Prevalence and Correlates of Vitamin D Deficiency among Young South African Infants: A Birth Cohort Study
Abstract
1. Introduction
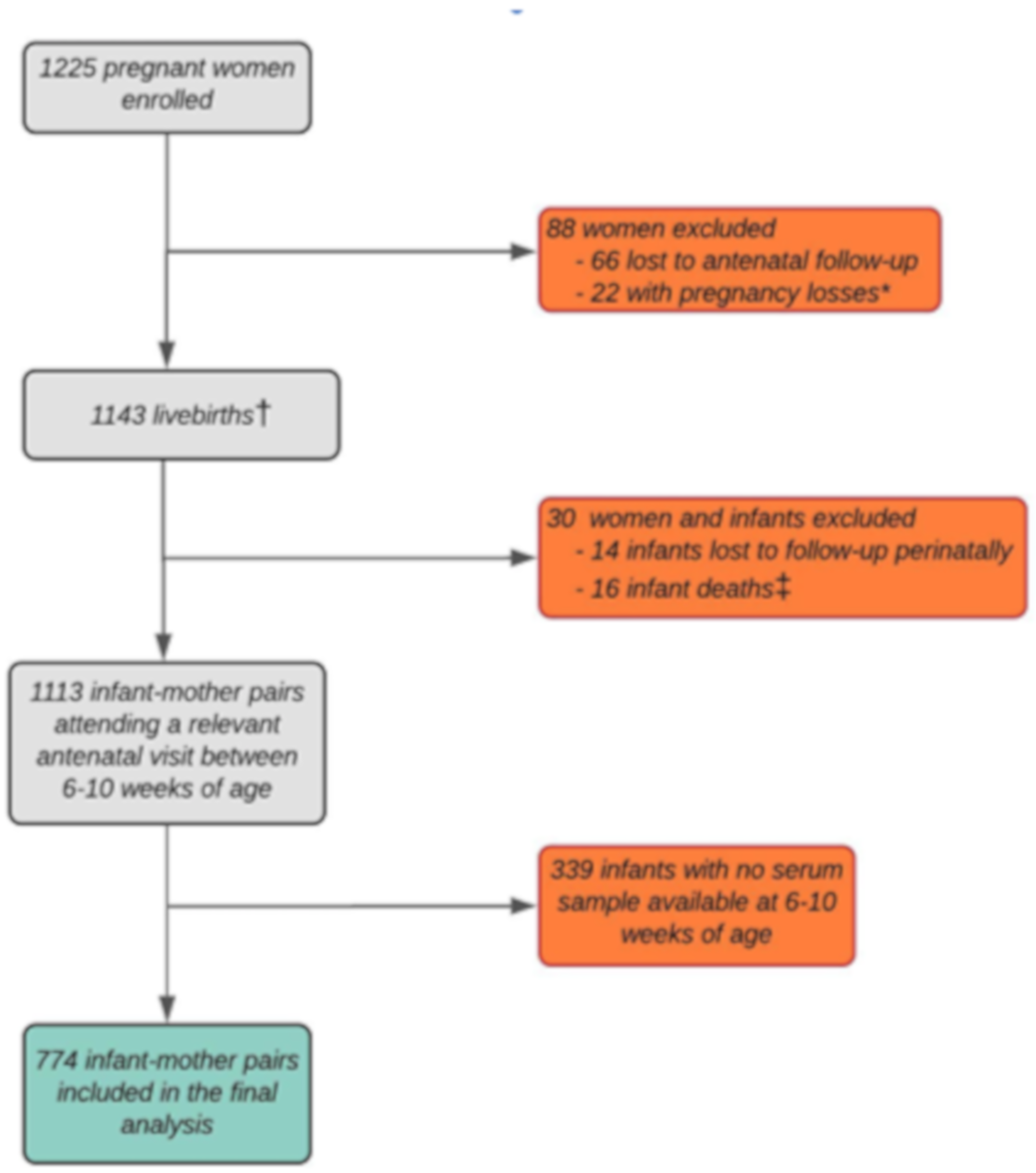
2. Materials and Methods
2.1. Study Setting and Participants
2.2. Vitamin D Status
2.3. Covariates
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Antonucci, R.; Locci, C.; Clemente, M.G.; Chicconi, E.; Antonucci, L. Vitamin D deficiency in childhood: Old lessons and current challenges. J. Pediatric Endocrinol. Metab. 2018, 31, 247–260. [Google Scholar] [CrossRef]
- Fiscaletti, M.; Stewart, P.; Munns, C.F. The importance of vitamin D in maternal and child health: A global perspective. Public Health Rev. 2017, 38, 19. [Google Scholar] [CrossRef]
- Larkin, A.; Lassetter, J. Vitamin D deficiency and acute lower respiratory infections in children younger than 5 years: Identification and treatment. J Pediatric Health Care 2014, 28, 572–582. [Google Scholar] [CrossRef] [PubMed]
- Esposito, S.; Lelii, M. Vitamin D and respiratory tract infections in childhood. BMC Infect. Dis. 2015, 15, 1–10. [Google Scholar] [CrossRef]
- Lai, S.-H.; Liao, S.-L.; Tsai, M.-H.; Hua, M.-C.; Chiu, C.-Y.; Yeh, K.-W.; Yao, T.-C.; Huang, J.-L. Low cord-serum 25-hydroxyvitamin D levels are associated with poor lung function performance and increased respiratory infection in infancy. PLoS ONE 2017, 12, e0173268. [Google Scholar] [CrossRef]
- Litonjua, A.A. Vitamin D and Childhood Asthma-causation and contribution to disease activity. Curr. Opin. Allergy Clin. Immunol. 2019, 19, 126. [Google Scholar] [CrossRef] [PubMed]
- Jolliffe, D.A.; Greenberg, L.; Hooper, R.L.; Griffiths, C.J.; Camargo, C.A., Jr.; Kerley, C.P.; Jensen, M.E.; Mauger, D.; Stelmach, I.; Urashima, M. Vitamin D supplementation to prevent asthma exacerbations: A systematic review and meta-analysis of individual participant data. Lancet Respir. Med. 2017, 5, 881–890. [Google Scholar] [CrossRef]
- Feng, R.; Li, Y.; Li, G.; Li, Z.; Zhang, Y.; Li, Q.; Sun, C. Lower serum 25 (OH) D concentrations in type 1 diabetes: A meta-analysis. Diabetes Res. Clin. Pract. 2015, 108, e71–e75. [Google Scholar] [CrossRef] [PubMed]
- Pilz, S.; Trummer, C.; Pandis, M.; Schwetz, V.; Aberer, F.; Gruebler, M.; Verheyen, N.; Tomaschitz, A.; Maerz, W. Vitamin D: Current guidelines and future outlook. Anticancer Res. 2018, 38, 1145–1151. [Google Scholar]
- Holick, M.F.; Chen, T.C. Vitamin D deficiency: A worldwide problem with health consequences. Am. J. Clin. Nutr. 2008, 87, 1080S–1086S. [Google Scholar] [CrossRef]
- Ali, N. Role of vitamin D in preventing of COVID-19 infection, progression and severity. J. Infect. Public Health 2020, 13, 1373–1380. [Google Scholar] [CrossRef]
- Dattola, A.; Silvestri, M.; Bennardo, L.; Passante, M.; Scali, E.; Patruno, C.; Nisticò, S.P. Role of Vitamins in Skin Health: A Systematic Review. Curr. Nutr. Rep. 2020, 9, 226–235. [Google Scholar] [CrossRef]
- Massoud, M.N.; Rizk, M.M.; Mahfouz, A.A.; Mahmoud, N.A. Vitamin D status in a neonate–mother pair attending Alexandria University Children’s Hospital during the first week of life. Alex. J. Pediatrics 2018, 31, 52. [Google Scholar]
- Salameh, K.; Al-Janahi, N.S.A.; Reedy, A.M.; Dawodu, A. Prevalence and risk factors for low vitamin D status among breastfeeding mother–infant dyads in an environment with abundant sunshine. Int. J. Women’s Health 2016, 8, 529. [Google Scholar]
- Ayadi, I.D.; Nouaili, E.B.; Talbi, E.; Ghdemssi, A.; Rached, C.; Bahlous, A.; Gammoudi, A.; Hamouda, S.B.; Bouguerra, B.; Bouzid, K. Prevalence of vitamin D deficiency in mothers and their newborns in a Tunisian population. Int. J. Gynecol. Obstet. 2016, 133, 192–195. [Google Scholar] [CrossRef] [PubMed]
- Blarduni, E.; Arrospide, A.; Galar, M.; Castaño, L.; Mar, J.; Group, G. Factors associated with the prevalence of hypovitaminosis D in pregnant women and their newborns. An. Pediatría 2019, 91, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Mehany, S.; Pöppelmeyer, C.; Helk, O.; Pachinger, O.; Widhalm, K. Low Vitamin D Blood Levels with Significant Differences Between the Sexes in Viennese School Children–the EDDY Study. Aktuelle Ernährungsmedizin 2017, 42, 447–451. [Google Scholar] [CrossRef]
- Zhang, J.Y.; Wang, J.; Hu, S.; Chen, D.; Lu, Q.; Wei, R.; Tan, M.; Lash, G.E. Cord serum vitamin D in a South China birth cohort. Asia Pac. J. Clin. Nutr. 2019, 28, 544–549. [Google Scholar] [PubMed]
- Bellows, A.L.; Smith, E.R.; Muhihi, A.; Briegleb, C.; Noor, R.A.; Mshamu, S.; Sudfeld, C.; Masanja, H.; Fawzi, W.W. Micronutrient Deficiencies among Breastfeeding Infants in Tanzania. Nutrients 2017, 9, 1258. [Google Scholar] [CrossRef]
- Sudfeld, C.R.; Manji, K.P.; Smith, E.R.; Aboud, S.; Kisenge, R.; Fawzi, W.W.; Duggan, C.P. Vitamin D deficiency is not associated with growth or the incidence of common morbidities among Tanzanian infants. J. Pediatric Gastroenterol. Nutr. 2017, 65, 467. [Google Scholar] [CrossRef]
- Bhimji, K.M.; Naburi, H.; Aboud, S.; Manji, K. Vitamin D Status and Associated Factors in Neonates in a Resource Constrained Setting. Int. J. Pediatrics 2018, 2018, 9614975. [Google Scholar] [CrossRef]
- Velaphi, S.C.; Izu, A.; Madhi, S.A.; Pettifor, J.M. Maternal and neonatal vitamin D status at birth in black South Africans. S. Afr. Med. J. 2019, 109, 807–813. [Google Scholar] [CrossRef] [PubMed]
- Stoutjesdijk, E.; Schaafsma, A.; Nhien, N.V.; Khor, G.L.; Kema, I.P.; Hollis, B.W.; Dijck-Brouwer, D.A.J.; Muskiet, F.A.J. Milk vitamin D in relation to the ‘adequate intake’ for 0–6-month-old infants: A study in lactating women with different cultural backgrounds, living at different latitudes. Br. J. Nutr. 2017, 118, 804–812. [Google Scholar] [CrossRef]
- Wagner, C.L.; Greer, F.R. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics 2008, 122, 1142–1152. [Google Scholar] [CrossRef] [PubMed]
- Braegger, C.; Campoy, C.; Colomb, V.; Decsi, T.; Domellof, M.; Fewtrell, M.; Hojsak, I.; Mihatsch, W.; Molgaard, C.; Shamir, R. Vitamin D in the healthy European paediatric population. J. Pediatric Gastroenterol. Nutr. 2013, 56, 692–701. [Google Scholar] [CrossRef]
- Paxton, G.A.; Teale, G.R.; Nowson, C.A.; Mason, R.S.; McGrath, J.J.; Thompson, M.J.; Siafarikas, A.; Rodda, C.P.; Munns, C.F. Vitamin D and health in pregnancy, infants, children and adolescents in Australia and New Zealand: A position statement. Med. J. Aust. 2013, 198, 142–143. [Google Scholar] [CrossRef]
- Budree, S.; Goddard, E.; Brittain, K.; Cader, S.; Myer, L.; Zar, H.J. Infant feeding practices in a South African birth cohort—A longitudinal study. Matern. Child Nutr. 2017, 13, e12371. [Google Scholar] [CrossRef]
- Faber, M.; Benadé, S. Breastfeeding, complementary feeding and nutritional status of 6–12-month-old infants in rural KwaZulu-Natal. S. Afr. J. Clin. Nutr. 2007, 20, 16–24. [Google Scholar]
- Zar, H.J.; Barnett, W.; Myer, L.; Stein, D.J.; Nicol, M.P. Investigating the early-life determinants of illness in Africa: The Drakenstein Child Health Study. Thorax 2015, 70, 592–594. [Google Scholar] [CrossRef]
- Zar, H.J.; Pellowski, J.A.; Cohen, S.; Barnett, W.; Vanker, A.; Koen, N.; Stein, D.J. Maternal health and birth outcomes in a South African birth cohort study. PLoS ONE 2019, 14, e0222399. [Google Scholar] [CrossRef]
- Snellman, G.; Melhus, H.; Gedeborg, R.; Byberg, L.; Berglund, L.; Wernroth, L.; Michaelsson, K. Determining vitamin D status: A comparison between commercially available assays. PLoS ONE 2010, 5, e11555. [Google Scholar] [CrossRef]
- Hollis, B.W. Measuring 25-hydroxyvitamin D in a clinical environment: Challenges and needs. Am. J. Clin. Nutr. 2008, 88, 507S–510S. [Google Scholar] [CrossRef]
- Saggese, G.; Vierucci, F.; Boot, A.M.; Czech-Kowalska, J.; Weber, G.; Camargo, C.A.; Mallet, E.; Fanos, M.; Shaw, N.J.; Holick, M.F. Vitamin D in childhood and adolescence: An expert position statement. Eur. J. Pediatrics 2015, 174, 565–576. [Google Scholar] [CrossRef] [PubMed]
- Tobin, J. Estimation of relationships for limited dependent variables. Econom. J. Econom. Soc. 1958, 26, 24–36. [Google Scholar] [CrossRef]
- Mokhtar, R.R.; Holick, M.F.; Sempértegui, F.; Griffiths, J.K.; Estrella, B.; Moore, L.L.; Fox, M.P.; Hamer, D.H. Vitamin D status is associated with underweight and stunting in children aged 6–36 months residing in the Ecuadorian Andes. Public Health Nutr. 2018, 21, 1974–1985. [Google Scholar] [CrossRef]
- Keller, A.; Händel, M.N.; Frederiksen, P.; Jacobsen, R.; Cohen, A.S.; McGrath, J.J.; Heitmann, B.L. Concentration of 25-hydroxyvitamin D from neonatal dried blood spots and the relation to gestational age, birth weight and Ponderal Index: The D-tect study. Br. J. Nutr. 2018, 119, 1416–1423. [Google Scholar] [CrossRef] [PubMed]
- Kassab, M.; Shaban, I.; Mohammad, K.; Creedy, D.K. Prevalence of hypovitaminosis D among jordanian healthy infants: A descriptive cross sectional study. J. Pediatric Nurs. 2016, 31, e119–e125. [Google Scholar] [CrossRef]
- Poopedi, M.A.; Norris, S.A.; Pettifor, J.M. Factors influencing the vitamin D status of 10-year-old urban South African children. Public Health Nutr. 2011, 14, 334–339. [Google Scholar] [CrossRef] [PubMed]
- Challa, A.; Ntourntoufi, A.; Cholevas, V.; Bitsori, M.; Galanakis, E.; Andronikou, S. Breastfeeding and vitamin D status in Greece during the first 6 months of life. European J. Pediatrics 2005, 164, 724–729. [Google Scholar] [CrossRef]
- Darmawikarta, D.; Chen, Y.; Lebovic, G.; Birken, C.S.; Parkin, P.C.; Maguire, J.L. Total duration of breastfeeding, vitamin D supplementation, and serum levels of 25-hydroxyvitamin D. Am. J. Public Health 2016, 106, 714–719. [Google Scholar] [CrossRef]

| Variables | Mbekweni (n = 411) | TC Newman (n = 363) | p-Value | Total (n = 774) |
|---|---|---|---|---|
| Maternal characteristics | ||||
| Median Age, years (IQR) | 27 (23–32) | 25 (21–29) | <0.001 | 26 (22–31) |
| Age group, years | ||||
| <20 | 36 (8.8) | 53 (14.6) | 89 (11.5) | |
| 20–24 | 122 (29.7) | 131 (36.1) | <0.001 | 253 (32.7) |
| 25–29 | 108 (26.3) | 101 (27.8) | 209 (27.0) | |
| ≥30 | 145 (35.3) | 78 (21.5) | 223 (28.8) | |
| Parity | ||||
| 0 | 137 (33.3) | 152 (41.9) | 289 (37.3) | |
| 1 | 162 (39.4) | 122 (33.6) | 0.048 | 284 (36.7) |
| ≥2 | 112 (27.3) | 89 (24.5) | 201 (26.0) | |
| Education | ||||
| Primary | 32 (7.8) | 26 (7.2) | 58 (7.5) | |
| Some Secondary | 227 (55.2) | 186 (51.2) | 0.296 | 413 (53.4) |
| Completed Secondary | 124 (30.2) | 132 (36.4) | 256 (33.1) | |
| Some Tertiary | 28 (6.8) | 19 (5.2) | 47 (6.1) | |
| HIV positive | 157 (38.2) | 9 (2.5) | <0.001 | 166 (21.4) |
| Smoking in pregnancy | 20 (4.9) | 162 (44.6) | <0.001 | 182 (23.5) |
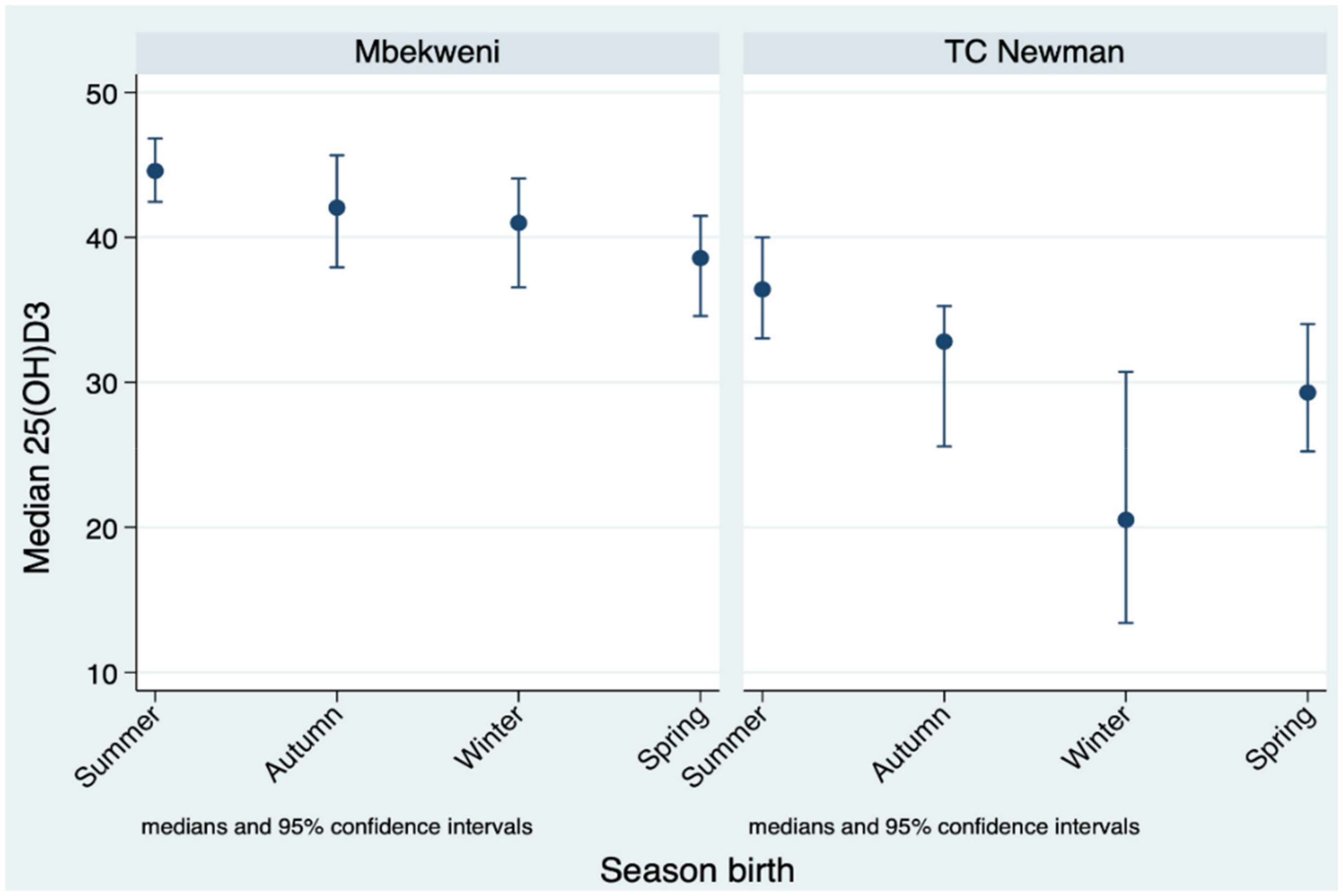
| Season birth | ||||
| Summer (Dec–Feb) | 123 (29.9) | 97 (26.7) | 220 (28.4) | |
| Autumn (Mar–May) | 100 (24.3) | 95 (26.2) | 0.539 | 195 (25.2) |
| Winter (June–Aug) | 104 (25.3) | 85 (32.4) | 189 (24.4) | |
| Spring (Sept–Nov) | 84 (20.4) | 86 (23.7) | 170 (22.0) | |
| Socioeconomic Status | ||||
| Lowest | 124 (30.2) | 60 (16.5) | 184 (23.8) | |
| Moderate Low | 108 (26.3) | 87 (24.0) | <0.001 | 195 (25.2) |
| Moderate high | 98 (23.8) | 100 (27.5) | 198 (25.6) | |
| High | 81 (19.7) | 116 (34.0) | 197 (25.4) | |
| Infant characteristics | ||||
| Weight-for-age z score | −0.16 (−0.92 to 0.51) | −0.63 (−1.30 to 0.06) | <0.001 | −0.39 (−1.15 to 0.33) |
| Height-for-age z score | −0.72 (−1.63 to −0.16) | −0.97 (−1.89 to −0.17) | 0.002 | −0.83 (−1.75 to −0.01) |
| Female | 206 (50.1) | 160 (44.1) | 0.093 | 366 (47.3) |
| Prematurity (<37 weeks) | 55 (13.4) | 43 (11.8) | 0.521 | 98 (12.7) |
| Breastfeeding initiated | 356 (86.6) | 362 (99.7) | <0.001 | 718 (92.8) |
| Vitamin D status | ||||
| 25(OH)D3 | ||||
| Mean 25(OH)D3 (SD) | 41.2 (15.3) | 31.0 (17.2) | <0.001 | 36.4 (17.0) |
| Median 25(OH)D3 (IQR) | 41.8 (32.8–49.9) | 32.1 (18.2–42.1) | <0.001 | 37.4 (25.8–47.3) |
| Sufficient 25(OH)D3 (≥75 nmol/L) | 9 (2.2) | 5 (1.4) | <0.001 | 14 (1.8) |
| Insufficient 25(OH)D3 (50–74 nmol/L) | 92 (22.4) | 44 (12.1) | 136 (17.6) | |
| Deficient 25(OH)D3 (<50 nmol/L) | 310 (76.4) | 314 (86.5) | 624 (80.6) | |
| 3-epi-25(OH)D3 | ||||
| Mean 3-epi-25(OH)D3 (SD) | 4.6 (3.5) | 4.4 (3.9) | 0.550 | 4.5 (3.7) |
| Median 3-epi-25(OH)D3 (IQR) | 3.9 (1.5–6.2) | 3.5 (1.5–5.8) | 0.550 | 3.7 (1.5–6.1) |
| Variables | Mbekweni | TC Newman | Overall | |||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | Coefficient | 95% CI | Coefficient | 95% CI | |
| Maternal characteristics | ||||||
| Smoker | 0.14 | −6.64 to 6.92 | −1.32 | −4.93 to 2.30 | −1.05 | −4.09 to 1.99 |
| Season birth | ||||||
| Summer (December–February) | 1 | Ref | 1 | Ref | 1 | Ref |
| Autumn (Mar–May) | −4.77 | −8.71 to −0.83 | −6.52 | −11.33 to −1.71 | −5.54 | −8.61 to −2.48 |
| Winter (June–August) | −6.43 | −10.32 to −2.53 | −12.51 | −17.44 to −7.58 | −9.29 | −12.37 to −6.21 |
| Spring (September–November) | −7.53 | −11.65 to −3.41 | −5.94 | −10.89 to −1.00 | −6.70 | −9.88 to −3.53 |
| Socioeconomic status | ||||||
| Lowest | 1 | Ref | 1 | Ref | 1 | Ref |
| Moderate Low | −2.80 | −6.72 to 1.12 | −0.13 | −5.71 to 5.45 | −1.87 | −5.09 to 1.35 |
| Moderate high | −3.89 | −7.73 to −0.06 | 0.87 | −4.72 to 6.47 | −1.89 | −5.08 to 1.31 |
| High | −2.08 | −6.23 to 2.07 | −2.09 | −7.55 to 3.37 | −2.80 | −6.05 to 0.45 |
| Infant characteristics | ||||||
| Male sex | −3.77 | −6.68 to −0.87 | −1.92 | −5.48 to 1.65 | −3.01 | −5.27 to −0.75 |
| Study Site | ||||||
| Mbekweni | … | … | … | … | 1 | Ref |
| TC Newman | … | … | … | … | −8.57 | −11.41 to −5.74 |
| WAZ at 6 weeks of age * | 1.28 | −0.04 to 2.61 | 0.89 | −0.86 to 2.64 | 1.09 | 0.03 to 2.16 |
| HIV exposure | −1.88 | −5.27 to 1.52 | −12.49 | −24.28 to −0.71 | −2.82 | −6.23 to 0.59 |
| Breastfeeding initiated | −9.17 | −14.02 to −4.31 | −13.66 | −48.91 to 21.59 | −9.75 | −14.79 to −4.71 |
| Adjusted Odds Ratio(95% CI), p-Value † | |||
|---|---|---|---|
| Vitamin D Deficiency | |||
| Not breastfed | 1 | Referent | … |
| Breastfed | 1.96 | 1.04–3.67 | 0.036 |
| Not breastfed ‡ | 1 | Referent | … |
| Breastfed < 1 month | 2.26 | 1.03–4.93 | 0.041 |
| Breastfed ≥ 1 months | 5.40 | 2.37–12.32 | <0.0001 |
| Adjusted Coefficient (95% CI), p-Value † | |||
| Vitamin D concentration, nmol/L | |||
| Not breastfed | 1 | Referent | … |
| Breastfed | −9.74 | −14.72, −4.76 | <0.0001 |
| Not breastfed ‡ | 1 | Referent | … |
| Breastfed < 1 month | −4.91 | −9.68, −0.15 | 0.043 |
| Breastfed ≥ 1 months | −16.22 | −21.06, −11.39 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ncayiyana, J.R.; Martinez, L.; Goddard, E.; Myer, L.; Zar, H.J. Prevalence and Correlates of Vitamin D Deficiency among Young South African Infants: A Birth Cohort Study. Nutrients 2021, 13, 1500. https://doi.org/10.3390/nu13051500
Ncayiyana JR, Martinez L, Goddard E, Myer L, Zar HJ. Prevalence and Correlates of Vitamin D Deficiency among Young South African Infants: A Birth Cohort Study. Nutrients. 2021; 13(5):1500. https://doi.org/10.3390/nu13051500
Chicago/Turabian StyleNcayiyana, Jabulani R., Leonardo Martinez, Elizabeth Goddard, Landon Myer, and Heather J. Zar. 2021. "Prevalence and Correlates of Vitamin D Deficiency among Young South African Infants: A Birth Cohort Study" Nutrients 13, no. 5: 1500. https://doi.org/10.3390/nu13051500
APA StyleNcayiyana, J. R., Martinez, L., Goddard, E., Myer, L., & Zar, H. J. (2021). Prevalence and Correlates of Vitamin D Deficiency among Young South African Infants: A Birth Cohort Study. Nutrients, 13(5), 1500. https://doi.org/10.3390/nu13051500






