Faith in Fat: A Multisite Examination of University Students’ Perceptions of Fat in the Diet
Abstract
1. Introduction
2. Materials and Methods
2.1. Faith in Fat Study Description
2.2. Ethics
2.3. Statistical Analysis
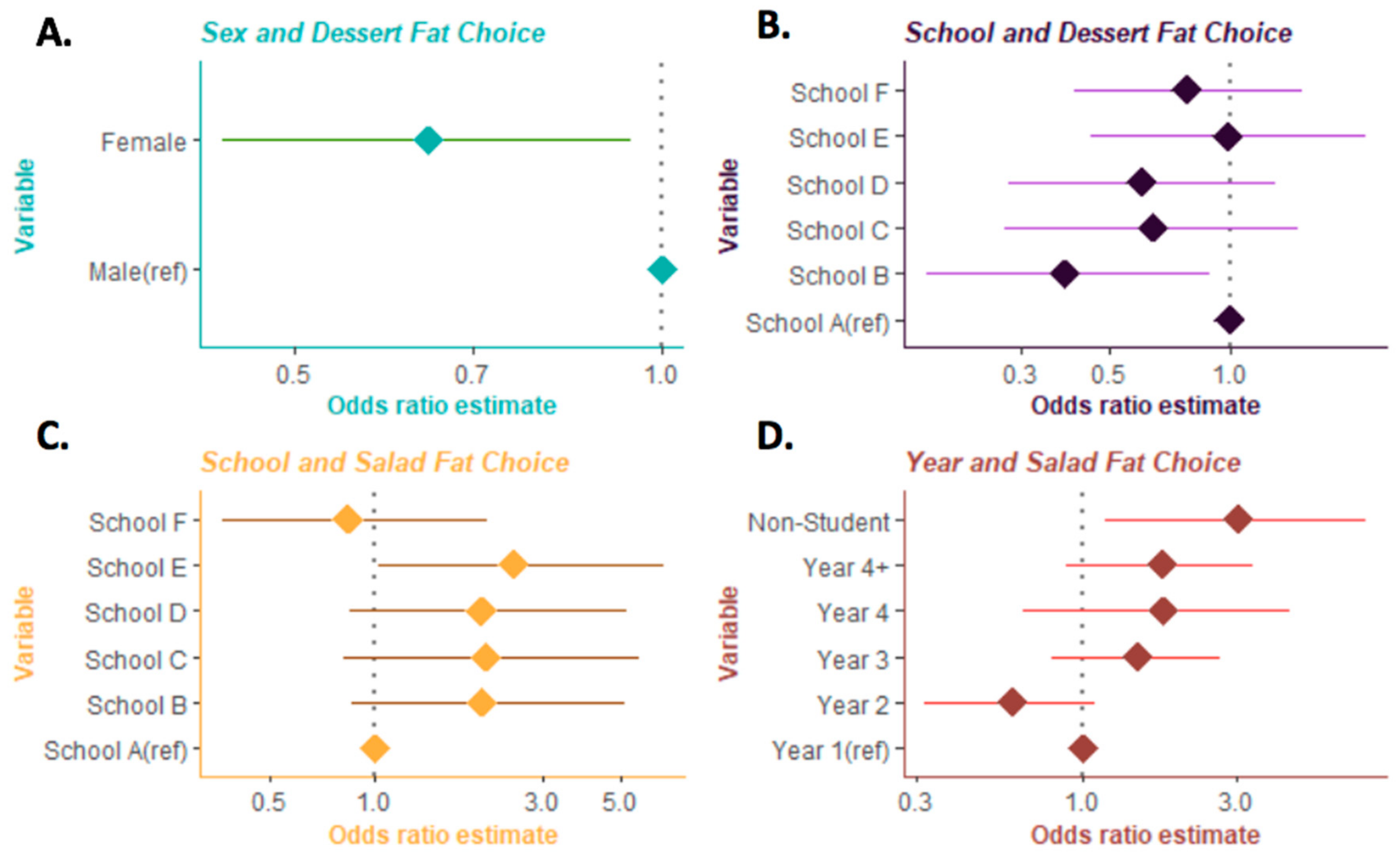
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Johnson, E.J.; Mohn, E.S. Fat-Soluble Vitamins. Nutr. Growth 2014, 111, 38–44. [Google Scholar] [CrossRef]
- Failla, M.L.; Chitchumronchokchai, C.; Ferruzzi, M.; Goltz, S.R.; Campbell, W.W. Unsaturated fatty acids promote bioaccessibility and basolateral secretion of carotenoids and α-tocopherol by Caco-2 cells. Food Funct. 2014, 5, 1101–1112. [Google Scholar] [CrossRef] [PubMed]
- Montmayeur, J.; le Coutre, J. Fat Detection: Taste, Texture, and Post Ingestive; CRC Press: Boca Raton, Fl, USA, 2010. [Google Scholar]
- Mela, D.J. The basis of dietary fat preferences. Trends Food Sci. Technol. 1990, 1, 71–73. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Ludwig, D.S. The 2015 US Dietary Guidelines: Lifting the Ban on Total Dietary Fat. JAMA 2015, 313, 2421–2422. [Google Scholar] [CrossRef] [PubMed]
- Gifford, K.D. Dietary fats, eating guides, and public policy: History, critique, and recommendations. Am. J. Med. 2002, 113, 89–106. [Google Scholar] [CrossRef]
- La Berge, A. How the ideology of low fat conquered america. J. Hist. Med. Allied Sci. 2007, 63, 139–177. [Google Scholar] [CrossRef]
- US Department of Health and Human Services; US Department of Agriculture. Dietary Guidelines for Americans 2015–2020, 8th ed.; US Government Printing Office: Washington, DC, USA, 2015. [Google Scholar]
- Dietary Guidelines Advisory Committee. Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Agriculture and the Secretary of Health and Human Services; U.S. Department of Agriculture, Agricultural Research Service: Washington, DC, USA, 2020. [Google Scholar]
- Astrup, A.; Magkos, F.; Bier, D.M.; Brenna, J.T.; Otto, M.C.D.O.; Hill, J.O.; King, J.C.; Mente, A.; Ordovas, J.M.; Volek, J.S.; et al. Saturated Fats and Health: A Reassessment and Proposal for Food-Based Recommendations. J. Am. Coll. Cardiol. 2020, 76, 844–857. [Google Scholar] [CrossRef]
- Eckel, R.H.; Kris-Etherton, P.; Lichtenstein, A.H.; Wylie-Rosett, J.; Groom, A.; Stitzel, K.F.; Yin-Piazza, S. Americans’ Awareness, Knowledge, and Behaviors Regarding Fats: 2006-2007. J. Am. Diet. Assoc. 2009, 109, 288–296. [Google Scholar] [CrossRef]
- Dickson-Spillmann, M.; Siegrist, M. Consumers’ knowledge of healthy diets and its correlation with dietary behaviour. J. Hum. Nutr. Diet. 2010, 24, 54–60. [Google Scholar] [CrossRef]
- Diekman, C.; Malcolm, K. Consumer Perception and Insights on Fats and Fatty Acids: Knowledge on the Quality of Diet Fat. Ann. Nutr. Metab. 2009, 54 (Suppl. S1), 25–32. [Google Scholar] [CrossRef]
- Colby, S.; Johnson, L.; Scheett, A.; Hoverson, B. Nutrition Marketing on Food Labels. J. Nutr. Educ. Behav. 2010, 42, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-T.J.; Yen, S.T. Knowledge of Dietary Fats among US Consumers. J. Am. Diet. Assoc. 2010, 110, 613–618. [Google Scholar] [CrossRef] [PubMed]
- Schapira, D.V.; Kumar, N.B.; Lyman, G.H.; McMillan, S.C. The value of current nutrition information. Prev. Med. 1990, 19, 45–53. [Google Scholar] [CrossRef]
- Nelson, M.C.; Story, M.; Larson, N.I.; Neumark-Sztainer, D.; Lytle, L.A. Emerging Adulthood and College-aged Youth: An Overlooked Age for Weight-related Behavior Change. Obesity 2008, 16, 2205–2211. [Google Scholar] [CrossRef]
- Unusan, N. University students’ food preference and practice now and during childhood. Food Qual. Preference 2006, 17, 362–368. [Google Scholar] [CrossRef]
- Carpenter, J. Nutrition Education in Public Elementary and Secondary Schools; U.S. Department of Education Office of Educational Research and Improvement: Washington, DC, USA, 1996; p. 64. [Google Scholar]
- Davy, S.R.; Benes, B.A.; Driskell, J.A. Sex Differences in Dieting Trends, Eating Habits, and Nutrition Beliefs of a Group of Midwestern College Students. J. Am. Diet. Assoc. 2006, 106, 1673–1677. [Google Scholar] [CrossRef]
- Steptoe, A.; Wardle, J.; Cui, W.; Bellisle, F.; Zotti, A.M.; Baranyai, R.; Sanderman, R. Trends in smoking, diet, physical exercise, and attitudes toward health in European university students from 13 countries, 1990–2000. Prev. Med. 2002, 35, 97–104. [Google Scholar] [CrossRef]
- Jasti, S.; Kovács, S. Use of Trans Fat Information on Food Labels and Its Determinants in a Multiethnic College Student Population. J. Nutr. Educ. Behav. 2010, 42, 307–314. [Google Scholar] [CrossRef]
- Fernandes, A.C.; de Oliveira, R.C.; Rodrigues, V.M.; Fiates, G.M.; da Costa Proenca, R.P. Perceptions of university students regarding calories, food healthiness, and the importance of calorie information in menu labelling. Appetite 2015, 91, 173–178. [Google Scholar] [CrossRef]
- Banna, J.C.; Gilliland, B.; Keefe, M.; Zheng, D. Cross-cultural comparison of perspectives on healthy eating among Chinese and American undergraduate students. BMC Public Health 2016, 16, 1015. [Google Scholar] [CrossRef]
- Lipsky, L.M.; Nansel, T.R.; Haynie, D.; Liu, D.; Li, K.; Pratt, C.A.; Iannotti, R.J.; Dempster, K.; Simons-Morton, B. Diet quality of US adolescents during the transition to adulthood: Changes and predictors. Am. J. Clin. Nutr. 2017, 105, 1424–1432. [Google Scholar] [CrossRef] [PubMed]
- Landry, M.; Asigbee, F.M.; Vandyousefi, S.; Khazaee, E.; Ghaddar, R.; Boisseau, J.B.; House, B.T.; Davis, J.N. Diet Quality Is an Indicator of Disease Risk Factors in Hispanic College Freshmen. J. Acad. Nutr. Diet. 2019, 119, 760–768. [Google Scholar] [CrossRef] [PubMed]
- The Culinary Institute of America. Menus of Change. Available online: https://www.menusofchange.org/ (accessed on 31 May 2020).
- The Culinary Institute of America. The Menus of Change University Research Collaborative. Available online: https://www.moccollaborative.org/ (accessed on 31 May 2020).
- Shan, Z.; Rehm, C.D.; Rogers, G.; Ruan, M.; Wang, D.D.; Hu, F.B.; Mozaffarian, D.; Zhang, F.F.; Bhupathiraju, S.N. Trends in Dietary Carbohydrate, Protein, and Fat Intake and Diet Quality Among US Adults, 1999–2016. JAMA 2019, 322, 1178–1187. [Google Scholar] [CrossRef] [PubMed]
- Austin, G.L.; Ogden, L.G.; Hill, J.O. Trends in carbohydrate, fat, and protein intakes and association with energy intake in normal-weight, overweight, and obese individuals: 1971–2006. Am. J. Clin. Nutr. 2011, 93, 836–843. [Google Scholar] [CrossRef] [PubMed]
- Fryar, C.D.; Carroll, M.D.; Ogden, C.L. Prevalence of Overweight, Obesity, and Extreme Obesity among Adults: United States, Trends 1960–1962 through 2009–2010; National Center for Health Statistics: Hyattsville, MD, USA, 2012. [Google Scholar]
- Sacks, F.M.; Lichtenstein, A.H.; Wu, J.H.; Appel, L.J.; Creager, M.A.; Kris-Etherton, P.M.; Miller, M.; Rimm, E.B.; Rudel, L.L.; Robinson, J.G.; et al. Dietary fats and cardiovascular disease: A presidential advisory from the American Heart Association. Circulation 2017, 136, e1–e23. [Google Scholar] [CrossRef] [PubMed]
- Hooper, L.; Martin, N.; Jimoh, O.F.; Kirk, C.; Foster, E.; Abdelhamid, A.S. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Syst. Rev. 2020, 5, CD011737. [Google Scholar] [CrossRef]
- Lusk, J.L. Consumer beliefs about healthy foods and diets. PLoS ONE 2019, 14, e0223098. [Google Scholar] [CrossRef]
- Gallup. Americans Divided on Leaving Fat, Sugar, Salt Off the Plate. Available online: https://news.gallup.com/poll/240635/americans-divided-leaving-fat-sugar-salt-off-plate.aspx (accessed on 31 May 2020).
- Kalra, S.; Singla, R.; Rosha, R.; Dhawan, M. Ketogenic diet: Situational analysis of current nutrition guidelines. J. Pak. Med. Assoc. 2018, 68, 1836–1839. [Google Scholar]
- Ludwig, D.S. The Ketogenic Diet: Evidence for Optimism but High-Quality Research Needed. J. Nutr. 2019, 150, 1354–1359. [Google Scholar] [CrossRef]
- Boek, S.; Bianco-Simeral, S.; Chan, K.; Goto, K. Gender and Race are Significant Determinants of Students’ Food Choices on a College Campus. J. Nutr. Educ. Behav. 2012, 44, 372–378. [Google Scholar] [CrossRef]
- Liebman, M.; Cameron, B.; Carson, D.; Brown, D.; Meyer, S. Dietary fat reduction behaviors in college students: Relationship to dieting status, gender and key psychosocial variables. Appetite 2001, 36, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Barker, M.E.; Tandy, M.; Stookey, J. How are Consumers of Low-fat and High-fat Diets Perceived by those with Lower and Higher Fat Intake? Appetite 1999, 33, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, D.M.; Laney, C.; Morris, E.K.; Loftus, E.F. False beliefs about fattening foods can have healthy consequences. Proc. Natl. Acad. Sci. USA 2005, 102, 13724–13731. [Google Scholar] [CrossRef]
- Gillen, M.M.; Lefkowitz, E.S. Gender and racial/ethnic differences in body image development among college students. Body Image 2012, 9, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Wardle, J.; Haase, A.M.; Steptoe, A.; Nillapun, M.; Jonwutiwes, K.; Bellisie, F. Gender differences in food choice: The contribution of health beliefs and dieting. Ann. Behav. Med. 2004, 27, 107–116. [Google Scholar] [CrossRef]
- White, W.S.; Zhou, Y.; Crane, A.; Dixon, P.; Quadt, F.; Flendrig, L.M. Modeling the dose effects of soybean oil in salad dressing on carotenoid and fat-soluble vitamin bioavailability in salad vegetables. Am. J. Clin. Nutr. 2017, 106, 1041–1051. [Google Scholar] [CrossRef]
- Tobias, D.K.; Chen, M.; Manson, J.E.; Ludwig, D.S.; Willett, W.; Hu, F.B. Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: A systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015, 3, 968–979. [Google Scholar] [CrossRef]
- Van Horn, L.; Carson, J.A.S.; Appel, L.J.; Burke, L.E.; Economos, C.; Karmally, W.; Lancaster, K.; Lichtenstein, A.H.; Johnson, R.K.; Thomas, R.J.; et al. Recommended Dietary Pattern to Achieve Adherence to the American Heart Association/American College of Cardiology (AHA/ACC) Guidelines: A Scientific Statement From the American Heart Association. Circulation 2016, 134, e505–e529. [Google Scholar] [CrossRef]
- Vannice, G.; Rasmussen, H. Position of the Academy of Nutrition and Dietetics: Dietary Fatty Acids for Healthy Adults. J. Acad. Nutr. Diet. 2014, 114, 136–153. [Google Scholar] [CrossRef]
- Yahia, N.; Brown, C.A.; Rapley, M.; Chung, M. Level of nutrition knowledge and its association with fat consumption among college students. BMC Public Health 2016, 16, 1047. [Google Scholar] [CrossRef]
- Carmona, R.H. Health literacy: A national priority. J. Gen. Intern. Med. 2006, 21, 803. [Google Scholar] [CrossRef]
- Liu, A.G.; Ford, N.A.; Hu, F.B.; Zelman, K.M.; Mozaffarian, D.; Kris-Etherton, P.M. A healthy approach to dietary fats: Understanding the science and taking action to reduce consumer confusion. Nutr. J. 2017, 16, 53. [Google Scholar] [CrossRef] [PubMed]
- De Castro, J.M. Eating behavior: Lessons from the real world of humans. Nutrition 2000, 16, 800–813. [Google Scholar] [CrossRef]
- Venn-Watson, S.; Lumpkin, R.; Dennis, E.A. Efficacy of dietary odd-chain saturated fatty acid pentadecanoic acid parallels broad associated health benefits in humans: Could it be essential? Sci. Rep. 2020, 10, 8161. [Google Scholar] [CrossRef]
- Forouhi, N.G.; Krauss, R.M.; Taubes, G.; Willett, W. Dietary fat and cardiometabolic health: Evidence, controversies, and consensus for guidance. BMJ 2018, 361, k2139. [Google Scholar] [CrossRef]
- Walker, T.B.; Parker, M.J. Lessons from the War on Dietary Fat. J. Am. Coll. Nutr. 2014, 33, 347–351. [Google Scholar] [CrossRef]
- Wang, D.D.; Hu, F.B. Dietary Fat and Risk of Cardiovascular Disease: Recent Controversies and Advances. Annu. Rev. Nutr. 2017, 37, 423–446. [Google Scholar] [CrossRef]
- Imamura, F.; Micha, R.; Wu, J.H.; Otto, M.C.D.O.; Otite, F.O.; Abioye, A.I.; Mozaffarian, D. Effects of Saturated Fat, Polyunsaturated Fat, Monounsaturated Fat, and Carbohydrate on Glucose-Insulin Homeostasis: A Systematic Review and Meta-analysis of Randomised Controlled Feeding Trials. PLoS Med. 2016, 13, e1002087. [Google Scholar] [CrossRef]

| Food Item | No-Fat Option | Unsaturated Fat Option | Saturated Fat Option |
|---|---|---|---|
| Garden Salad | Lemon Juice Dressing | Olive Oil Dressing | Ranch Dressing |
| Chicken Breast Entree | Baked with Italian Herbs | Sautéed in Olive Oil | Sautéed in a Lemon Butter Caper Sauce |
| Oatmeal Cookie Dessert | Prepared with Applesauce | Prepared with Olive Oil | Prepared with Butter |
| Characteristic | All Schools | School A | School B | School C | School D | School E | School F |
|---|---|---|---|---|---|---|---|
| Sample (n) | 533 | 52 | 88 | 54 | 81 | 57 | 201 |
| Sex (%) | |||||||
| Male | 52.2 | 63.5 | 54.6 | 48.2 | 43.2 | 64.9 | 49.3 |
| Female | 47.7 | 34.6 | 45.5 | 51.9 | 56.8 | 35.1 | 50.8 |
| Not Listed | 0.1 | 1.9 | 0 | 0 | 0 | 0 | 0 |
| Classification (%) | |||||||
| First Year | 43.0 | 42.3 | 19.3 | 42.6 | 93.8 | 14.0 | 41.3 |
| Second Year | 24.8 | 25.0 | 27.3 | 33.3 | 2.5 | 14.0 | 33.3 |
| Third Year | 14.1 | 11.5 | 21.6 | 9.3 | 2.5 | 17.5 | 16.4 |
| Fourth Year | 9.9 | 7.7 | 25.0 | 9.3 | 1.2 | 7.0 | 8.5 |
| >Fourth Year | 4.3 | 1.9 | 5.7 | 1.9 | 0 | 21.1 | 0.5 |
| Not a Student | 3.9 | 3.9 | 1.1 | 3.7 | 0 | 26.3 | 0 |
| Meal Type | Sex | Year Classification | School | |||
|---|---|---|---|---|---|---|
| χ2 | p-Value | χ2 | p-Value | χ2 | p-Value | |
| Garden Salad | 2.5 | 0.64 | 19.6 | 0.03 | 44.0 | <0.001 |
| Chicken Breast Entree | 6.9 | 0.14 | 16.4 | 0.09 | 51.2 | <0.001 |
| Oatmeal Cookie Dessert | 12.1 | 0.02 | 8.7 | 0.57 | 11.0 | 0.36 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Landry, M.J.; Olvany, J.M.; Mueller, M.P.; Chen, T.; Ikeda, D.; Sinclair, D.; Schatz, L.E.; Connors, P.; Valgenti, R.T.; Amsler Challamel, G.; et al. Faith in Fat: A Multisite Examination of University Students’ Perceptions of Fat in the Diet. Nutrients 2020, 12, 2560. https://doi.org/10.3390/nu12092560
Landry MJ, Olvany JM, Mueller MP, Chen T, Ikeda D, Sinclair D, Schatz LE, Connors P, Valgenti RT, Amsler Challamel G, et al. Faith in Fat: A Multisite Examination of University Students’ Perceptions of Fat in the Diet. Nutrients. 2020; 12(9):2560. https://doi.org/10.3390/nu12092560
Chicago/Turabian StyleLandry, Matthew J., Jasmine M. Olvany, Megan P. Mueller, Tiffany Chen, Dana Ikeda, Danielle Sinclair, Lesley E. Schatz, Priscilla Connors, Robert T. Valgenti, Ghislaine Amsler Challamel, and et al. 2020. "Faith in Fat: A Multisite Examination of University Students’ Perceptions of Fat in the Diet" Nutrients 12, no. 9: 2560. https://doi.org/10.3390/nu12092560
APA StyleLandry, M. J., Olvany, J. M., Mueller, M. P., Chen, T., Ikeda, D., Sinclair, D., Schatz, L. E., Connors, P., Valgenti, R. T., Amsler Challamel, G., Gardner, C. D., & Policastro, P. (2020). Faith in Fat: A Multisite Examination of University Students’ Perceptions of Fat in the Diet. Nutrients, 12(9), 2560. https://doi.org/10.3390/nu12092560








