Prevalence and Factors Associated with the Triple Burden of Malnutrition among Mother-Child Pairs in Sub-Saharan Africa
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
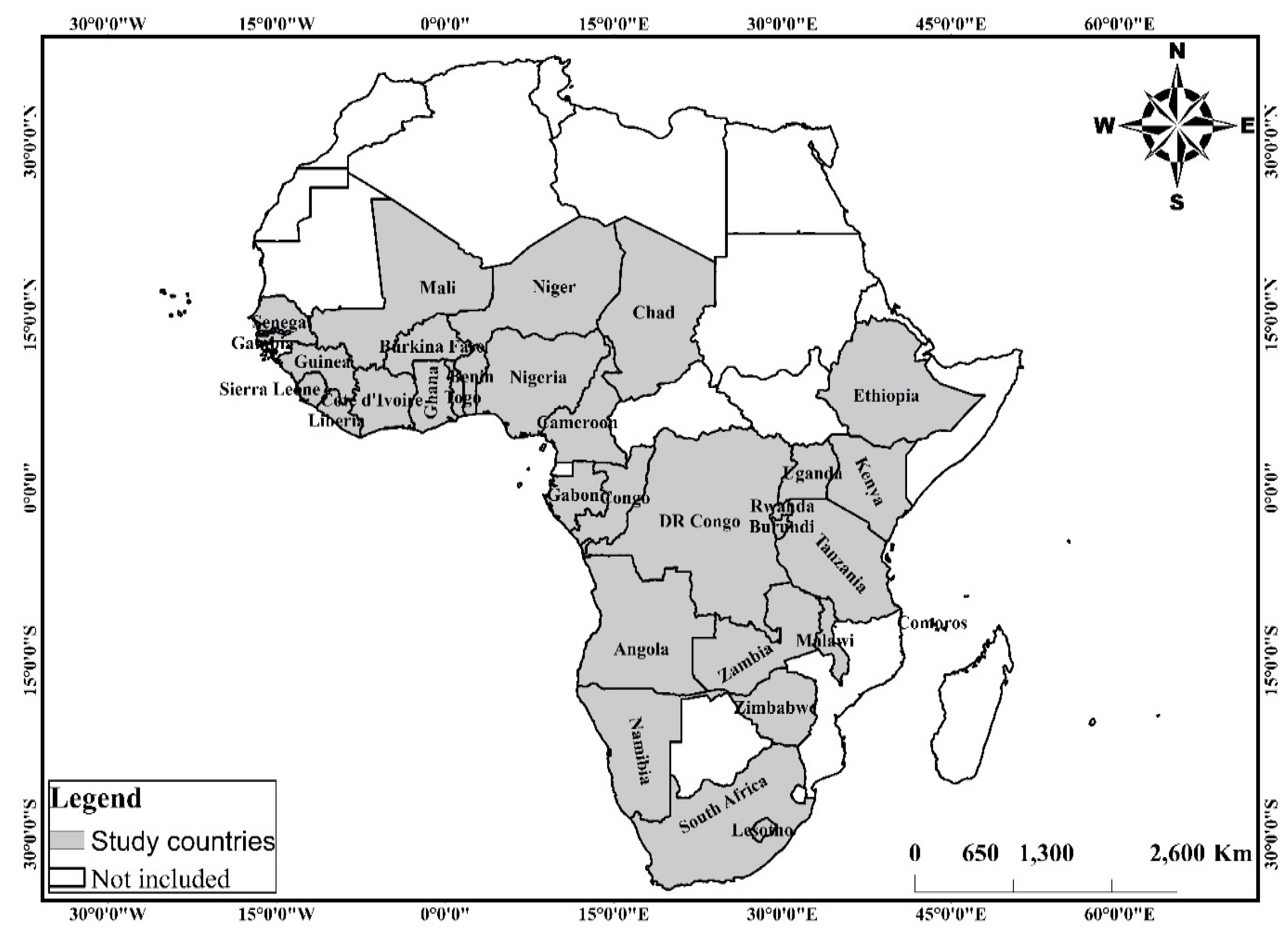
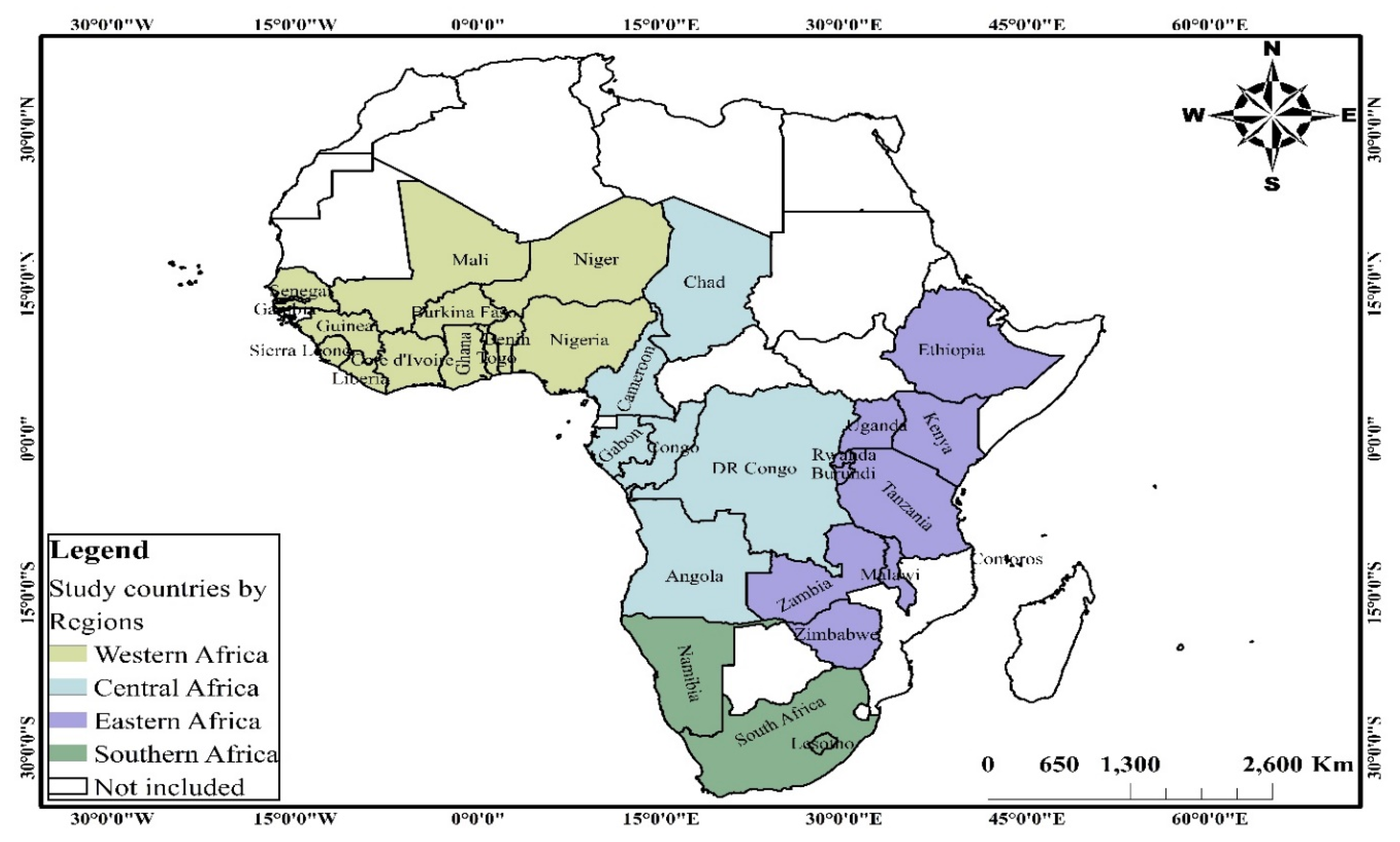
2.2. Data Source, Sampling and Data Collection Procedure
2.3. Measurements
2.3.1. Outcome Variable
2.3.2. Independent Variables
2.4. Data Analyses
2.5. Ethical Approval
3. Results
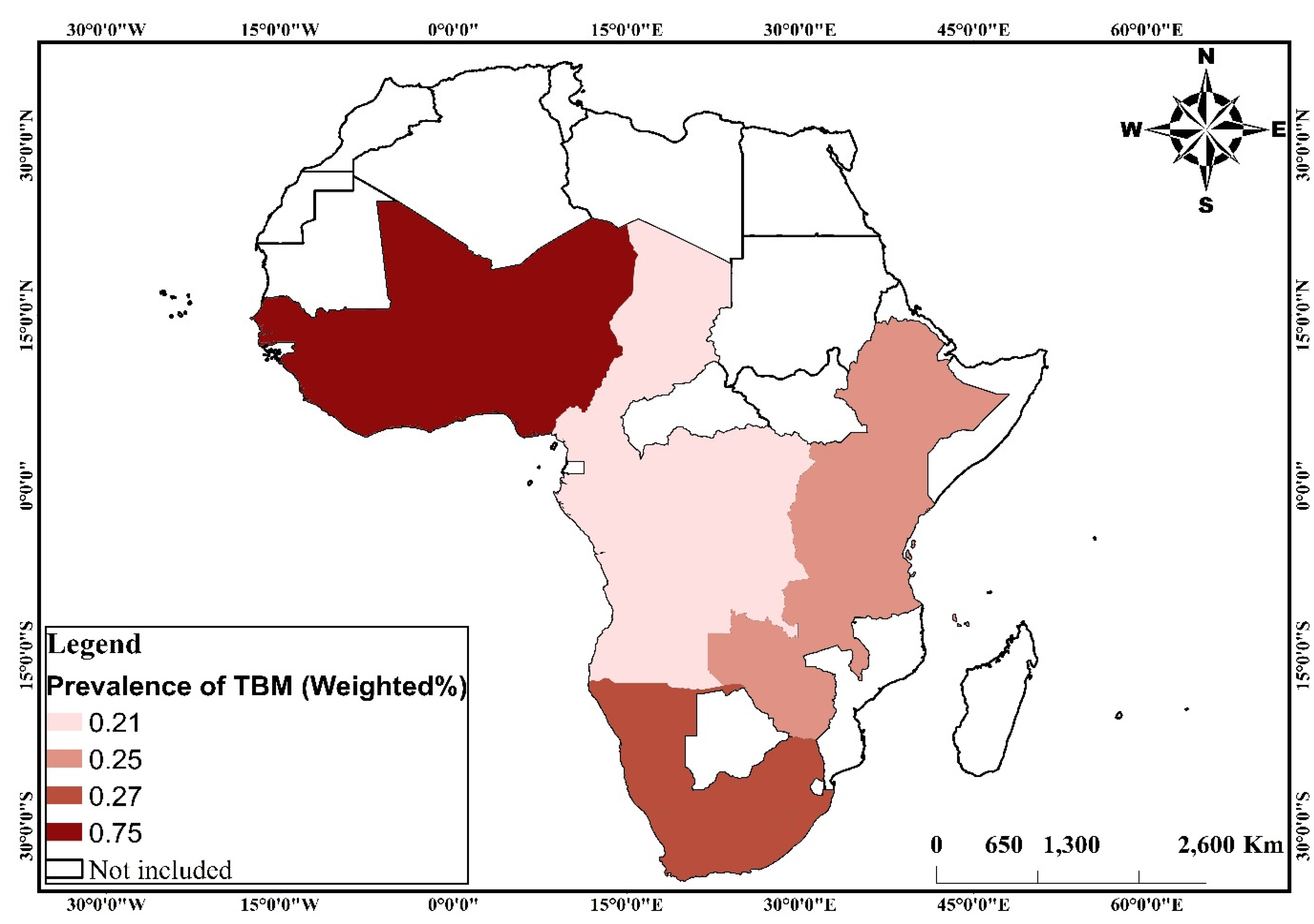
3.1. Descriptive Analysis on TBM Across Four Geographic Regions in SSA
3.2. Multivariate Analysis on the Predictors of TBM
4. Discussion
4.1. Strengths and Limitations
4.2. Practical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SSA | Sub-Saharan Africa |
| TBM | Triple burden of malnutrition |
| DBM | Double burden of malnutrition |
| ANC | Antenatal care visits |
| PNC | Postnatal care visits |
| SDGs | Sustainable Development Goals |
| DHS | Demographic and Health Surveys |
| OM/AC | Obese/overweight mother and anaemic child |
| OM/SC | Obese/overweight mother and stunted child |
| OM/WC | Obese/overweight mother and wasted child |
| OM/UC | Obese/overweight mother and underweight child |
| STROBE | Strengthening the reporting of observational studies in epidemiology |
| aOR | Adjusted odds ratios |
| OR | Odds ratio |
| CI | Confidence intervals |
References
- United Nations. Sustainable Development Goals; United Nations: New York, NY, USA, 2015. [Google Scholar]
- Kumar, P.; Chauhan, S.; Patel, R.; Srivastava, S.; Bansod, D.W. Prevalence and factors associated with triple burden of malnutrition among mother-child pairs in India: A study based on National Family Health Survey 2015–16. BMC Public Health 2021, 21, 1–2. [Google Scholar] [CrossRef]
- Patel, R.; Srivastava, S.; Kumar, P.; Chauhan, S. Factors associated with double burden of malnutrition among mother-child pairs in India: A study based on National Family Health Survey 2015–16. Child. Youth Serv. Rev. 2020, 1, 105256. [Google Scholar] [CrossRef]
- Food and Agriculture Organisation. The State Of Food Security And Nutrition In The World. Rome: Building Resilience for Peace and Food Security. Available online: http://www.fao.org/3/I7695e/I7695e.pdf (accessed on 7 June 2021).
- Pal, A.; Pari, A.K.; Sinha, A.; Dhara, P.C. Prevalence of undernutrition and associated factors: A cross-sectional study among rural adolescents in West Bengal, India. Int. J. Pediatrics Adolesc. Med. 2017, 4, 9–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biswas, T.; Townsend, N.; Magalhaes, R.S.; Islam, M.S.; Hasan, M.M.; Mamun, A. Current progress and future directions in the double burden of malnutrition among women in South and Southeast Asian countries. Curr. Dev. Nutr. 2019, 3, nzz026. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bain, L.E.; Awah, P.K.; Geraldine, N.; Kindong, N.P.; Siga, Y.; Bernard, N.; Tanjeko, A.T. Malnutrition in Sub–Saharan Africa: Burden, causes and prospects. Pan Afr. Med J. 2013, 15, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Meenakshi, J.V. Trends and patterns in the triple burden of malnutrition in India. Agric. Econ. 2016, 47, 115–134. [Google Scholar] [CrossRef] [Green Version]
- Kulkarni, V.S.; Kulkarni, V.S.; Gaiha, R. “Double Burden of Malnutrition” Reexamining the Coexistence of Undernutrition and Overweight Among Women in India. Int. J. Health Serv. 2017, 47, 108–133. [Google Scholar] [CrossRef] [PubMed]
- Mondal, N.; Basumatary, B.; Kropi, J.; Bose, K. Prevalence of double burden of malnutrition among urban school going Bodo children aged 5-11 years of Assam, Northeast India. Epidemiol. Biostat. Public Health 2015, 12. [Google Scholar]
- Davis, J.N.; Oaks, B.M.; Engle-Stone, R. The Double Burden of Malnutrition: A Systematic Review of Operational Definitions. Curr. Dev. Nutr. 2020, 4, nzaa127. [Google Scholar] [CrossRef]
- Sunuwar, D.R.; Singh, D.R.; Pradhan, P.M. Prevalence and factors associated with double and triple burden of malnutrition among mothers and children in Nepal: Evidence from 2016 Nepal Demographic and Health Survey. BMC Public Health 2020, 20, 1–11. [Google Scholar] [CrossRef]
- Amadu, I.; Seidu, A.A.; Duku, E.; Okyere, J.; Hagan, J.E.; Hormenu, T.; Ahinkorah, B.O. The Joint Effect of Maternal Marital Status and Type of Household Cooking Fuel on Child Nutritional Status in Sub-Saharan Africa: Analysis of Cross-Sectional Surveys on Children from 31 Countries. Nutrients 2021, 13, 1541. [Google Scholar] [CrossRef]
- Akombi, B.J.; Agho, K.E.; Merom, D.; Renzaho, A.M.; Hall, J.J. Child malnutrition in sub-Saharan Africa: A meta-analysis of demographic and health surveys (2006–2016). PLoS ONE 2017, 12, e0177338. [Google Scholar] [CrossRef] [Green Version]
- Akombi, B.J.; Agho, K.E.; Hall, J.J.; Wali, N.; Renzaho, A.; Merom, D. Stunting, wasting and underweight in sub-Saharan Africa: A systematic review. Int. J. Environ. Res. Public Health 2017, 14, 863. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akombi, B.J.; Chitekwe, S.; Sahle, B.W.; Renzaho, A. Estimating the double burden of malnutrition among 595,975 children in 65 low-and middle-income countries: A meta-analysis of demographic and health surveys. Int. J. Environ. Res. Public Health 2019, 16, 2886. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Armah, F.A.; Ekumah, B.; Yawson, D.O.; Odoi, J.O.; Afitiri, A.R.; Nyieku, F.E. Access to improved water and sanitation in sub-Saharan Africa in a quarter century. Heliyon 2018, 4, e00931. [Google Scholar] [CrossRef] [Green Version]
- Afitiri, A.R.; Armah, F.A.; Ekumah, B.; Nyieku, F.E.; Yawson, D.O.; Odoi, J.O. Cumulative effects of environmental factors on household childhood diarrhoea in Ghana. Water Pract. Technol. 2020, 15, 1032–1049. [Google Scholar] [CrossRef]
- Armah, F.A.; Ekumah, B.; Yawson, D.O.; Odoi, J.O.; Afitiri, A.R.; Nyieku, F.E. Predictive probabilities of access to clean cooking: Evidence from the demographic and health surveys in 31 countries in sub-saharan Africa. Environ. Justice 2019, 12, 118–131. [Google Scholar] [CrossRef] [Green Version]
- Amegah, A.K.; Boachie, J.; Näyhä, S.; Jaakkola, J.J. Association of biomass fuel use with reduced body weight of adult Ghanaian women. J. Expo. Sci. Environ. Epidemiol. 2020, 30, 670–679. [Google Scholar] [CrossRef]
- Aitkin, M.A.; Aitkin, M.; Francis, B.; Hinde, J. Statistical Modelling in GLIM 4; OUP: Oxford, UK, 2005. [Google Scholar]
- Fahrmeir, L.; Tutz, G. Multivariate Statistical Modelling Based on Generalized Linear Models; Springer Science & Business Media: New York, NY, USA, 2013. [Google Scholar]
- Amugsi, D.A.; Dimbuene, Z.T.; Kyobutungi, C. Correlates of the double burden of malnutrition among women: An analysis of cross sectional survey data from sub-Saharan Africa. BMJ Open 2019, 9, e029545. [Google Scholar] [CrossRef] [Green Version]
- Sámano, R.; Martínez-Rojano, H.; Martínez, E.G.; Jiménez, B.S.; Rodríguez, G.P.; Zamora, J.P.; Casanueva, E. Effects of breastfeeding on weight loss and recovery of pregestational weight in adolescent and adult mothers. Food Nutr. Bull. 2013, 34, 123–130. [Google Scholar] [CrossRef]
- Yourkavitch, J.; Burgert-Brucker, C.; Assaf, S.; Delgado, S. Using geographical analysis to identify child health inequality in sub-Saharan Africa. PLoS ONE 2018, 13, e0201870. [Google Scholar] [CrossRef] [Green Version]
- Hollinger, F.; Staatz, J.M. Agricultural Growth in West Africa. In Market and Policy Drivers; Pobrano październik; FAO, African Development Bank, ECOWAS: Rome, Italy, 2015. [Google Scholar]
- Development Initiatives Poverty Research Ltd. Country Nutrition Profiles. 2020. Available online: https://globalnutritionreport.org/resources/nutrition-profiles/africa/ (accessed on 6 June 2021).
- Behera, S.; Bulliyya, G. Magnitude of anemia and hematological predictors among children under 12 years in Odisha, India. Anemia 2016, 2016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Headey, D.; Menon, P.; Nguyen, P. The Timing of Growth Faltering in India Has Changed Significantly over 1992–2016, with Variations in Prenatal and Postnatal Improvement (P10-005-19). Curr. Dev. Nutr. 2019, 3 (Suppl.1), nzz034-P10. [Google Scholar] [CrossRef]
- Manggala, A.K.; Kenwa, K.W.; Kenwa, M.M.; Jaya, A.A.; Sawitri, A.A. Risk factors of stunting in children aged 24–59 months. Paediatr. Indones. 2018, 58, 205–212. [Google Scholar] [CrossRef]
- Sultana, M.; Sarker, A.R.; Sheikh, N.; Akram, R.; Ali, N.; Mahumud, R.A.; Alam, N.H. Prevalence, determinants and health care-seeking behavior of childhood acute respiratory tract infections in Bangladesh. PLoS ONE 2019, 14, e0210433. [Google Scholar] [CrossRef]
- Trivers, R.L.; Willard, D.E. Natural selection of parental ability to vary the sex ratio of offspring. Science 1973, 179, 90–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wamani, H.; Åstrøm, A.N.; Peterson, S.; Tumwine, J.K.; Tylleskär, T. Boys are more stunted than girls in sub-Saharan Africa: A meta-analysis of 16 demographic and health surveys. BMC Pediatrics 2007, 7, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Sandersa, D.; Hendricksb, M.; Krollc, F.; Puoaned, T.; Ramokoloe, V.; Swartf, R.; Tsolekileg, L. The triple burden of malnutrition in childhood: Causes, policy implementation and recommendations. Child Adolesc. Health 2019, 145. [Google Scholar]
- Singh, K.; Bloom, S.; Brodish, P. Gender equality as a means to improve maternal and child health in Africa. Health Care Women Int. 2015, 36, 57–69. [Google Scholar] [CrossRef]
- Islam, S.; Rana, M.J.; Mohanty, S.K. Cooking, smoking, and stunting: Effects of household air pollution sources on childhood growth in India. Indoor Air 2021, 31, 229–249. [Google Scholar] [CrossRef]
- Upadhyay, A.K.; Singh, A.; Kumar, K.; Singh, A. Impact of indoor air pollution from the use of solid fuels on the incidence of life threatening respiratory illnesses in children in India. BMC Public Health 2015, 15, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variable | Weighted n | (%) | Variable | Weighted n | (%) |
|---|---|---|---|---|---|
| OM/WC | Employment status | ||||
| Normal | 166,058 | 98 | No | 59,817 | 37 |
| Wasting | 3335 | 2 | Yes | 100,628 | 63 |
| OM/SC | ANC | ||||
| Normal | 156,387 | 92 | No | 12,262 | 10 |
| Stunting | 13,007 | 8 | Yes | 106,281 | 90 |
| OM/UC | PNC | ||||
| Normal | 162,158 | 96 | No | 63,838 | 59 |
| Underweight | 7236 | 4 | Yes | 45,140 | 41 |
| OM/AC | Household characteristics | ||||
| Normal | 148,790 | 88 | Age of household head | ||
| Anemic | 20,604 | 12 | Young adults | 75,105 | 44 |
| TBM | Middle-aged adults | 73,311 | 43 | ||
| Normal | 168,660 | 99 | Old-aged adults | 20,975 | 12 |
| OM/SC/WC/UC and AC | 734 | 1 | Sex of household head | ||
| Child characteristics | Male | 136,212 | 80 | ||
| Age of child | Female | 33,182 | 20 | ||
| 0 | 34,564 | 20 | Household size | ||
| 1 | 35,793 | 21 | Small | 69,944 | 41 |
| 2 | 33,487 | 20 | Medium | 78,415 | 46 |
| 3 | 33,693 | 20 | Large | 21,035 | 12 |
| 4 | 31,856 | 19 | Wealth status | ||
| Sex of child | Poor | 75,261 | 44 | ||
| Male | 85,523 | 50 | Middle | 33,996 | 20 |
| Female | 83,871 | 50 | Rich | 60,136 | 36 |
| Birth order | Access to electricity | ||||
| 1 | 35,347 | 21 | No | 119,345 | 70 |
| 2 | 81,981 | 48 | Yes | 50,032 | 30 |
| 3 and above | 52,065 | 31 | Source of drinking water | ||
| Perceived birth size | Improved | 109,141 | 64 | ||
| Larger than average | 54,853 | 34 | Unimproved | 60,232 | 36 |
| Average | 78,374 | 49 | Type of toilet facility | ||
| Smaller than average | 24,950 | 16 | Improved | 72,110 | 43 |
| Do not know | 2314 | 1 | Unimproved | 97,246 | 57 |
| Mother characteristics | Type of cooking fuel | ||||
| Age of mother | Unclean | 154,729 | 91 | ||
| 15–19 | 9383 | 6 | Clean | 14,648 | 9 |
| 20–24 | 36,523 | 22 | Contextual | ||
| 25–29 | 47,310 | 28 | Urbanicity | ||
| 30–34 | 36,577 | 22 | Urban | 52,513 | 31 |
| 35–49 | 25,071 | 15 | Rural | 116,881 | 69 |
| 40–44 | 11,200 | 7 | Geographic region | ||
| 45–49 | 3330 | 2 | Western Africa | 63,978 | 38 |
| Educational attainment | Eastern Africa | 69,144 | 41 | ||
| No formal | 67,012 | 40 | Central Africa | 32,899 | 19 |
| Primary | 58,079 | 34 | Southern Africa | 3373 | 2 |
| Secondary | 38,671 | 23 | n | 169,394 | |
| Higher | 5633 | 3 |
| Variable | TBM (Weighted %) | 95% CIs | p-Value | Variable | TBM (Weighted %) | 95% CIs | p-Value |
|---|---|---|---|---|---|---|---|
| Child characteristics | Household characteristics | ||||||
| Age of child | Age of household head | ||||||
| 0 | 0.26 | 0.21–0.30 | <0.001 | Young adults | 0.37 | 0.32–0.41 | 0.001 |
| 1 | 0.88 | 0.79–0.98 | Middle-aged adults | 0.50 | 0.45–0.55 | ||
| 2 | 0.40 | 0.34–0.48 | Old-aged adults | 0.43 | 0.37–0.55 | ||
| 3 | 0.29 | 0.23–0.35 | Sex of household head | 0.008 | |||
| 4 | 0.30 | 0.24–0.37 | Male | 0.46 | 0.43–0.50 | ||
| Sex of child | Female | 0.31 | 0.26–0.38 | ||||
| Male | 0.56 | 0.51–0.61 | <0.001 | Household size | |||
| Female | 0.31 | 0.27–0.34 | Small | 0.36 | 0.32–0.41 | <0.001 | |
| Birth order | Medium | 0.41 | 0.37–0.46 | ||||
| 1 | 0.31 | 0.25–0.37 | <0.001 | Large | 0.74 | 0.63–0.86 | |
| 2 | 0.39 | 0.34–0.43 | Wealth status | ||||
| 3 and above | 0.59 | 0.53–0.66 | Poor | 0.56 | 0.51–0.62 | <0.001 | |
| Perceived birth size | Middle | 0.42 | 0.36–0.50 | ||||
| Larger than average | 0.27 | 0.22–0.32 | <0.001 | Rich | 0.28 | 0.24–0.32 | |
| Average | 0.47 | 0.42–0.52 | Access to electricity | ||||
| Smaller than average | 0.83 | 0.72–0.95 | No | 0.48 | 0.44–0.53 | <0.001 | |
| Do not know | 0.51 | 0.28–0.90 | Yes | 0.31 | 0.27–0.37 | ||
| Mother characteristics | Source of drinking water | ||||||
| Age of mother | Improved | 0.42 | 0.38–0.46 | 0.038 | |||
| 15–19 | 0.40 | 0.28–0.54 | 0.284 | Unimproved | 0.46 | 0.41–0.52 | |
| 20–24 | 0.33 | 0.28–0.40 | Type of toilet facility | ||||
| 25–29 | 0.42 | 0.36–0.48 | Improved | 0.28 | 0.24–0.32 | <0.001 | |
| 30–34 | 0.46 | 0.39–0.53 | Unimproved | 0.55 | 0.50–0.59 | ||
| 35–49 | 0.55 | 0.46–0.70 | Type of cooking fuel | ||||
| 40–44 | 0.45 | 0.33–0.59 | Unclean | 0.47 | 0.43–0.50 | <0.001 | |
| 45–49 | 0.69 | 0.44–10.3 | Clean | 0.08 | 0.04–0.10 | ||
| Educational attainment | Contextual | ||||||
| No formal | 0.75 | 0.69–0.82 | <0.001 | Urbanicity | |||
| Primary | 0.28 | 0.24–0.33 | Urban | 0.26 | 0.22–0.31 | <0.001 | |
| Secondary | 0.15 | 0.11–0.19 | Rural | 0.51 | 0.47–0.55 | ||
| Higher | 0.20 | 0.10–0.35 | Geographic region | ||||
| Employment status | Western Africa | 0.75 | 0.69–0.82 | <0.001 | |||
| No | 0.51 | 0.45–0.57 | <0.001 | Eastern Africa | 0.25 | 0.22–0.29 | |
| Yes | 0.43 | 0.39–0.47 | Central Africa | 0.21 | 0.16–0.26 | ||
| ANC | Southern Africa | 0.27 | 0.12–0.51 | ||||
| No | 0.91 | 0.75–10.9 | <0.001 | ||||
| Yes | 0.42 | 0.38–0.46 | |||||
| PNC | |||||||
| No | 0.54 | 0.48–0.60 | 0.113 | ||||
| Yes | 0.43 | 0.37–0.50 |
| Variable | aOR | Robust SE | p-Value | 95% CIs | |
|---|---|---|---|---|---|
| Child characteristics | |||||
| Age of child (Ref: 0) | |||||
| 1 | 1.283 | 0.036 | <0.001 | 1.215 | 1.355 |
| 2 | 1.133 | 0.035 | <0.001 | 1.067 | 1.204 |
| 3 | 0.996 | 0.043 | 0.928 | 0.916 | 1.084 |
| 4 | 1.013 | 0.051 | 0.792 | 0.918 | 1.118 |
| Sex of child (Ref: male) | |||||
| Female | 0.859 | 0.019 | <0.001 | 0.824 | 0.896 |
| Perceived birth size (Ref: larger than average) | |||||
| Average | 1.133 | 0.030 | <0.001 | 1.076 | 1.193 |
| Smaller than average | 1.278 | 0.039 | <0.001 | 1.204 | 1.356 |
| Do not know | 1.180 | 0.117 | 0.094 | 0.972 | 1.432 |
| Birth order (Ref: 0) | |||||
| 2 | 1.031 | 0.032 | 0.329 | 0.970 | 1.096 |
| 3 and above | 1.062 | 0.037 | 0.084 | 0.992 | 1.136 |
| Mother characteristics | |||||
| Educational attainment (Ref: no formal) | |||||
| Primary | 0.922 | 0.030 | 0.014 | 0.865 | 0.984 |
| Secondary | 0.829 | 0.028 | <0.001 | 0.777 | 0.885 |
| Higher | 0.955 | 0.086 | 0.611 | 0.800 | 1.140 |
| Employment status (Ref: no) | |||||
| Yes | 0.969 | 0.022 | 0.155 | 0.927 | 1.012 |
| ANC (Ref: no) | |||||
| Yes | 0.941 | 0.028 | 0.043 | 0.887 | 0.998 |
| Household characteristics | |||||
| Age of household head (Ref: young adult) | |||||
| Middle-aged adults | 1.020 | 0.026 | 0.451 | 0.969 | 1.073 |
| Old-aged adults | 0.981 | 0.032 | 0.552 | 0.920 | 1.046 |
| Sex of household head (Ref: male) | |||||
| Female | 0.973 | 0.029 | 0.362 | 0.917 | 1.032 |
| Household size (Ref: small) | |||||
| Medium | 0.980 | 0.026 | 0.453 | 0.930 | 1.033 |
| Large | 1.059 | 0.034 | 0.078 | 0.994 | 1.128 |
| Wealth status (Ref: poor) | |||||
| Middle | 0.978 | 0.026 | 0.415 | 0.928 | 1.031 |
| Rich | 0.958 | 0.030 | 0.170 | 0.901 | 1.018 |
| Source of drinking water (Ref: improved) | |||||
| Unimproved | 0.985 | 0.021 | 0.472 | 0.945 | 1.027 |
| Type of toilet facility (Ref: improved) | |||||
| Unimproved | 1.052 | 0.030 | 0.077 | 0.994 | 1.113 |
| Type of Cooking fuel (Ref: unclean) | |||||
| Clean | 0.724 | 0.062 | <0.001 | 0.612 | 0.857 |
| Access to electricity (Ref: no) | |||||
| Yes | 0.992 | 0.031 | 0.785 | 0.932 | 1.054 |
| Contextual factors | |||||
| Urbanicity (Ref: urban) | |||||
| Rural | 1.035 | 0.033 | 0.283 | 0.972 | 1.102 |
| Geographic region (Ref: western Africa) | |||||
| Eastern Africa | 0.837 | 0.025 | <0.001 | 0.789 | 0.888 |
| Central Africa | 0.822 | 0.028 | <0.001 | 0.768 | 0.880 |
| Southern Africa | 0.859 | 0.080 | 0.103 | 0.715 | 1.031 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahinkorah, B.O.; Amadu, I.; Seidu, A.-A.; Okyere, J.; Duku, E.; Hagan, J.E., Jr.; Budu, E.; Archer, A.G.; Yaya, S. Prevalence and Factors Associated with the Triple Burden of Malnutrition among Mother-Child Pairs in Sub-Saharan Africa. Nutrients 2021, 13, 2050. https://doi.org/10.3390/nu13062050
Ahinkorah BO, Amadu I, Seidu A-A, Okyere J, Duku E, Hagan JE Jr., Budu E, Archer AG, Yaya S. Prevalence and Factors Associated with the Triple Burden of Malnutrition among Mother-Child Pairs in Sub-Saharan Africa. Nutrients. 2021; 13(6):2050. https://doi.org/10.3390/nu13062050
Chicago/Turabian StyleAhinkorah, Bright Opoku, Iddrisu Amadu, Abdul-Aziz Seidu, Joshua Okyere, Eric Duku, John Elvis Hagan, Jr., Eugene Budu, Anita Gracious Archer, and Sanni Yaya. 2021. "Prevalence and Factors Associated with the Triple Burden of Malnutrition among Mother-Child Pairs in Sub-Saharan Africa" Nutrients 13, no. 6: 2050. https://doi.org/10.3390/nu13062050









