24–27 February 2016; pp. 426–429. [Google Scholar]
- Chen, L.-H.; Liu, K.-C.; Hsieh, C.-Y.; Chan, C.-T. Drinking gesture spotting and identification using single wrist-worn inertial sensor. In Proceedings of the 2017 International Conference on Applied System Innovation (ICASI), Sapporo, Japan, 13–17 May 2017; pp. 299–302. [Google Scholar]
- Hamatani, T.; Elhamshary, M.; Uchiyama, A.; Higashino, T. FluidMeter: Gauging the Human Daily Fluid Intake Using Smartwatches. Proc. ACM Interact. Mobile Wearable Ubiquitous Technol. 2018, 2, 1–25. [Google Scholar] [CrossRef]
- Huang, H.-Y.; Hsieh, C.-Y.; Liu, K.-C.; Hsu, S.J.-P.; Chan, C.-T. Fluid Intake Monitoring System Using a Wearable Inertial Sensor for Fluid Intake Management. Sensors 2020, 20, 6682. [Google Scholar] [CrossRef] [PubMed]
- Moschetti, A.; Fiorini, L.; Esposito, D.; Dario, P.; Cavallo, F. Recognition of Daily Gestures with Wearable Inertial Rings and Bracelets. Sensors 2016, 16, 1341. [Google Scholar] [CrossRef]
- Dong, B.; Biswas, S. Meal-time and duration monitoring using wearable sensors. Biomed. Signal Process. Control. 2017, 32, 97–109. [Google Scholar] [CrossRef]
- Anderez, D.O.; Lotfi, A.; Pourabdollah, A. Temporal convolution neural network for food and drink intake recognition. In Proceedings of the 12th ACM International Conference on Pervasive Technologies Related to Assistive Environments, Rhodes, Greece, 5–7 June 2019; ACM: New York, NY, USA, 2019; pp. 580–586. [Google Scholar]
- Anderez, D.O.; Lotfi, A.; Pourabdollah, A. A deep learning based wearable system for food and drink intake recognition. J. Ambient. Intell. Humaniz. Comput. 2020, 1–13. [Google Scholar] [CrossRef]
- Chun, K.S.; Sanders, A.B.; Adaimi, R.; Streeper, N.; Conroy, D.E.; Thomaz, E. Towards a generalizable method for detecting fluid intake with wrist-mounted sensors and adaptive segmentation. In Proceedings of the 24th International Conference on Intelligent User Interfaces, Marina del Ray, CA, USA, 17–20 March 2019; ACM: New York, NY, USA, 2019; pp. 80–85. [Google Scholar] [CrossRef]
- Flutura, S.; Seiderer, A.; Aslan, I.; Dang, C.T.; Schwarz, R.; Schiller, D.; André, E. DrinkWatch: A Mobile Wellbeing Application Based on Interactive and Cooperative Machine Learning. In Proceedings of the 2018 International Conference on Digital Health, Lyon, France, 23–26 April 2018; ACM: New York, NY, USA, 2018. [Google Scholar] [CrossRef]
- Gomes, D.; Mendes-Moreira, J.; Sousa, I.; Silva, J. Eating and Drinking Recognition in Free-Living Conditions for Triggering Smart Reminders. Sensors 2019, 19, 2803. [Google Scholar] [CrossRef]
- Amft, O.; Junker, H.; Tröster, G. Detection of eating and drinking arm gestures using inertial body-worn sensors. In Proceedings of the Ninth IEEE International Symposium on Wearable Computers (ISWC’05), Osaka, Japan, 18–21 October 2005; pp. 160–163. [Google Scholar]
- Junker, H.; Amft, O.; Lukowicz, P.; Tröster, G. Gesture spotting with body-worn inertial sensors to detect user activities. Pattern Recognit. 2008, 41, 2010–2024. [Google Scholar] [CrossRef]
- Ordóñez, F.J.; Roggen, D. Deep Convolutional and LSTM Recurrent Neural Networks for Multimodal Wearable Activity Recognition. Sensors 2016, 16, 115. [Google Scholar] [CrossRef] [PubMed]
- Merck, C.; Maher, C.; Mirtchouk, M.; Zheng, M.; Huang, Y.; Kleinberg, S. Multimodality Sensing for Eating Recognition. In Proceedings of the 10th EAI International Conference on Pervasive Computing Technologies for Healthcare, Cancun, Mexico, 16–19 May 2016; ICST (Institute for Computer Sciences, Social-Informatics and Telecommunications Engineering): Brussels, Belgium, 2016; pp. 130–137. [Google Scholar]
- Mirtchouk, M.; Merck, C.; Kleinberg, S. Automated Estimation of Food Type and Amount Consumed from Body-Worn Audio and Motion Sensors. In Proceedings of the 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing, Heidelberg, Germany, 12–16 September 2016; Association for Computing Machinery: New York, NY, USA, 2016; pp. 451–462. [Google Scholar]
- Mirtchouk, M.; Lustig, D.; Smith, A.; Ching, I.; Zheng, M.; Kleinberg, S. Recognizing Eating from Body-Worn Sensors: Combining Free-Living and Laboratory Data. Proc. ACM Interact. Mobile Wearable Ubiquitous Technol. 2017, 1, 85:1–85:20. [Google Scholar] [CrossRef]
- Cheng, J.; Amft, O.; Lukowicz, P. Active Capacitive Sensing: Exploring a New Wearable Sensing Modality for Activity Recognition. In Proceedings of the International Conference on Pervasive Computing, Helsinki, Finland, 17–20 May 2010; Springer: Berlin/Heidelberg, Germany, 2010; pp. 319–336. [Google Scholar]
- Cheng, J.; Zhou, B.; Kunze, K.; Rheinländer, C.C.; Wille, S.; Wehn, N.; Weppner, J.; Lukowicz, P. Activity recognition and nutrition monitoring in every day situations with a textile capacitive neckband. In Proceedings of the 2013 ACM Conference on Pervasive and Ubiquitous Computing Adjunct Publication, Zurich, Switzerland, 8–12 September 2013; ACM: New York, NY, USA, 2013; pp. 155–158. [Google Scholar]
- Zhang, R.; Freund, M.; Amft, O.; Cheng, J.; Zhou, B.; Lukowicz, P.; Fernando, S.; Chabrecek, P. A generic sensor fabric for multi-modal swallowing sensing in regular upper-body shirts. In Proceedings of the 2016 ACM International Symposium on New Ideas, New Paradigms, and Reflections on Programming and Software, Amsterdam, The Netherlands, 2–4 November 2016; ACM: New York, NY, USA, 2016; pp. 46–47. [Google Scholar]
- Amft, O.; Troster, G. Methods for Detection and Classification of Normal Swallowing from Muscle Activation and Sound. In Proceedings of the 2006 Pervasive Health Conference and Workshops, Innsbruck, Austria, 29 November–1 December 2006; pp. 1–10. [Google Scholar]
- Amft, O.; Tröster, G. Recognition of dietary activity events using on-body sensors. Artif. Intell. Med. 2008, 42, 121–136. [Google Scholar] [CrossRef] [PubMed]
- Farooq, M.; Fontana, J.M.; Sazonov, E. A novel approach for food intake detection using electroglottography. Physiol. Meas. 2014, 35, 739–751. [Google Scholar] [CrossRef] [PubMed]
- Moreau–Gaudry, A.; Sabil, A.; Benchetrit, G.; Franco, A. Use of Respiratory Inductance Plethysmography for the Detection of Swallowing in the Elderly. Dysphagia 2005, 20, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Dong, B.; Biswas, S. Swallow monitoring through apnea detection in breathing signal. In Proceedings of the 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 28 August–1 September 2012; Volume 2012, pp. 6341–6344. [Google Scholar]
- Dong, B.; Biswas, S. Liquid Intake Monitoring through Breathing Signal Using Machine Learning. In Proceedings of the Sensing Technologies for Global Health, Military Medicine, and Environmental Monitoring III, Baltimore, Baltimore, MD, USA, 29 April–1 May 2013; International Society for Optics and Photonics: Bellingham, WA, USA, 2013; Volume 8723, p. 872315. [Google Scholar]
- Dong, B.; Biswas, S. Wearable Diet Monitoring through Breathing Signal Analysis. In Proceedings of the 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Osaka, Japan, 3–7 July 2013; pp. 1186–1189. [Google Scholar]
- Dong, B.; Biswas, S. Wearable sensing for liquid intake monitoring via apnea detection in breathing signals. Biomed. Eng. Lett. 2014, 4, 378–387. [Google Scholar] [CrossRef]
- Dong, B.; Biswas, S. Analyzing Breathing Signals and Swallow Sequence Locality for Solid Food Intake Monitoring. J. Med. Biol. Eng. 2016, 36, 765–775. [Google Scholar] [CrossRef]
- Tatulli, E.; Fontecave-Jallon, J.; Calabrese, P.; Gumery, P.-Y. Respiratory Inductance Plethysmography for Automated Swallowing Detection. Int. J. E-Health Med. Commun. 2020, 11, 64–77. [Google Scholar] [CrossRef]
- Chang, K.; Liu, S.; Chu, H.; Hsu, J.Y.; Chen, C.; Lin, T.; Chen, C.; Huang, P. The Diet-Aware Dining Table: Observing Dietary Behaviors over a Tabletop Surface. In Pervasive Computing; Fishkin, K.P., Schiele, B., Nixon, P., Quigley, A., Eds.; Springer: Berlin/Heidelberg, Germany, 2006; pp. 366–382. [Google Scholar]
- Zhou, B.; Cheng, J.; Sundholm, M.; Lukowicz, P. From Smart Clothing to Smart Table Cloth: Design and Implementation of a Large Scale, Textile Pressure Matrix Sensor. Trans. Petri Nets Other Mod. Concurr. XV 2014, 8350, 159–170. [Google Scholar] [CrossRef]
- Zhou, B.; Cheng, J.; Sundholm, M.; Reiss, A.; Huang, W.; Amft, O.; Lukowicz, P. Smart table surface: A novel approach to pervasive dining monitoring. In Proceedings of the 2015 IEEE International Conference on Pervasive Computing and Communications (PerCom), St. Louis, MO, USA, 23–27 March 2015; pp. 155–162. [Google Scholar]
- Haarman, J.A.M.; De Vries, R.A.J.; Harmsen, E.C.; Hermens, H.J.; Heylen, D.K.J. Sensory Interactive Table (SIT)—Development of a Measurement Instrument to Support Healthy Eating in a Social Dining Setting. Sensors 2020, 20, 2636. [Google Scholar] [CrossRef]
- Mattfeld, R.S.; Muth, E.R.; Hoover, A.W. Measuring the Consumption of Individual Solid and Liquid Bites Using a Table-Embedded Scale During Unrestricted Eating. IEEE J. Biomed. Health Inform. 2017, 21, 1711–1718. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, T.; Shimokakimoto, T.; Jayatilake, D.; Inoue, M.; Suzuki, K. A portable sensor sheet for measuring the eating pace in meal assistance care. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 4297–4300. [Google Scholar]
- Lessel, P.; Altmeyer, M.; Kerber, F.; Barz, M.; Leidinger, C.; Krüger, A. WaterCoaster: A Device to Encourage People in a Playful Fashion to Reach Their Daily Water Intake Level. In Proceedings of the 2016 CHI Conference Extended Abstracts on Human Factors in Computing Systems—CHI EA ’16, San Jose, CA, USA, 7–12 May 2016; ACM Press: New York, NY, USA, 2016; pp. 1813–1820. [Google Scholar]
- Chan, A.; Scaer, R. Hydration Tracking Coaster with BLE Android App; Major Qualifying Projects (All Years); Worcester Polytechnic Institute: Worcester, MA, USA, 2018. [Google Scholar]
- Plecher, D.A.; Eichhorn, C.; Lurz, M.; Leipold, N.; Böhm, M.; Krcmar, H.; Ott, A.; Volkert, D.; Klinker, G. Interactive Drinking Gadget for the Elderly and Alzheimer Patients. In Human Aspects of IT for the Aged Population. Social Media, Games and Assistive Environments; Zhou, J., Salvendy, G., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 444–463. [Google Scholar]
- Chua, J.-L.; Chang, Y.C.; Jaward, M.H.; Parkkinen, J.; Wong, K.-S. Vision-based hand grasping posture recognition in drinking activity. In Proceedings of the 2014 International Symposium on Intelligent Signal Processing and Communication Systems (ISPACS), Kuching, Malaysia, 1–4 December 2014; pp. 185–190. [Google Scholar]
- Tham, J.S.; Chang, Y.C.; Fauzi, M.F.A. Automatic identification of drinking activities at home using depth data from RGB-D camera. In Proceedings of the 2014 International Conference on Control, Automation and Information Sciences (ICCAIS 2014), Gwangju, Korea, 2–5 December 2014; pp. 153–158. [Google Scholar]
- Kassim, M.F.; Mohd, M.N.H.; Tomari, M.R.M.; Suriani, N.S.; Zakaria, W.N.W.; Sari, S. A non-invasive and non-wearable food intake monitoring system based on depth sensor. Bull. Electr. Eng. Inform. 2020, 9, 2342–2349. [Google Scholar] [CrossRef]
- Cunha, A.; Pádua, L.; Costa, L.; Trigueiros, P. Evaluation of MS Kinect for Elderly Meal Intake Monitoring. Procedia Technol. 2014, 16, 1383–1390. [Google Scholar] [CrossRef]
- Burgess, R.A.; Hartley, T.; Mehdi, Q.; Mehdi, R. Monitoring of patient fluid intake using the Xbox Kinect. In Proceedings of the CGAMES’2013, Louisville, KY, USA, 30 July–1 August 2013; pp. 60–64. [Google Scholar]
- Cippitelli, E.; Gasparrini, S.; Gambi, E.; Spinsante, S. Unobtrusive intake actions monitoring through RGB and depth information fusion. In Proceedings of the 2016 IEEE 12th International Conference on Intelligent Computer Communication and Processing (ICCP), Cluj-Napoca, Romania, 8–10 September 2016; pp. 19–26. [Google Scholar]
- Iosifidis, A.; Marami, E.; Tefas, A.; Pitas, I. Eating and drinking activity recognition based on discriminant analysis of fuzzy distances and activity volumes. In Proceedings of the 2012 IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP), Kyoto, Japan, 25–30 March 2012; pp. 2201–2204. [Google Scholar]
- Cebanov, E.; Dobre, C.; Gradinaru, A.; Ciobanu, R.-I.; Stanciu, V.-D. Activity Recognition for Ambient Assisted Living Using Off-the-shelf Motion Sensing Input Devices. In Proceedings of the 2019 Global IoT Summit (GIoTS), Aarhus, Denmark, 17–21 June 2019. [Google Scholar]
- Chang, M.-J.; Hsieh, J.-T.; Fang, C.-Y.; Chen, S.-W. A Vision-Based Human Action Recognition System for Moving Cameras Through Deep Learning. In Proceedings of the 2019 2nd International Conference on Signal Processing and Machine Learning, Hangzhou, China, 27–29 November 2019; Association for Computing Machinery: New York, NY, USA, 2019; pp. 85–91. [Google Scholar]
- Brena, R.F.; Nava, A. Activity Recognition in Meetings with One and Two Kinect Sensors. In Proceedings of the Mexican Conference on Pattern Recognition, Guanajuato, Mexico, 22–25 June 2016; Springer: Berlin/Heidelberg, Germany, 2016; pp. 219–228. [Google Scholar]
- O’Loughlin, G.; Cullen, S.J.; McGoldrick, A.; O’Connor, S.; Blain, R.; O’Malley, S.; Warrington, G.D. Using a Wearable Camera to Increase the Accuracy of Dietary Analysis. Am. J. Prev. Med. 2013, 44, 297–301. [Google Scholar] [CrossRef]
- Gemming, L.; Doherty, A.; Utter, J.; Shields, E.; Ni Mhurchu, C. The use of a wearable camera to capture and categorise the environmental and social context of self-identified eating episodes. Appetite 2015, 92, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Davies, A.; Chan, V.; Bauman, A.; Signal, L.; Hosking, C.; Gemming, L.; Allman-Farinelli, M. Using wearable cameras to monitor eating and drinking behaviours during transport journeys. Eur. J. Nutr. 2021, 60, 1875–1885. [Google Scholar] [CrossRef] [PubMed]
- Doulah, A.B.M.S.U. A Wearable Sensor System for Automatic Food Intake Detection and Energy Intake Estimation in Humans. Ph.D. Thesis, University of Alabama Libraries, Tuscaloosa, AL, USA, 2018. [Google Scholar]
- Raju, V.; Sazonov, E. Processing of Egocentric Camera Images from a Wearable Food Intake Sensor. In Proceedings of the 2019 SoutheastCon, Huntsville, AL, USA, 11–14 April 2019; pp. 1–6. [Google Scholar]
- Zhu, F.; Bosch, M.; Boushey, C.J.; Delp, E.J. An image analysis system for dietary assessment and evaluation. In Proceedings of the 2010 IEEE International Conference on Image Processing, Hong Kong, China, 26–29 September 2010; pp. 1853–1856. [Google Scholar] [CrossRef]
- Zhu, F.; Bosch, M.; Khanna, N.; Boushey, C.J.; Delp, E. Multilevel Segmentation for Food Classification in Dietary Assessment. In Proceedings of the 2011 7th International Symposium on Image and Signal Processing and Analysis (ISPA), Dubrovnik, Croatia, 4–6 September 2011; pp. 337–342. [Google Scholar]
- Puri, M.; Zhu, Z.; Yu, Q.; Divakaran, A.; Sawhney, H.S. Recognition and volume estimation of food intake using a mobile device. In Proceedings of the 2009 Workshop on Applications of Computer Vision (WACV), Snowbird, UT, USA, 7–8 December 2009; pp. 1–8. [Google Scholar]
- Kong, F.; Tan, J. DietCam: Automatic dietary assessment with mobile camera phones. Pervasive Mob. Comput. 2012, 8, 147–163. [Google Scholar] [CrossRef]
- Hafiz, R.; Islam, S.; Khanom, R.; Uddin, M.S. Image based drinks identification for dietary assessment. In Proceedings of the 2016 International Workshop on Computational Intelligence (IWCI), Dhaka, Bangladesh, 12–13 December 2016; pp. 192–197. [Google Scholar] [CrossRef]
- Shah, S.A.; Fioranelli, F. Human Activity Recognition: Preliminary Results for Dataset Portability using FMCW Radar. In Proceedings of the 2019 International Radar Conference (RADAR), Toulon, France, 23–27 September 2019; pp. 1–4. [Google Scholar]
- Kreutzer, J.F.; Ramesberger, S.; Reimer, S.M.F.; Entsfellner, K.; Lueth, T.C. Automatically detecting fluid intake using conductivity measurements of beverages in a cup. In Proceedings of the 2015 IEEE International Conference on Automation Science and Engineering (CASE), Gothenburg, Sweden, 24–28 August 2015; pp. 1546–1551. [Google Scholar]
- Gellersen, H.-W.; Beigl, M.; Krull, H. The MediaCup: Awareness Technology Embedded in an Everyday Object. In Transactions on Petri Nets and Other Models of Concurrency XV; Springer: Berlin/Heidelberg, Germany, 1999; pp. 308–310. [Google Scholar]
- Liu, K.-C.; Hsieh, C.-Y.; Huang, H.-Y.; Chiu, L.-T.; Hsu, S.J.-P.; Chan, C.-T. Drinking Event Detection and Episode Identification Using 3D-Printed Smart Cup. IEEE Sens. J. 2020, 20, 13743–13751. [Google Scholar] [CrossRef]
- Dong, B.; Gallant, R.; Biswas, S. A self-monitoring water bottle for tracking liquid intake. In Proceedings of the 2014 IEEE Healthcare Innovation Conference (HIC), Seattle, WA, USA, 8–10 October 2014; pp. 311–314. [Google Scholar]
- Griffith, H.; Shi, Y.; Biswas, S. A Container-Attachable Inertial Sensor for Real-Time Hydration Tracking. Sensors 2019, 19, 4008. [Google Scholar] [CrossRef]
- Griffith, H.; Biswas, S. Towards Improved Drink Volume Estimation Using Filter-Based Feature Selection. In Proceedings of the Advances in Information and Communication, San Francisco, CA, USA, 14–15 March 2019; Arai, K., Bhatia, R., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 280–290. [Google Scholar]
- Griffith, H.; Shi, Y.; Biswas, S. Verification of IMU-Based Inclination Estimates Using Video Motion Capture. In Proceedings of the 2019 IEEE International Conference on Consumer Electronics (ICCE), Las Vegas, NV, USA, 11–13 January 2019; pp. 1–4. [Google Scholar]
- Griffith, H.; Shi, Y.; Biswas, S. A Dynamic Partitioning Algorithm for Sip Detection using a Bottle-Attachable IMU Sensor. Int. J. Adv. Comput. Sci. Appl. 2019, 10. [Google Scholar] [CrossRef]
- Zimmermann, C.; Zeilfelder, J.; Bloecher, T.; Diehl, M.; Essig, S.; Stork, W. Evaluation of a smart drink monitoring device. In Proceedings of the 2017 IEEE Sensors Applications Symposium (SAS), Glassboro, NJ, USA, 13–15 March 2017; pp. 1–5. [Google Scholar]
- Kreutzer, J.F.; Flaschberger, J.; Hein, C.M.; Lueth, T.C. Capacitive detection of filling levels in a cup. In Proceedings of the 2016 IEEE 13th International Conference on Wearable and Implantable Body Sensor Networks (BSN), San Francisco, CA, USA, 14–17 June 2016; pp. 31–36. [Google Scholar]
- Bobin, M.; Amroun, H.; Boukalle, M.; Anastassova, M.; Ammi, M. Smart Cup to Monitor Stroke Patients Activities During Everyday Life. In Proceedings of the 2018 IEEE International Conference on Internet of Things (iThings) and IEEE Green Computing and Communications (GreenCom) and IEEE Cyber, Physical and Social Computing (CPSCom) and IEEE Smart Data (SmartData), Halifax, NS, Canada, 30 July–3 August 2018; pp. 189–195. [Google Scholar]
- Gao, C.; Li, Y.; Zhang, X. LiveTag: Sensing Human-Object Interaction Through Passive Chipless Wi-Fi Tags. GetMobile Mob. Comput. Commun. 2019, 22, 32–35. [Google Scholar] [CrossRef]
- Ren, Y.; Tan, S.; Zhang, L.; Wang, Z.; Yang, J. Liquid Level Sensing Using Commodity WiFi in a Smart Home Environment. Proc. Interact. Mobile Wearable Ubiquitous Technol. Arch. 2020. [Google Scholar] [CrossRef]
- Fan, M.; Truong, K.N. SoQr: Sonically Quantifying the Content Level inside Containers. In Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing—UbiComp ’15, Osaka, Japan, 7–11 September 2015; ACM Press: New York, NY, USA, 2015; pp. 3–14. [Google Scholar]
- Akbar, A.F.; Oktivasari, P. Smart bottle work design using waterflow sensor based on Raspberry Pi and Android. J. Phys. Conf. Ser. 2019, 1193, 012007. [Google Scholar] [CrossRef]
- H2Opal Specs. Available online: https://www.h2opal.com/pages/specs (accessed on 21 September 2020).
- Soubam, S.; Agrawal, M.; Naik, V. Using an Arduino and a smartwatch to measure liquid consumed from any container. In Proceedings of the 2017 9th International Conference on Communication Systems and Networks (COMSNETS), Bengaluru, India, 4–8 January 2017; pp. 464–467. [Google Scholar]
- Chiu, M.-C.; Chang, S.; Chang, Y.; Chu, H.-H.; Chen, C.; Hsiao, F.; Ko, J.-C. Playful Bottle: A Mobile Social Persuasion System to Motivate Healthy Water Intake. UbiComp 2009. [Google Scholar] [CrossRef]
- Wang, S.-W.; Chen, C.-C.; Wu, C.-M.; Huang, C.-M. A continuous water-level sensor based on load cell and floating pipe. In Proceedings of the 2018 IEEE International Conference on Applied System Invention (ICASI), Chiba, Japan, 13–17 April 2018; pp. 151–154. [Google Scholar]
- Dietz, P.H.; Leigh, D.; Yerazunis, W.S. Wireless liquid level sensing for restaurant applications. In Proceedings of the Sensors, 2002 IEEE, Orlando, FL, USA, 12–14 June 2002; Volume 1, pp. 715–720. [Google Scholar]
- Rimo, G.; Rani, S.S.; Ramyarani, N.; Pavithra, C. Non-Contact Continuous Capacitive Liquid Level Sensing. Int. J. Pure Appl. Math. 2018, 119, 1921–1929. [Google Scholar]
- Fan, M.; Truong, K.N.; Ranjan, A. Exploring the Use of Capacitive Sensing to Externally Measure Liquid in Fluid Containers. 2016. Available online: http://hdl.handle.net/1807/70970 (accessed on 18 June 2021).
- Kreutzer, J.F.; Schmid, R.; Reimer, S.M.F.; Lueth, T.C.; D’Angelo, L.T. Radio frequency identification based detection of filling levels for automated monitoring of fluid intake. In Proceedings of the 2014 IEEE International Conference on Robotics and Biomimetics (ROBIO 2014), Bali, Indonesia, 5–10 December 2014; pp. 2049–2054. [Google Scholar]
- Jayatilaka, A.; Ranasinghe, D.C. Real-time fluid intake gesture recognition based on batteryless UHF RFID technology. Pervasive Mob. Comput. 2017, 34, 146–156. [Google Scholar] [CrossRef]
- Jayatilaka, A.; Ranasinghe, D.C. Towards unobtrusive real-time fluid intake monitoring using passive UHF RFID. In Proceedings of the 2016 IEEE International Conference on RFID (RFID), Orlando, FL, USA, 3–5 May 2016; pp. 1–4. [Google Scholar]
- Bhattacharyya, R.; Floerkemeier, C.; Sarma, S.E. RFID tag antenna based sensing: Does your beverage glass need a refill? In Proceedings of the 2010 IEEE International Conference on RFID (IEEE RFID 2010), Orlando, FL, USA, 14–16 April 2010; pp. 126–133. [Google Scholar]
- Wang, J.; Xiong, J.; Chen, X.; Jiang, H.; Balan, R.K.; Fang, D. TagScan: Simultaneous Target Imaging and Material Identification with Commodity RFID Devices. In Proceedings of the 23rd Annual International Conference on Mobile Computing and Networking, Snowbird, UT, USA, 16–20 October 2017; ACM: New York, NY, USA, 2017; pp. 288–300. [Google Scholar]
- Nakagawa, T.; Hyodo, A.; Kogo, K.; Kurata, H.; Osada, K.; Oho, S. Contactless Liquid-Level Measurement with Frequency-Modulated Millimeter Wave Through Opaque Container. IEEE Sens. J. 2013, 13, 926–933. [Google Scholar] [CrossRef]
- Ryu, J.; Jeong, H.; Chen, Y.; Oh, C.; Kim, J.; Kim, H.; Cho, S.; No, K.; Park, Y.-H.; Park, S.; et al. Flexible piezoelectric liquid volume sensor. Sens. Actuators A Phys. 2018, 276, 219–225. [Google Scholar] [CrossRef]
- Tommy, R.; Raja, V.V.; Krishna, A.S. Interactive Water Bottle Application on a Smart Phone to Enhance User Water Consumption. In Proceedings of the 2017 International Conference on Current Trends in Computer, Electrical, Electronics and Communication (CTCEEC), Mysore, India, 8–9 September 2017; pp. 1072–1073. [Google Scholar]
- Vithanage, J.; de Silva, R.; Karunaratne, K.; Silva, M.D.; Bogoda, P.; Kankanamge, R.; Kehelella, P.; Jayakody, K.D.; Wijekoon, J.L. SmartOne: IoT-Based Smart Platform to Manage Personal Water Usage. In Proceedings of the 2019 International Conference on Advancements in Computing (ICAC), Malabe, Sri Lanka, 5–7 December 2019; pp. 398–403. [Google Scholar]
- Wijanarko, A.E.; Abdurohman, M.; Putrada, A.G. A Fuzzy Logic Based Internet of Things (IoT) for Smart Water Bottle. In Proceedings of the 2019 5th International Conference on Computing Engineering and Design (ICCED), Singapore, 11–13 April 2019; pp. 1–6. [Google Scholar]
- Pankajavalli, P.; Saikumar, R.; Maheswaran, R. Hydration reminding smart bottle: IoT experimentation. In Proceedings of the 2017 Innovations in Power and Advanced Computing Technologies (i-PACT), Vellore, India, 21–22 April 2017. [Google Scholar] [CrossRef]
- Ayoola, I.B.I.; Ansems, K.E.; Chen, W.; Feijs, L.M.G. Design of a Smart Cup—A Tele-medical System for Behavioral Intervention through Interactive Materiality. In Proceedings of the VI Latin American Congress on Biomedical Engineering CLAIB 2014, Paraná, Argentina, 29–31 October 2014; pp. 96–99. [Google Scholar]
- Lester, J.; Tan, D.; Patel, S.; Brush, A.B. Automatic classification of daily fluid intake. In Proceedings of the 4th International ICST Conference on Pervasive Computing Technologies for Healthcare, Munich, Germany, 22–25 March 2010; pp. 1–8. [Google Scholar]
- Borofsky, M.S.; Dauw, C.A.; York, N.; Terry, C.; Lingeman, J.E. Accuracy of daily fluid intake measurements using a “smart” water bottle. Urolithiasis 2017, 46, 343–348. [Google Scholar] [CrossRef] [PubMed]
- HidrateSpark 3 Smart Water Bottle & Free Hydration Tracker App—Black. Available online: https://hidratespark.com/products/black-hidrate-spark-3 (accessed on 21 April 2021).
- HidrateSpark Inc. Smart Water Bottle—HidrateSpark Bluetooth Water Bottle + Tracker App. Available online: https://hidratespark.com/ (accessed on 9 November 2020).
- Thermos® Connected Hydration Bottle with Smart Lid. Available online: https://www.thermos.com/smartlid (accessed on 9 November 2020).
- Ozmo Smart Cup: Water Hydration & Coffee Enjoyment. Available online: https://www.kickstarter.com/projects/ozmo/ozmo-smart-cup-water-hydration-and-coffee-enjoymen (accessed on 9 November 2020).
- Ozmo Java+ Smart Coffee Mug. Available online: https://www.touchofmodern.com/sales/ozmo/ozmo-java-smart-coffee-mug (accessed on 9 November 2020).
- DrinKup Smart Water Bottle Review—The Gadgeteer. Available online: https://the-gadgeteer.com/2018/05/02/drinkup-smart-water-bottle-review/ (accessed on 18 June 2021).
- HydraCoach Fitness Intellingent Water Bottle. Available online: https://www.gadgetreview.com/hydracoach-fitness-intellingent-water-bottle (accessed on 21 April 2021).
- Droplet Hydration Aid|Memory Aid for Dehydration. Available online: https://www.droplet-hydration.com/introducing-droplet-hydration/ (accessed on 21 April 2021).
- Hondori, H.M.; Khademi, M.; Lopes, C.V. Monitoring Intake Gestures Using Sensor Fusion (Microsoft Kinect and Inertial Sensors) for Smart Home Tele-Rehab Setting. In Proceedings of the 2012 1st Annual IEEE Healthcare Innovation Conference, Houston, TX, USA, 7–9 November 2012. [Google Scholar]
- Troost, P.S. Vision and On-Body Sensor Fusion for Monitoring Food Intake Behaviour in a Restaurant Environment. Master’s Thesis, Technische Universiteit Eindhoven, Eindhoven, The Netherlands, 2013. [Google Scholar]
- Seiderer, A.; Flutura, S.; André, E. Development of a mobile multi-device nutrition logger. In Proceedings of the 2nd ACM SIGCHI International Workshop on Multisensory Approaches to Human-Food Interaction, Glasgow, UK, 13 November 2017; ACM: New York, NY, USA, 2017; pp. 5–12. [Google Scholar]
- Jovanov, E.; Nallathimmareddygari, V.R.; Pryor, J.E. SmartStuff: A Case Study of a Smart Water Bottle. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Orlando, FL, USA, 16–20 August 2016; pp. 6307–6310. [Google Scholar] [CrossRef]
- Garcia-Constantino, M.; Konios, A.; Mustafa, M.A.; Nugent, C.; Morrison, G. Ambient and Wearable Sensor Fusion for Abnormal Behaviour Detection in Activities of Daily Living. In Proceedings of the 2020 IEEE International Conference on Pervasive Computing and Communications Workshops (PerCom Workshops), Austin, TX, USA, 23–27 March 2020; pp. 1–6. [Google Scholar]
- Du, B.; Lu, C.X.; Kan, X.; Wu, K.; Luo, M.; Hou, J.; Li, K.; Kanhere, S.; Shen, Y.; Wen, H. HydraDoctor: Real-Time Liquids Intake Monitoring by Collaborative Sensing. In Proceedings of the 20th International Conference on Distributed Computing and Networking, Bangalore, India, 4–7 January 2019; ACM: New York, NY, USA, 2019; pp. 213–217. [Google Scholar]


| Ref. | #Sen. | Method | #Sub | System Accuracy (%) | Drinking Detection Accuracy (%) | System F1-Score (%) | Drinking Detection F1-Score (%) | Null Class |
|---|---|---|---|---|---|---|---|---|
| [46] | 2 | Binary CNN 1 LSTM 2 | 41 | 95.7 | - | 96.5 | - | √ |
| 81.4 | 85.5 | |||||||
| [52] | 1 | 5-class RNN 3 + LSTM 2 | NA | 99.6 | 100 | 99.2 | 100 | × |
| [54] | 1 | Binary RF 4 | 6 | 97.4 | 97.4 | 96.7 | 95.3 | √ |
| 3-class ANN 5 | 98.2 | 99 | 95.3 | 93.3 | ||||
| 5-class ANN 6 | 97.8 | 98.6 | 87.2 | 90.9 | ||||
| [59] | 1 | 2-stage CRF 7: 8-class | 70 | - | - | 60 | 85.5 | √ |
| 3-class | 81.1 | 93.4 | ||||||
| [60] | 1 | Binary Adaboost | 20 | 94.4 | 96.2 | - | √ | |
| 5-class RF 4 | - | - | 91 | 95 | ||||
| [61] | 5 | 9-class SVM 7 | 20 | 91.8 | - | 91.1 | - | × |
| 2 | 89 | 88.4 | 93.4 | |||||
| [62] | 3 | 3-stage SVM 7 + HMM 8 | 14 | - | - | 87.2 | - | √ |
| Ref. | #Sen | Method | #Sub | System Accuracy (%) | Drinking Detection Accuracy (%) | Weight Error/ Accuracy | Limitations |
|---|---|---|---|---|---|---|---|
| [87] | 9+ | Rule-based, template matching | 3 | 80 | - | 82.62% accuracy | Small sample size, all objects need RFID |
| [89] | 1264 | DT 1, 7-class No LOSO 2 | 5 | 91 | 99 | 16% RMSE | Low weight accuracy |
| With LOSO 2 | 76 | 99 | |||||
| [91] | 1 | Segmentation and thresholding | 271 | 39% of bites are undetected | 39% of drink sips undetected | - | Many false positives and undetected intakes |
| [92] | 8 | Comparing against acoustic neck microphone | 2 | - | - | <9 g error | Small sample size |
| Ref. | #Sen. | Method | #Sub | System Accuracy/ Precision (%) | Drinking Detection Accuracy (%) | Null Class |
|---|---|---|---|---|---|---|
| [101] | 1 | ANN 1 | 33 | 98.3 | - | × |
| [104] | 1 | 3D CNN 2, 13 classes | 1950 videos | 96.4 | 92 | √ |
| [102] | 4 | Fuzzy vector quantization, LDA 3 3 class | 4 | 93.3 | 100 | √ |
| [105] * | 2 | kNN 4 4 class | 2 | 89.13 | 100 | √ |
| kNN 4 6 class | 95.4 | 93.1 | ||||
| kNN 4 5 class | 98.7 | 96.88 |
| Ref. | Technology | #Sen. | #Sub | System Accuracy (%) | Weight Error |
|---|---|---|---|---|---|
| [120] | IMU | 1 | 7 | 99 | 25% volume |
| [125] | Strain gauge + IMU | 2 | 15 | - | 2 mL |
| [126] | Capacitance | 20 | 1 | - | 3–6% |
| [127] | Conductive electrodes + IMU | 6 | 15 | 94.33 | - |
| [128] | Metal tag + WiFi | 3 | - | 90 | - |
| [129] | Vibration transducer + WiFi | 1 | 6 liquids, 3 containers | >97 | <10% liquid level |
| [147] | IMU + ultrasound, humidity/temperature sensor + pH + turbidity sensor | 6 | 6 | - | - |
| [131] | Water flow sensor | 1 | Unknown | - | 8 mL, 2% |
| Product Name | Price (USD) | Pros | Cons | Size (oz) |
|---|---|---|---|---|
| Hidrate Spark 3 | $59.95 | Clinically validated, Offline glow reminders, Plastic—Light, Saves data locally, sync later | Not rechargeable, No API, Large size | 20 |
| Hidrate Spark Steel | $64.99 | Clinically validated, Rechargeable, Offline glow reminders, Allows ice, Saves data locally, sync later | Hand wash only, No hot drinks, 10–14 day battery, No API, Steel—Heavy | 17/21 |
| H2OPal | $99.99 | API available, Compatible with any bottle of same size, Dishwasher safe, Saves data locally, sync later, Hot liquid allowed | Needs setup, Not rechargeable, No offline reminders | 18.6 |
| Ozmo Active/ Java+ | $69.99 | Differentiates water and coffee, Java + regulates temperature, Real-time sync in app, Rechargeable, LED to indicate hydration goals, Offline vibration reminders | Hand wash only, No API | 16 |
| Thermos Smart lid | $42.35 | Temperature sensor, Rechargeable, Stores locally for up to 1 week, Plastic—Light | No hot liquids, Must be upright to record, Large size | 24 |
| DrinKup | $69 | Shows amount and temperature, Determines whether water is stale, Allows ice, Rechargeable, Stores locally, Simple, subtle design | Not available, limited information | 17 |
| HydraCoach 2.0 | $27.94 | Allows ice, Dishwasher safe, Results directly on bottle | Low-intensity sips may not register, Offline use only, No data transfer, No hot drinks | 22 |
| Droplet | $47.53 | Designed for elderly (light, ergonomic), Looks like normal cup/mug, Compatible base, Light, Voice reminders on bottle, Dishwasher safe | Offline, No access to data | 9.5–11.2 |
| Ref. | Technology | #Sub | Duration of Data | F1-Score from Lab | F1-Score from Free Living Conditions |
|---|---|---|---|---|---|
| [47] | Wearable | 12 lab, 5 free living | - | 97% | 85% |
| [56] | Wearable | 7 free living | 35 days | - | 75.6% |
| [59] | Wearable | 70 total, 8 free living | 24 h | 85.5% | 68.5% |
| [125] | Smart Container | 15 free living | 5 months | - | 2 mL |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cohen, R.; Fernie, G.; Roshan Fekr, A. Fluid Intake Monitoring Systems for the Elderly: A Review of the Literature. Nutrients 2021, 13, 2092. https://doi.org/10.3390/nu13062092
Cohen R, Fernie G, Roshan Fekr A. Fluid Intake Monitoring Systems for the Elderly: A Review of the Literature. Nutrients. 2021; 13(6):2092. https://doi.org/10.3390/nu13062092
Chicago/Turabian StyleCohen, Rachel, Geoff Fernie, and Atena Roshan Fekr. 2021. "Fluid Intake Monitoring Systems for the Elderly: A Review of the Literature" Nutrients 13, no. 6: 2092. https://doi.org/10.3390/nu13062092
APA StyleCohen, R., Fernie, G., & Roshan Fekr, A. (2021). Fluid Intake Monitoring Systems for the Elderly: A Review of the Literature. Nutrients, 13(6), 2092. https://doi.org/10.3390/nu13062092







