Designing Sustainable Digital Platforms for Ageing Societies: A User-Centred Multi-Level Theoretical Framework
Abstract
1. Introduction
2. Literature Review
2.1. Review of Health-Oriented Needs Among Older Adults
2.2. Review of the Design and Application of Digital Platforms for Elderly Care
2.3. Research Gaps and Theoretical Motivation of This Study
3. Research Methodology
3.1. Semi-Structured Interviews and Qualitative Data Collection
3.1.1. Interview Design and Theoretical Foundations
3.1.2. Interview Sample and Data Sources
3.1.3. User Journey Mapping
- (1)
- Lack of service integration: Participants commonly reported discontinuities between health and rehabilitation services, a shortage of emotional and social support resources, and weak horizontal coordination between daily living and medical services.
- (2)
- Misalignment between demand and service supply: Most services offered were standardized and failed to account for individual health conditions and life contexts, lacking both flexibility and adaptability.
- (3)
- Accessibility and resource bottlenecks: Barriers such as inadequate equipment and staffing, inflexible social work arrangements, and age-unfriendly transportation and appointment systems reduced both willingness and ability to engage with services.
3.2. Application of Grounded Theory and Qualitative Analysis
3.3. Coding Procedures and Analytical Objectives
3.4. Quantitative Survey for Model Validation
3.4.1. Questionnaire Module Design
3.4.2. Questionnaire Distribution Strategy
3.4.3. Data Analysis Methods
- 1.
- Exploratory Factor Analysis (EFA):
- 2.
- Correlation Analysis:
- 3.
- Multiple Regression Analysis:
4. Results
4.1. Results of Grounded Theory Analysis
4.1.1. Initial Coding Phase
4.1.2. Focused Coding Phase
4.1.3. Axial Coding Phase
4.1.4. Theoretical Coding Phase
- 1.
- Three-Tier Classification Framework
- 2.
- Contextual Coding for Layer Verification
- 3.
- Derivation of Platform Response Logic
- “I need tailored advice for my condition→ Health Management Need”
- “The platform should automatically push updates → Smart Matching Mechanism”
- “It makes me feel reassured to know what to do → Perceived Need Fulfillment”
- 4.
- Supplementary Analysis of Semantic Co-occurrence
4.1.5. Theoretical Saturation Test
4.2. Constructed Grounded Theory Model: Structure and Explanation
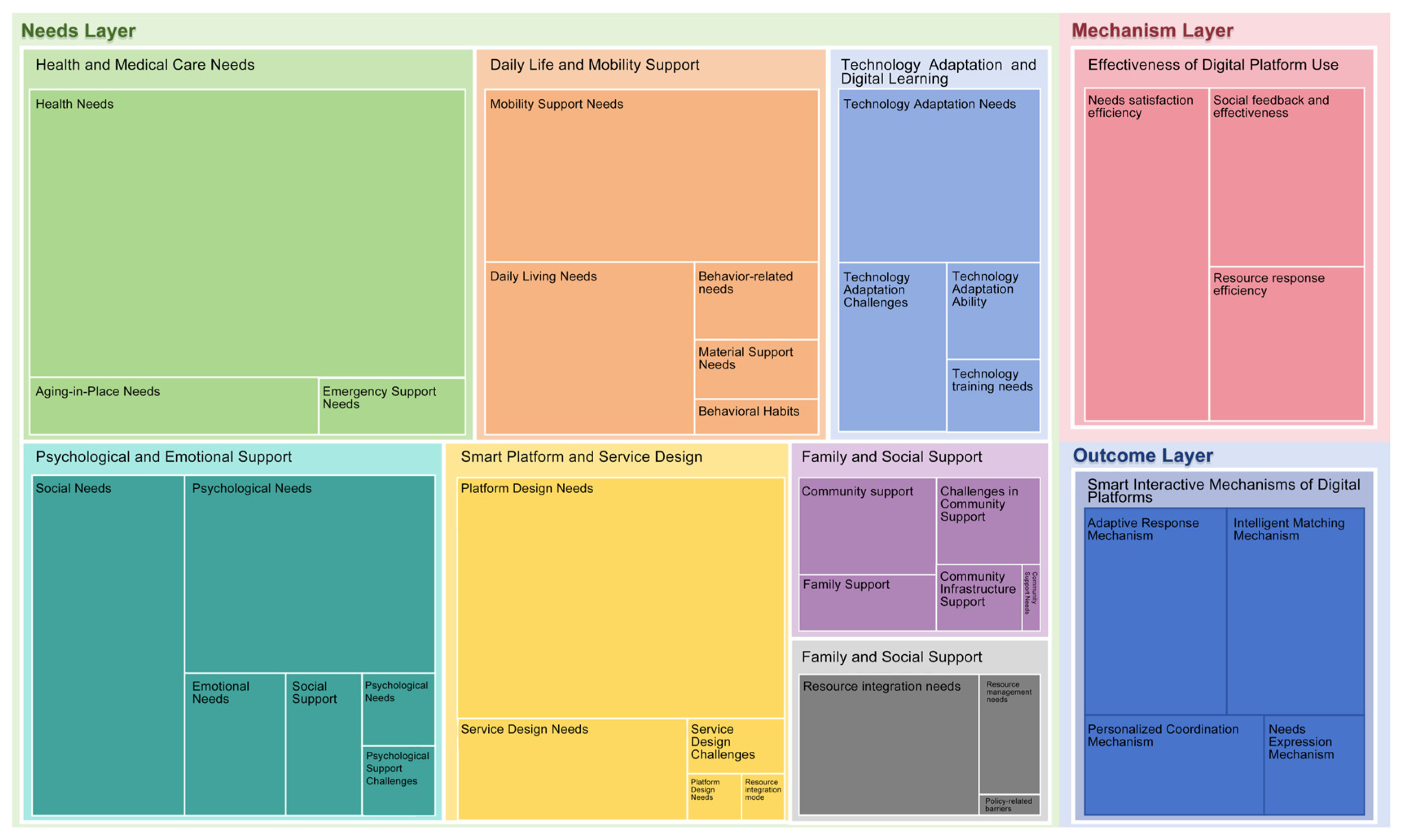
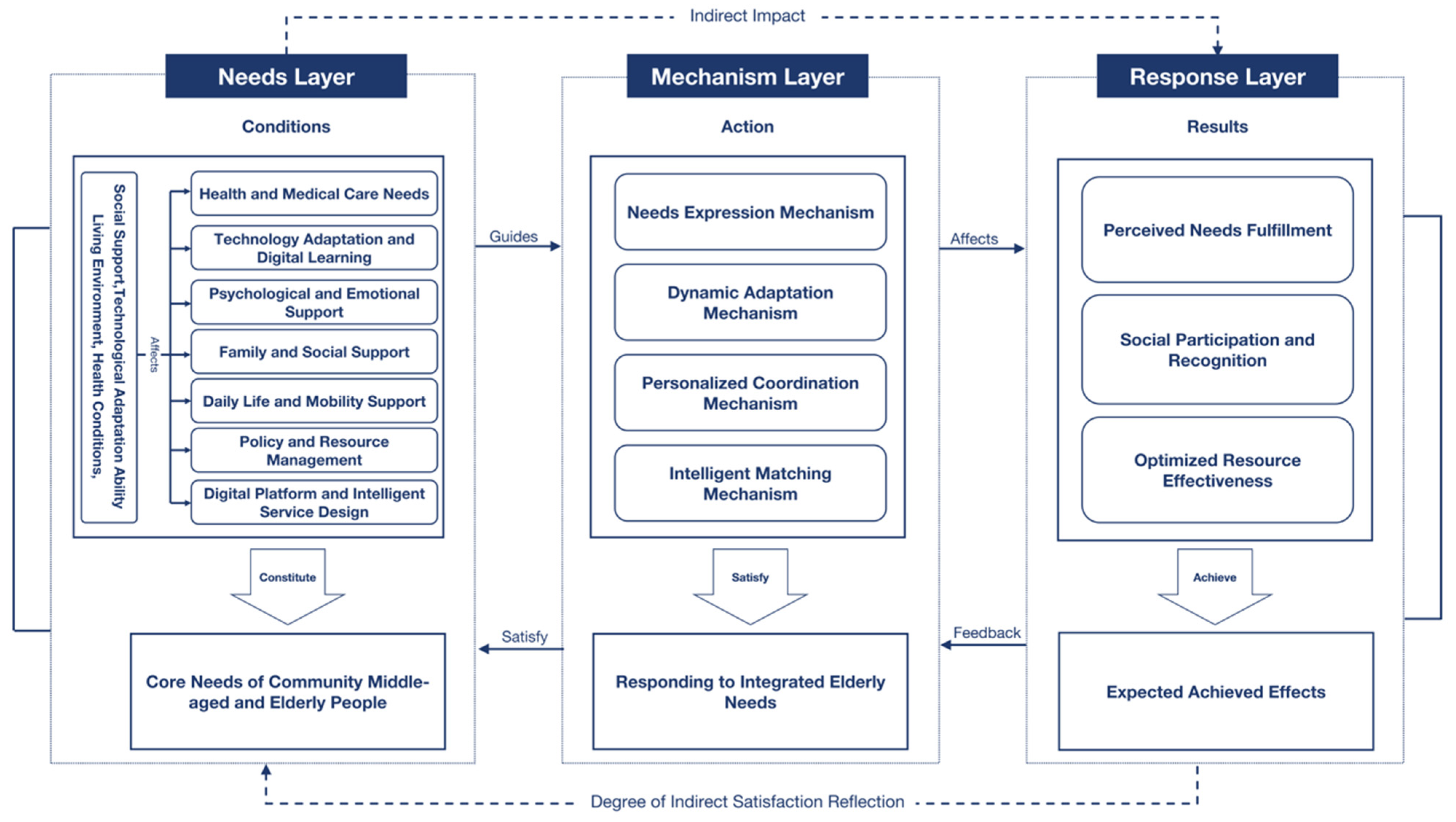
- 1.
- Needs Layer: Core Identification
- 2.
- Mechanisms Layer: Translating Needs into Responses
- 3.
- Outcomes Layer: Fulfillment and Feedback
4.3. Model Validation
4.3.1. Questionnaire Design and Data Collection
4.3.2. Data Analysis Results
- 1.
- Reliability and Validity Testing
- 2.
- Exploratory Factor Analysis (EFA) Results
- 3.
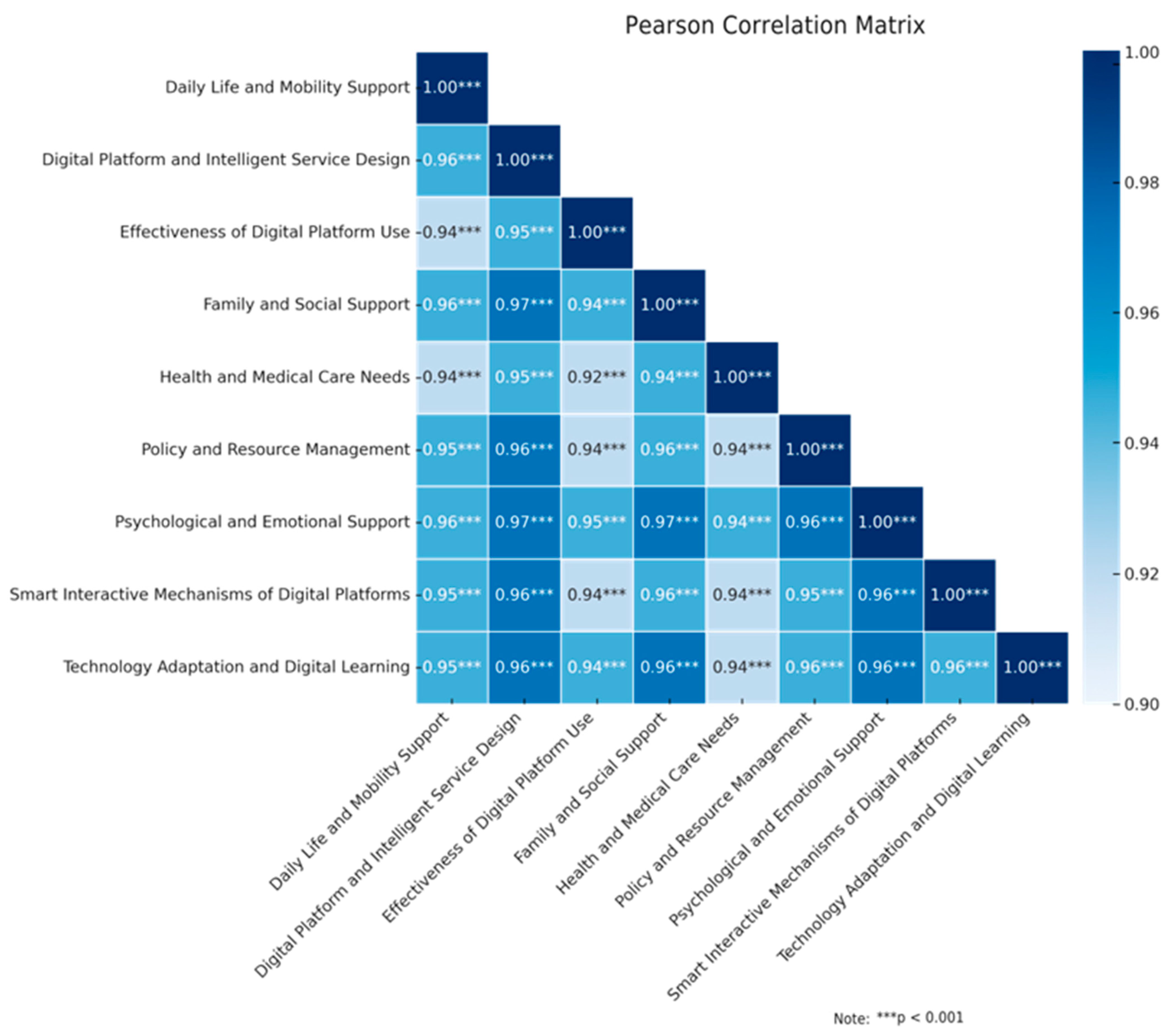
- Correlation Analysis
- 4.
- Multiple Linear Regression Analysis
4.4. Integrated Discussion of Qualitative and Quantitative Results
5. Discussion
5.1. Theoretical Positioning and Literature Dialogue of the Grounded Model
5.2. Model-Driven Transformation into Design Strategies
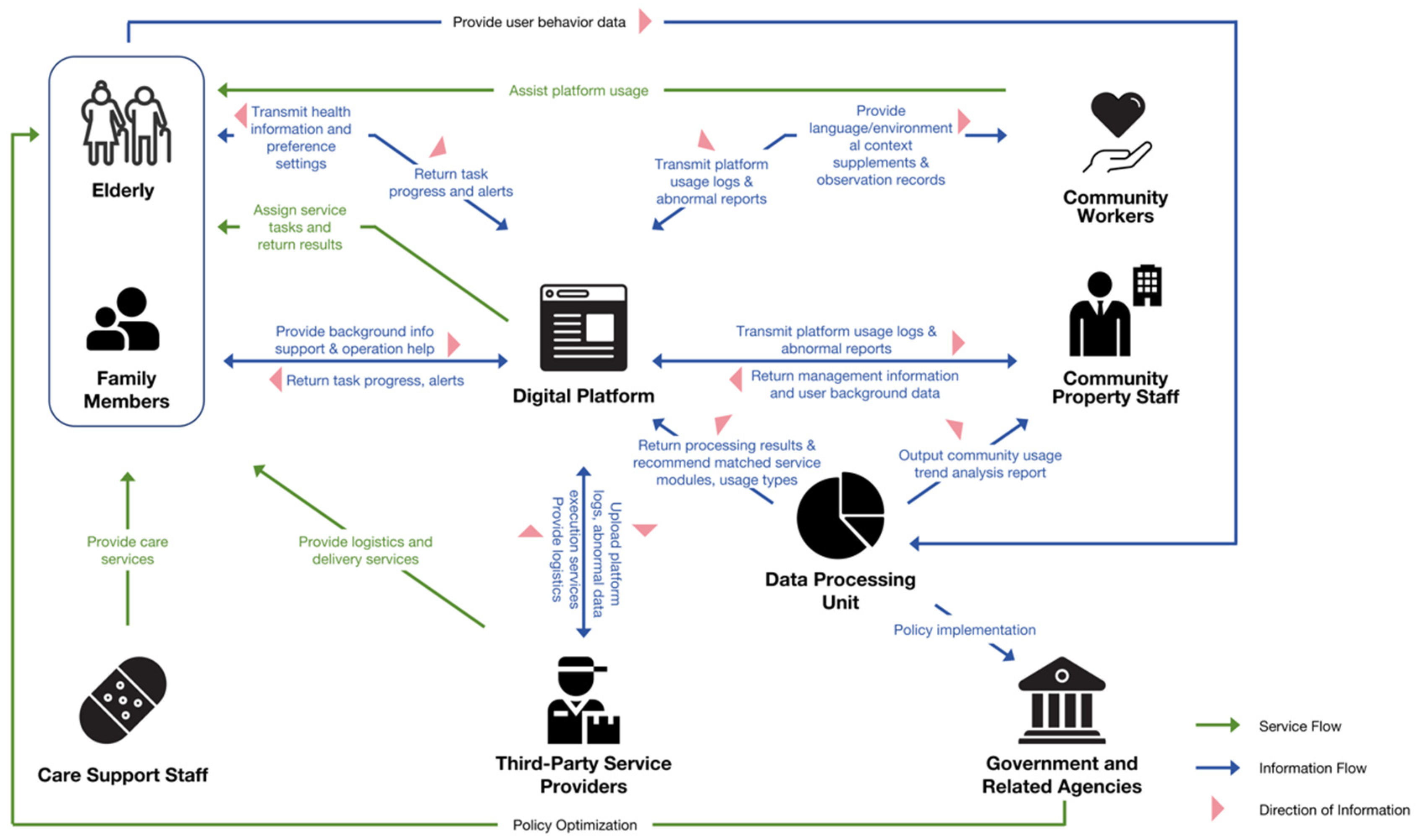
5.3. Application from a Stakeholder-Collaborative Perspective
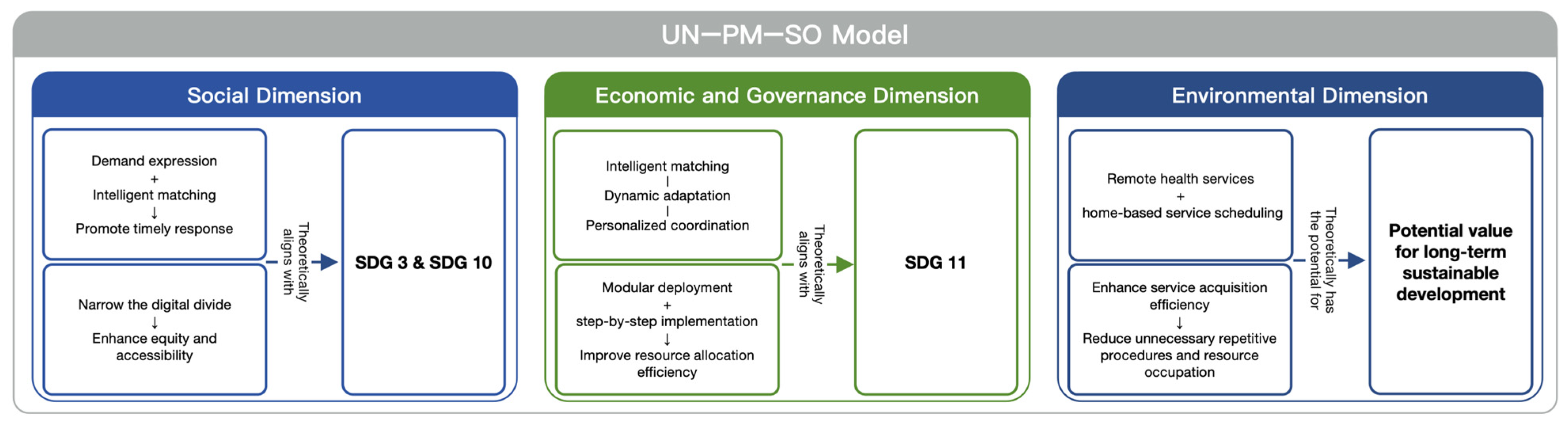
5.4. Multidimensional Sustainability Value of the Theoretical Model
6. Conclusions
- Theoretical and Content Innovation
- Theoretical Contributions
- Practical Contributions
- Sustainability Value
- Limitations
- Future Research Directions
- Sample expansion and cross-context validation: Future research should extend beyond Pearl River Delta cities to central, western, and rural areas and compare elderly care settings such as home-based care, community day-care centers, and integrated medical-care institutions. Samples should also include older adults of different age cohorts, family caregivers, and professional service providers to assess the model’s applicability, stability, and generalizability across diverse socio-cultural and service contexts.
- Prototype and Usability Testing: Translate the theoretical model into platform prototypes and conduct user-centred design testing. Although prior works such as Cristiano have outlined initial functional structures for smart health platforms, they lack integrated multi-level needs logic, which this study seeks to supplement [84].
- Behavioral Data and Longitudinal Tracking: Incorporate behavioral data and longitudinal methods to assess how platform mechanisms affect user experience and needs fulfillment. Sumner has identified the potential for smart platforms to enhance elder participation and self-management, though empirical evidence remains limited [85].
- Cross-Module and Service Integration: Strengthen platform responsiveness by developing strategies for inter-module coordination and scenario-switching, particularly across health management, social interaction, and care services, and explore the feasibility of multi-stakeholder governance collaboration to promote joint participation from government, communities, and enterprises.
- Inclusive Design for Bridging the Digital Divide: Address digital inequalities by improving interface design, assistive technologies, and educational support, creating a more inclusive and user-friendly environment that increases elderly participation and confidence.
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| PRD | Pearl River Delta |
| CGT | Constructivist Grounded Theory |
| UN-PM-SO model | “User Needs–Platform Mechanisms–Service Outcomes” model |
| EFA | Exploratory Factor Analysis |
| PCA | Principal Component Analysis |
| KMO | Kaiser-Meyer-Olkin |
| TAM | Technology Acceptance Model |
| UTAUT | Unified Theory of Acceptance and Use of Technology |
| SDG | Sustainable Development Goals |
| HCI | Human-Computer Interaction |
| ICT | Information and Communication Technology |
| OECD | Organisation for Economic Co-operation and Development |
Appendix A
Complete Correlation Matrix of Exploratory Factor Analysis (EFA)
| Var1 | Var2 | Correlation | p_Value |
|---|---|---|---|
| Technology Adaptation and Digital Learning | Technology Adaptation and Digital Learning | 1 | 0 |
| Technology Adaptation and Digital Learning | Family and Social Support | 0.96357531 | 2.3768 × 10−185 |
| Technology Adaptation and Digital Learning | Health and Medical Care Needs | 0.93806564 | 2.3154 × 10−149 |
| Technology Adaptation and Digital Learning | Daily Life and Mobility Support | 0.95080266 | 6.5401 × 10−165 |
| Technology Adaptation and Digital Learning | Effectiveness of Digital Platform Use | 0.94005322 | 1.4737 × 10−151 |
| Technology Adaptation and Digital Learning | Digital Platform and Intelligent Service Design | 0.9605918 | 5.523 × 10−180 |
| Technology Adaptation and Digital Learning | Smart Interactive Mechanisms of Digital Platforms | 0.95740412 | 1.0852 × 10−174 |
| Technology Adaptation and Digital Learning | Psychological and Emotional Support | 0.96470498 | 1.6837 × 10−187 |
| Technology Adaptation and Digital Learning | Policy and Resource Management | 0.95899841 | 2.7584 × 10−177 |
| Family and Social Support | Technology Adaptation and Digital Learning | 0.96357531 | 2.3768 × 10−185 |
| Family and Social Support | Family and Social Support | 1 | 0 |
| Family and Social Support | Health and Medical Care Needs | 0.9441222 | 2.6785 × 10−156 |
| Family and Social Support | Daily Life and Mobility Support | 0.95752861 | 6.8624 × 10−175 |
| Family and Social Support | Effectiveness of Digital Platform Use | 0.94486429 | 3.3501 × 10−157 |
| Family and Social Support | Digital Platform and Intelligent Service Design | 0.97157984 | 2.5823 × 10−202 |
| Family and Social Support | Smart Interactive Mechanisms of Digital Platforms | 0.95909992 | 1.8705 × 10−177 |
| Family and Social Support | Psychological and Emotional Support | 0.96743689 | 5.2915 × 10−193 |
| Family and Social Support | Policy and Resource Management | 0.95853604 | 1.5984 × 10−176 |
| Health and Medical Care Needs | Technology Adaptation and Digital Learning | 0.93806564 | 2.3154 × 10−149 |
| Health and Medical Care Needs | Family and Social Support | 0.9441222 | 2.6785 × 10−156 |
| Health and Medical Care Needs | Health and Medical Care Needs | 1 | 0 |
| Health and Medical Care Needs | Daily Life and Mobility Support | 0.93824476 | 1.4782 × 10−149 |
| Health and Medical Care Needs | Effectiveness of Digital Platform Use | 0.9228431 | 1.2435 × 10−134 |
| Health and Medical Care Needs | Digital Platform and Intelligent Service Design | 0.94805226 | 3.1536 × 10−161 |
| Health and Medical Care Needs | Smart Interactive Mechanisms of Digital Platforms | 0.93590732 | 4.661 × 10−147 |
| Health and Medical Care Needs | Psychological and Emotional Support | 0.94258348 | 1.8247 × 10−154 |
| Health and Medical Care Needs | Policy and Resource Management | 0.9354414 | 1.4298 × 10−146 |
| Daily Life and Mobility Support | Technology Adaptation and Digital Learning | 0.95080266 | 6.5401 × 10−165 |
| Daily Life and Mobility Support | Family and Social Support | 0.95752861 | 6.8624 × 10−175 |
| Daily Life and Mobility Support | Health and Medical Care Needs | 0.93824476 | 1.4782 × 10−149 |
| Daily Life and Mobility Support | Daily Life and Mobility Support | 1 | 0 |
| Daily Life and Mobility Support | Effectiveness of Digital Platform Use | 0.93850973 | 7.5912 × 10−150 |
| Daily Life and Mobility Support | Digital Platform and Intelligent Service Design | 0.95893483 | 3.5164 × 10−177 |
| Daily Life and Mobility Support | Smart Interactive Mechanisms of Digital Platforms | 0.94938985 | 5.4107 × 10−163 |
| Daily Life and Mobility Support | Psychological and Emotional Support | 0.95619028 | 8.8188 × 10−173 |
| Daily Life and Mobility Support | Policy and Resource Management | 0.95284754 | 8.6595 × 10−168 |
| Effectiveness of Digital Platform Use | Technology Adaptation and Digital Learning | 0.94005322 | 1.4737 × 10−151 |
| Effectiveness of Digital Platform Use | Family and Social Support | 0.94486429 | 3.3501 × 10−157 |
| Effectiveness of Digital Platform Use | Health and Medical Care Needs | 0.9228431 | 1.2435 × 10−134 |
| Effectiveness of Digital Platform Use | Daily Life and Mobility Support | 0.93850973 | 7.5912 × 10−150 |
| Effectiveness of Digital Platform Use | Effectiveness of Digital Platform Use | 1 | 0 |
| Effectiveness of Digital Platform Use | Digital Platform and Intelligent Service Design | 0.94860421 | 5.97 × 10−162 |
| Effectiveness of Digital Platform Use | Smart Interactive Mechanisms of Digital Platforms | 0.93779121 | 4.5933 × 10−149 |
| Effectiveness of Digital Platform Use | Psychological and Emotional Support | 0.9457405 | 2.7721 × 10−158 |
| Effectiveness of Digital Platform Use | Policy and Resource Management | 0.93968962 | 3.7649 × 10−151 |
| Digital Platform and Intelligent Service Design | Technology Adaptation and Digital Learning | 0.9605918 | 5.523 × 10−180 |
| Digital Platform and Intelligent Service Design | Family and Social Support | 0.97157984 | 2.5823 × 10−202 |
| Digital Platform and Intelligent Service Design | Health and Medical Care Needs | 0.94805226 | 3.1536 × 10−161 |
| Digital Platform and Intelligent Service Design | Daily Life and Mobility Support | 0.95893483 | 3.5164 × 10−177 |
| Digital Platform and Intelligent Service Design | Effectiveness of Digital Platform Use | 0.94860421 | 5.97 × 10−162 |
| Digital Platform and Intelligent Service Design | Digital Platform and Intelligent Service Design | 1 | 0 |
| Digital Platform and Intelligent Service Design | Smart Interactive Mechanisms of Digital Platforms | 0.96429047 | 1.0546 × 10−186 |
| Digital Platform and Intelligent Service Design | Psychological and Emotional Support | 0.97197551 | 2.8285 × 10−203 |
| Digital Platform and Intelligent Service Design | Policy and Resource Management | 0.96419292 | 1.619 × 10−186 |
| Smart Interactive Mechanisms of Digital Platforms | Technology Adaptation and Digital Learning | 0.95740412 | 1.0852 × 10−174 |
| Smart Interactive Mechanisms of Digital Platforms | Family and Social Support | 0.95909992 | 1.8705 × 10−177 |
| Smart Interactive Mechanisms of Digital Platforms | Health and Medical Care Needs | 0.93590732 | 4.661 × 10−147 |
| Smart Interactive Mechanisms of Digital Platforms | Daily Life and Mobility Support | 0.94938985 | 5.4107 × 10−163 |
| Smart Interactive Mechanisms of Digital Platforms | Effectiveness of Digital Platform Use | 0.93779121 | 4.5933 × 10−149 |
| Smart Interactive Mechanisms of Digital Platforms | Digital Platform and Intelligent Service Design | 0.96429047 | 1.0546 × 10−186 |
| Smart Interactive Mechanisms of Digital Platforms | Smart Interactive Mechanisms of Digital Platforms | 1 | 0 |
| Smart Interactive Mechanisms of Digital Platforms | Psychological and Emotional Support | 0.96388205 | 6.2958 × 10−186 |
| Smart Interactive Mechanisms of Digital Platforms | Policy and Resource Management | 0.95463378 | 2.0736 × 10−170 |
| Psychological and Emotional Support | Technology Adaptation and Digital Learning | 0.96470498 | 1.6837 × 10−187 |
| Psychological and Emotional Support | Family and Social Support | 0.96743689 | 5.2915 × 10−193 |
| Psychological and Emotional Support | Health and Medical Care Needs | 0.94258348 | 1.8247 × 10−154 |
| Psychological and Emotional Support | Daily Life and Mobility Support | 0.95619028 | 8.8188 × 10−173 |
| Psychological and Emotional Support | Effectiveness of Digital Platform Use | 0.9457405 | 2.7721 × 10−158 |
| Psychological and Emotional Support | Digital Platform and Intelligent Service Design | 0.97197551 | 2.8285 × 10−203 |
| Psychological and Emotional Support | Smart Interactive Mechanisms of Digital Platforms | 0.96388205 | 6.2958 × 10−186 |
| Psychological and Emotional Support | Psychological and Emotional Support | 1 | 0 |
| Psychological and Emotional Support | Policy and Resource Management | 0.96058721 | 5.6248 × 10−180 |
| Policy and Resource Management | Technology Adaptation and Digital Learning | 0.95899841 | 2.7584 × 10−177 |
| Policy and Resource Management | Family and Social Support | 0.95853604 | 1.5984 × 10−176 |
| Policy and Resource Management | Health and Medical Care Needs | 0.9354414 | 1.4298 × 10−146 |
| Policy and Resource Management | Daily Life and Mobility Support | 0.95284754 | 8.6595 × 10−168 |
| Policy and Resource Management | Effectiveness of Digital Platform Use | 0.93968962 | 3.7649 × 10−151 |
| Policy and Resource Management | Digital Platform and Intelligent Service Design | 0.96419292 | 1.619 × 10−186 |
| Policy and Resource Management | Smart Interactive Mechanisms of Digital Platforms | 0.95463378 | 2.0736 × 10−170 |
| Policy and Resource Management | Psychological and Emotional Support | 0.96058721 | 5.6248 × 10−180 |
| Policy and Resource Management | Policy and Resource Management | 1 | 0 |
References
- World Health Organization Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 8 August 2025).
- OECD. Integrating Care to Prevent and Manage Chronic Diseases: Best Practices in Public Health; OECD: Paris, France, 2023; ISBN 978-92-64-71291-1. [Google Scholar]
- National Bureau of Statistics of China Seventh National Population Census Bulletin. Available online: https://www.stats.gov.cn/sj/zxfb/202302/t20230203_1901085.html (accessed on 16 April 2025).
- Miyatake, H.; Kosaka, M.; Arita, S.; Tsunetoshi, C.; Masunaga, H.; Kotera, Y.; Nishikawa, Y.; Ozaki, A.; Beniya, H. Videoconferencing for Home Care Delivery in Japan: Observational Study. J. Med. Internet Res. 2021, 23, e23539. [Google Scholar] [CrossRef]
- Martela, F.; Nandram, S. Buurtzorg: Scaling up an Organization with Hundreds of Self-Managing Teams but No Middle Managers. J. Organ. Des. 2025, 14, 1–19. [Google Scholar] [CrossRef]
- State Council of China the 14th Five-Year Plan for the Development of the National Aging Cause and the Elderly Care Service System. Available online: https://www.gov.cn/zhengce/content/2022-02/21/content_5674844.htm (accessed on 16 April 2025).
- Ministry of Civil Affairs of China Smart Health and Elderly Care Industry Development Action Plan (2021–2025). 2021. Available online: https://www.nhc.gov.cn/lljks/c100158/202110/a871dfd3e1fd45b89e9af1f40e44ba12/files/1733127377323_94303.pdf (accessed on 14 September 2024).
- Cui, S.; Tian, Y.; Yang, S. Actively Addressing Population Ageing and Promoting the Development of the Elderly Care Service Industry—Summary of the Academic Symposium on ‘Challenges and Countermeasures for Elderly Care Services in the Context of Population Ageing’. Chin. J. Popul. Sci. 2018, 3, 121–125. [Google Scholar]
- Li, S. Community-Based Day Care Service for Older People: Its Current Situation, Problems, Causes, and Countermeasures. Sci. Res. Aging 2023, 11, 30–46. [Google Scholar]
- Awan, M.; Ali, S.; Ali, M.; Abrar, M.F.; Ullah, H.; Khan, D. Usability Barriers for Elderly Users in Smartphone App Usage: An Analytical Hierarchical Process-Based Prioritization. Sci. Prog. 2021, 2021, 2780257. [Google Scholar] [CrossRef]
- Fang, Z.; Liu, Y.; Peng, B. Empowering Older Adults: Bridging the Digital Divide in Online Health Information Seeking. Humanit. Soc. Sci. Commun. 2024, 11, 1748. [Google Scholar] [CrossRef]
- Hung, J. Smart Elderly Care Services in China: Challenges, Progress, and Policy Development. Sustainability 2023, 15, 178. [Google Scholar] [CrossRef]
- Van Deursen, A.J.; Van Dijk, J.A. The Digital Divide Shifts to Differences in Usage. New Media Soc. 2014, 16, 507–526. [Google Scholar] [CrossRef]
- Wei, K.-K.; Teo, H.-H.; Chan, H.C.; Tan, B.C.Y. Conceptualizing and Testing a Social Cognitive Model of the Digital Divide. Inf. Syst. Res. 2011, 22, 170–187. [Google Scholar] [CrossRef]
- Olphert, W.; Damodaran, L. Older People and Digital Disengagement: A Fourth Digital Divide? Gerontology 2013, 59, 564–570. [Google Scholar] [CrossRef]
- Eurostat. Skills for the Digital Age—Statistics Explained. 2024. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Skills_for_the_digital_age (accessed on 3 September 2025).
- CNNIC. The 54th Statistical Report on China’s Internet Development. 2024. Available online: https://www.cnnic.cn/NMediaFile/2024/0911/MAIN1726017626560DHICKVFSM6.pdf (accessed on 3 September 2025).
- van Deursen, A.J.A.M.; Dijk, J.A.G.M. van Internet Skills Performance Tests: Are People Ready for eHealth? J. Med. Internet Res. 2011, 13, e1581. [Google Scholar] [CrossRef]
- Ofcom. Adults’ Media Use and Attitudes Report 2022. 2022. Available online: https://www.ofcom.org.uk/siteassets/resources/documents/research-and-data/media-literacy-research/adults/adults-media-use-and-attitudes-2022/defnydd-oedolion-or-cyfryngau-au-hagweddau-atynt-2022.pdf?v=327650 (accessed on 3 September 2025).
- Yang, H.; Huang, X.; Liang, J.; Jia, Z.; Wei, Q.; Wang, H. Differences in the Elderly Care Service Demand, Preference, and Tendency Between Urban and Rural Areas in the Pearl River Delta. Acta Acad. Med. Sin. 2024, 46, 193–203. [Google Scholar]
- Huang, R.; Hong, S. ‘Space-Power’ Dynamic Matching: Prospects for Spatial Governance Models and Reforms in the Pearl River Delta Local Administrative Regions from the Perspective of Scale Transition. JPA 2020, 13, 41–57+205–206. [Google Scholar]
- Zhang, G.; Gong, H. Research on Population Aging and Equilibrium of Elderly Care Resources Allocation in Guangdong Province. South China Popul. 2022, 37, 1–13. [Google Scholar]
- Heilmann, S. Policy Experimentation in China’s Economic Rise. Stud. Comp. Int. Dev. 2008, 43, 1–26. [Google Scholar] [CrossRef]
- Henfridsson, O.; Bygstad, B. The Generative Mechanisms of Digital Infrastructure Evolution. MIS Q. 2013, 37, 907–931. [Google Scholar] [CrossRef]
- Spagnoletti, P.; Resca, A.; Lee, G. A Design Theory for Digital Platforms Supporting Online Communities: A Multiple Case Study. J. Inf. Technol. 2015, 30, 364–380. [Google Scholar] [CrossRef]
- Dong, Y.; Cheng, L.; Cao, H. Impact of Informal Social Support on the Mental Health of Older Adults. Front. Public Health 2024, 12, 1446246. [Google Scholar] [CrossRef]
- Chen, J.-J.; Liu, L.-F.; Lin, C.-I.; Lin, H.-C. Multidimensional Determinants of Well-Being Among Community-Dwelling Older Adults During the Early Stage of the COVID-19 Pandemic in Taiwan. Gerontol. Geriatr. Med. 2022, 8, 23337214221111227. [Google Scholar] [CrossRef]
- Upasen, R.; Saengpanya, W.; Awae, W.; Prasitvej, P. The Influence of Resilience and Social Support on Mental Health of Older Adults Living in Community: A Cross-Sectional Study. BMC Psychol. 2024, 12, 397. [Google Scholar] [CrossRef]
- Gimie, A.M.; Castillo, A.I.M.; Mullins, C.D.; Falvey, J.R. Epidemiology of Public Transportation Use among Older Adults in the United States. J. Am. Geriatr. Soc. 2022, 70, 3549–3559. [Google Scholar] [CrossRef]
- Zhang, N.; Zhang, J.; Yang, Q.; Skitmore, M.; Yang, N.; Shi, B.; Zhang, X.; Qin, X. The Impact of Transport Inclusion on Active Aging: A Perceived Value Analysis. Transp. Res. Part D Transp. Environ. 2024, 127, 104029. [Google Scholar] [CrossRef]
- Maresova, P.; Krejcar, O.; Maskuriy, R.; Bakar, N.A.A.; Selamat, A.; Truhlarova, Z.; Horak, J.; Joukl, M.; Vítkova, L. Challenges and Opportunity in Mobility among Older Adults—Key Determinant Identification. BMC Geriatr. 2023, 23, 447. [Google Scholar] [CrossRef]
- Gadermann, A.C.; Thomson, K.C.; Richardson, C.G.; Gagné, M.; McAuliffe, C.; Hirani, S.; Jenkins, E. Examining the Impacts of the COVID-19 Pandemic on Family Mental Health in Canada: Findings from a National Cross-Sectional Study. BMJ Open 2021, 11, e042871. [Google Scholar] [CrossRef]
- Valtorta, N.K.; Moore, D.C.; Barron, L.; Stow, D.; Hanratty, B. Older Adults’ Social Relationships and Health Care Utilization: A Systematic Review. Am. J. Public Health 2018, 108, e1–e10. [Google Scholar] [CrossRef]
- Zhao, R.; Huo, M.; Tan, M.; Wang, L.; Liu, Q.; Li, J.; Wang, R.; Li, H. Enhancing Older Care Services: A Comprehensive Internet + Community Home Indicator System. BMC Public Health 2024, 24, 2713. [Google Scholar] [CrossRef]
- Hou, H.; Wei, H.; Wang, Y.; Yu, J.; Qiu, G. Construction Path of Smart Health Care Platform for the Elderly in China. Chin. J. Eng. Sci. 2022, 24, 170. [Google Scholar] [CrossRef]
- Zhu, J.; Weng, H.; Ou, P.; Li, L. Use and Acceptance of Smart Elderly Care Apps among Chinese Medical Staff and Older Individuals: Web-Based Hybrid Survey Study. JMIR Form. Res. 2023, 7, e41919. [Google Scholar] [CrossRef]
- He, J.; Sui, D.; Li, L.; Lv, X. Fueling the Development of Elderly Care Services in China with Digital Technology: A Provincial Panel Data Analysis. Heliyon 2025, 11, e41490. [Google Scholar] [CrossRef]
- Wang, X.; Du, W. Literature Review on Smart Elderly Care Research. Aging Res. 2024, 11, 689–696. [Google Scholar] [CrossRef]
- Liu, R. Research on the Current Dilemmas and Countermeasures of Community Smart Elderly Care in the Context of Digital Intelligence. Aging Res. 2024, 11, 2698–2705. [Google Scholar] [CrossRef]
- Samal, L.; Dykes, P.C.; Greenberg, J.O.; Hasan, O.; Venkatesh, A.K.; Volk, L.A.; Bates, D.W. Care Coordination Gaps Due to Lack of Interoperability in the United States: A Qualitative Study and Literature Review. BMC Health Serv. Res. 2016, 16, 143. [Google Scholar] [CrossRef]
- Ming, Y.; Li, Y.; Liu, Y. Digital Technologies as Solutions to China’s Aging Population: A Systematic Review of Their Opportunities and Challenges in Rural Development. Front. Public Health 2025, 12, 1416968. [Google Scholar] [CrossRef]
- Elmi, A.A.; Abdullahi, M.O.; Abdullahi, H.O. Internet of Things in Telemedicine: A Systematic Review of Current Trends and Future Directions. Instrum. Mes. Métrol. 2024, 23, 463–472. [Google Scholar] [CrossRef]
- Jat, A.S.; Grønli, T.-M. Harnessing the Digital Revolution: A Comprehensive Review of mHealth Applications for Remote Monitoring in Transforming Healthcare Delivery. In International Conference on Mobile Web and Intelligent Information Systems; Springer Nature: Cham, Switzerland, 2023; pp. 55–67. [Google Scholar] [CrossRef]
- Nasr, M.; Islam, M.M.; Shehata, S.; Karray, F.; Quintana, Y. Smart Healthcare in the Age of AI: Recent Advances, Challenges, and Future Prospects. IEEE Access 2021, 9, 145248–145270. [Google Scholar] [CrossRef]
- Sharma, S.; Rawal, R.; Shah, D. Addressing the Challenges of AI-Based Telemedicine: Best Practices and Lessons Learned. J. Educ. Health Promot. 2023, 12, 338. [Google Scholar] [CrossRef]
- Guo, Q.; Chen, P. Construction and Optimization of Health Behavior Prediction Model for the Older Adult in Smart Older Adult Care. Front. Public Health 2024, 12, 1486930. [Google Scholar] [CrossRef]
- Chen, S. Age-Appropriate Design of Smart Senior Care Product APP Interface Based on Deep Learning. Heliyon 2024, 10, e28567. [Google Scholar] [CrossRef]
- Aljohani, A. AI-Driven Decision-Making for Personalized Elderly Care: A Fuzzy MCDM-Based Framework for Enhancing Treatment Recommendations. BMC Med. Inf. Decis. Mak. 2025, 25, 119. [Google Scholar] [CrossRef]
- Aarons, G.; Green, A.E.; Palinkas, L.A.; Self-Brown, S.; Whitaker, D.J.; Lutzker, J.R.; Silovsky, J.F.; Hecht, D.B.; Chaffin, M.J. Dynamic Adaptation Process to Implement Evidence-Based Child Maltreatment Intervention. Implement. Sci. 2012, 7, 32. [Google Scholar] [CrossRef]
- Kouroubali, A.; Kondylakis, H.; Logothetidis, F.; Katehakis, D.G. Developing an AI-Enabled Integrated Care Platform for Frailty. Health Care (Don Mills) 2022, 10, 443. [Google Scholar] [CrossRef]
- Li, Y.; Luo, L.; Dong, H. Delivering Integrated Community Care for the Elderly: A Qualitative Case Study in Southern China. Int. J. Environ. Res. Public Health 2024, 21, 680. [Google Scholar] [CrossRef]
- Luo, S.; Hu, Y. Model Innovation Driven by Service Design. Packag. Eng. 2015, 36, 28. [Google Scholar] [CrossRef]
- Liu, Y.; Yin, Y.; Song, Y.; Bai, X.; Chen, Q. Research and Construction of Creative Service Design Pattern for Intelligent Interactive Products. Packag. Eng. 2024, 45, 489. [Google Scholar] [CrossRef]
- He, X.; Song, N. Campus Print Center Service Design Based on User Behavior. Packag. Eng. 2020, 41, 166–174. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, Y.; Zeng, Y.; Su, J.; Li, Z. An Investigation into the Acceptance of Intelligent Care Systems: An Extended Technology Acceptance Model (TAM). Sci. Rep. 2025, 15, 17912. [Google Scholar] [CrossRef]
- Yu, S.; Chen, T. Understanding Older Adults’ Acceptance of Chatbots in Healthcare Delivery: An Extended UTAUT Model. Front. Public Health 2024, 12, 1435329. [Google Scholar] [CrossRef]
- Yang, H.J.; Lee, J.-H.; Lee, W. Factors Influencing Health Care Technology Acceptance in Older Adults Based on the Technology Acceptance Model and the Unified Theory of Acceptance and Use of Technology: Meta-Analysis. J. Med. Internet Res. 2025, 27, e65269. [Google Scholar] [CrossRef]
- Peruchi, D.F.; de Jesus Pacheco, D.A.; Todeschini, B.V.; ten Caten, C.S. Moving towards Digital Platforms Revolution? Antecedents, Determinants and Conceptual Framework for Offline B2B Networks. J. Bus. Res. 2022, 142, 344–363. [Google Scholar] [CrossRef]
- Farage, M.A.; Miller, K.W.; Ajayi, F.; Hutchins, D. Design Principles to Accommodate Older Adults. Glob. J. Health Sci. 2012, 4, p2. [Google Scholar] [CrossRef]
- White, P.J. Designing Products for Older People’s Social and Emotional Needs: A Case Study. Anthropol. Aging 2022, 43, 24–39. [Google Scholar] [CrossRef]
- Mois, G.; Fortuna, K.L. Visioning the Future of Gerontological Digital Social Work. J. Gerontol. Soc. Work 2020, 63, 412–427. [Google Scholar] [CrossRef]
- Mills, J.; Bonner, A.; Francis, K. The Development of Constructivist Grounded Theory. Int. J. Qual. Methods 2006, 5, 25–35. [Google Scholar] [CrossRef]
- Jia, X.; Tan, X. The Actual Value of the Classical Grounded Theory and Its Spirit to China Management Research. Chin. J. Manag. 2010, 7, 656–665. [Google Scholar]
- Wang, G.; Albayrak, A.; Kortuem, G.; van der Cammen, T.J. A Digital Platform for Facilitating Personalized Dementia Care in Nursing Homes: Formative Evaluation Study. JMIR Form. Res. 2021, 5, e25705. [Google Scholar] [CrossRef]
- Jia, X.; Heng, L. The “jungle”,history, and approach road of the grounded theory. Sci. Res. Manag. 2020, 41, 151–163. [Google Scholar] [CrossRef]
- Cullen, M.M.; Brennan, N.M. Grounded Theory: Description, Divergences and Application. Account. Financ. Gov. Rev. 2021, 27. [Google Scholar] [CrossRef]
- Makri, C.; Neely, A. Grounded Theory: A Guide for Exploratory Studies in Management Research. Int. J. Qual. Methods 2021, 20, 16094069211013654. [Google Scholar] [CrossRef]
- Hennink, M.M.; Kaiser, B.N.; Marconi, V.C. Code Saturation versus Meaning Saturation: How Many Interviews Are Enough? Qual. Health Res. 2017, 27, 591–608. [Google Scholar] [CrossRef]
- Davis, F.D. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Q. 1989, 13, 319. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. 2003, 27, 425. [Google Scholar] [CrossRef]
- Heart, T.; Kalderon, E. Older Adults: Are They Ready to Adopt Health-Related ICT? Int. J. Med. Inf. 2013, 82, e209–e231. [Google Scholar] [CrossRef] [PubMed]
- Peek, S.T.M.; Wouters, E.J.M.; Van Hoof, J.; Luijkx, K.G.; Boeije, H.R.; Vrijhoef, H.J.M. Factors Influencing Acceptance of Technology for Aging in Place: A Systematic Review. Int. J. Med. Inf. 2014, 83, 235–248. [Google Scholar] [CrossRef] [PubMed]
- Robson, J.I.; Crellin, J.M. The Role of User’s Perceived Control in Interface Design, Employing Verbal Protocol Analysis. Appl. Ergon. 1989, 20, 246–251. [Google Scholar] [CrossRef]
- Sonboli, N.; Smith, J.J.; Cabral Berenfus, F.; Burke, R.; Fiesler, C. Fairness and Transparency in Recommendation: The Users’ Perspective. In Proceedings of the 29th ACM Conference on User Modeling, Adaptation and Personalization, Utrecht, The Netherlands, 21 June 2021; pp. 274–279. [Google Scholar]
- Siepmann, C.; Chatti, M.A. Trust and Transparency in Recommender Systems 2023. arXiv 2023, arXiv:2304.08094. [Google Scholar] [CrossRef]
- Jonkisz, A.; Karniej, P.; Krasowska, D. The Servqual Method as an Assessment Tool of the Quality of Medical Services in Selected Asian Countries. Int. J. Environ. Res. Public Health 2022, 19, 7831. [Google Scholar] [CrossRef]
- Suragarn, U.; Hain, D.; Pfaff, G. Approaches to Enhance Social Connection in Older Adults: An Integrative Review of Literature. Aging Health Res. 2021, 1, 100029. [Google Scholar] [CrossRef]
- Marwaha, J.S.; Landman, A.B.; Brat, G.A.; Dunn, T.; Gordon, W.J. Deploying Digital Health Tools within Large, Complex Health Systems: Key Considerations for Adoption and Implementation. NPJ Digit. Med. 2022, 5, 13. [Google Scholar] [CrossRef]
- Alruwaili, M.M.; Shaban, M.; Elsayed Ramadan, O.M. Digital Health Interventions for Promoting Healthy Aging: A Systematic Review of Adoption Patterns, Efficacy, and User Experience. Sustainability 2023, 15, 16503. [Google Scholar] [CrossRef]
- Mantri, M.; Sunder, G.; Kadam, S.; Abhyankar, A. A Perspective on Digital Health Platform Design and Its Implementation at National Level. Front. Digit. Health 2024, 6, 1260855. [Google Scholar] [CrossRef] [PubMed]
- Robert Koch Institut Current Landscape of Guidelines, Frameworks and Tools for Digital Health Programming 2024. Available online: https://www.bmz-digital.global/wp-content/uploads/2024/10/Current-Landscape-of-Guidelines-Frameworks-and-Tools-for-Digital-Health-Programing-Robert-Koch-Institut_DIPC-1.pdf (accessed on 4 September 2025).
- Gordienko, Y.; Stirenko, S.; Alienin, O.; Skala, K.; Soyat, Z.; Rojbi, A.; Benito, J.R.L.; González, E.A.; Lushchyk, U.; Sajn, L.; et al. Augmented Coaching Ecosystem for Non-Obtrusive Adaptive Personalized Elderly Care on the Basis of Cloud-Fog-Dew Computing Paradigm. In Proceedings of the 2017 40th International Convention on Information and Communication Technology, Electronics and Microelectronics (MIPRO), Opatija, Croatia, 22–26 May 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 359–364. [Google Scholar]
- Parmar, B.L.; Freeman, R.E.; Harrison, J.S. Stakeholder Theory: The State of the Art; Cambridge University Press: Cambridge, UK, 2010. [Google Scholar]
- Cristiano, A.; Musteata, S.; De Silvestri, S.; Bellandi, V.; Ceravolo, P.; Cesari, M.; Azzolino, D.; Sanna, A.; Trojaniello, D. Older Adults’ and Clinicians’ Perspectives on a Smart Health Platform for the Aging Population: Design and Evaluation Study. JMIR Aging 2022, 5, e29623. [Google Scholar] [CrossRef] [PubMed]
- Sumner, J.; Chong, L.S.; Bundele, A.; Lim, Y.W. Co-Designing Technology for Aging in Place: A Systematic Review. Gerontologist 2021, 61, e395–e409. [Google Scholar] [CrossRef] [PubMed]




| Service Scenario | Scenario Description | Interview Questions |
|---|---|---|
| A. Health Management Services | Focuses on health checkups, medication, and health monitoring, as well as related service access and barriers. | A-1. How do you usually manage your daily health? |
| A-2. Are the current community healthcare services meeting your needs? | ||
| B. Rehabilitation and Long-term Care Services | Addresses challenges in chronic disease management, post-treatment rehabilitation, and long-term care support. | B-1. Have you ever received rehabilitation or long-term care services? What problems did you encounter? |
| B-2. In your opinion, what are the current shortcomings of rehabilitation services? | ||
| C. Emotional Support and Social Interaction Services | Explores the impact of insufficient emotional support or limited social interaction on health status and service participation. | C-1. When feeling unwell, do you also feel lonely? |
| C-2. Are you able to obtain sufficient emotional support from your surroundings? | ||
| D. Integrated Daily Life Support Services | Focuses on difficulties related to transportation, household support, and daily living assistance. | D-1. What are your basic non-medical needs in daily life? |
| D-2. Are these needs currently well supported? | ||
| E. Community Service Access Services | Examines the accessibility and usability of community service systems. | E-1. Have you encountered any difficulties when using community services? |
| E-2. Does the service system design meet your expectations? | ||
| F. Personalised Service Design Services | Investigates the feasibility of providing personalised services tailored to individual needs. | F-1. If a unified platform could provide all of the above functions, what features would you most desire? |
| F-2. What type of interface design would be easiest for you to use? |
| Participant Group | Age | Gender | Education Level | Pre-retirement Occupation | Region |
|---|---|---|---|---|---|
| Community elderly | 63 | Female | Junior high school | Textile factory worker | Dongguan |
| 62 | Male | Senior high school | Laborer | ||
| 63 | Male | Vocational school | Construction worker | ||
| 70 | Female | Technical secondary school | Primary school teacher | Foshan | |
| 70 | Female | Primary school | Laborer | ||
| 63 | Female | Junior college | Market vendor | ||
| 72 | Female | Senior high school | Community care worker | ||
| 65 | Male | Vocational school | Technician | Guangzhou | |
| 68 | Male | University | University lecturer | ||
| 64 | Male | University | Medical administration | ||
| 65 | Female | Primary school | Laborer | Shenzhen | |
| 70 | Female | Junior high school | Bus driver | ||
| 69 | Male | Junior college | Laborer | ||
| 68 | Female | Junior high school | Housewife | ||
| 67 | Male | Senior high school | Taxi driver | ||
| 63 | Male | Senior high school | Retail salesperson | Zhuhai | |
| 65 | Male | Primary school | Tailor | ||
| 67 | Female | Senior high school | Manufacturing worker | ||
| 66 | Female | Senior high school | Primary school teacher | Zhongshan | |
| 66 | Female | Junior high school | Primary school teacher | ||
| 60 | Female | Primary school | Owner of a sewing shop | ||
| 62 | Male | Junior high school | Secondary school teacher | ||
| Community worker | Undisclosed | Female | Bachelor | / | Foshan |
| 42 | Male | Bachelor | / | Guangzhou | |
| 28 | Female | Master | / | Shenzhen | |
| 35 | Female | Bachelor | / | Dongguan | |
| 49 | Male | Senior high school | / | Zhongshan |
| Coding Stage | Objective of the Stage |
|---|---|
| A. Initial Coding | Initial coding involves breaking down interview transcripts line-by-line to identify meaningful units, allowing detailed interpretation of each participant’s narrative. The goal is to capture older adults’ service pain points, needs, and emotional responses while maintaining semantic consistency. Key pain points and service demands are inductively identified during this phase. |
| B. Focused Coding | After initial coding, this stage involves consolidating and abstracting frequently occurring or conceptually representative codes to extract core subthemes. Through constant comparison, these subthemes enable preliminary categorization of service demands, providing the basis for later theoretical construction. |
| C. Axial Coding | Axial coding integrates the concepts generated from focused coding, analyzing their causal relationships. This phase constructs a “Condition-Action-Result (C-A-R)” model, aiming to reveal the underlying mechanisms behind various types of service needs and how they interact with platform features. |
| D. Theoretical Coding | In the theoretical coding phase, prior findings are synthesized to generate abstract yet operable theoretical models. The outcome is a logic-based, generalizable framework that serves as the conceptual foundation for platform design and theoretical integration. |
| Code ID | Original Transcript (in Chinese) | Segment Code | Initial Coding (in Chinese) |
|---|---|---|---|
| T4-21 | “I still hope to receive continuous rehabilitation guidance … and ongoing rehabilitation training.” | T4-a21 | Hopes for post-discharge rehabilitation guidance and structured training to enhance recovery effectiveness. |
| T6-26 | “More rehabilitation therapists … to correct my movements.” | T6-a26 | Expects more individualized instruction from therapists to improve rehabilitation outcomes. |
| T1-29 | “The current rehabilitation and nursing services … are just passable.” | T1-a29 | Perceives current rehabilitation and nursing services as substandard, with a need for quality improvement. |
| Code ID | Original Transcript (in Chinese) | Initial Code ID | Initial Coding (in Chinese) | Focused Code ID | Focused Concept |
|---|---|---|---|---|---|
| T4-21 | “I still hope to receive continuous rehabilitation guidance … and ongoing rehabilitation training.” | T4-a21 | Hopes for post-discharge rehabilitation guidance and structured training to improve recovery outcomes. | T4-aa21 | Service Content Orientation |
| T6-26 | “More rehabilitation therapists … to correct my movements.” | T6-a26 | Expects therapists to provide more individualized guidance to enhance rehabilitation effectiveness. | T6-aa26 | Quality of Rehabilitation Service Delivery |
| T1-29 | “The current rehabilitation and nursing services … are just passable.” | T1-a29 | Perceives current rehabilitation and nursing services as suboptimal and needing improvement. | T1-aa29 | Personalised Collaboration |
| Code ID | Focused Concept (in Chinese) | Axial Code | Axial Category (Sub-Dimension) |
|---|---|---|---|
| T1-aa2 | Health information advice | A1 | Health Needs |
| S1-aa39 | Elderly individuals prefer ageing in place | A2 | Ageing-in-Place Needs |
| T8-aa75 | Emergency health response | A3 | Emergency Support Needs |
| Code | Subcategory (Subdimension) | Code | Core Category (Thematic Domain) |
|---|---|---|---|
| A1 | Health-related needs | AA1 | Health and Medical Care Needs |
| A2 | Ageing-in-place needs | ||
| A3 | Emergency support needs | ||
| B1 | Technology adaptation ability | BB1 | Technology Adaptation and Digital Learning |
| B2 | Technology Adaptation Challenges | ||
| B3 | Technology Adaptation Needs | ||
| B4 | Technology training needs | ||
| C1 | Emotional Needs | CC1 | Psychological and Emotional Support |
| C2 | Emotional Support | ||
| C3 | Social Needs | ||
| C4 | Social Support | ||
| C5 | Psychological needs | ||
| C6 | Psychological Support Challenges | ||
| D1 | Family support | DD1 | Family and Social Support |
| D2 | Community support | ||
| D3 | Challenges in Community Support | ||
| D4 | Community Support Needs | ||
| D5 | Community Infrastructure Support | ||
| E1 | Behavior-related needs | EE1 | Daily Life and Mobility Support |
| E2 | Lifestyle habits | ||
| E3 | Daily living needs | ||
| E4 | Material support needs | ||
| F1 | Policy-related barriers | FF1 | Policy and Resource Management |
| F2 | Resource management needs | ||
| F3 | Resource integration needs | ||
| G1 | Service content orientation | GG1 | Digital Platform and Intelligent Service Design |
| G2 | Service design challenges | ||
| G3 | Service design needs | ||
| G4 | Platform Design Needs | ||
| G5 | Resource integration mode | ||
| H1 | Adaptive Response Mechanism | HH1 | Smart Interactive Mechanisms of Digital Platforms |
| H2 | Personalised Coordination Mechanism | ||
| H3 | Intelligent Matching Mechanism | ||
| H4 | Needs Expression Mechanism | ||
| I1 | Social feedback and effectiveness | II1 | Effectiveness of Digital Platform Use |
| I2 | Resource response efficiency | ||
| I3 | Needs satisfaction efficiency |
| Needs Layer | Mechanism Layer | Outcome Layer |
|---|---|---|
| Health and Medical Care Needs | Intelligent Interaction Mechanisms of Digital Platforms | Usage Outcomes of Digital Platforms |
| Technology Adaptation and Digital Learning | (Subdimensions)
| (Subdimensions)
|
| Psychological and Emotional Support | ||
| Family and Social Support | ||
| Daily Life and Mobility Support | ||
| Policy and Resource Management | ||
| Smart Service Design of Digital Platforms |
| Original Quote (in Chinese) | Corresponding Needs Layer | Corresponding Mechanism Layer | Corresponding Outcome Layer |
|---|---|---|---|
| “When I first used the smart wristband to check my heart rate and step count, it was a bit confusing to set up.” | Technology Adaptation and Digital Learning | Adaptive Response Mechanism | Needs Fulfillment Effectiveness |
| “Sometimes the scheduling of community health lectures is inconvenient—either overlapping or at the wrong time.” | Health and Medical Care Needs | Adaptive Response Mechanism | Needs Fulfillment Effectiveness |
| “If the platform could help me book doctor appointments and specialist numbers in advance, it would save me a lot of trouble each time I go to a big hospital.” | Smart Service Design of Digital Platforms | Personalised Matching Mechanism | Resource Optimisation Effectiveness |
| Analytical Unit | Interpretation of Analytical Content |
|---|---|
| Need characteristics → Mechanism selection | Based on empirical data, older adults’ health management, technical interaction, emotional support, and behavioral convenience needs may trigger preferences for specific functional mechanisms. This leads to the selection of smart interactive mechanisms. For example, the need for blood pressure monitoring may activate the “simplified processing” function, while “overly complicated interfaces” may reduce usability. |
| Need types → Mechanism preference | Different types of needs correspond to preferences for different mechanisms. For example, health management may correspond to personalised matching; digital learning needs may activate adaptive response; and social participation needs may align with needs expression and feedback, highlighting the platform’s adaptive allocation capability. |
| Smart platform mechanism → Need responsiveness | Whether the smart platform’s embedded mechanisms are perceived as “useful” or “helpful” by older adults determines its responsiveness. For instance, a medication reminder feature or device may reduce memory-related health risks. Real-time interaction functions enhance clarity and convenience, thus improving perceived responsiveness. |
| Adaptive response mechanism → Technical barrier mitigation | For older adults who struggle with digital tools, adaptive response mechanisms can simplify usage through habit-based personalization, streamlined operations, and auxiliary prompts, ultimately reducing interaction burden and increasing motivation. |
| Intelligent matching mechanism → Accurate service targeting | This mechanism enables the system to analyze health profiles and automatically recommend appropriate services (e.g., dietary suggestions, activity matching), thereby improving life efficiency and increasing trust in the platform’s “lifestyle compatibility.” |
| Personalised collaboration mechanism → Cross-domain integration support | When needs span multiple domains—e.g., health, transportation, recreation—this mechanism coordinates support from various modules such as booking, escort services, or family co-care, ensuring seamless integration and enhanced service delivery. |
| Needs expression mechanism → Action-driven interaction | If the platform lacks accessible channels for articulating needs (e.g., one-click assistance, emotional support), older adults may disengage over time. Therefore, facilitating intuitive need expression is key to sustaining user participation. |
| Smart mechanism use → Perceived effectiveness | If the platform mechanisms function inconsistently, such as redundant services or unclear functions, this undermines perceived efficiency and trust. On the contrary, effective integration improves perceived system reliability and user confidence. |
| Original Quote (in Chinese) | Relationship Code | Thematic Relationship |
|---|---|---|
| “If there were a health platform, I hope it could manage things like medication reminders. My memory isn’t great, and I often forget appointments or which specialist to see at the hospital—it’s really troublesome. Also, if I could consult with a health coach when needed, that would be great for minor issues or mental concerns.” | A digital platform can support health monitoring, reminders, remote consultations, etc., improving healthcare service accessibility and helping older adults manage their health. | Health and Medical Needs ←→ Smart Platform Service Design |
| “My family really cares for me. They often check in on my physical condition and accompany me to see doctors. This emotional warmth makes me feel less anxious. But sometimes I feel lonely; I wish there were more community activities to talk, share stories, and feel less alone.” | The concern of family and friends has a direct emotional effect; when paired with community support, it helps alleviate loneliness. | Psychological and Emotional Support ←→ Family and Social Support |
| “Policies should help arrange more convenient transport services for the elderly, like community shuttles or easy access vehicles. Sometimes I don’t even know how to get to the hospital. Policies that consider this can really improve older adults’ ability to move freely.” | Policy design affects older adults’ ability to maintain independent mobility—for instance, through accessible transport or barrier-free environments. | Daily Living and Mobility Support ←→ Policy and Resource Management |
| Questionnaire Module | Corresponding Core Category from Theoretical Model | Associated Layer |
|---|---|---|
| Health and Medical Care Needs | Health and Medical Care Needs | Needs Layer |
| Technology Adaptation and Digital Learning | Technology Adaptation and Digital Learning | |
| Psychological and Emotional Support | Psychological and Emotional Support | |
| Family and Social Support | Family and Social Support | |
| Daily Life and Mobility Support | Daily Life and Mobility Support | |
| Policy and Resource Management | Policy and Resource Management | |
| Smart Service Design of Digital Platforms | Smart Service Design of Digital Platforms | Mechanism Layer |
| Intelligent Interaction Mechanisms of Digital Platforms | Intelligent Interaction Mechanisms of Digital Platforms | |
| Perceived Effectiveness of Digital Platform Use | Perceived Effectiveness of Digital Platform Use | Outcome Layer |
| Dimension | Cronbach’s Alpha |
|---|---|
| Health and Medical Care Needs | 0.91 |
| Technology Adaptation and Digital Learning Needs | 0.95 |
| Psychological and Emotional Support Needs | 0.96 |
| Family and Social Support Needs | 0.96 |
| Daily Life and Mobility Support Needs | 0.95 |
| Policy and Resource Management Needs | 0.95 |
| Smart Service Design of Digital Platforms | 0.97 |
| Intelligent Interaction Mechanisms of Digital Platforms | 0.95 |
| Perceived Effectiveness of Digital Platform Use | 0.94 |
| Dimension | KMO (Overall) | Bartlett’s Chi-Square | df | p-Value |
|---|---|---|---|---|
| Health and Medical Care Needs | 0.92 | 1240.369 | 15 | 3.48 × 10−255 |
| Technology Adaptation and Digital Learning Needs | 0.97 | 2588.731 | 45 | 0 |
| Psychological and Emotional Support Needs | 0.98 | 3939.056 | 91 | 0 |
| Family and Social Support Needs | 0.98 | 4001.502 | 91 | 0 |
| Daily Life and Mobility Support Needs | 0.96 | 2666.347 | 45 | 0 |
| Policy and Resource Management Needs | 0.96 | 2521.239 | 45 | 0 |
| Smart Service Design of Digital Platforms | 0.98 | 4717.906 | 120 | 0 |
| Intelligent Interaction Mechanisms of Digital Platforms | 0.97 | 2518.097 | 45 | 0 |
| Perceived Effectiveness of Digital Platform Use | 0.95 | 2022.101 | 28 | 0 |
| Dimension | Item | Factor Loading | Communality | Meets Threshold |
|---|---|---|---|---|
| Health and Medical Care Needs | 1 | 0.93 | 0.89 | Yes |
| Health and Medical Care Needs | 2 | 0.85 | 0.71 | Yes |
| Health and Medical Care Needs | 3 | 0.85 | 0.71 | Yes |
| … | … | … | … | Yes |
| Variable | Model 1 β | p-Value | Model 2 β | p-Value |
|---|---|---|---|---|
| Intercept | 32.98 | <0.001 *** | 32.57 | <0.001 *** |
| PCA1 | 4.38 | <0.001 *** | 4.25 | <0.001 *** |
| Variable | Model 1 β | p-Value | Model 2 β | p-Value |
|---|---|---|---|---|
| Intercept | 26.32 | <0.001 *** | 27.70 | <0.001 *** |
| PCA1 | 3.53 | <0.001 *** | 3.39 | <0.001 *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pan, L.; Hu, X. Designing Sustainable Digital Platforms for Ageing Societies: A User-Centred Multi-Level Theoretical Framework. Sustainability 2025, 17, 8305. https://doi.org/10.3390/su17188305
Pan L, Hu X. Designing Sustainable Digital Platforms for Ageing Societies: A User-Centred Multi-Level Theoretical Framework. Sustainability. 2025; 17(18):8305. https://doi.org/10.3390/su17188305
Chicago/Turabian StylePan, Langqian, and Xin Hu. 2025. "Designing Sustainable Digital Platforms for Ageing Societies: A User-Centred Multi-Level Theoretical Framework" Sustainability 17, no. 18: 8305. https://doi.org/10.3390/su17188305
APA StylePan, L., & Hu, X. (2025). Designing Sustainable Digital Platforms for Ageing Societies: A User-Centred Multi-Level Theoretical Framework. Sustainability, 17(18), 8305. https://doi.org/10.3390/su17188305






