Caregiver Social Status and Health-Related Quality of Life in Neurologically Impaired Children on Home Enteral Nutrition
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Data Collection
2.3. Statistical Analysis
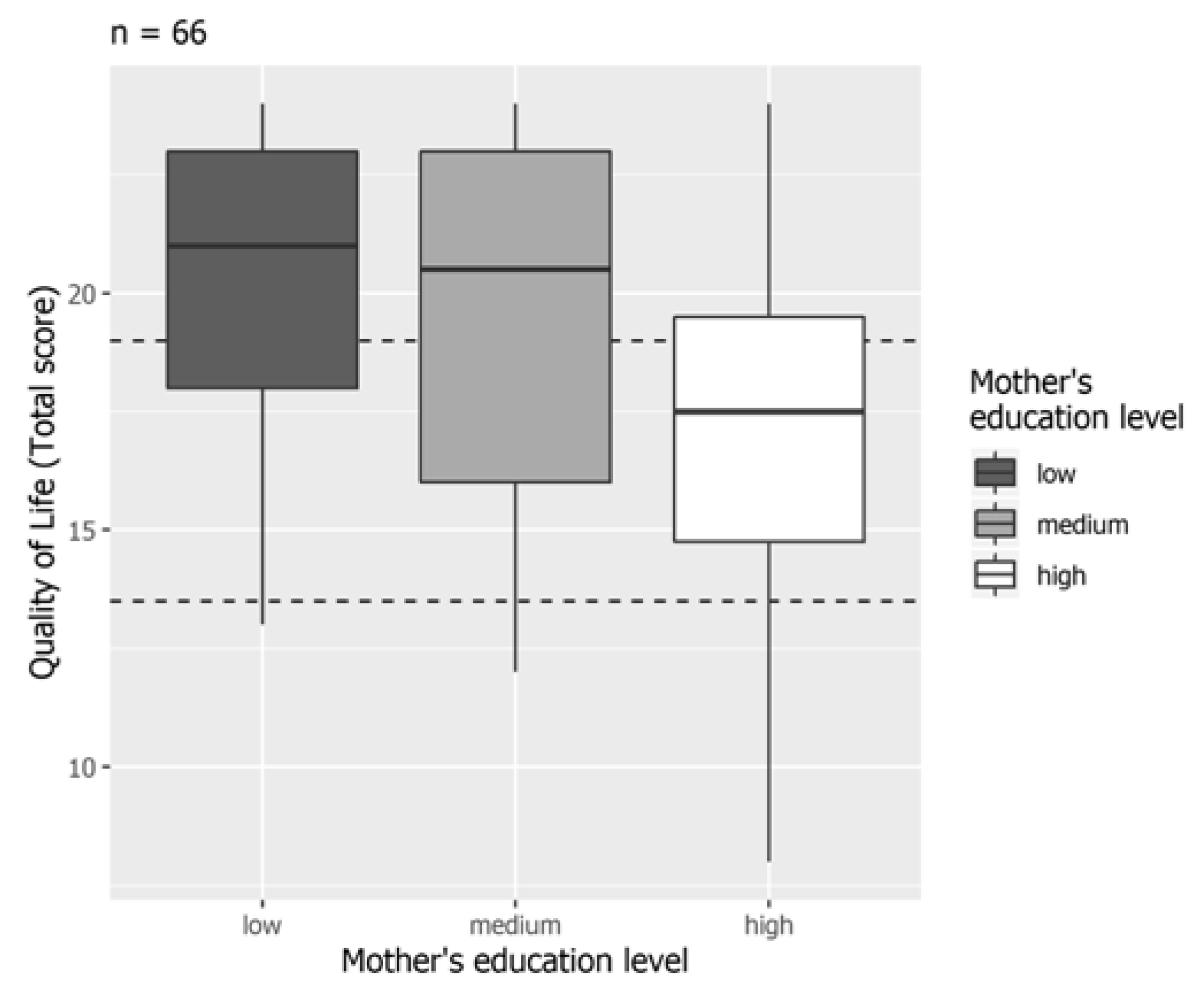
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Measuring Healthy Days: Population Assessment of Health-Related Quality of Life; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2000. [Google Scholar]
- Bottomley, A. The cancer patient and quality of life. Oncologist 2002, 7, 120–125. [Google Scholar] [CrossRef]
- Bjornson, K.F.; McLaughlin, J.F. The measurement of health-related quality of life (HRQL) in children with cerebral palsy. Eur. J. Neurol. 2001, 8, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Barreto, T.M.; Bento, M.N.; Barreto, T.M.; Jagersbacher, J.G.; Jones, N.S.; Lucena, R.; Bandeira, I.D. Prevalence of depression, anxiety, and substance-related disorders in parents of children with cerebral palsy: A systematic review. Dev. Med. Child Neurol. 2020, 62, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Dipasquale, V.; Catena, M.A.; Cardile, S.; Romano, C. Standard Polymeric Formula Tube Feeding in Neurologically Impaired Children: A Five-Year Retrospective Study. Nutrients 2018, 10, 684. [Google Scholar] [CrossRef] [PubMed]
- Romano, C.; van Wynckel, M.; Hulst, J.; Broekaert, I.; Bronsky, J.; Dall’Oglio, L.; Mis, N.F.; Hojsak, I.; Orel, R.; Papadopoulou, A.; et al. European Society for Paediatric Gastroenterology, Hepatology and Nutrition Guidelines for the Evaluation and Treatment of Gastrointestinal and Nutritional Complications in Children With Neurological Impairment. J. Pediatr. Gastroenterol. Nutr. 2017, 65, 242–264. [Google Scholar] [CrossRef] [PubMed]
- Romano, C.; Dipasquale, V.; Gottrand, F.; Sullivan, P.B. Gastrointestinal and nutritional issues in children with neurological disability. Dev. Med. Child Neurol. 2018, 60, 892–896. [Google Scholar] [CrossRef]
- McNamara, E.P.; Flood, P.; Kennedy, N.P. Home tube feeding: An integrated multidisciplinary approach. J. Hum. Nutr. Diet. 2001, 14, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Daveluy, W.; Guimber, D.; Uhlen, S.; Lescut, D.; Michaud, L.; Turck, D.; Gottrand, F. Dramatic Changes in Home-based Enteral Nutrition Practices in Children During an 11-year Period. J. Pediatr. Gastroenterol. Nutr. 2006, 43, 240–244. [Google Scholar] [CrossRef]
- Diamanti, A.; Di Ciommo, V.M.; Tentolini, A.; Lezo, A.; Spagnuolo, M.I.; Campanozzi, A.; Panetta, F.; Basso, M.S.; Elia, D.; Gambarara, M. Home enteral nutrition in children: A 14-year multicenter survey. Eur. J. Clin. Nutr. 2012, 67, 53–57. [Google Scholar] [CrossRef]
- Sullivan, P.B.; Juszczak, E.; Bachlet, A.M.; Thomas, A.G.; Lambert, B.; Vernon-Roberts, A.; Grant, H.W.; Eltumi, M.; Alder, N.; Jenkinson, C. Impact of gastrostomy tube feeding on the quality of life of carers of children with cerebral palsy. Dev. Med. Child Neurol. 2004, 46, 796–800. [Google Scholar] [CrossRef]
- Grzybowska-Chlebowczyk, U.; Więcek, S.; Popinska, K.; Szlagatys-Sidorkiewicz, A.; Toporowska-Kowalska, E.; Hapyn, E.; Wernicka, A.; Sibilska, M.; Gębora-Kowalska, B.; Borkowska, A.; et al. The evaluation of life quality of families of children after percutaneous endoscopic gastrostomy. Pediatr. Polska 2015, 90, 103–107. [Google Scholar] [CrossRef]
- Sauder, M.; Lynn, F.; Podolny, J.M. Status: Insights from Organizational Sociology. Annu. Rev. Sociol. 2012, 38, 267–283. [Google Scholar] [CrossRef]
- Adler, N.E.; Boyce, T.; Chesney, M.A.; Cohen, S.; Folkman, S.; Kahn, R.L.; Syme, S.L.; Al, E. Socioeconomic status and health: The challenge of the gradient. Am. Psychol. 1994, 49, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, H.; Taki, Y.; Nouchi, R.; Yokoyama, R.; Kotozaki, Y.; Nakagawa, S.; Sekiguchi, A.; Iizuka, K.; Yamamoto, Y.; Hanawa, S.; et al. The Effects of Family Socioeconomic Status on Psychological and Neural Mechanisms as Well as Their Sex Differences. Front. Hum. Neurosci. 2019, 12, 543. [Google Scholar] [CrossRef] [PubMed]
- Hair, N.L.; Hanson, J.L.; Wolfe, B.; Pollak, S.D. Association of Child Poverty, Brain Development, and Academic Achievement. JAMA Pediatr. 2015, 169, 822–829. [Google Scholar] [CrossRef] [PubMed]
- Noble, K.; Wolmetz, M.E.; Ochs, L.G.; Farah, M.J.; McCandliss, B.D. Brain?behavior relationships in reading acquisition are modulated by socioeconomic factors. Dev. Sci. 2006, 9, 642–654. [Google Scholar] [CrossRef]
- Bowey, J.A. Socioeconomic status differences in preschool phonological sensitivity and first-grade reading achievement. J. Educ. Psychol. 1995, 87, 476–487. [Google Scholar] [CrossRef]
- Noble, K.; McCandliss, B.D.; Farah, M.J. Socioeconomic gradients predict individual differences in neurocognitive abilities. Dev. Sci. 2007, 10, 464–480. [Google Scholar] [CrossRef] [PubMed]
- Evans, G.W.; English, K. The Environment of Poverty: Multiple Stressor Exposure, Psychophysiological Stress, and Socioemotional Adjustment. Child Dev. 2002, 73, 1238–1248. [Google Scholar] [CrossRef]
- Evans, G.W.; Gonnella, C.; Marcynyszyn, L.A.; Gentile, L.; Salpekar, N. The Role of Chaos in Poverty and Children’s Socioemotional Adjustment. Psychol. Sci. 2005, 16, 560–565. [Google Scholar] [CrossRef]
- Sirin, S.R. Socioeconomic Status and Academic Achievement: A Meta-Analytic Review of Research. Rev. Educ. Res. 2005, 75, 417–453. [Google Scholar] [CrossRef]
- Sweitzer, M.M.; Donny, E.C.; Dierker, L.C.; Flory, J.D.; Manuck, S.B. Delay discounting and smoking: Association with the Fagerstrom Test for Nicotine Dependence but not cigarettes smoked per day. Nicotine Tob. Res. 2008, 10, 1571–1575. [Google Scholar] [CrossRef]
- Didsbury, M.S.; Kim, S.; Medway, M.M.; Tong, A.; McTaggart, S.J.; Walker, A.M.; White, S.; Mackie, F.E.; Kara, T.; Craig, J.C.; et al. Socio-economic status and quality of life in children with chronic disease: A systematic review. J. Paediatr. Child Heal. 2016, 52, 1062–1069. [Google Scholar] [CrossRef]
- Vanz, A.P.; Félix, T.M.; Da Rocha, N.S.; Schwartz, I.V.D. Quality of life in caregivers of children and adolescents with Osteogenesis Imperfecta. Heal. Qual. Life Outcomes 2015, 13, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Xiang, L.; Su, Z.; Liu, Y.; Huang, Y.; Zhang, X.; Li, S.; Zhang, H. Impact of Family Socioeconomic Status on Health-Related Quality of Life in Children With Critical Congenital Heart Disease. J. Am. Hear. Assoc. 2019, 8, e010616. [Google Scholar] [CrossRef] [PubMed]
- Dipasquale, V.; Ventimiglia, M.; Gramaglia, S.M.C.; Parma, B.; Furnari, C.; Selicorni, A.; Armano, C.; Salvatore, S.; Romano, C. Health-Related Quality of Life and Home Enteral Nutrition in Children with Neurological Impairment: Report from a Multicenter Survey. Nutrients 2019, 11, 2968. [Google Scholar] [CrossRef] [PubMed]
- Khayatzadeh, M.M.; Rostami, H.R.; Amirsalari, S.; Karimloo, M. Investigation of quality of life in mothers of children withcerebral palsy in Iran: Association with socio-economic status, marital satisfaction and fatigue. Disabil. Rehabil. 2012, 35, 803–808. [Google Scholar] [CrossRef] [PubMed]
- Sundrum, R.; Logan, S.; Wallace, A.; Spencer, N. Cerebral palsy and socioeconomic status: A retrospective cohort study. Arch. Dis. Child. 2005, 90, 15–18. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Odding, E.; Roebroeck, M.E.; Stam, H.J. The epidemiology of cerebral palsy: Incidence, impairments and risk factors. Disabil. Rehabil. 2006, 28, 183–191. [Google Scholar] [CrossRef]
- Solaski, M.; Majnemer, A.; Oskoui, M. Contribution of socio-economic status on the prevalence of cerebral palsy: A systematic search and review. Dev. Med. Child Neurol. 2014, 56, 1043–1051. [Google Scholar] [CrossRef]
- Raina, P.; O’Donnell, M.; Schwellnus, H.; Rosenbaum, P.; King, G.; Brehaut, J.; Russell, D.; Swinton, M.; King, S.; Wong, M.; et al. Caregiving process and caregiver burden: Conceptual models to guide research and practice. BMC Pediatr. 2004, 4, 1. [Google Scholar] [CrossRef]
- Blacher, J.; Shapiro, J.; Lopez, S.; Diaz, L.; Fusco, J. Depression in Latina mothers of children with mental retardation: A ne-glected concern. Am. J. Ment. Retard. 1997, 101, 483–496. [Google Scholar]
- Yilmaz, H.; Erkin, G.; Izki, A.A. Quality of Life in Mothers of Children with Cerebral Palsy. ISRN Rehabil. 2013, 2013, 1–5. [Google Scholar] [CrossRef]
- Adegoke, B.; Adenuga, O.O.; Olaleye, O.A.; Akosile, C.O. Quality of life of mothers of children with cerebral palsy and their age-matched controls. Afr. J. Neurol. Sci. 2014, 33, 71–78. [Google Scholar]
- Nelson, K.E.; Lacombe-Duncan, A.; Cohen, E.; Nicholas, D.B.; Rosella, L.C.; Guttmann, A.; Mahant, S. Family Experiences With Feeding Tubes in Neurologic Impairment: A Systematic Review. Pediatrics 2015, 136, e140–e151. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.; Lee, E.O. Caregiver Burden and Social Support among Mothers Raising Children with Developmental Disabilities in South Korea. Int. J. Disabil. Dev. Educ. 2009, 56, 149–167. [Google Scholar] [CrossRef]
- Ones, K.; Yilmaz, E.; Cetinkaya, B.; Caglar, N. Assessment of the Quality of Life of Mothers of Children with Cerebral Palsy (Primary Caregivers). Neurorehabil. Neural Repair 2005, 19, 232–237. [Google Scholar] [CrossRef]

| Total Score | HRQoL | Total, n = 75 |
|---|---|---|
| 20–24 | Excellent | 47 (62.7%) |
| 14–19 | Good | 22 (29.3%) |
| 7–13 | Acceptable | 6 (8.0%) |
| 0–6 | Poor | 0 |
| Variable | Mothers, n = 66 | Fathers, n = 23 | Grandmothers, n = 4 |
|---|---|---|---|
| Education level | |||
| Low | 30 (45.4%) | 14 (60.9%) | 2 (50.0%) |
| Medium | 33 (48.5%) | 7 (30.4%) | 2 (50.0%) |
| High | 4 (6.1%) | 2 (8.7%) | 0 |
| Occupation level | |||
| Level 1 | 55 (83.3%) | 16 (69.6%) | 2 (50.0%) |
| Level 2 | 8 (12.1%) | 6 (26.1%) | 1 (25.0%) |
| Level 3 | 3 (4.6%) | 1 (4.3%) | 1 (25.0%) |
| Marital status | |||
| Married | 57 (86.4%) | 21 (91.3%) | 2 (50.0%) |
| Divorced/separated | 8 (12.1%) | 2 (8.7%) | 2 (50.0%) |
| Widow(er) | 1 (1.5%) | 0 | 0 |
| Variable | β | (95% CI) | p |
|---|---|---|---|
| (intercept) | 13.02 | (6.72, 19.75) | <0.001 |
| Neurological disease (ref = genetic) | 3.09 | (1.04, 5.11) | 0.004 |
| Metabolic disease (ref = genetic) | 1.19 | (−2.38, 4.97) | 0.528 |
| Caregiver both parents (ref = only mother) | 1.55 | (−0.48, 3.60) | 0.141 |
| Age at hen beginning (years) | 0.05 | (−0.21, 0.32) | 0.708 |
| HEN duration (years) | −0.24 | (−0.50, 0.01) | 0.065 |
| Mother’s occupation level 2 (ref = level 1) | 0.70 | (−2.66, 4.16) | 0.690 |
| Mother’s occupation level 3 (ref = level 1) | 4.50 | (−1.42, 10.65) | 0.113 |
| Mother’s education level low (ref = high) | 5.97 | (0.10, 11.51) | 0.027 |
| Mother’s education level medium (ref = high) | 4.85 | (−0.53, 9.87) | 0.044 |
| Variable | β | (95% CI) | p |
|---|---|---|---|
| (intercept) | 19.52 | (16.80, 22.34) | <0.001 |
| Neurological disease (ref = genetic) | 5.07 | (2.38, 7.70) | 0.002 |
| Metabolic disease (ref = genetic) | 2.21 | (−0.78, 5.21) | 0.173 |
| HEN duration (years) | −0.27 | (−0.52, −0.01) | 0.058 |
| Father occupation level 2 (ref = level 1) | −0.63 | (−3.50, 2.28) | 0.682 |
| Father occupation level 3 (ref = level 1) | 6.17 | (−0.19, 12.61) | 0.081 |
| Father’s education level low (ref = high) | 6.28 | (1.58, 10.69) | 0.017 |
| Father’s education level medium (ref = high) | 5.50 | (1.00, 9.67) | 0.025 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dipasquale, V.; Ventimiglia, M.; Gramaglia, S.M.C.; Parma, B.; Funari, C.; Selicorni, A.; Armano, C.; Salvatore, S.; Romano, C. Caregiver Social Status and Health-Related Quality of Life in Neurologically Impaired Children on Home Enteral Nutrition. Nutrients 2021, 13, 1928. https://doi.org/10.3390/nu13061928
Dipasquale V, Ventimiglia M, Gramaglia SMC, Parma B, Funari C, Selicorni A, Armano C, Salvatore S, Romano C. Caregiver Social Status and Health-Related Quality of Life in Neurologically Impaired Children on Home Enteral Nutrition. Nutrients. 2021; 13(6):1928. https://doi.org/10.3390/nu13061928
Chicago/Turabian StyleDipasquale, Valeria, Marco Ventimiglia, Simone Maria Calogero Gramaglia, Barbara Parma, Caterina Funari, Angelo Selicorni, Chiara Armano, Silvia Salvatore, and Claudio Romano. 2021. "Caregiver Social Status and Health-Related Quality of Life in Neurologically Impaired Children on Home Enteral Nutrition" Nutrients 13, no. 6: 1928. https://doi.org/10.3390/nu13061928
APA StyleDipasquale, V., Ventimiglia, M., Gramaglia, S. M. C., Parma, B., Funari, C., Selicorni, A., Armano, C., Salvatore, S., & Romano, C. (2021). Caregiver Social Status and Health-Related Quality of Life in Neurologically Impaired Children on Home Enteral Nutrition. Nutrients, 13(6), 1928. https://doi.org/10.3390/nu13061928







