Compound Sarcopenia in Hospitalized Patients with Cirrhosis Worsens Outcomes with Increasing Age
Abstract
1. Introduction
2. Materials and Methods
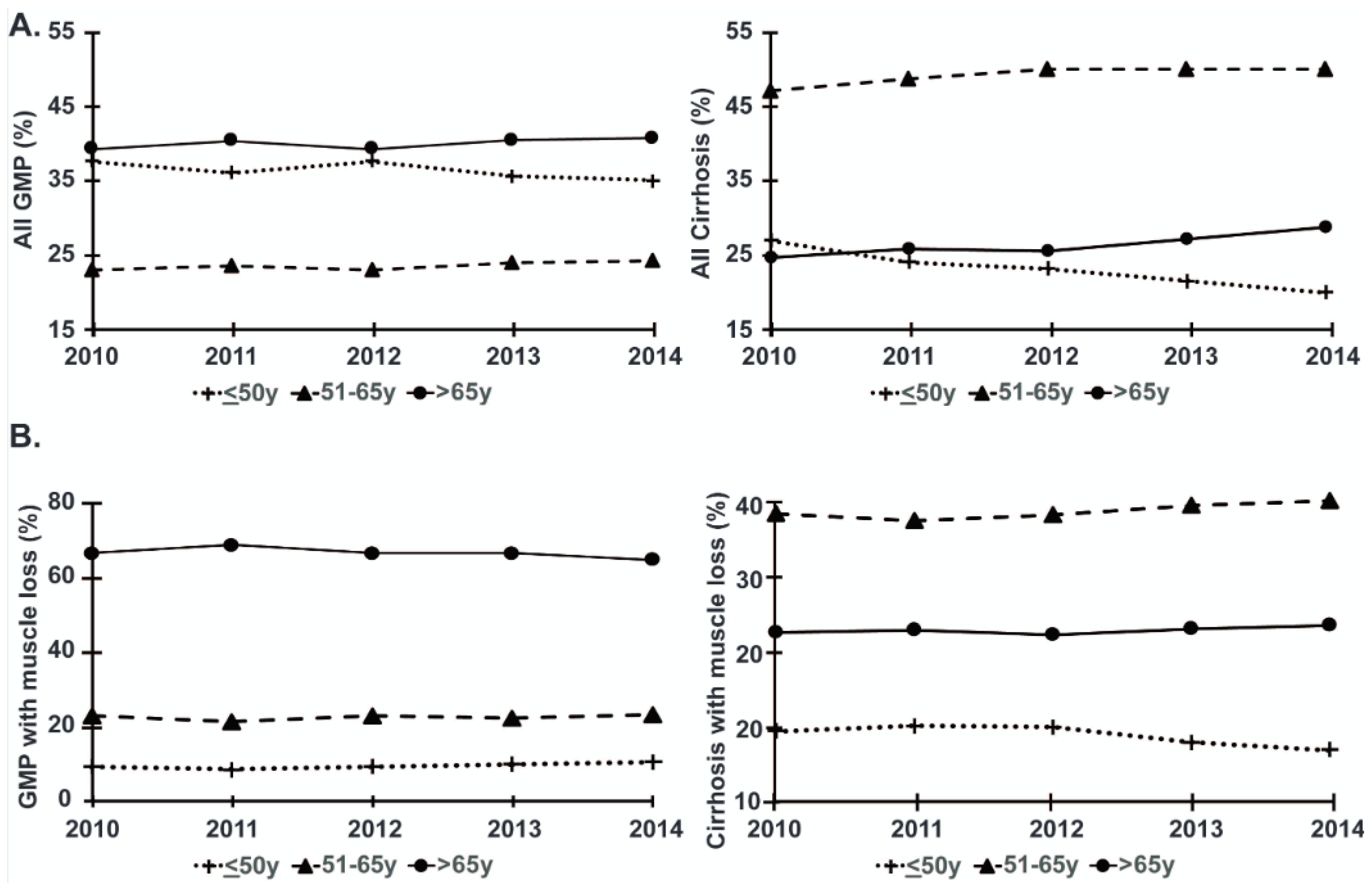
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ortman, J.M.; Velkoff, V.A.; Hogan, H. An Aging Nation: The Older Population in the United States; Current Population Reports P25-1140; U.S. Census Bureau: Washington, DC, USA, 2014. [Google Scholar]
- Kim, D.; Li, A.A.; Perumpail, B.J.; Gadiparthi, C.; Kim, W.; Cholankeril, G.; Glenn, J.S.; Harrison, S.A.; Younossi, Z.M.; Ahmed, A. Changing Trends in Etiology-Based and Ethnicity-Based Annual Mortality Rates of Cirrhosis and Hepatocellular Carcinoma in the United States. Hepatology 2019, 69, 1064–1074. [Google Scholar] [CrossRef]
- Antunes, A.C.; Araújo, D.A.; Veríssimo, M.T.; Amaral, T.F. Sarcopenia and hospitalisation costs in older adults: A cross-sectional study. Nutr. Diet. 2017, 74, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Hazra, N.C.; Rudisill, C.; Gulliford, M.C. Determinants of health care costs in the senior elderly: Age, comorbidity, impairment, or proximity to death? Eur. J. Health Econ. 2018, 19, 831–842. [Google Scholar] [CrossRef]
- van Vugt, J.L.A.; Buettner, S.; Alferink, L.J.M.; Bossche, N.; de Bruin, R.W.F.; Darwish Murad, S.; Polak, W.G.; Metselaar, H.J.; IJzermans, J.N.M. Low skeletal muscle mass is associated with increased hospital costs in patients with cirrhosis listed for liver transplantation-a retrospective study. Transpl. Int. 2018, 31, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Collaborators GBDC. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2020, 5, 245–266. [Google Scholar] [CrossRef]
- Kamimura, K.; Sakamaki, A.; Kamimura, H.; Setsu, T.; Yokoo, T.; Takamura, M.; Terai, S. Considerations of elderly factors to manage the complication of liver cirrhosis in elderly patients. World J. Gastroenterol. 2019, 25, 1817–1827. [Google Scholar] [CrossRef]
- Durand, F.; Levitsky, J.; Cauchy, F.; Gilgenkrantz, H.; Soubrane, O.; Francoz, C. Age and liver transplantation. J. Hepatol. 2019, 70, 745–758. [Google Scholar] [CrossRef] [PubMed]
- Kim, I.H.; Kisseleva, T.; Brenner, D.A. Aging and liver disease. Curr. Opin. Gastroenterol. 2015, 31, 184–191. [Google Scholar] [CrossRef]
- Mooney, H.; Roberts, R.; Cooksley, W.G.; Halliday, J.W.; Powell, L.W. Alterations in the liver with ageing. Clin. Gastroenterol. 1985, 14, 757–771. [Google Scholar]
- Premoli, A.; Paschetta, E.; Hvalryg, M.; Spandre, M.; Bo, S.; Durazzo, M. Characteristics of liver diseases in the elderly: A review. Minerva Gastroenterol. Dietol. 2009, 55, 71–78. [Google Scholar]
- Dasarathy, S. Cause and management of muscle wasting in chronic liver disease. Curr. Opin. Gastroenterol. 2016, 32, 159–165. [Google Scholar] [CrossRef]
- Dasarathy, S. Posttransplant Sarcopenia: An Underrecognized Early Consequence of Liver Transplantation. Dig. Dis. Sci. 2013, 58, 3103–3111. [Google Scholar] [CrossRef] [PubMed]
- Dasarathy, S. Consilience in sarcopenia of cirrhosis. J. Cachexia Sarcopenia Muscle 2012, 3, 225–237. [Google Scholar] [CrossRef] [PubMed]
- Periyalwar, P.; Dasarathy, S. Malnutrition in Cirrhosis: Contribution and Consequences of Sarcopenia on Metabolic and Clinical Responses. Clin. Liver Dis. 2012, 16, 95–131. [Google Scholar] [CrossRef]
- Vural, A.; Attaway, A.; Welch, N.; Zein, J.; Dasarathy, S. Skeletal muscle loss phenotype in cirrhosis: A nationwide analysis of hospitalized patients. Clin. Nutr. 2020, 39, 3711–3720. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef]
- Welch, C.; Hassan-Smith, Z.K.; Greig, C.A.; Lord, J.M.; Jackson, T.A. Acute Sarcopenia Secondary to Hospitalisation—An Emerging Condition Affecting Older Adults. Aging Dis. 2018, 9, 151–164. [Google Scholar] [CrossRef]
- English, K.L.; Paddon-Jones, D. Protecting muscle mass and function in older adults during bed rest. Curr. Opin. Clin. Nutr. Metab. Care 2010, 13, 34–39. [Google Scholar] [CrossRef]
- Kortebein, P.; Ferrando, A.; Lombeida, J.; Wolfe, R.; Evans, W.J. Effect of 10 Days of Bed Rest on Skeletal Muscle in Healthy Older Adults. JAMA 2007, 297, 1769–1774. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. International Classification of Diseases, Clinical Modifications (ICD-9-CM), 6th ed.; DHHS Publication No. (PHS) 96-1260; Health Care Financing Administration: Washington, DC, USA, 1997. [Google Scholar]
- Fox, K.M.; Brooks, J.M.; Gandra, S.R.; Markus, R.; Chiou, C.F. Estimation of Cachexia among Cancer Patients Based on Four Definitions. J. Oncol. 2009, 2009, 693458. [Google Scholar] [CrossRef]
- Attaway, A.H.; Welch, N.; Hatipoğlu, U.; Zein, J.G.; Dasarathy, S. Muscle loss contributes to higher morbidity and mortality in COPD: An analysis of national trends. Respirology 2021, 26, 62–71. [Google Scholar] [CrossRef]
- Covinsky, K.E.; Palmer, R.M.; Fortinsky, R.H.; Counsell, S.R.; Stewart, A.L.; Rn, D.K.; Ma, C.J.B.; Landefeld, C.S. Loss of Independence in Activities of Daily Living in Older Adults Hospitalized with Medical Illnesses: Increased Vulnerability with Age. J. Am. Geriatr. Soc. 2003, 51, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Sam, J.; Nguyen, G.C. Protein-calorie malnutrition as a prognostic indicator of mortality among patients hospitalized with cirrhosis and portal hypertension. Liver Int. 2009, 29, 1396–1402. [Google Scholar] [CrossRef]
- Menendez, M.E.; Neuhaus, V.; Van Dijk, N.C.; Ring, D. The Elixhauser Comorbidity Method Outperforms the Charlson Index in Predicting Inpatient Death After Orthopaedic Surgery. Clin. Orthop. Relat. Res. 2014, 472, 2878–2886. [Google Scholar] [CrossRef]
- Little, J.; Higgins, J.P.; Ioannidis, J.P.; Moher, D.; Gagnon, F.; Von Elm, E.; Khoury, M.J.; Cohen, B.; Davey-Smith, G.; Grimshaw, J.M.; et al. STrengthening the REporting of Genetic Association Studies (STREGA): An Extension of the STROBE Statement. Ann. Intern. Med. 2009, 150, 206–215. [Google Scholar] [CrossRef]
- Bell, B.P.; Manos, M.M.; Zaman, A.; Terrault, N.; Thomas, A.; Navarro, V.J.; Dhotre, K.B.; Murphy, R.C.; Van Ness, G.R.; Stabach, N.; et al. The Epidemiology of Newly Diagnosed Chronic Liver Disease in Gastroenterology Practices in the United States: Results from Population-Based Surveillance. Am. J. Gastroenterol. 2008, 103, 2727–2736. [Google Scholar] [CrossRef]
- Orman, E.S.; Roberts, A.; Ghabril, M.; Nephew, L.; Desai, A.P.; Patidar, K.; Chalasani, N. Trends in Characteristics, Mortality, and Other Outcomes of Patients with Newly Diagnosed Cirrhosis. JAMA Netw. Open 2019, 2, e196412. [Google Scholar] [CrossRef] [PubMed]
- Aduen, J.F.; Sujay, B.; Dickson, R.C.; Heckman, M.G.; Hewitt, W.R.; Stapelfeldt, W.H.; Steers, J.L.; Harnois, D.M.; Kramer, D.J. Outcomes after liver transplant in patients aged 70 years or older compared with those younger than 60 years. Mayo Clin. Proc. 2009, 84, 973–978. [Google Scholar] [CrossRef]
- Parrish, N.F.; Feurer, I.D.; Matsuoka, L.K.; Rega, S.A.; Perri, R.; Alexopoulos, S.P. The Changing Face of Liver Transplantation in the United States: The Effect of HCV Antiviral Eras on Transplantation Trends and Outcomes. Transplant. Direct 2019, 5, e427. [Google Scholar] [CrossRef] [PubMed]
- Su, F.; Yu, L.; Berry, K.; Liou, I.W.; Landis, C.S.; Rayhill, S.C.; Reyes, J.D.; Ioannou, G.N. Aging of Liver Transplant Registrants and Recipients: Trends and Impact on Waitlist Outcomes, Post-Transplantation Outcomes, and Transplant-Related Survival Benefit. Gastroenterology 2016, 150, 441–453.e6. [Google Scholar] [CrossRef]
- Wong, R.J.; Singal, A.K. Trends in Liver Disease Etiology Among Adults Awaiting Liver Transplantation in the United States, 2014–2019. JAMA Netw. Open 2020, 3, e1920294. [Google Scholar] [CrossRef] [PubMed]
- Haugen, C.E.; McAdams-DeMarco, M.; Holscher, C.M.; Ying, H.; Gurakar, A.O.; Garonzik-Wang, J.; Cameron, A.M.; Segev, D.L.; Lai, J.C. Multicenter Study of Age, Frailty, and Waitlist Mortality Among Liver Transplant Candidates. Ann. Surg. 2020, 271, 1132–1136. [Google Scholar] [CrossRef]
- Sharpton, S.R.; Feng, S.; Hameed, B.; Yao, F.; Lai, J.C. Combined effects of recipient age and model for end-stage liver disease score on liver transplantation outcomes. Transplantation 2014, 98, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Van Wagner, L.B.; Harinstein, M.E.; Runo, J.R.; Darling, C.; Serper, M.; Hall, S.; Kobashigawa, J.A.; Hammel, L.L. Multidisciplinary approach to cardiac and pulmonary vascular disease risk assessment in liver transplantation: An evaluation of the evidence and consensus recommendations. Am. J. Transplant. 2018, 18, 30–42. [Google Scholar] [CrossRef]
- Watt, K.D.; Pedersen, R.A.; Kremers, W.K.; Heimbach, J.K.; Charlton, M.R. Evolution of Causes and Risk Factors for Mortality Post-Liver Transplant: Results of the NIDDK Long-Term Follow-Up Study. Arab. Archaeol. Epigr. 2010, 10, 1420–1427. [Google Scholar] [CrossRef]
- Dellon, E.S.; Galanko, J.A.; Medapalli, R.K.; Russo, M.W. Impact of Dialysis and Older Age on Survival after Liver Transplantation. Am. J. Transplant. 2006, 6, 2183–2190. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.W.; Feng, S.; Covinsky, K.E.; Hayssen, H.; Zhou, L.Q.; Yeh, B.M.; Lai, J.C. A Comparison of Muscle Function, Mass, and Quality in Liver Transplant Candidates: Results from the Functional Assessment in Liver Transplantation Study. Transplantation 2016, 100, 1692–1698. [Google Scholar] [CrossRef]
- Tapper, E.B.; Finkelstein, D.; Mittleman, M.A.; Piatkowski, G.; Lai, M. Standard assessments of frailty are validated predictors of mortality in hospitalized patients with cirrhosis. Hepatology 2015, 62, 584–590. [Google Scholar] [CrossRef]
- Marineo, G.; Marotta, F.; Sisti, G. Cirrhosis Progression as a Model of Accelerated Senescence: Affecting the Biological Aging Clock by a Breakthrough Biophysical Methodology. Ann. N. Y. Acad. Sci. 2004, 1019, 572–576. [Google Scholar] [CrossRef] [PubMed]
- Aravinthan, A.D.; Alexander, G.J. Senescence in chronic liver disease: Is the future in aging? J. Hepatol. 2016, 65, 825–834. [Google Scholar] [CrossRef] [PubMed]
- McDaniel, J.G.; Davuluri, G.; Hill, E.A.; Moyer, M.; Runkana, A.; Prayson, R.; Van Lunteren, E.; Dasarathy, S. Hyperammonemia results in reduced muscle function independent of muscle mass. Am. J. Physiol. Gastrointest. Liver Physiol. 2016, 310, G163–G170. [Google Scholar] [CrossRef] [PubMed]
- Davuluri, G.; Allawy, A.; Thapaliya, S.; Rennison, J.H.; Singh, D.; Kumar, A.; Sandlers, Y.; Van Wagoner, D.R.; Flask, C.A.; Hoppel, C.; et al. Hyperammonaemia-induced skeletal muscle mitochondrial dysfunction results in cataplerosis and oxidative stress. J. Physiol. 2016, 594, 7341–7360. [Google Scholar] [CrossRef]
- Salim, T.I.; Nestlerode, L.C.; Lucatorto, E.L.; Wasserman, T.L.; Din, H.A.; Landsittel, D.P.; Tevar, A.D.; Johnson, J.T.; Duarte-Rojo, A.; Dunn, M.A. Frailty as Tested by Gait Speed Is a Risk Factor for Liver Transplant Respiratory Complications. Am. J. Gastroenterol. 2020, 115, 859–866. [Google Scholar] [CrossRef] [PubMed]
- Huisman, E.J.; Trip, E.J.; Siersema, P.D.; Van Hoek, B.; Van Erpecum, K.J. Protein energy malnutrition predicts complications in liver cirrhosis. Eur. J. Gastroenterol. Hepatol. 2011, 23, 982–989. [Google Scholar] [CrossRef]
- Vaz, J.; Eriksson, B.; Strömberg, U.; Buchebner, D.; Midlöv, P. Incidence, aetiology and related comorbidities of cirrhosis: A Swedish population-based cohort study. BMC Gastroenterol. 2020, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Mukthinuthalapati, V.V.P.K.; Akinyeye, S.; Fricker, Z.P.; Syed, M.; Orman, E.S.; Nephew, L.; Vilar-Gomez, E.; Slaven, J.; Chalasani, N.; Balakrishnan, M.; et al. Early predictors of outcomes of hospitalization for cirrhosis and assessment of the impact of race and ethnicity at safety-net hospitals. PLoS ONE 2019, 14, e0211811. [Google Scholar] [CrossRef] [PubMed]
- Tsien, C.; Garber, A.; Narayanan, A.; Shah, S.N.; Barnes, D.; Eghtesad, B.; Fung, J.; McCullough, A.J.; Dasarathy, S. Post-liver transplantation sarcopenia in cirrhosis: A prospective evaluation. J. Gastroenterol. Hepatol. 2014, 29, 1250–1257. [Google Scholar] [CrossRef] [PubMed]
- Pagadala, M.; Dasarathy, S.; Eghtesad, B.; McCullough, A.J. Posttransplant metabolic syndrome: An epidemic waiting to happen. Liver Transplant. 2009, 15, 1662–1670. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, L.J.; Barbagallo, M. The biology of the metabolic syndrome and aging. Curr. Opin. Clin. Nutr. Metab. Care 2016, 19, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Guirguis, J.; Chhatwal, J.; Dasarathy, J.; Rivas, J.M.; McMichael, D.; Nagy, L.E.; McCullough, A.J.; Dasarathy, S. Clinical Impact of Alcohol-Related Cirrhosis in the Next Decade: Estimates Based on Current Epidemiological Trends in the United States. Alcohol. Clin. Exp. Res. 2015, 39, 2085–2094. [Google Scholar] [CrossRef]
- Sajja, K.C.; Mohan, D.P.; Rockey, D.C. Age and Ethnicity in Cirrhosis. J. Investig. Med. 2014, 62, 920–926. [Google Scholar] [CrossRef]
- Bond, M.J.; Herman, A.A. Lagging Life Expectancy for Black Men: A Public Health Imperative. Am. J. Public Health 2016, 106, 1167–1169. [Google Scholar] [CrossRef] [PubMed]
| GMP | Patients with Cirrhosis | |||||
|---|---|---|---|---|---|---|
| Age Categories (Years) | ≤50 | 51–65 | >65 | ≤50 | 51–65 | >65 |
| Number of patients | 188,510 | 121,829 | 207,266 | 24,848 | 52,969 | 29,018 |
| Female (%) | 131,500 (69.8) c,f | 60,668 (49.8) c,i | 117,519 (56.7) f,i | 15,682 (63.1) ***,c,f | 34,978 (66.0) ***,c,i | 15,618 (53.8) ***,f,i |
| Age (mean (SD)) | 34.1 (9.4) | 58.1 (4.3) | 78.1 (7.8) | 43.2 (6.4) *** | 57.3 (4.1) *** | 74.1 (6.5) *** |
| Race (%) | ||||||
| White | 108,484 (57.5) c,f | 83,825 (68.8) c,i | 162,751 (78.5) f,i | 16,372 (65.9) ***,c,f | 36,330 (68.6) c,i | 21,447 (73.9) ***,f,i |
| Black | 36,259 (19.2) c,f | 21,769 (17.9) c,i | 21,446 (10.3) f,i | 2195 (8.8) ***,c,e | 5708 (10.8) ***,c,i | 2005 (6.9) ***,e,i |
| Hispanic | 29,665 (15.7) c,f | 10,262 (8.4) c,i | 13,603 (6.6) f,i | 4592 (18.5) ***,c,f | 8230 (15.5) ***,c,i | 3946 (13.6) ***,f,i |
| Others | 14,102 (7.5) c,f | 5973 (4.9) c,i | 9466 (4.6) f,i | 1689 (6.8) ***,c,f | 2701 (5.1) c,g | 1620 (5.6) ***,g,i |
| LoS (mean (SD)) | 3.8 (5.7) c,f | 5.1 (6.90) c,i | 5.4 (6.6) f,i | 7.7 (10.8) ***,c,f | 8.1 (10.0) ***,c,i | 8.2 (8.6) ***,f,i |
| In-hospital mortality (%) | 948 (0.5) c,f | 2393 (2.0) c,i | 8011 (3.9) f,i | 1974 (7.9) ***,c,f | 5121 (9.7) ***,c,i | 3362 (11.6) ***,f,i |
| CoH in USD (median (IQR)) | 4768.0 (2979.0, 8367.0) c,f | 8197.0 (4664.0, 14,755.0) c,i | 8007.00 (4735.0, 14,121.0) f,i | 9631.8 (5610.2, 19,696.6) ***,c,f | 10,643.2 (6000.5, 22,137.5) ***,c,i | 11,408.4 (6569.9, 21,598.4) ***,f,i |
| Muscle loss phenotype (%) | 1058 (0.6) c,f | 2417 (2.0) c,i | 7052 (3.4) f,i | 2511 (10.1) ***,c,f | 6688 (12.6) ***,c,i | 4501 (15.5) ***,f,i |
| Number of diagnoses on discharge (mean (SD)) | 6.7 (4.5) c,f | 10.4 (5.6) c,i | 12.3 (5.7) f,i | 15.5 (7.2) ***,c,f | 17.5 (7.5) ***,c,i | 20.1 (7.2) ***,f,i |
| Elixhauser score (mean (SD)) | 0.8 (6.4) c,f | 3.9 (9.0) c,i | 7.2 (9.7) f,i | 12.1 (11.6) ***,c,f | 14.3 (12.3) ***,c,i | 18.3 (12.9) ***,f,i |
| Comorbidities (%) | ||||||
| Acute kidney injury | 6075 (3.2) c,f | 13,329 (10.9) c,i | 40,755 (19.7) f,i | 2948 (11.9) ***,c,f | 10,964 (20.7) ***,c,i | 10,912 (37.6) ***,f,i |
| Alcohol abuse | 9879 (5.2) c,f | 8494 (7.0) c,i | 3863 (1.9) f,i | 16,556 (66.6) ***,c,f | 28,710 (54.2) ***,c,i | 7072 (24.4) ***,f,i |
| Diabetes (uncomplicated) | 13,969 (7.4) c,f | 29,136 (23.9) c,i | 53,496 (25.8) f,i | 3888 (15.6) ***,c,f | 13,733 (25.9) ***,c,i | 10,911 (37.6) ***,f,i |
| Diabetes (complicated) | 3597 (1.9) c,f | 7667 (6.3) c,i | 11,664 (5.6) f,i | 979 (3.9) ***,c,f | 4481 (8.5) ***,c,i | 3486 (12.0) ***,f,i |
| Hypertension | 36,017 (19.1) c,f | 71,179 (58.4) c,i | 145,906 (70.4) f,i | 8017 (32.3) ***,c,f | 25,695 (48.5) ***,c,i | 18,740 (64.6) ***,f,i |
| Home discharge | 166,183 (88.7) c,f | 84,046 (70.4) c,i | 92,455 (46.4) f,i | 16,764 (73.4) ***,c,f | 29,707 (62.2) ***,f,i | 10,258 (40.1) ***,f,i |
| GMP with Muscle Loss Phenotype | Patients with Cirrhosis with Muscle Loss Phenotype | |||||
|---|---|---|---|---|---|---|
| Age categories (years) | ≤50 | 51–65 | >65 | ≤50 | 51–65 | >65 |
| Number of patients | 1058 | 2417 | 7052 | 2511 | 6688 | 4501 |
| Female (%) | 519 (49.1) d | 1111 (46.0) i | 3749 (53.2) d,i | 1386 (55.2) ***,c | 4377 (65.4) ***,c,i | 2474 (55.0) i |
| Age (mean (SD)) | 40.1 (8.4) | 58.7 (4.2) | 79.4 (7.8) | 43.0 (6.59) *** | 57.7 (4.1) | 74.5 (6.7) *** |
| Race (%) | ||||||
| White | 637 (60.2) f | 1579 (65.3) i | 5274 (74.8) f,i | 1751 (69.7) *** | 4742 (70.9) *** | 3304 (73.4) |
| Black | 230 (21.7) f | 533 (22.1) i | 942 (13.4) f,i | 242 (9.6) ***,a | 809 (12.1) ***,a,i | 370 (8.2) ***,i |
| Hispanic | 120 (11.3) e | 187 (7.7) | 471 (6.7) e | 320 (12.7) | 752 (11.2) *** | 531 (11.8) *** |
| Others | 71 (6.7) | 118 (4.9) | 365 (5.2) | 198 (7.9) a | 385 (5.8) a | 296 (6.6) ** |
| LoS (mean (SD)) | 18.1 (20.8) c,f | 14.5 (15.8) c,i | 11.5 (12.2) f,i | 15.8 (17.1) ***,c,f | 14.7 (14.7) c,i | 12.3 (11.8) ***,f,i |
| In-hospital mortality (%) | 70 (6.6) b,f | 276 (11.4) b | 834 (11.8) f | 444 (17.7) ***,cf | 1248 (18.7) ***,c,i | 897 (19.9) ***,f,i |
| CoH in USD (median (IQR)) | 25,214.5 (11,835.5, 58,475.0) c,f | 19,629.0 (10,221.0, 42,480.3) c,i | 14,611.0 (8059.0, 28,393.0) f,i | 25,506.7 (13,172.4, 52,870.7) f | 23,538.8 (12,421.5, 48,347.4) ***,i | 18,645.07 (10,762.5, 35,458.6) ***,f,i |
| Number of diagnoses on discharge (mean (SD)) | 21.3 (3.7) | 21.4 (3.8) | 21.4 (3.6) | 24.2 (3.7) ***,c,f | 24.7 (3.5) ***,c,i | 25.1 (3.1) ***,f,i |
| Elixhauser score (mean (SD)) | 19.3 (11.1) c,f | 21.4 (11.4) c,i | 22.4 (11.0) f,i | 25.6 (10.3) ***,c,f | 26.8 (10.8) ***,c,i | 29.5 (11.2) ***,f,i |
| Comorbidities (%) | 19.3 (11.1) c,f | 21.4 (11.4) c,i | 22.4 (11.0) f,i | 25.6 (10.3) ***,c,f | 26.8 (10.8) ***,c,i | 29.5 (11.2) ***,f,i |
| Acute kidney injury | 224 (21.2) c,f | 588 (24.3) c,i | 2331 (33.1) f,i | 532 (21.2) c,f | 1887 (28.2) ***,c,i | 1878 (41.7) ***,f,i |
| Alcohol abuse | 130 (12.3) f | 325 (13.4) i | 229 (3.2) f,i | 1602 (63.8) ***,c,f | 3709 (55.5) ***,c,i | 1228 (27.3) ***,f,i |
| Diabetes (uncomplicated) | 159 (15.0) c,f | 518 (21.4) c,h | 1719 (24.4) f,h | 378 (15.1) c,f | 1551 (23.2) c,i | 1374 (30.5) ***,f,i |
| Diabetes (complicated) | 109 (10.3) | 294 (12.2) i | 668 (9.5) i | 141 (5.6) c,f | 652 (9.7) ***,c,i | 535 (11.9) ***,f,i |
| Hypertension | 411 (38.8) c,f | 1367 (56.6) c,i | 4864 (69.0) f,i | 899 (35.8) c,f | 3404 (50.9) ***,c,i | 2837 (63.0) ***,f,i |
| Home discharge | 393 (39.8) c,f | 609 (28.5) c,i | 906 (14.6) f,i | 944 (45.8) ***,c,f | 1837 (33.8) ***,c,i | 679 (18.9) ***,f,i |
| Patients with Cirrhosis vs. General Medical Patients Age ≤ 50 | Patients with Cirrhosis vs. General Medical Patients Age 51–65 | Patients with Cirrhosis vs. General Medical Patients Age > 65 | ||||
|---|---|---|---|---|---|---|
| Unadjusted OR (95% CI) | Adjusted * OR (95% CI) | Unadjusted OR (95% CI) | Adjusted * OR (95% CI) | Unadjusted OR (95% CI) | Adjusted * OR (95% CI) | |
| Cost of hospitalization | 1.00 (0.93, 1.08) | 0.92 (0.81, 1.04) | 1.20 (1.14, 1.25) | 1.24 (1.15, 1.34) | 1.26 (1.22, 1.31) | 1.10 (1.04, 1.17) |
| Hospital mortality | 2.89 (2.06–4.17) | 2.15 (1.44–3.27) | 1.98 (1.63, 2.43) | 1.86 (1.49–2.33) | 1.87 (1.62–2.16) | 1.77 (1.50–2.08) |
| Length of stay | 0.94 (0.89, 1.00) | 0.91 (0.82, 1.01) | 1.05 (1.01, 1.09) | 1.10 (1.03, 1.16) | 1.09 (1.06, 1.12) | 1.02 (0.98, 1.07) |
| GMP without Muscle Loss Phenotype | GMP with Muscle Loss Phenotype | |||||
|---|---|---|---|---|---|---|
| Age categories (years) | ≤50 | 51–65 | >65 | ≤50 | 51–65 | >65 |
| Number of patients | 187,452 | 119,412 | 200,214 | 1058 | 2417 | 7052 |
| Female (%) | 130,981 (69.9) c,f | 59,557 (49.9) c,i | 113,770 (56.8) f,i | 519 (49.1) ***,d | 1111 (46.0) ***,i | 3749 (53.2) ***,d,i |
| Age (mean (SD)) | 34.1 (9.3) | 58.1 (4.3) | 78.0 (7.8) | 40.1 (8.4) *** | 58.7 (4.2) *** | 79.4 (7.8) *** |
| Race (%) | ||||||
| White | 108,484 (57.5) c,f | 83,825 (68.8) c,i | 162,751 (78.5) f,i | 637 (60.2) | 1579 (65.3) *** | 5274 (74.8) *** |
| Black | 36,259 (19.2) c,f | 21,769 (17.9) c,i | 21,446 (10.3) f,i | 230 (21.7) *,a | 533 (22.1) ***,a,i | 942 (13.4) ***,i |
| Hispanic | 29,665 (15.7) c,f | 10,262 (8.4) c,i | 13,603 (6.6) f,i | 120 (11.3) *** | 187 (7.7) | 471 (6.7) |
| Others | 14,102 (7.5) c,f | 5973 (4.9) c,i | 9466 (4.6) f,i | 71 (6.7) a | 118 (4.9) a | 365 (5.2) * |
| LoS (mean (SD)) | 3.7 (5.3) c,f | 4.9 (6.5) c,i | 5.2 (6.2) f,i | 18.1 (20.8) ***,c,f | 14.5 (15.8) ***,c,i | 11.5 (12.2) ***,f,i |
| In-hospital mortality (%) | 878 (0.5) c,f | 2117 (1.8) c,i | 7177 (3.6) f,i | 70 (6.6) ***c,f | 276 (11.4) ***c,i | 834 (11.8) ***f,i |
| CoH in USD (median (IQR)) | 4746.0 (2971.0, 8284.0) c,f | 8080.0 (4622.0, 14,465.5) c,i | 7871.0 (4672.5, 13,787.0) f,i | 25,214.5 (11,835.5, 58,475.0) ***,c,f | 19,629.0 (10,221.0, 42,480.3) ***,c,i | 14,611.0 (8059.0, 28,393.0) ***,f,i |
| Number of diagnoses on discharge (mean (SD)) | 6.6 (4.4) c,f | 10.2 (5.4) c,i | 12.0 (5.5) f,i | 21.3 (3.7) *** | 21.4 (3.8) *** | 21.4 (3.6) *** |
| Elixhauser score (mean (SD)) | 0.7 (6.2) c,f | 3.6 (8.6) c,i | 6.6 (9.2) f,i | 19.3 (11.1) ***,c,f | 21.4 (11.4) ***,c,i | 22.4 (11.0) ***,f,i |
| Comorbidities (%) | 0.7 (6.2) c,f | 3.6 (8.6) c,i | 6.6 (9.2) f,i | 19.3 (11.1) ***,c,f | 21.4 (11.4) ***,c,i | 22.4 (11.0) ***,f,i |
| Acute kidney injury | 5851 (3.1) c,f | 12,741 (10.7) c,i | 38,424 (19.2) f,i | 224 (21.2) ***,f | 588 (24.3) ***,i | 2331 (33.1) ***,f,i |
| Alcohol abuse | 9749 (5.2) c,f | 8169 (6.8) c,i | 3634 (1.8) f,i | 130 (12.3) ***,f | 325 (13.4) ***,i | 229 (3.2) ***,f,i |
| Diabetes (uncomplicated) | 13,810 (7.4) c,f | 28,618 (24.0) c,i | 51,777 (25.9) f,i | 159 (15.0) ***,c,f | 518 (21.4) **,c,h | 1719 (24.4) **,f,h |
| Diabetes (complicated) | 3488 (1.9) c,f | 7373 (6.2) c,i | 10,996 (5.5) f,i | 109 (10.3) *** | 294 (12.2) ***,i | 668 (9.5) ***,i |
| Hypertension | 35,606 (19.0) c,f | 69,812 (58.5) c,i | 141,042 (70.4) f,i | 411 (38.8) ***,c,f | 1367 (56.6) c,i | 4864 (69.0) *,f,i |
| Home discharge | 165,790 (88.9) c,f | 83,437 (71.2) c,i | 91,549 (47.5) f,i | 393 (39.8) ***,c,f | 609 (28.5) ***,c,i | 906 (14.6) ***,f,i |
| Patients with Cirrhosis without Muscle Loss Phenotype | Patients with Cirrhosis with Muscle Loss Phenotype | |||||
|---|---|---|---|---|---|---|
| Age categories (years) | ≤50 | 51–65 | >65 | ≤50 | 51–65 | >65 |
| Number of patients | 22,337 | 46,281 | 24,517 | 2511 | 6688 | 4501 |
| Female (%) | 14,296 (64.0) c,f | 30,601 (66.1) c,i | 13,144 (53.6) f,i | 1386 (55.2) ***c | 4377 (65.4) c,i | 2474 (55.0) i |
| Age (mean (SD)) | 43.2 (6.4) | 57.3 (4.1) | 74.1 (6.5) | 43.0 (6.6) | 57.7 (4.1) *** | 74.5 (6.7) *** |
| Race (%) | ||||||
| White | 16,372 (65.9) c,f | 36,330 (68.6) c,i | 21,447 (73.9) f,i | 1751 (69.7) *** | 4742 (70.9) *** | 3304 (73.4) |
| Black | 2195 (8.8) c,e | 5708 (10.8) c,i | 2005 (6.9) e,i | 242 (9.6) a | 809 (12.1) **,a,i | 370 (8.2) **,i |
| Hispanic | 4592 (18.5) c,f | 8230 (15.5) c,i | 3946 (13.6) f,i | 320 (12.7) *** | 752 (11.2) *** | 531 (11.8) ** |
| Others | 1689 (6.8) c,f | 2701 (5.1) c,g | 1620 (5.6) g,i | 198 (7.9) *,a | 385 (5.8) *,a | 296 (6.6) ** |
| LoS (mean (SD)) | 6.8 (9.4) c,f | 7.2 (8.8) c,h | 7.4 (7.7) f,h | 15.8 (17.1) ***,b,f | 14.7 (14.7) ***,b,i | 12.3 (11.8) ***,f,i |
| In-hospital mortality (%) | 1530 (6.8) c,f | 3873 (8.4) c,i | 2465 (10.1) f,i | 444 (17.7) *** | 1248 (18.7) *** | 897 (19.9) *** |
| CoH in USD (median (IQR)) | 8921.3 (5342.8, 16,837.6) c | 9680.6 (5621.7, 18,898.9) c,i | 10,439.6 (6164.0, 19,323.8) i | 25,506.7 (13,172.4, 52,870.7) ***,c,f | 23,538.8 (12,421.5, 48,347.4) ***,c,i | 18,645.07 (10,762.5, 35,458.6) ***,f,i |
| Number of diagnoses on discharge (mean (SD)) | 14.5 (6.8) c,f | 16.5 (7.3) c,i | 19.2 (7.4) f,i | 24.2 (3.7) ***,c,f | 24.7 (3.5) ***,c,i | 25.1 (3.1) ***,f,i |
| Elixhauser score (mean (SD)) | 10.6 (10.7) c,f | 12.4 (11.4) c,i | 16.2 (12.1) f,i | 25.6 (10.3) ***,c,f | 26.8 (10.8) ***,c,i | 29.5 (11.2) ***,f,i |
| Comorbidities (%) | ||||||
| Acute kidney injury | 2416 (10.8) c,f | 9077 (19.6) c,i | 9034 (36.8) f,i | 532 (21.2) ***,c,f | 1887 (28.2) ***,c,i | 1878 (41.7) ***,f,i |
| Alcohol abuse | 14,954 (66.9) c,f | 25,001 (54.0) c,i | 5844 (23.8) f,i | 1602 (63.8) **,c,f | 3709 (55.5) *,c,i | 1228 (27.3) ***,f,i |
| Diabetes (uncomplicated) | 3510 (15.7) c,f | 12,182 (26.3) c,i | 9537 (38.9) f,i | 378 (15.1) c,f | 1551 (23.2) ***,c,i | 1374 (30.5) ***,f,i |
| Diabetes (complicated) | 838 (3.8) c,f | 3829 (8.3) c,i | 2951 (12.0) f,i | 141 (5.6) ***,c,f | 652 (9.7) ***,c,i | 535 (11.9) f,i |
| Hypertension | 7118 (31.9) c,f | 22,291 (48.2) c,i | 15,903 (64.9) f,i | 899 (35.8) ***,c,f | 3404 (50.9) ***,c,i | 2837 (63.0) *,f,i |
| Home discharge | 15,820 (76.1) c,f | 27,870 (65.8) c,i | 9579 (43.5) f,i | 944 (45.8) ***,c,f | 1837 (33.8) ***,c,i | 679 (18.9) ***,f,i |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Welch, N.; Attaway, A.; Bellar, A.; Alkhafaji, H.; Vural, A.; Dasarathy, S. Compound Sarcopenia in Hospitalized Patients with Cirrhosis Worsens Outcomes with Increasing Age. Nutrients 2021, 13, 659. https://doi.org/10.3390/nu13020659
Welch N, Attaway A, Bellar A, Alkhafaji H, Vural A, Dasarathy S. Compound Sarcopenia in Hospitalized Patients with Cirrhosis Worsens Outcomes with Increasing Age. Nutrients. 2021; 13(2):659. https://doi.org/10.3390/nu13020659
Chicago/Turabian StyleWelch, Nicole, Amy Attaway, Annette Bellar, Hayder Alkhafaji, Adil Vural, and Srinivasan Dasarathy. 2021. "Compound Sarcopenia in Hospitalized Patients with Cirrhosis Worsens Outcomes with Increasing Age" Nutrients 13, no. 2: 659. https://doi.org/10.3390/nu13020659
APA StyleWelch, N., Attaway, A., Bellar, A., Alkhafaji, H., Vural, A., & Dasarathy, S. (2021). Compound Sarcopenia in Hospitalized Patients with Cirrhosis Worsens Outcomes with Increasing Age. Nutrients, 13(2), 659. https://doi.org/10.3390/nu13020659







