Exclusive Breastfeeding Is Not Associated with Maternal–Infant Bonding in Early Postpartum, Considering Depression, Anxiety, and Parity
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Participants
2.3. Measurements
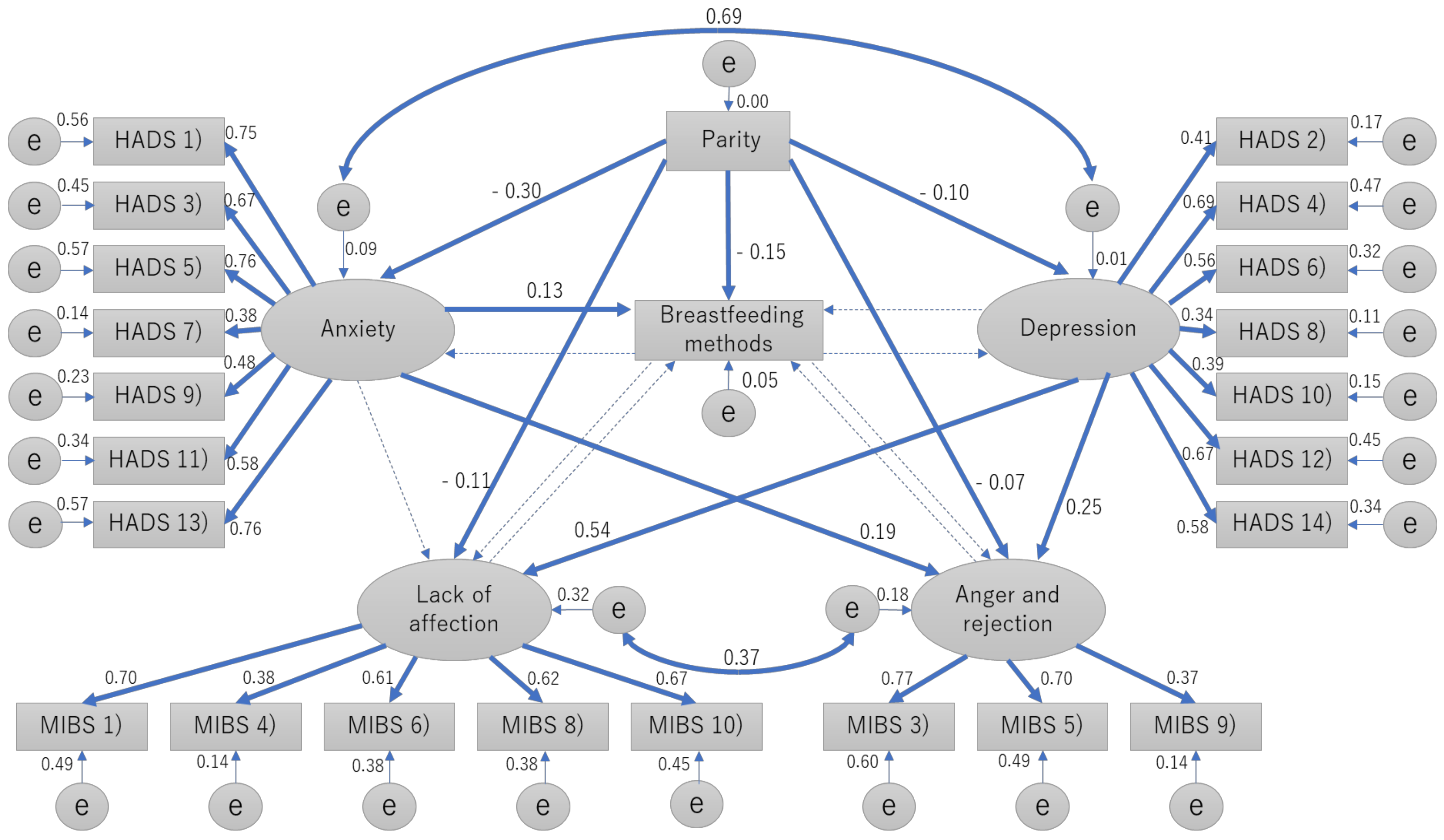
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statements
Acknowledgments
Conflicts of Interest
References
- Kennell, J.H.; Klaus, M.H. Mother-infant bonding: Weighing the evidence. Dev. Rev. 1984, 4, 275–282. [Google Scholar] [CrossRef]
- Fergusson, D.M.; Woodward, L.J. Breast feeding and later psychosocial adjustment. Paediatr. Perinat. Epidemiol. 1999, 13, 144–157. [Google Scholar] [CrossRef]
- World Health Organization. Counselling for Maternal and Newborn Health Care: A handbook for Building Skills: World Health Organization. 2010. Available online: http://bit.ly/2rd1wkS (accessed on 30 August 2015).
- Cernadas, J.M.C.; Noceda, G.; Barrera, L.; Martinez, A.M.; Garsd, A. Maternal and perinatal factors influencing the duration of exclusive breastfeeding during the first 6 months of life. J. Hum. Lact. 2003, 19, 136–144. [Google Scholar] [CrossRef]
- Else-Quest, N.M.; Hyde, J.S.; Clark, R. Breastfeeding, bonding, and the motherinfant relationship. Merrill Palmer. Q. 2003, 49, 495–517. [Google Scholar] [CrossRef]
- Nishioka, E.; Haruna, M.; Ota, E.; Matsuzaki, M.; Murayama, R.; Yoshimura, K.; Murashima, S. A prospective study of the relationship between breastfeeding and postpartum depressive symptoms appearing at 1-5 months after delivery. J. Affect. Disord. 2011, 133, 553–559. [Google Scholar] [CrossRef]
- Motegi, T.; Watanabe, Y.; Fukui, N.; Ogawa, M.; Hashijiri, K.; Tsuboya, R.; Sugai., T.; Egawa, J.; Mitome, S.; Araki, R.; et al. Depression, anxiety and primiparity are negatively associated with mother–infant bonding in Japanese mothers. Neuropsychiatr. Dis. Treat. 2020, 16, 3117–3122. [Google Scholar] [CrossRef]
- Figueiredo, B.; Canário, C.; Field, T. Breastfeeding is negatively affected by prenatal depression and reduces postpartum depression. Psychol. Med. 2014, 44, 927–936. [Google Scholar] [CrossRef] [PubMed]
- Ystrom, E. Breastfeeding cessation and symptoms of anxiety and depression: A longitudinal cohort study. BMC Pregnancy Childbirth 2012, 12, 36. [Google Scholar] [CrossRef] [PubMed]
- Fallon, V.; Groves, R.; Halford, J.C.; Bennett, K.M.; Harrold, J.A. Postpartum anxiety and infant-feeding outcomes. J. Hum. Lact. 2016, 32, 740–758. [Google Scholar] [CrossRef] [PubMed]
- Vieira, E.S.; Caldeira, N.T.; Eugênio, D.S.; Lucca, M.M.D.; Silva, I.A. Breastfeeding self-efficacy and postpartum depression: A cohort study. Rev. Lat. Am. Enfermagem. 2018, 6, e3035. [Google Scholar] [CrossRef]
- Motegi, T.; Fukui, N.; Hashijiri, K.; Tsuboya, R.; Sugai, T.; Egawa, J.; Mitome, S.; Araki, R.; Haino, K.; Yamaguchi, M.; et al. Identifying the factor structure of the Mother-to-Infant Bonding Scale for post-partum women and examining its consistency during pregnancy. Psychiatry Clin. Neurosci. 2019, 73, 661–662. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, M.; Watanabe, Y.; Motegi, T.; Fukui, N.; Hashijiri, K.; Tsuboya, R.; Sugai, T.; Egawa, J.; Araki, R.; Haino, K.; et al. Factor Structure and Measurement Invariance of the Hospital Anxiety and Depression Scale Across the Peripartum Period Among Pregnant Japanese Women. Neuropsychiatr. Dis. Treat. 2020, 26, 221–227. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Kitamura, T. Hospital anxiety and depression scale. Arch. Psychiatr. Diagn. Clin. Eval. 1993, 4, 371–372. (In Japanese) [Google Scholar]
- Kumar, R.C. “Anybody’s child”: Severe disorders of mother-to-infant bonding. Br. J. Psychiatry 1997, 171, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Taylor, A.; Atkins, R.; Kumar, R.; Adams, D.; Glover, V. A new Mother-to-Infant Bonding Scale: Links with early maternal mood. Arch. Womens Ment. Health 2005, 8, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, K.; Yamashita, H.; Conroy, S.; Marks, M.; Kumar, C. A Japanese version of Mother-to-Infant Bonding Scale: Factor structure, longitudinal changes and links with maternal mood during the early postnatal period in Japanese mothers. Arch. Womens Ment. Health 2012, 15, 343–352. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Mode. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- American Psychiatric Association, DSM-5 Task Force. Diagnostic and Statistical Manual of Mental Disorders: DSM-5TH, 5th ed.; American Psychiatric Publishing, Inc: Arlington, VA, USA, 2013. [Google Scholar]
- Gjerdingen, D.; Crow, S.; McGovern, P.; Miner, M.; Center, B. Changes in depressive symptoms over 0-9 months postpartum. J. Womens Health Larchmt. 2011, 20, 381–386. [Google Scholar] [CrossRef]
- Hairston, I.S.; Handelzalts, J.E.; Lehman-Inbar, T.; Kovo, M. Mother-infant bonding is not associated with feeding type: A community study sample. BMC Pregnancy Childbirth 2019, 19, 125. [Google Scholar] [CrossRef] [PubMed]
- Minamida, T.; Iseki, A.; Sakai, H.; Imura, M.; Okano, T.; Tanii, H. Do postpartum anxiety and breastfeeding self-efficacy and bonding at early postpartum predict postpartum depression and the breastfeeding method? Infant. Ment. Health J. 2020, 41, 662–676. [Google Scholar] [CrossRef]
- Cox, E.Q.; Stuebe, A.; Pearson, B.; Grewen, K.; Rubinow, D.; Meltzer-Brody, S. Oxytocin and HPA stress axis reactivity in postpartum women. Psychoneuroendocrinology 2015, 55, 164–172. [Google Scholar] [CrossRef] [PubMed]
- Stuebe, A.M.; Grewen, K.; Meltzer-Brody, S. Association between maternal mood and oxytocin response to breastfeeding. J. Womens Health Larchmt. 2013, 22, 352–361. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, R.M. Attachment figure’s regulation of infant brain and behavior. Psychodyn. Psychiatry 2017, 45, 475–498. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Oras., P.; Ljungberg, T.; Hellström-Westas, L.; Funkquist, E.L. A breastfeeding support program changed breastfeeding patterns but did not affect the mothers’ self-efficacy in breastfeeding at two months. Early. Hum. Dev. 2020, 151, 105242. [Google Scholar] [CrossRef] [PubMed]
- Bell, A.F.; Erickson, E.N.; Carter, C.S. Beyond labor: The role of natural and synthetic oxytocin in the transition to motherhood. J. Midwifery Womens Health 2014, 59, 35–42. [Google Scholar] [CrossRef]
| Exclusive Group | Mixed Group | Formula-Feeding Group | Statistics | |
|---|---|---|---|---|
| Number | n = 1029 | n = 945 | n = 46 | |
| Parity | ||||
| Primipara | n = 385 (41.1%) # | n = 529 (56.5%) # | n = 23 (2.5%) | |
| Multipara | n = 644 (59.5%) # | n = 416 (38.4%) # | n = 23 (2.1%) | χ2 = 68.5, p < 0.001 * |
| Age (year) | 31.9 ± 4.76 | 31.2 ± 4.80 | 32.4 ± 4.75 | F = 4.46, p = 0.012 |
| HADS score (point) | ||||
| Total | 10.79 ± 5.93 | 12.67 ± 6.68 a | 13.54 ± 7.56 b | F = 23.7, p < 0.001 * |
| Anxiety | 4.92 ± 3.60 | 6.08 ± 4.07 c | 6.57 ± 4.25 d | F = 24.1, p < 0.001 * |
| Depression | 5.87 ± 3.16 | 6.59 ± 3.44 e | 6.98 ± 3.83 | F = 13.1, p < 0.001 * |
| MIBS score (point) | ||||
| Total | 1.85 ± 2.21 | 2.63 ± 2.74 f | 2.80 ± 3.22 g | F = 25.5, p < 0.001 * |
| Lack of affection | 0.73 ± 1.09 | 1.02 ± 1.30 h | 1.13 ± 1.44 | F = 15.4, p < 0.001 * |
| Anger and rejection | 0.31 ± 0.73 | 0.46 ± 0.94 i | 0.54 ± 0.96 | F = 8.59, p < 0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fukui, N.; Motegi, T.; Watanabe, Y.; Hashijiri, K.; Tsuboya, R.; Ogawa, M.; Sugai, T.; Egawa, J.; Enomoto, T.; Someya, T. Exclusive Breastfeeding Is Not Associated with Maternal–Infant Bonding in Early Postpartum, Considering Depression, Anxiety, and Parity. Nutrients 2021, 13, 1184. https://doi.org/10.3390/nu13041184
Fukui N, Motegi T, Watanabe Y, Hashijiri K, Tsuboya R, Ogawa M, Sugai T, Egawa J, Enomoto T, Someya T. Exclusive Breastfeeding Is Not Associated with Maternal–Infant Bonding in Early Postpartum, Considering Depression, Anxiety, and Parity. Nutrients. 2021; 13(4):1184. https://doi.org/10.3390/nu13041184
Chicago/Turabian StyleFukui, Naoki, Takaharu Motegi, Yuichiro Watanabe, Koyo Hashijiri, Ryusuke Tsuboya, Maki Ogawa, Takuro Sugai, Jun Egawa, Takayuki Enomoto, and Toshiyuki Someya. 2021. "Exclusive Breastfeeding Is Not Associated with Maternal–Infant Bonding in Early Postpartum, Considering Depression, Anxiety, and Parity" Nutrients 13, no. 4: 1184. https://doi.org/10.3390/nu13041184
APA StyleFukui, N., Motegi, T., Watanabe, Y., Hashijiri, K., Tsuboya, R., Ogawa, M., Sugai, T., Egawa, J., Enomoto, T., & Someya, T. (2021). Exclusive Breastfeeding Is Not Associated with Maternal–Infant Bonding in Early Postpartum, Considering Depression, Anxiety, and Parity. Nutrients, 13(4), 1184. https://doi.org/10.3390/nu13041184





