Fit for the Future? A New Approach in the Debate about What Makes Healthcare Systems Really Sustainable
Abstract
:1. Introduction
2. Methods
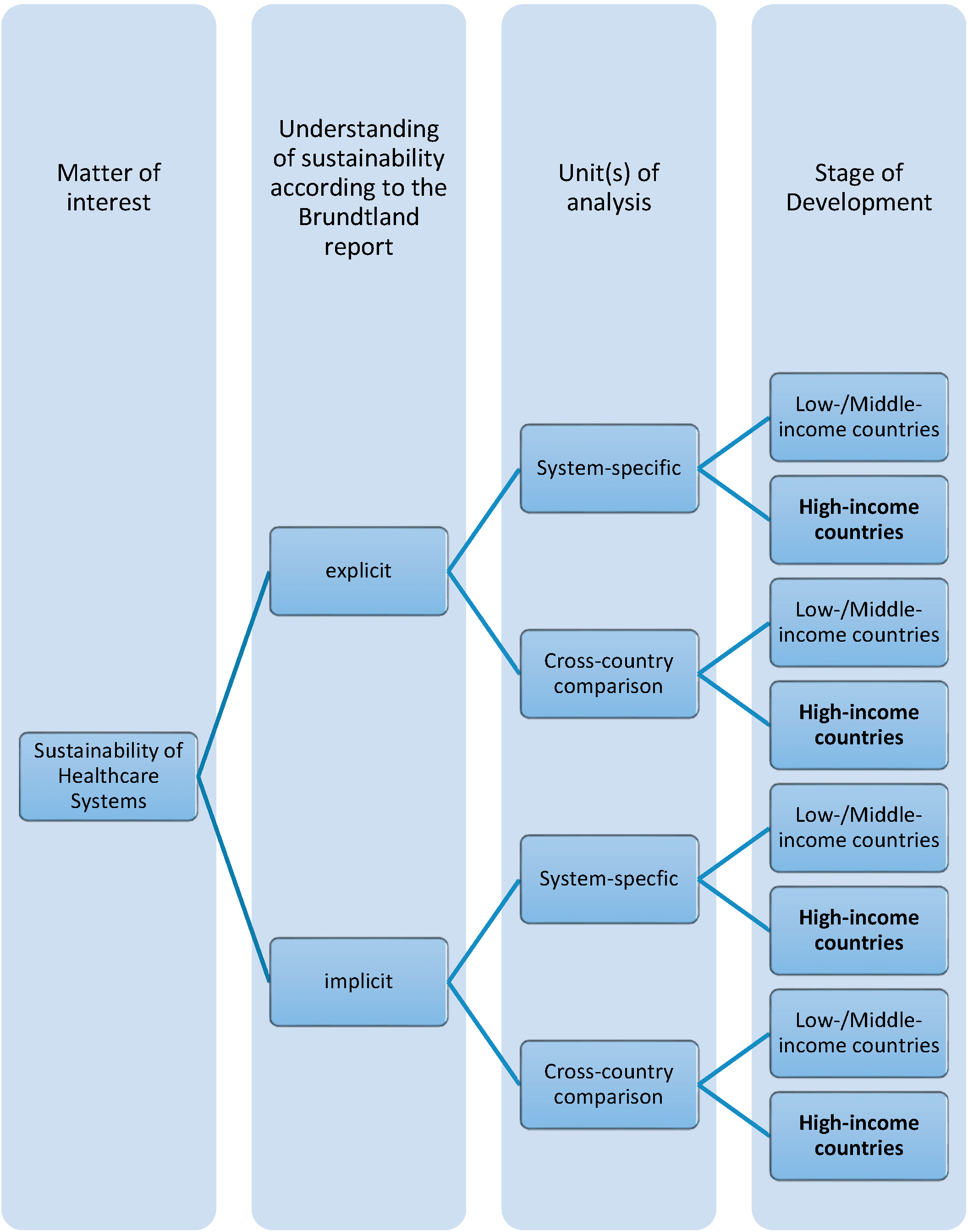
3. Defining Sustainable Healthcare Systems
4. Characterizing Sustainable Healthcare Systems—Existing Approaches
4.1. System-Specific Approach with an Explicit Reference to the Brundtland Report
|
|
|
|
|
|
|
|
|
|
|
4.2. Cross-Country-Comparison Approach with an Explicit Reference to the Brundtland Report
4.3. System-Specific Approach with an Implicit Reference to the Brundtland Report
4.4. Cross-Country-Comparison Approach with an Implicit Reference to the Brundtland Report
|
|
|
|
|
|
|
|
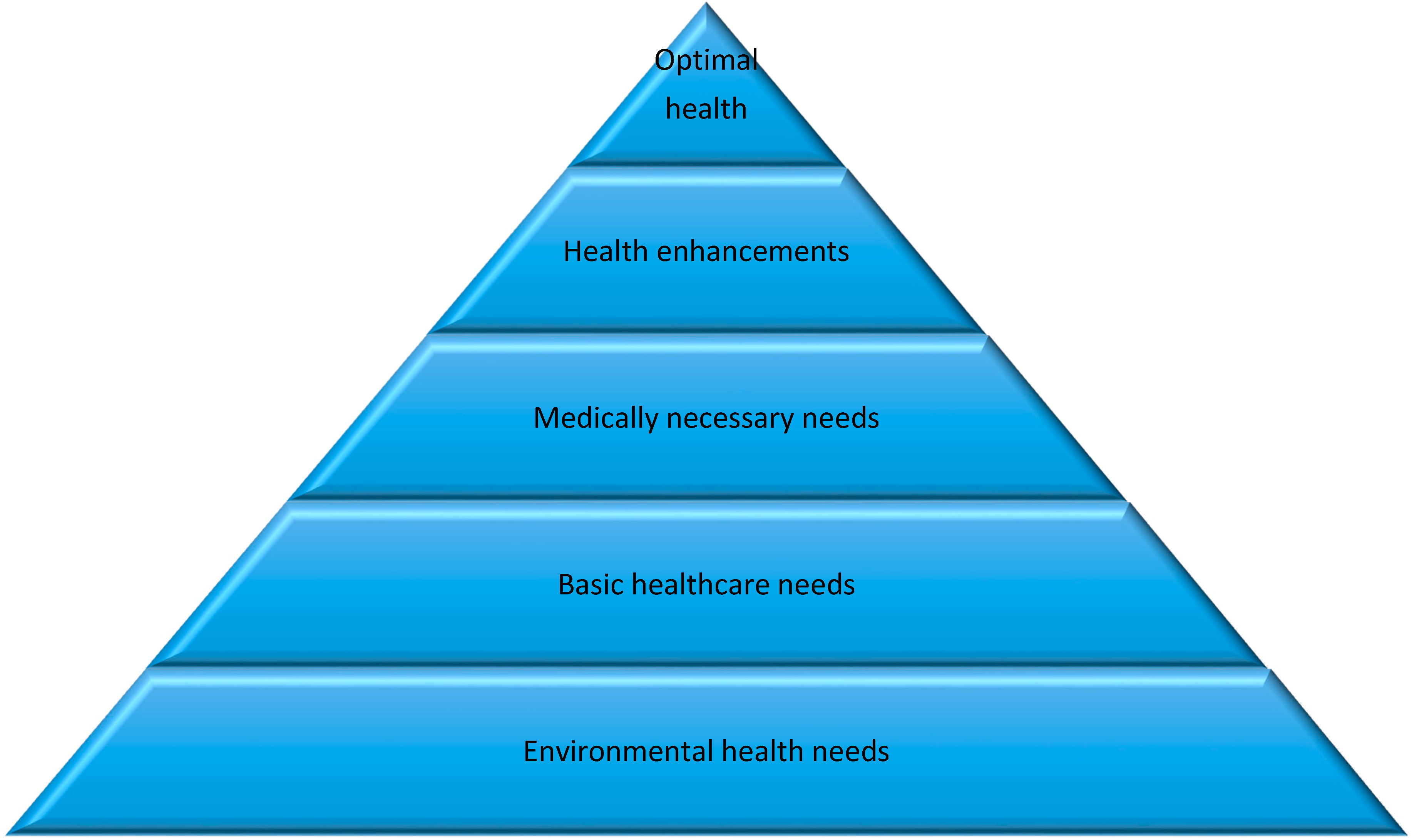
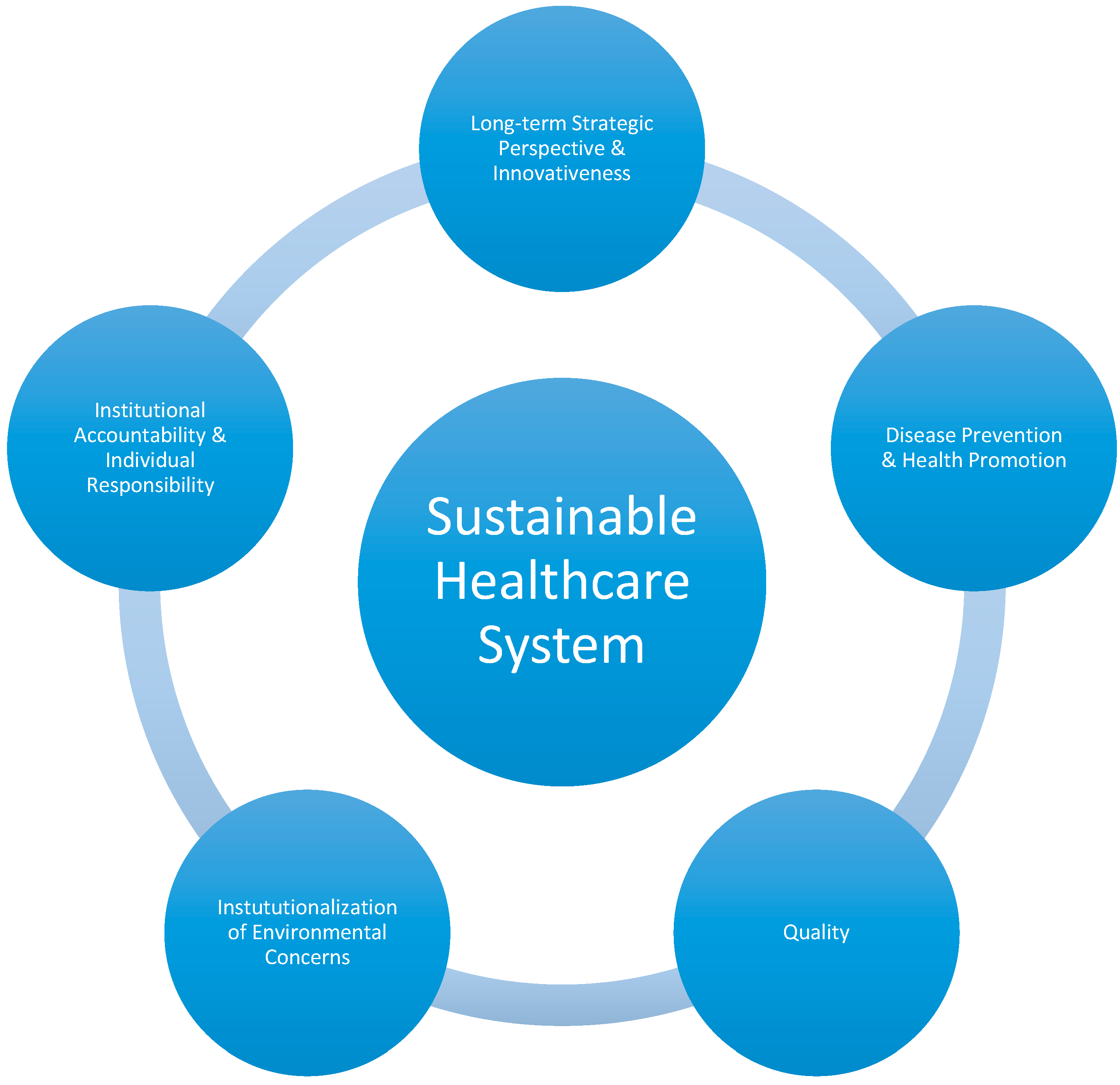
5. Relevant Dimensions for Sustainable Healthcare Systems—Conceptual Framework
5.1. Long-Term Strategic Perspective and Innovativeness
5.2. Disease Prevention and Health Promotion
5.3. Quality
5.4. Institutionalization of Environmental Concerns
5.5. Institutional Accountability and Individual Responsibility
6. Discussion and Conclusions
Acknowledgments
Conflicts of Interest
References
- Coiera, E.; Hovenga, E. Building a Sustainable Health System. In IMIA Yearbook of Medical Informatics: Biomedical Informatics for Sustainable Health Systems; Geissbuhler, A., Haux, R., Kulikowski, C., Eds.; Schattauer: Celle, Germany, 2007; pp. 11–18. [Google Scholar]
- Braun, A.; Rijkers-Defrasne, S.; Zweck, A.; Butter, M.; Dumay, A.; Leis, M. Special Issue on Health Care. Healthy Ageing and the Future of Public Healthcare Systems; European Comission Directorate-General for Research: Brussels, Belgium, 2009. [Google Scholar]
- European Commission. The European Union Explained: Public Health Improving Health for All EU Citizens; European Commission, Directorate-General for Communication: Brussels, Belgium, 2014. [Google Scholar]
- Report of the World Commission on Environment and Development: Our Common Future. Available online: http://www.un-documents.net/our-common-future.pdf (accessed on 12 December 2014).
- Arah, O.A.; Westert, G.P.; Hurst, J.; Klazinga, N.S. A conceptual framework for the OECD health care quality indicators project. Int. J. Qual. Health Care 2006, 18, (Suppl. 1). 5–13. [Google Scholar] [CrossRef]
- Faezipour, M.; Ferreira, S. Applying systems thinking to assess sustainability in healthcare system of systems. IJSSE 2006, 2, 290–308. [Google Scholar] [CrossRef]
- Berman, P. Health sector reform: Making health development sustainable. Health Policy 1995, 32, 13–28. [Google Scholar] [CrossRef] [PubMed]
- Hudson, C.G.; Vissing, Y.M. Sustainability at the Edge of Chaos: Its Limits and Possibilities in Public Health. BMRI 2013, 2013. Article 801614. [Google Scholar]
- Mackay, R.; Wolbring, G. Sustainable Consumption of Healthcare: Linking Sustainable Consumption with Sustainable Healthcare and Health Consumer Discourses. Available online: http://www.sciforum.net/conference/wsf3/paper/2162 (accessed on 12 December 2014).
- World Health Organization (WHO). The World Health Report 2000. Health Systems: Improving Performance; WHO: Geneva, Switzerland, 2000. [Google Scholar]
- Grad, F.P. The Preamble of the Constitution of the World Health Organization. Bull. World Health Organ. 2002, 80, 981–982. [Google Scholar] [PubMed]
- Plsek, P.E.; Greenhalgh, T. The challenge of complexity in health care. BMJ 2001, 323, 625–628. [Google Scholar] [CrossRef]
- Muzyka, D.; Hodgson, G.; Prada, G. The Inconvenient Truths about Canadian Health Care. Available online: http://www.conferenceboard.ca/cashc/research/2012/inconvenient_truths.aspx (accessed on 12 December 2014).
- Harrison, A.; Dixon, J.; New, B.; Judge, K. Funding the NHS. Is the NHS sustainable? BMJ 1997, 314, 296–298. [Google Scholar] [CrossRef] [PubMed]
- Henke, K.D.; Schreyögg, J. Towards Sustainable Health Care Systems: Strategies in Health Insurance Schemes in France, Germany, Japan and The Netherlands; International Social Security Association: Geneva, Switzerland, 2005. (In German) [Google Scholar]
- Lewis, S.; Donaldson, C.; Mitton, C.; Currie, G. The future of health care in Canada. BMJ 2001, 323, 926–929. [Google Scholar] [CrossRef] [PubMed]
- Jameton, A.; McGuire, C. Toward sustainable health-care services: Principles, challenges, and a process. IJSHE 2002, 3, 113–127. [Google Scholar]
- Schön, R. Nachhaltiges Gesundheitswesen. Für eine gesunde Zukunft, für ein zukunftsfähiges Gesundheitswesen; Zentrum BATS: Zurich, Switzerland, 2004. (In German) [Google Scholar]
- Alliance for Natural Health (ANH). Sustainable Healthcare—Working Towards the Paradigm Shift. White Paper (June 2010 Update); Alliance for Natural Health: Dorking, UK, 2010. [Google Scholar]
- Grunwald, A.; Kopfmüller, J. Nachhaltigkeit; Campus: Frankfurt am Main, Germany, 2006. (In German) [Google Scholar]
- Prada, G. Sustainability: What Does This Mean for Canada’s Health Care Systems. In Proceedings of the Collaborative Meeting of the Conference Board of Canada’s Health-Related Executive Networks, Toronto, ON, Canada, 16 April 2012.
- Faezipour, M.; Ferreira, S. A system dynamics perspective of patient satisfaction in healthcare. Procedia Comput. Sci. 2013, 16, 148–156. [Google Scholar] [CrossRef]
- European Commission. Sustainable Development in the European Union—2011 Monitoring Report of the EU Sustainable Development Strategy; Publications Office of the European Union: Luxembourg, Luxembourg, 2011. [Google Scholar]
- Stuart, N.; Adams, J. The Sustainability of Canada’s Healthcare System: A Framework for Advancing the Debate. Healthc. Q. 2007, 10, 96–102. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Climate Change and Health: A Tool to Estimate Health and Adaption Costs; World Health Organization Office for Europe: Copenhagen, Denmark, 2013. [Google Scholar]
- World Health Organization (WHO). Burden of Disease from Household Air Pollution for 2012. Summary of Results. Available online: http://www.who.int/phe/health_topics/outdoorair/databases/FINAL_HAP_AAP_BoD_24March2014.pdf (accessed on 12 December 2014).
- Keune, H.; Kretsch, C.; de Blust, G.; Gilbert, M.; Flandroy, L.; van den Berge, K.; Versteirt, V.; Hartig, T.; de Keersmaecker, L.; Eggermont, H.; et al. Science–policy challenges for biodiversity, public health and urbanization: Examples from Belgium. Environ. Res. Lett. 2013, 8, 1–19. [Google Scholar] [CrossRef]
- Prada, G.; Brown, T. The Canadian Health Care Debate: A Survey and Assessment of Key Studies; The Conference Board of Canada: Ottawa, ON, Canada, 2012. [Google Scholar]
- Prada, G.; Grimes, K.; McCleery, A.; Nguyen, D.; Pomey, M.P.; Reed, V.; Stonebridge, C.; Roberts, G. Challenging Health Care System Sustainability. Understanding Health System Performance of Leading Countries; The Conference Board of Canada: Ottawa, ON, Canada, 2004. [Google Scholar]
- Macino, J.; Starfield, B.; Shi, L. The contributon of primary care systems to health outcomes within Organization for Economic Cooperation and Development (OECD) countries, 1970–1998. Health Serv. Res. 2003, 38, 831–865. [Google Scholar] [CrossRef] [PubMed]
- Rapoport, J.; Jacobs, P.; Bell, N.R.; Klarenbach, S. Refining the Measurement of the Economic Burden of Chronic Disease in Canada. Chronic Dis. Can. 2004, 25, 13–21. [Google Scholar] [PubMed]
- Thorpe, K.E.; Howard, D.H. The rise in spending among Medicare beneficiaries: The role of chronic disease prevalence and changes in treatment intensity. Health Affair. 2006, 25, w378–w388. [Google Scholar] [CrossRef]
- Morgan, M.W.; Zamora, N.; Hindmarsh, M.F. An inconvenient truth: A sustainable healthcare system requires chronic disease prevention and management transformation. Healthc. Papers 2007, 7, 6–23. [Google Scholar] [CrossRef]
- Baumann, A.; O’Brien-Pallas, L.; Armstrong-Stassen, M.; Blythe, J.; Bourbonnais, R.; Cameron, S.; Irvine Doran, D.; Kerr, M.; McGillis Hall, L.; Vezina, M.; et al. Commitment and Care: The Benefits of a Healthy Workplace for Nurses, Their Patients and the System; Canadian Health Services Research Foundation: Ottawa, ON, Canada, 2001. [Google Scholar]
- Institute of Medicine. Medicare: A Strategy for Quality Assurance. Volume I; National Academy Press: Washington, DC, USA, 1990. [Google Scholar]
- Donabadian, A. Evaluating the quality of medical care. Milbank Mem. Fund Q. 1966, 44, 166–206. [Google Scholar] [CrossRef] [PubMed]
- Weiser, T.G.; Regenbogen, S.E.; Thompson, K.D.; Haynes, A.B.; Lipsitz, S.R.; Berry, W.R.; Gawande, A.A. An estimation of the global volume of surgery: A modelling strategy based on available data. Lancet. 2008, 372, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Organisation for Economic Co-operation and Development (OECD). Geographic Variations in Health Care: What Do We Know and What can be Done to Improve Health System Performance? OECD Health Policy Studies; OECD Publishing: Paris, France, 2014. [Google Scholar]
- Brulle, R.J.; Pellow, D.N. Environmental justice: Human health and environmental inequalities. Annu. Rev. Public Health. 2006, 27, 103–124. [Google Scholar] [CrossRef] [PubMed]
- Leiserowitz, A.A.; Kates, R.W.; Parris, T.M. Sustainability values, attitudes, and behaviors: A review of multinational and global trends. Annu. Rev. Environ. Resour. 2006, 31, 413–444. [Google Scholar] [CrossRef]
- Heinrichs, H.; Laws, N. “Sustainability State” in the Making? Institutionalization of Sustainability in German Federal Policy Making. Sustainability 2014, 6, 2623–2641. [Google Scholar] [CrossRef]
- Dahlgren, G.; Whitehead, M. Policies and Strategies to Promote Equity in Health; World Health Organization: Copenhagen, Denmark, 1991. [Google Scholar]
- Dahlgren, G.; Whitehead, M. Tackling inequalities in health: What can we learn from what has been tried? In Working Paper Prepared for the King’s Fund International Seminar on Tackling Inequalities in Health, September 1993, Ditchley Park, Oxfordshire; King’s Fund (Mimeo): London, UK, 1993. [Google Scholar]
- European Commission. Impact Assessment Board Report for 2013. Available online: http://ec.europa.eu/smart-regulation/impact/key_docs/docs/iab_report_2013_en.pdf (accessed on 12 December 2014).
- Prüss-Üstün, A.; Corvalán, C. Preventing Disease through Healthy Environments. Towards an Estimate of the Environmental Burden of Disease; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- Greene, V.W. Reuse of Disposable Medical Devices: Historical and Current Aspects. Infect. Control 1986, 7, 508–513. [Google Scholar] [PubMed]
- Kümmerer, K. Pharmaceuticals in the environment. Annu. Rev. Env. Resour. 2010, 35, 57–75. [Google Scholar] [CrossRef]
- Harvey, A.L. Natural products in drug discovery. Drug Discov. Today 2008, 13, 894–901. [Google Scholar] [CrossRef] [PubMed]
- Newman, D.J.; Kilama, J.; Bernstein, A.; Chivian, E. Medicines from nature. In Sustaining Life: How Human Health Depends on Biodiversity; Chivian, E., Bernstein, A., Eds.; Oxford University Press: New York, NY, USA, 2008; pp. 117–162. [Google Scholar]
- Randolph, S.E.; Dobson, A.D.M. Pangloss revisited: A critique of the dilution effect and the biodiversity-buffers-disease paradigm. Parasitology 2012, 139, 847–863. [Google Scholar] [CrossRef] [PubMed]
- Götz, K.; Deffner, J. Options for a More Environmentally Friendly Handling of Pharmaceuticals. In Green and Sustainable Pharmacy; Kümmerer, K., Hempel, M., Eds.; Springer: Berlin, Germany, 2010; pp. 149–163. [Google Scholar]
- Collier, R. The ethics of reusing single-use devices. CMAJ 2011, 183. Article 1245. [Google Scholar]
- Weinstein, M.C.; Skinner, J.A. Comparative Effectiveness and Health Care Spending—Implications for Reform. N. Engl. J. Med. 2010, 362, 460–465. [Google Scholar] [CrossRef] [PubMed]
- Agenda 21. United Nations Conference on Environment and Development Rio de Janeiro, Brazil, 3 to 14 June 1992. Available online: http://sustainabledevelopment.un.org/content/documents/Agenda21.pdf (accessed on 12 December 2014).
- Lifvergren, S.; Docherty, P.; Shani, A.B.R. Chapter 4 towards a sustainable healthcare system: Transformation through participation. In Organizing for Sustainable Effectiveness; Mohrman, S.A., Shani, A.B.R., Worley, C., Eds.; Emerald Group Publishing: Bingley, UK, 2011; pp. 99–125. [Google Scholar]
- Mohrman, S.A.; Shani, A.B.R.; McCracken, A. Chapter 1 Organizing for sustainable healthcare: The emerging global challenge. In Organizing for Sustainable Health Care (Organizing for Sustainable Effectiveness); Mohrman, S.A., Shani, A.B.R., Eds.; Emerald Group Publishing: Bingley, UK, 2012; pp. 1–39. [Google Scholar]
- World Economic Forum (WEF). Sustainable Health Systems. Visions, Strategies, Critical Uncertainties and Scenarios. A report from the World Economic Forum Prepared in Collaboration with McKinsey & Company; World Economic Forum: Geneva, Switzerland, 2013. [Google Scholar]
- Boulkedid, R.; Abdoul, H.; Loustau, M.; Sibony, O.; Alberti, C. Using and reporting the Delphi method for selecting healthcare quality indicators: A systematic review. PLoS One 2011, 6. Article e20476. [Google Scholar] [CrossRef]
- Pringle, M.; Wilson, T.; Grol, R. Measuring “goodness” in individuals and healthcare systems. BMJ 2002, 325, 704–707. [Google Scholar] [CrossRef] [PubMed]
- Luke, D.A.; Calhoun, A.; Robichaux, C.B.; Elliott, M.B.; Moreland-Russell, S. The Program Sustainability Assessment Tool: A New Instrument for Public Health Programs. Prev. Chronic Dis. 2014, 11. Article 130184. [Google Scholar] [CrossRef]
- Schell, S.F.; Luke, D.A.; Schooley, M.W.; Elliot, M.B.; Herbers, S.H.; Mueller, N.B.; Bunger, A.C. Public health program capacity for sustainability: A new framework. Implement. Sci. 2014, 8. Article 15. [Google Scholar]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fischer, M. Fit for the Future? A New Approach in the Debate about What Makes Healthcare Systems Really Sustainable. Sustainability 2015, 7, 294-312. https://doi.org/10.3390/su7010294
Fischer M. Fit for the Future? A New Approach in the Debate about What Makes Healthcare Systems Really Sustainable. Sustainability. 2015; 7(1):294-312. https://doi.org/10.3390/su7010294
Chicago/Turabian StyleFischer, Matthias. 2015. "Fit for the Future? A New Approach in the Debate about What Makes Healthcare Systems Really Sustainable" Sustainability 7, no. 1: 294-312. https://doi.org/10.3390/su7010294
APA StyleFischer, M. (2015). Fit for the Future? A New Approach in the Debate about What Makes Healthcare Systems Really Sustainable. Sustainability, 7(1), 294-312. https://doi.org/10.3390/su7010294






