Abstract
Background: There exist several prediction equations for the estimation of resting energy expenditure (REE). However, none of these equations have been validated in the Chilean female population yet. The aims of this study are (1) to determine the accuracy of existing equations for prediction of REE and (2) to develop new equations in a sample of healthy Chilean women. Methods: A cross-sectional descriptive study was carried out on 620 Chilean women. The sample showed an age range between 18 and 73 years, a body mass index average of 28.5 ± 5.2 kg/m2, and a prevalence of overweight and obesity of 41% and 33.2%, respectively. REE was measured by indirect calorimetry (REEIC), which was used as the gold standard to determine the accuracy of twelve available REE prediction equations and to calculate alternative formulas for estimation of REE. Paired t-tests and Bland–Altman plots were used to know the accuracy of the estimation equations with REEIC. At the same time, multiple linear regressions were performed to propose possible alternative equations. The analyses were carried out by age groups and according to nutritional status. Results: All the equations showed a tendency to overestimate REE, regardless of age or nutritional status. Overall, the Ireton-Jones equation achieved the highest mean percentage difference from REEIC at 67.1 ± 31%. The alternative new equations, containing variables of body composition, reached a higher percentage of classification within ±10% of REEIC. Conclusions: The available equations do not adequately estimate REE in this sample of Chilean women. Although they must be validated, the new formulas proposed show better adaptation to this Chilean sample.
1. Introduction
Mortality due to non-communicable diseases (NCDs) has been increasing steadily in recent years. Currently, NCDs cause 41 million deaths per year, representing 71% of the total number of deaths worldwide [1]. These include those due to cardiovascular diseases (the world’s leading cause of death), cancer, respiratory diseases, and diabetes [2]. NCDs may increase mortality rates and decrease life quality by reducing disability-adjusted life years, life expectancy, and potential life years lost [3].
NCDs’ development is related to several cardiovascular risk factors (CRF) [4,5,6]. Among the CFR, overweight and obesity stand out. These conditions are considered as severe public health problems because of their high prevalence and impact on health at all life stages [7,8]. It should be noted that this problem is more prevalent in the female than in the male population. In 2016, the prevalence of overweight was estimated at 39% in men and 40% in women, and the prevalence of obesity reached 11% in men and 15% in women [9]. For instance, between 1975 and 2016, worldwide, women suffering from obesity increased from 69 to 390 million, while in men, this rate varied from 31 to 281 million [10]. This problem also impacts the economic and social aspects of families and national health systems [11].
For these reasons, early lifestyle interventions are essential to ensure good health. It is necessary to emphasize that diet plays a fundamental role in the development of NCDs [12]. Although improving food quality and controlling the percentages of macronutrients that provide daily energy is crucial, an essential element of any dietary approach aimed at body fat loss is the relationship between energy intake and expenditure (energy balance) [13]. A positive energy balance (energy intake > energy expenditure) leads to weight gain, so all recommendations on body fat loss include energy intake reduction and an increase in energy expenditure, primarily through physical activity, to ensure a proper energy flux [14,15]. To know the total energy expenditure (TEE) is fundamental to be able to adjust this relationship. TEE is composed of the thermic effect of activity, non-exercise activity thermogenesis, the thermic effect of food, and resting energy expenditure (REE) [15]. Of these four TEE components, REE represents the highest proportion, reaching between 60 and 70%, depending on the level of physical activity performed [16]. Therefore, to adjust the energy intake, it is necessary to estimate REE, for which there are various methods available such as direct and indirect calorimetry. However, access to the devices that allow their measurement is not easy because they are sophisticated equipment that requires specially trained staff and entails a high cost [17].
Alternatively, there are different prediction equations available that allow estimation of REE based on more accessible parameters (e.g., age, height, weight). In this sense, sex is an essential variable in estimating REE, and it is used in the most common predictive equations because women generally have a lower REE than men [18]. These equations allow for quicker and low-cost utilization without requiring trained personnel [19]. However, these formulas are not adapted to all populations, which leads to a lack of accuracy when their results are compared with data collected using a gold standard (e.g., indirect calorimetry) [20]. In addition to the lack of accuracy, the wide variety of equations available makes it difficult to choose the most appropriate one.
Several studies have reported that these discrepancies may be increased depending on the characteristics of the study population (origin, altered metabolic state, pathologies) [21]. Two factors with a significant influence on the accuracy of the equations are age and body weight [22]. Considering age is very important because REE decreases as aging progresses [23]. In this sense, and given the significant variability of formulas (according to individuals’ age group and nutritional status) for the REE estimate [22,24], it is very complex to extrapolate and standardize the results to allow comparisons between different populations. For this reason, researchers recommend using these formulas in populations with similar characteristics to those from which they were initially developed. If they are utilized in other populations with different characteristics, it is recommended to validate or adapt them to know or improve their accuracy [22,23,24,25,26].
Therefore, this study aims (1) to determine the accuracy of twelve already available equations for estimation of REE and (2) to develop new, more accurate equations in a sample of healthy Chilean women.
2. Materials and Methods
2.1. Design, Population, and Sample
A cross-sectional descriptive study was carried out, including women who attended the nutrition consultation at the Healthy Life Centre (Concepción, Chile) between January 2016 and June 2019, where indirect calorimetry was performed. The sample size was estimated through Epidat 4.2. (Department of Health, Xunta de Galicia, Galicia, Spain). For the sample size calculation, the female population over 18 years of age in Chile was taken as a reference. The minimum sample size calculated was 537 subjects for a precision of 4%, a power of 80%, a confidence level of 95% (α = 0.05), and an expected overweight prevalence of 33.7% [27].
Women over 18 years of age were included, and those with chronic pathologies that could affect REE (such as cancer, hyperthyroidism, or hypothyroidism) or who presented an error on indirect calorimetry (given by a coefficient of variation (CV, applied to the mean of VO2 and VCO2) over 10% or measurement time below 25 min) were excluded. From the initial sample of 653 women, 33 were dismissed.
2.2. Antropometrics Measurements
The independent variables collected were age (years) and anthropometric measurements: weight (kg), height (cm), body mass index (BMI, kg/m2), body fat percentage (BF%), fat mass (FM, kg), fat-free mass (FFM, kg), and body water (BW, kg).
The anthropometric measurements were collected following the recommendations of the manual of standardized anthropometry [28]. Since the calorimeter demands anthropometric data (weight, height, and lean mass), the measurement was made before the indirect calorimetry study. For measuring height, a SECA 700 (Seca GmbH, Hambrug, Germany) stadiometer and balance were used, with an accuracy of 0.1 cm. The height measurement was made without shoes, with the feet together, heels, buttocks, and upper back touching the stadiometer, with the head in the plane of Frankfort, after a deep inspiration. We utilized the Tanita BC-418 (TANITA, Tokyo, Japan) with eight electrodes in the study of body composition. Body composition and weight were measured with light clothing and bare feet, removing metal objects such as earrings, watches, and bracelets. In addition, fasting (10–12 h), empty bladder, abstinence from alcohol or stimulant drinks, and no physical exercise 24 h before the day of the study were required for measurement. All the measures were taken by specialized personnel. Each measurement was repeated three times by the same assessor, and the average of the three value was calculated and used for further analysis.
The nutritional status classification was made according to the BMI following the WHO’s recommendations: normal weight, 18.5 to <25 kg/m2; overweight, 25 to <30 kg/m2; obesity, ≥30 kg/m2 [29].
2.3. Indirect Calorimetry and Estimation Formulas
REE (result variable) was measured using indirect calorimetry (gold standard). The modified Weir formula was used for its calculation, based on the oxygen consumed and the carbon dioxide produced [30].
REE (Kcal/day) = [(VO2 × 3.941) + [(VCO2 × 1.11)] × 1440
REE was measured using the Ultima CCM device (MGC Diagnostics, Minnesota, USA), designed to measure indirect calorimetry through respiratory gases. Before the measurement, the flow and equipment were calibrated, controlling the environmental temperature (21.6 ± 0.7 °C), the humidity (48.3 ± 5.4%), and the room’s atmospheric pressure. The measurements were made at 12 m above sea level. The REE measurement was made during the morning between 8:00 and 10:00 a.m. All women who underwent indirect calorimetry followed a strict protocol in which they were instructed to do the following: fast for 12 h, not to consume stimulant beverages, not to smoke, and not to perform physical activity in the 12 h before the test. Once the women arrived at the center for the assessment, they rested for 30 min. During calorimetry, participants were in the supine position with a face piece on, awake in the room. The process lasted 25 min, without considering the first five minutes of the REE measurement. The values’ average of the remaining 20 min was used to compute REE.
Further, we estimated REE (Kcal/day) through the formulas presented in Table 1.

Table 1.
Estimation formulas for women.
2.4. Ethical and Legal Aspects
The study was carried out in compliance with the fundamental principles laid down in the Declaration of Helsinki (1964), the Council of Europe Convention on Human Rights and Biomedicine (1997), and the UNESCO Universal Declaration on the Human Genome and Human Rights (1997), as well as with the requirements laid down in Chilean legislation in the fields of biomedical research, the protection of personal data, and bioethics. The Bioethics Committee of the Vice-Rectory of Research of the University of Concepción approved the study protocol (October 2019; Code: 538-2019).
2.5. Statistical Analysis
The quantitative variables are presented with mean and standard deviation, and the qualitative values are shown with frequencies and percentages.
To contrast the goodness of fit to a normal distribution of the data from the quantitative variables, the Kolmogorov–Smirnov test with Lilliefors correction was applied. One-way ANOVA for three means or more and the post hoc Bonferroni test were performed for the bivariate hypothesis contrast. Paired t-tests were performed to compare REEIC and REE estimated by the formulas. For the qualitative variables, the chi-square and Fisher exact tests were used when necessary. Pearson’s correlation coefficient (r) was applied to correlate REEIC with anthropometric variables and REEIC with REE estimated by the formulas. The cut-off points established to assess the strength of association were: very weak, 0 to 0.19; weak, 0.2 to 0.39; moderate, 0.4 to 0.59; strong, 0.6 to 0.79; and very strong 0.8 to 1.0 [41]. We performed Cohen’s d to study the size effect of the mean differences.
Adjusted multiple linear regressions were performed to develop various predictive formulas that would fit with indirect calorimetry measurements. These regressions were developed following the stepwise regression backward method. This method begins with an equation that includes all the explanatory variables and extracts, one by one, the variables with the highest “p value,” until a final model is reached with all the significant explanatory variables (p < 0.05). To determine the models’ goodness of fit, we analyzed the standard error, the adjusted coefficient of determination, the F statistic, the collinearity analysis (computing the variance inflation factor (VIF) and the tolerance statistic), and the residuals.
The concordance between REEIC and REE estimated by the equations was analyzed using Bland–Altman plots. In Bland–Altman plots, positive values show overestimation of equations and negative values show underestimation. Based on previous studies [25], we assessed the percentage difference between REE measured by the indirect calorimeter and that estimated by the equations (). In addition, we studied the percentage of women whose estimated REE was within ±10% of that measured by the gold standard. All the results are shown in the total sample, considering the nutritional status, according to the age groups traditionally stated in the literature (18 to <30 years, 30 to <60 years, and ≥60 years).
The probability of an α error below 5% (p < 0.05) was considered statistically significant for all the hypothesis contrasts, and the confidence interval was calculated at 95%. For the statistical analysis, IBM SPSS Statistics 22.0 software (IBM, Chicago, IL, USA) was used.
3. Results
3.1. Description of the Sample
The final sample consisted of 620 women. The women showed an age range between 18 and 73 years. Following the BMI criteria, the prevalence of overweight (≥25 kg/m2) and obesity (≥30 kg/m2) was 41% (95%CI 37.1–45%) and 33.2% (95%CI 29.5–37.1), respectively. The mean CV was 4.9 ± 1.6%.
Concerning the body composition, results show that BF% increased among the age groups, although this increase was not significant among the 18 to <30 years and 30 to <60 years groups (mean difference (MD) = 1.6; p = 0.073). On the other hand, FM decreased significantly among the age groups, although the decrease was not significant among the 30 to <60 years and ≥60 years groups (MD = 1.4; p = 0.419). All variables analyzed showed significant differences between the different nutritional states, except for: (i) age between 25 to <30 and ≥30 kg/m2 (MD = 0.3; p = 1.000), (ii) height between 18.5 to <25 and 25 to <30 kg/m2 (MD = 0.5; p = 1.000), and (iii) height between 25 to <30 and ≥30 kg/m2 (MD = 1.1; p = 0.194). Table 2 shows the characteristics of the sample by age and nutritional status according to BMI. Table S1 shows size effects of each group comparison.

Table 2.
Characteristics of participants according to age groups and nutritional status.
3.2. Differences between REEs Measured by Indirect Calorimetry (REEIC) and Estimated by Twelve Available Formulas
Table 3 and Table 4 show the accuracy of the twelve equations in the total sample, according to the age groups and the nutritional status of the women studied. For all three comparisons (total sample, according to age group, and nutritional status), the estimation equations tend to significantly overestimate what was measured through indirect calorimetry, with percentage differences of more than 10% between REEIC and REE estimated by the equations. Tables S2 and S3 show size effects of each group comparison, and Table S4 shows the size effect of the paired t-test.

Table 3.
Resting energy expenditure (REE) (Kcal/day) by age groups.

Table 4.
Resting energy expenditure (Kcal/day) by nutritional status
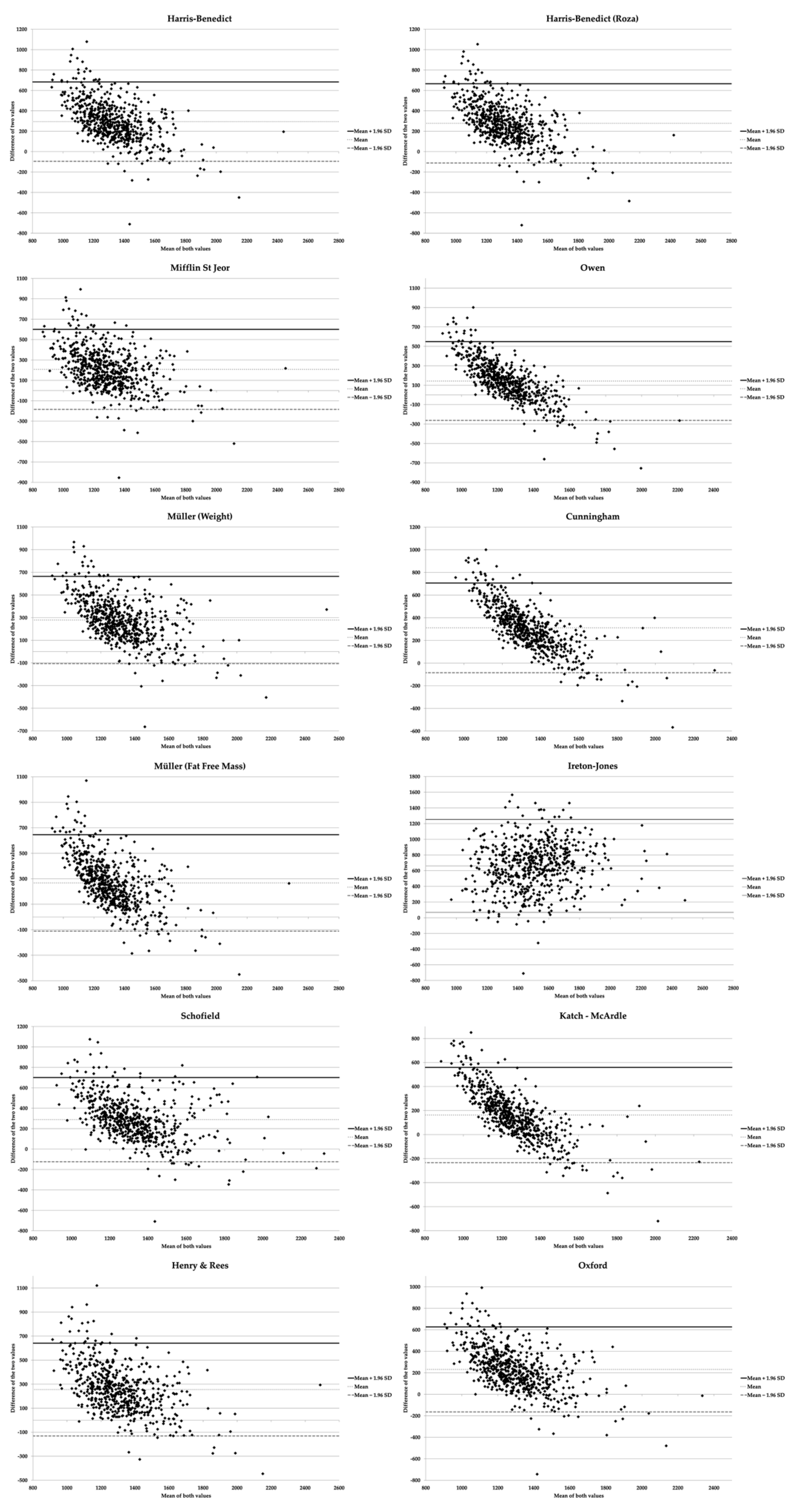
Figure 1 shows that, in the total sample, all the equations tended to overestimate in women with lower REE, while they reduced and even underestimated when REE increased. The equation proposed by Ireton-Jones [35] was the only one that overestimated independently of REEIC. Further, the mean of the differences between the calculated formulas and REEIC was higher than 0 (Table 3), which confirms that, in general, the formulas tend to overestimate REE.
Figure 1.
Bland–Altman graphs for resting energy expenditure equations using indirect calorimetry as the gold standard.
In the whole sample and the three age groups analyzed, the Ireton-Jones [35] equation was the one that overestimated REE the most. In contrast, the equation proposed by Owen [34] showed the lowest overall overestimate (16.5 ± 24.1%), from 18 to <30 years (13.5 ± 23.1%) and 30 to <60 years (17.1 ± 24.2%). In women ≥60 years, the Mifflin St. Jeor [32] equation showed the smallest mean difference (11.9 ± 24.2%).
Finally, the Katch-McArdle [38] equation achieved the highest proportion of classification within ±10% in the total sample (39.5%) and in the 30 to <60 age group (40.4%). In groups from 18 to <30 years and ≥60 years, the Owen [34] (43.8%) and Mifflin St. Jeor [32] (37.9%) equations showed better classification percentages, respectively. According to the BMI categories (Table 4), the Ireton-Jones [35] equation held the greatest overestimation across all nutritional status groups, and the Owen [34] equation the smallest. However, the Owen [34] equation only obtained the best classification percentage within ±10% in the group with a BMI of 18.5 to <25 kg/m2 (33.8%). The Katch–McArdle [38] equation was more accurate in the other two BMI groups, with 37% (25 to <30 kg/m2) and 53.4% (≥30 kg/m2). We have found discrepancies between most of the calculated equations and REEIC in women with normal weight, overweight, and ≥60 years. The correlations can explain these discrepancies because although significant, they were low (Table 3 and Table 4).
3.3. New Equations for the Estimation of REE
Table 5 shows the bivariate correlations between REEIC and the different anthropometric variables. In the total sample, the ≥30 kg/m2 group and the three age groups, weight, FFM, and FM showed a moderate to strong correlation. In the normal weight and overweight groups, the correlation, although significant, was lower.

Table 5.
Linear correlations between REEIC (Kcal/d) and independent variables.
Table 6 presents several estimation formulas for the whole sample, depending on age and nutritional status. The equations that do not require the measurement of body composition showed an overestimation close to 3%, being lower in the group of 18 to <25 kg/m2 (2.7 ± 18.2%). The computed equations showed that about 50% of the women in the study obtained an estimation of their REE within ±10% of REE measured by indirect calorimetry. On the other hand, the formulas based on body composition data provided more homogeneity in the estimation (the 95% CI of the mean difference is closer) and higher classification percentage within ±10%, except in the group of ≥60 years and with a BMI from 18 to <25 kg/m2.

Table 6.
Proposed formulas for resting energy expenditure estimation.
4. Discussion
The purpose of the study was to determine the accuracy of twelve already existing equations for REE estimation in a sample of healthy Chilean women. In addition, we developed several equations for this sample stratified by age and nutritional status to provide alternatives that health care professionals can use depending on their tools available (e.g., based on anthropometric or body composition values).
The prevalence of overweight and obesity among participants was 41% and 33.2%, respectively. These rates are similar to those shown by the Chilean National Health Survey (36.4% and 33.7%) [27]. All the equations analyzed tended to overestimate REE, with it being greater in those participants with lower REE. Further, while REE increases, a gradual reduction in this overestimation can be observed, reaching underestimations in the highest values. In the literature, the results between different research are not consistent. Although some authors evidenced a similar trend to that shown in our population [42,43], Anjos et al. [25] found that REE calculated in women following the Schofield [37], Henry–Rees [39], and Harris–Benedict [31] equations was higher than that measured by the indirect calorimeter, regardless of age group and BMI. Galgani et al. [44] evidenced that these equations showed a higher percentage of overestimation than underestimation. However, they achieved, globally, higher accuracy than that obtained in our results. Willis et al. [45] argued that the Mifflin St. Jeor [32] and Harris–Benedict [31] equations overestimated REE, something observed in our results, while Owen’s [34] formula underestimated it. In summary, the literature shows significant variability in the accuracy of the available formulas, mediated by various factors [46].
One of the most studied is the influence of the nutritional status, according to BMI, on REE. In this regard, the main problem found is that the authors recommend different formulas depending on the reference population, making standardization difficult. Our results show how REEIC increased significantly among the normal weight (1054.4 ± 185.2 Kcal/day), overweight (1142.8 ± 198 Kcal/day), and obesity (1331.1 ± 285 Kcal/day) groups and, in general, the accuracy of the REE estimation increased with the rise in BMI. Similarly to our results, Jesus et al. [47] showed that the accuracy of the equations studied was higher among people with higher BMI. Of the analyzed equations, that proposed by Owen [34] in the normal weight group (18 to <25 kg/m2) and the Katch–McArdle equation [38] for the overweight (25 to <30 kg/m2) and obesity (≥30 kg/m2) groups were the ones that obtained the best classification within ±10%, with 33.8%, 37%, and 53.4%, respectively.
Although the classification improved in the overweight and obesity groups in comparison to normal weight group, it remained low due to the wide bias shown. Poli et al. [48], in their work on women suffering from obesity, reported similar results, finding a low agreement between what is predicted by the equations and what is measured by indirect calorimetry and concluding that the Harris–Benedict [31] and FAO/WHO equations offered the highest accuracy. Namazami et al. [49] recommended using the Mifflin St. Jeor [32] equation in women with normal weight and overweight (especially in overweight, where this formula has shown greater accuracy). Finally, Amaro-Gahete et al. [22,24], in their research focused on young and middle-aged adults, concluded that it was necessary to choose a different formula for each nutritional status.
Another variable that influences REE, and which a large part of the equations analyzed considers, is age. Our findings show that predictive capacity also varies depending on the age group studied. In this regard, the Owen [34], Katch–McArdle [38], and Mifflin St. Jeor [32] equations achieved a higher proportion of correct classification in the 18 to <30 years, 30 to <60 years, and ≥60 years groups, respectively. However, as with BMI, previous studies reported significant heterogeneity in recommending formulas based on population age [22,24,25].
These facts reveal that it is very complicated to establish which equation should be used in each clinical setting. This difficulty is linked to significant inter-population variability, which can be influenced by aspects such as the geographical origin [50]. In this sense, the equations analyzed were developed in samples with specific characteristics, which means that their predictive capacity decreases when testing their validity in other places. Various research has shown that REE varies according to ethnic group, mainly due to physical characteristics (abdominal fat, percentage of body fat, fat-free mass, etc.) [51,52,53]. For instance, Spaeth et al. [54] showed that the African-American population had a lower REE than the Caucasian population. Some authors consider that race is essential when developing estimation formulas to improve the nutritional approach, especially in those that do not include body composition variables [55,56]. This omission could explain part of the lack of accuracy of some equations, since the ethnic groups present in the Chilean population, and their characteristics, are different from the populations in which the equations were generally developed (Europe, United States, etc.) [57,58]. In this sense, when population-specific equations are developed, it is possible to improve REE estimation [25,59]. For instance, in the adaptation carried out in our population, all the proposed formulas reduced the bias and the mean percentage difference. In addition, the classification percentage within ±10% was also increased. Wahrlich et al. [59] achieved a higher correct percentage of classification in women than we found in our results (77.5% vs. 51.4%) when they validated the formula proposed by Anjos et al. in a tropical urban population. However, their sample size was smaller, and the population characteristics were distinct.
In a study carried out in the Mexican population, the researchers developed an equation that improved REE estimation. However, no accuracy analysis was shown, so it is difficult to determine its real predictive capacity [60].
Cruz et al. [61], in a study of the Spanish population, achieved an R2 of 0.230 among those with a BMI of ≥ 25 kg/m2 using sex, age, and weight as independent variables. In our case, an R2 of 0.141 was reached in the group of 25 to <30 kg/m2. This rate reached 0.387 in the group of ≥30 kg/m2 with the same variables and larger sample size.
On the other hand, our results show less variability explained by the proposed formulas among women with normal weight and overweight. In these cases, it is possible that other sources of variation such as hormonal aspects, the performance of resistance training, or alterations that are not usually controlled in protocols, such as modifications of sleep patterns or quality, could alter the measurement of REEIC [54,62,63].
From our perspective, the wide variety of proposed equations should not be a problem for its use. For instance, all of them could be incorporated into a mobile health application (mHealth) where values of the variables that any clinical professional manages in their particular clinical setting (with or without body composition analysis) could be introduced [64]. Finally, the app could use different equations—according to the data introduced—and show the estimated REEs, the formulas used, their accuracy, and the confidence margins for each one. The evidence clarifies that REE estimation is fundamental for adequate management of patients who need to regulate their energy balance through dietary interventions. Therefore, these tools would facilitate their implementation when the necessary equipment is not available due to high costs [65,66].
Limitations and Strenghts
To our knowledge, there is not a study of this type in the Chilean population, so there is no possibility of comparing results. This research’s main limitations derive from the fact that it only considers healthy females without knowing their ethnicity.
Further, the range of the percentage of women within ±10% of REEIC was between 47.7 and 58.6% depending on age and nutritional status. This percentage means that there is still a very high proportion (nearly half of the women) where their estimated REE is >10% different from their REE measured by indirect calorimetry. For this reason, it would be advisable to use calorimetry, if possible, to measure REE the first time a patient comes in for consultation. Subsequently, in following consultations (if a measurement is not possible), health professionals could use the equations, considering the estimation’s error. Nevertheless, the equations developed present a higher accuracy than those published in the literature, at least in healthy Chilean women.
Future studies should focus on some particular conditions seen in women that might influence energy expenditure, such as polycystic ovary syndrome, postpartum, or breast cancer [67,68,69]. Further, urinary nitrogen introduction would allow a more accurate measurement of resting energy expenditure through calorimetry. Finally, since this work has only focused on comparing equations in this specific population and showing that more accurate equations can be developed, the formulas must be validated in a different sample with similar characteristics but from the same population to ensure their accuracy.
5. Conclusions
The available equations for REE estimation are not accurate enough for application in Chilean adult women, regardless of age or nutritional status, so it is impossible to recommend and standardize its use. This study has shown that it is possible to develop more accurate equations adapted to this population’s characteristics, presenting greater accuracy than what is measured by indirect calorimetry. Finally, this research makes available different equations as alternatives to indirect calorimetry when it is impossible to perform it. However, only when and if the formulas are validated would it be possible to make use of them. The fact that the different formulas proposed are based on different variables also offers choosing one or another (being aware of each one’s estimation errors), depending on the tools or data to which health care professionals have access.
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6643/13/2/345/s1, Figure S1: Bland–Altman graph for Harris-Benedict versus indirect calorimetry, Figure S2: Bland–Altman graph for Harris-Benedict (Roza) versus indirect calorimetry, Figure S3: Bland–Altman graph for Mifflin St Jeor versus indirect calorimetry, Figure S4: Bland–Altman graph for Owen versus indirect calorimetry, Figure S5: Bland–Altman graph for Müller (Weight) versus indirect calorimetry, Figure S6: Bland–Altman graph for Cunningham versus indirect calorimetry, Figure S7: Bland–Altman graph for Müller (Fat-free Mass) versus indirect calorimetry, Figure S8: Bland–Altman graph for Ireton-Jones versus indirect calorimetry, Figure S9: Bland–Altman graph for Schofield versus indirect calorimetry, Figure S10: Bland–Altman graph for Katch-McArdle versus indirect calorimetry, Figure S11: Bland–Altman graph for Henry & Rees versus indirect calorimetry, Figure S12: Bland–Altman graph for Oxford versus indirect calorimetry, Table S1: Size effect (Cohen´s d) of the means difference of independent variables according to age and nutritional status groups, Table S2: Size effect (Cohen´s d) of Resting Energy Expenditure (Kcal/day) means difference between age groups, Table S3: Size effect (Cohen´s d) of Resting Energy Expenditure (Kcal/day) means difference between nutritional status groups, Table S4: Size effect (Cohen´s d) of means difference between Resting Energy Expenditure (Kcal/day) estimated by equations and measured by indirect calorimetry according to age and nutritional status groups.
Author Contributions
Conceptualization, R.M.-L.; data curation, R.M.-L., F.C.-M., C.M.-U., N.U., and G.M.-R.; formal analysis, R.M.-L.; investigation, F.C.-M. and C.M.-U.; methodology, R.M.-L. and M.R.-S.; writing—review and editing, R.M.-L., F.C.-M., N.U., M.R.-S., and G.M.-R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by Ethics Committee of Vice-Rectory of Research of the University of Concepción approved the study protocol (October 2019; Code: 538-2019).
Informed Consent Statement
Patient consent was waived due to the use of an anonymised database.
Data Availability Statement
The data presented in this study are available on request to the corresponding author.
Conflicts of Interest
The author(s) declare that they have no conflict of interests.
References
- Organización Mundial de la Salud. Noncommunicable Diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 30 May 2020).
- Bennett, J.E.; Stevens, G.A.; Mathers, C.D.; Bonita, R.; Rehm, J.; Kruk, M.E.; Riley, L.M.; Dain, K.; Kengne, A.P.; Chalkidou, K.; et al. NCD Countdown 2030: Worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet 2018, 392, 1072–1088. [Google Scholar] [CrossRef]
- Roth, G.A.; Johnson, C.O.; Abate, K.H.; Abd-Allah, F.; Ahmed, M.; Alam, K.; Alam, T.; Alvis-Guzman, N.; Ansari, H.; Ärnlöv, J.; et al. The Burden of Cardiovascular Diseases Among US States, 1990–2016. JAMA Cardiol. 2018, 3, 375–389. [Google Scholar] [PubMed]
- Forouzanfar, M.H.; Afshin, A.; Alexander, L.T.; Anderson, H.R.; Bhutta, Z.A.; Biryukov, S.; Brauer, M.; Burnett, R.; Cercy, K.; Charlson, F.J.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1659–1724. [Google Scholar] [CrossRef]
- Yusuf, S.; Joseph, P.; Rangarajan, S.; Islam, S.; Mente, A.; Hystad, P.; Brauer, M.; Kutty, V.R.; Gupta, R.; Wielgosz, A.; et al. Modifiable risk factors, cardiovascular disease, and mortality in 155,722 individuals from 21 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet 2020, 395, 795–808. [Google Scholar] [CrossRef]
- Ng, R.; Sutradhar, R.; Yao, Z.; Wodchis, W.P.; Rosella, L.C. Smoking, drinking, diet and physical activity—modifiable lifestyle risk factors and their associations with age to first chronic disease. Int. J. Epidemiol. 2019, 49, 113–130. [Google Scholar] [CrossRef]
- Naghavi, M.; Abajobir, A.A.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Adetokunboh, O.; Ärnlöv, J.; Afshin, A.; et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Glob. Health 2017, 390, 1151–1210. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 2016, 387, 1377–1396. [Google Scholar] [CrossRef]
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 10 January 2021).
- Abarca-Gómez, L.; Abdeen, A.Z.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar]
- Organización Panamericana de la Salud. Panorama de la Seguridad Alimentaria y Nutricional. Available online: http://www.fao.org/3/a-i6747s.pdf (accessed on 30 May 2020).
- Johns, D.J.; Hartmann-Boyce, J.; Jebb, S.A.; Averyard, P. Diet or Exercise Interventions vs Combined Behavioral Weight Management Programs: A Systematic Review and Meta-Analysis of Direct Comparisons. J. Acad. Nutr. Diet. 2014, 114, 1557–1568. [Google Scholar] [CrossRef]
- Hall, K.D.; Ayuketah, A.; Brychta, R.; Cai, H.; Cassimatis, T.; Chen, K.Y.; Chung, S.T.; Costa, E.; Courville, A.; Darcey, V.; et al. Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell Metab. 2019, 30, 67–77.e3. [Google Scholar] [CrossRef]
- Romieu, I.; Dossus, L.; Barquera, S.; Blottière, H.M.; Franks, P.W.; Gunter, M.; Hwalla, N.; Hursting, S.D.; Leitzmann, M.; Margetts, B.; et al. Energy balance and obesity: What are the main drivers? Cancer Causes Control 2017, 28, 247–258. [Google Scholar] [CrossRef] [PubMed]
- Hume, D.J.; Yokum, S.; Stice, E. Low energy intake plus low energy expenditure (low energy flux), not energy surfeit, predicts future body fat gain. Am. J. Clin. Nutr. 2016, 103, 1389–1396. [Google Scholar] [CrossRef] [PubMed]
- Trexler, E.T.; Smith-Ryan, A.E.; Norton, L.E. Metabolic Adaptation to Weight Loss: Implications for the Athlete. Int. Soc. Sports Nutr. 2014, 11, 7. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, A.C.; Esteves, F.C.; Moreira, R.D.; Bressan, J. Energy expenditure: Components and evaluation methods. Nutr. Hosp. 2011, 26, 430–440. [Google Scholar]
- Buchholz, A.C.; Rafii, M.; Pencharz, P.B. Is resting metabolic rate different between men and women? Br. J. Nutr. 2001, 86, 641–646. [Google Scholar] [CrossRef]
- Blasco, R. Resting energy expenditure; assessment methods and applications. Nutr. Hosp. 2015, 31 (Suppl. 3), 245–254. [Google Scholar]
- Pasdar, Y.; Moradi, S.; Hamzeh, B.; Najafi, F.; Nachvak, S.M.; Mostafai, R.; Abdollahzad, H.; Nelson, M. The validity of resting energy expenditure predictive equations in adults with central obesity: A sub-sample of an RaNCD cohort study. Nutr. Health 2019, 25, 217–224. [Google Scholar] [CrossRef]
- Lopes, E.; Santiago, R.; Bressan, J.; Martínez, J.A. Effectiveness of prediction equations in estimating energy expenditure sample of Brazilian and Spanish women with excess body weight. Nutr. Hosp. 2014, 29, 513–518. [Google Scholar]
- Amaro-Gahete, F.J.; Jurado-Fasoli, L.; De-la-O, A.; Gutierrez, A.; Castillo, M.J.; Ruiz, J.R. Accuracy and Validity of Resting Energy Expenditure Predictive Equations in Middle-Aged Adults. Nutrients 2018, 10, 1635. [Google Scholar] [CrossRef]
- Geisler, C.; Braun, W.; Pourhassan, M.; Schweitzer, L.; Glüer, C.C.; Bosy-Westphal, A.; Müller, M.J. Age-Dependent Changes in Resting Energy Expenditure (REE): Insights from Detailed Body Composition Analysis in Normal and Overweight Healthy Caucasians. Nutrients 2016, 8, 322. [Google Scholar] [CrossRef]
- Amaro-Gahete, F.J.; Sanchez-Delgado, G.; Alcantara, J.M.A.; Martinez-Tellez, B.; Muñoz-Hernandez, V.; Merchan-Ramirez, E.; Löf, M.; Labayen, I.; Ruiz, J.R. Congruent Validity of Resting Energy Expenditure Predictive Equations in Young Adults. Nutrients 2019, 11, 223. [Google Scholar] [CrossRef] [PubMed]
- Anjos, L.A.; Wahrlich, V.; Vasconcellos, M.T.L. BMR in a Brazilian adult probability sample: The Nutrition, Physical Activity and Health Survey. Public Health Nutr. 2014, 17, 853–860. [Google Scholar] [CrossRef] [PubMed]
- Roza, A.M.; Shizgal, H.M. The Harris Benedict equation reevaluated: Resting energy requirements and the body cell mass. Am. J. Clin. Nutr. 1984, 40, 168–182. [Google Scholar] [CrossRef]
- Ministerio de Salud de Chile. Primeros y Segundos Resultados de la Encuesta Nacional de Salud 2016–2017. Available online: https://www.minsal.cl/wp-content/uploads/2017/11/ENS-2016-17_PRIMEROS-RESULTADOS.pdf (accessed on 30 December 2020).
- Callaway, C.W.; Chumlea, W.C.; Bouchard, C.; Himes, J.H.; Lohman, T.G.; Martin, A.D.; Mitchell, C.D.; Mueller, W.H.; Roche, A.F.; Seefeldt, V.D. Circumferences. In Anthropometric Standardization Reference Manual; Lohman, T.G., Roche, A.F., Martorell, R., Eds.; Human Kinetics Books: Champaign, IL, USA, 1988; pp. 44–45. [Google Scholar]
- World Health Organization. Body Mass Index. Available online: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 30 May 2020).
- Weir, J.B.V. New methods for calculating metabolic rate with special reference to protein metabolism. J. Physiol. 1949, 109, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.A.; Benedict, F.G. A Biometric study of Human Basal Metabolism. Proc. Natl. Acad. Sci. USA 1918, 4, 370–373. [Google Scholar] [CrossRef]
- Mifflin, M.D.; St Jeor, S.T.; Hill, L.A.; Scott, B.J.; Daugherty, S.A.; Koh, Y.O. A new predictive equation for resting energy expenditure in healthy individuals. Am. J. Clin. Nutr. 1990, 51, 241–247. [Google Scholar] [CrossRef]
- Müller, M.J.; Bosy-Westphal, A.; Klaus, S.; Kreymmann, G.; Lührmann, P.M.; Neuhäuser-Berthold, M.; Noack, R.; Pirke, K.M.; Platte, P.; Selberg, O.; et al. World Health Organization equations have shortcomings for predicting resting energy expenditure in persons from a modern, affluent population: Generation of a new reference standard from a retrospective analysis of a German database of resting energy expenditure. Am. J. Clin. Nutr. 2004, 80, 1379–1390. [Google Scholar]
- Owen, O.E. Resting metabolic requirements of men and women. Mayo Clin. Proc. 1988, 63, 503–510. [Google Scholar] [CrossRef]
- Ireton-Jones, C.; Jones, J.D. Improved equations for predicting energy expenditure in patients: The Ireton-Jones equations. Nutr. Clin. Pract. 2002, 17, 29–31. [Google Scholar] [CrossRef]
- Cunningham, J.J. A Reanalysis of the factors influencing basal metabolic rate in normal adults. Am. J. Clin. Nutr. 1980, 33, 2372–2374. [Google Scholar] [CrossRef]
- Schofield, W.N. Predicting basal metabolic rate, new standards and review of previous work. Human Nutrition. Hum. Nutr. Clin. Nutr. 1985, 39 (Suppl. 1), 5–41. [Google Scholar] [PubMed]
- McArdle, W.D.; Katch, F.I.; Katch, V.L. Human energy expenditure during rest and physical activity. In Exercise Physiolog—Energy, Nutrition and Human Performance, 5th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2001; pp. 187–200. [Google Scholar]
- Henry, C.J.; Rees, D.G. New predictive equations for the estimation of basal metabolic rate in tropical peoples. Eur. J. Clin. Nutr. 1991, 45, 177–185. [Google Scholar] [PubMed]
- Henry, C.J. Basal metabolic rate studies in humans: Measurement and development of new equations. Pub. Health Nutr. 2005, 8, 1133–1152. [Google Scholar] [CrossRef] [PubMed]
- The BMJ. Correlation and Regression. Available online: https://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one/11-correlation-and-regression (accessed on 30 December 2020).
- Flack, K.D.; Siders, W.A.; Johnson, L.; Roemmich, J.N. Cross-Validation of Resting Metabolic Rate Prediction Equations. J. Acad. Nutr. Diet. 2016, 116, 1413–1422. [Google Scholar] [CrossRef] [PubMed]
- Schusdziarra, V.; Wolfschläger, K.; Hausmann, M.; Wagenpfeil, S.; Erdmann, J. Accuracy of Resting Energy Expenditure Calculations in Unselected Overweight and Obese Patients. Ann. Nutr. Metab. 2014, 65, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Galgani, J.E.; Castro-Sepulveda, M.; Pérez-Luco, C.; Fernández-Verdejo, R. Validity of predictive equations for resting metabolic rate in healthy humans. Clin. Sci. (London) 2018, 132, 1741–1751. [Google Scholar] [CrossRef]
- Willis, E.A.; Herrmann, S.D.; Ptomey, L.T.; Honas, J.J.; Bessmer, C.T.; Donnelly, J.E.; Washbum, R.A. Predicting resting energy expenditure in young adults. Obes. Res. Clin. Pract. 2016, 10, 304–314. [Google Scholar] [CrossRef]
- de la Cruz, S.; de Mateo, B.; Camina, M.A.; Carreño, L.; Miján, A.; Galgani, J.E.; Redondo, M.A. Agreement between indirect calorimetry and predictive equations in a sample of spanish healthy adults. Nutr. Hosp. 2015, 32, 888–896. [Google Scholar]
- Jésus, P.; Achamrah, N.; Grigioni, S.; Charles, J.; Rimbert, A.; Folope, V.; Petit, A.; Déchelotte, P.; Coëffier, M. Validity of predictive equations for resting energy expenditure according to the body mass index in a population of 1726 patients followed in a Nutrition Unit. Clin. Nutr. 2015, 34, 529–535. [Google Scholar] [CrossRef]
- Poli, V.F.; Sanches, R.B.; Moraes, A.D.; Fidalgo, J.P.; Nascimiento, M.A.; Andrade-Silva, S.G.; Clemente, J.C.; Yi, L.C.; Caranti, D.A. Resting energy expenditure in obese women: Comparison between measured and estimated values. Br. J. Nutr. 2016, 116, 1306–1313. [Google Scholar] [CrossRef]
- Namazi, N.; Aliasgharzadeh, S.; Mahdavi, R.; Kolahdooz, F. Accuracy of the Common Predictive Equations for Estimating Resting Energy Expenditure among Normal and Overweight Girl University Students. J. Am. Coll. Nutr. 2016, 35, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Olivier, N.; Wenhold, F.A.M.; Becker, P. Resting Energy Expenditure of Black Overweight Women in South Africa Is Lower than of White Women. Ann. Nutr. Metab. 2016, 69, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Tershakovec, A.M.; Kuppler, K.M.; Zemel, B.; Stallings, V.A. Age, sex, ethnicity, body composition, and resting energy expenditure of obese African American and white children and adolescents. Am. J. Clin. Nutr. 2002, 75, 867–871. [Google Scholar] [CrossRef] [PubMed]
- Luke, A.; Dugas, L.; Kramer, H. Ethnicity, energy expenditure and obesity: Are the observed black/white differences meaningful? Curr. Opin. Endocrinol. Diabetes Obes. 2007, 14, 370–373. [Google Scholar] [CrossRef] [PubMed]
- Wouters-Adriaens, M.P.; Westerterp, K.R. Low resting energy expenditure in Asians can be attributed to body composition. Obesity (Silver Spring) 2008, 16, 2212–2216. [Google Scholar] [CrossRef]
- Spaeth, A.M.; Dinges, D.F.; Goel, N. Resting metabolic rate varies by race and by sleep duration. Obesity (Silver Spring) 2015, 23, 2349–2356. [Google Scholar] [CrossRef] [PubMed]
- Martin, K.; Wallace, P.; Rust, P.F.; Garvey, W.T. Estimation of resting energy expenditure considering effects of race and diabetes status. Diabetes Care 2004, 27, 1405–1511. [Google Scholar] [CrossRef]
- Reneau, J.; Obi, B.; Moosreiner, A.; Kidambi, S. Do we need race-specific resting metabolic rate prediction equations? Nutr. Diabetes 2019, 9, 1–8. [Google Scholar] [CrossRef]
- Castellucci, H.I.; Viviani, C.A.; Molenbroek, J.F.M.; Arezes, P.M.; Martínez, M.; Aparici, V.; Bragança, S. Anthropometric characteristics of Chilean workers for ergonomic and design purposes. Ergonomics 2019, 62, 459–474. [Google Scholar] [CrossRef]
- Vanegas, J.; Villalón, M.; Valenzuela, C. Consideraciones acerca del uso de la variable etnia/raza en investigación epidemiológica para la Salud Pública: A propósito de investigaciones en inequidades. Rev. Med. Chile 2008, 136, 637–644. [Google Scholar] [CrossRef][Green Version]
- Wahrlich, V.; Teixeira, T.M.; Anjos, L. Validity of a population-specific BMR predictive equation for adults from an urban tropical setting. Clin. Nutr. 2018, 37, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Quiroz-Olguín, G.; Serralde-Zúñiga, A.E.; Saldaña-Morales, M.V.; Gulias-Herrero, A.; Guevara-Cruz, M. Validating an energy expenditure prediction equation in overweight and obese Mexican patients. Nutr. Hosp. 2014, 30, 749–755. [Google Scholar] [PubMed]
- Cruz, S.; Mateo, B.; Camina, M.A.; Carreño, L.; Miján, A.; Galgani, J.E.; Redondo, M.A. Proposal for a new formula for estimating resting energy expenditure for healthy spanish population. Nutr. Hosp. 2015, 32, 2346–2352. [Google Scholar]
- Aristizabal, J.C.; Freidenreich, D.J.; Volk, B.M.; Kupchak, B.R.; Saenz, C.; Maresh, C.M.; Kraemer, W.J.; Volek, J.S. Effect of resistance training on resting metabolic rate and its estimation by a dual-energy X-ray absorptiometry metabolic map. Eur. J. Clin. Nutr. 2015, 69, 831–836. [Google Scholar] [CrossRef] [PubMed]
- Marzullo, P.; Minocci, A.; Mele, C.; Fessehatsion, R.; Tagliaferri, M.; Pagano, L.; Scacchi, M.; Aimaretti, G.; Sartorio, A. The relationship between resting energy expenditure and thyroid hormones in response to short-term weight loss in severe obesity. PLoS ONE 2018, 13, e0205293. [Google Scholar] [CrossRef]
- Chung, I.Y.; Jung, M.; Lee, S.B.; Lee, J.W.; Park, Y.R.; Cho, D.; Chung, H.; Youn, S.; Min, Y.H.; Park, H.J.; et al. An Assessment of Physical Activity Data Collected via a Smartphone App and a Smart Band in Breast Cancer Survivors: Observational Study. J. Med. Internet Res. 2019, 21, 13463. [Google Scholar] [CrossRef]
- Massarini, S.; Ferrulli, A.; Ambrogi, F.; Macrì, C.; Terruzzi, I.; Benedini, S.; Luzi, L. Routine resting energy expenditure measurement increases effectiveness of dietary intervention in obesity. Acta Diabetol. 2017, 55, 75–85. [Google Scholar] [CrossRef]
- Steemburgo, T.; Lazzari, C.; Farinha, J.B.; Pedroso, T.; Vercoza, L.; Reischak, A.; Jobim, M. Basal metabolic rate in Brazilian patients with type 2 diabetes: Comparison between measured and estimated values. Arch. Endocrinol. Metab. 2019, 63, 53–61. [Google Scholar] [CrossRef]
- Broskey, N.T.; Klempel, M.C.; Gilmore, L.A.; Sutton, E.F.; Altazan, A.D.; Burton, J.H.; Ravussin, E.; Redman, L.M. Assessing Energy Requirements in Women with Polycystic Ovary Syndrome: A Comparison Against Doubly Labeled Water. J. Clin. Endocrinol. Metab. 2017, 102, 1951–1959. [Google Scholar] [CrossRef][Green Version]
- Sousa, T.M.; Maioli, T.U.; Santos, A.L.S.; Santos, L.C. Energy expenditure in the immediate postpartum period: Indirect calorimetry versus predictive equations. Nutrition 2017, 39, 36–42. [Google Scholar] [CrossRef]
- Pereira, C.; Ceolin, A.L.; Toulson, M.I. Energy expenditure in women with breast cancer. Nutrition 2015, 31, 556–559. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).