Abstract
Breastfeeding is the natural way to feed a baby in the first months of life. It is an option with a low environmental impact, as it is a natural and renewable food that does not pollute. It is the optimal food for the infant, with nutritional and immunological advantages that reduce the prevalence of pregnancy disorders and provide benefits for the infant, the mother, and the environment. Its premature abandonment may have medium- and long-term consequences, as the use of formula milk is much more polluting. A descriptive, observational, cross-sectional study was carried out between December 2020 and January 2021, involving 96 breastfeeding women. Sociodemographic and obstetric variables were collected. A validated Spanish version of the Breastfeeding Self-efficacy Scale-Short Form (BSES-SF) was used. Factors that may lead to the early cessation of breastfeeding among the mothers that were studied are a high level of education, a lack of preparation for childbirth, a lack of security, a lack of confidence in preparation for childbirth, a lack of self-confidence, discomfort with breastfeeding in the presence of others, and a low level of maternal satisfaction. Married women and women whose partners support breastfeeding are significantly more satisfied with exclusive breastfeeding than single and divorced women. Adequate and protocolised care must be provided. Education and support for parents to allow for optimal breastfeeding and reduce the environmental impact of formula feeding is essential.
1. Introduction
Breastfeeding is the most effective natural way to feed a baby in the first months of life [1]. For millennia, breast milk has been the sole source of nourishment for newborns (NBs). It is the optimal food for infants, providing them with many nutritional and immunological benefits [2]. Breast milk also reduces the prevalence of digestive disorders, bacteraemia, and pneumonia, among others [3]. In addition, breastfeeding provides psychological benefits for both the infant and the mother [4]. The premature abandonment of breastfeeding can lead to serious medium- to long-term consequences for the infant such as hypertriglyceridaemia and malnutrition [5].
Human milk has come to be considered “the first vaccine” a child receives, as it has the ability to protect the child from the frequent infections that can occur in the first year of life. The importance of breast milk in the first year of life is critical, as this is the period of the most rapid growth and development in human life [6].
Vila Candel et al. [6] stated the importance of supporting breastfeeding mothers and their environment to ensure the maintenance of exclusive breastfeeding (EBF), as the prevalence of this is low in our country (Spain) compared to other European countries. Nurses play a key role in promoting EBF until at least 6 months and in complying with the World Health Organisation’s (WHO) maintenance recommendations. To do this, we need to raise awareness in society [7,8,9].
1.1. Breastfeeding
BF is the natural way to feed a baby. Breastmilk is a fluid adapted that is to the baby’s nutritional and immunological needs as he or she grows [8]. During the first six months of life, healthy newborns do not need to take any additional supplements. It is from the age of 6 months that the WHO recommends the gradual incorporation of other foods [10] and EBF is recommended during the first 6 months of life due to all the benefits of this practice. More and more cases are observed where mothers abandon BF before this time [11]. The early abandonment of breastfeeding leads to personal, social, and health difficulties [12]. One of the factors involved in the abandonment of BF are the sociological changes that occurred throughout the 19th and 20th century, including the incorporation of women into salaried work. Another factor that may interfere with the abandonment is the advances in chemical sciences, which modify cow’s milk, making it acceptable, and thus causing it to substitute natural milk [13].
Currently, BF is offered to the baby ad libitum. It is therefore recommended to offer breastfeeding when the baby asks for it, bearing in mind that crying is a late sign of hunger, and for as long as the baby wants, until it spontaneously releases the mother’s nipple [14]. According to Mangesi et al. [15], milk production is regulated according to the baby’s needs, the composition of milk at the beginning and end of the feeding is different, and the baby feeds until good emptying of the breast is achieved. This avoids the excessive accumulation of milk, which can cause engorgement and mastitis [16].
The Spanish Association of Paediatrics (AEP) states that many babies, in addition to nourishment, seek comfort at the breast. Delayed feeding has a negative effect on the baby and the mother [17].
1.2. Sustainability of Breast Milk
In addition to all the analysed advantages, BF is undoubtedly an option with a high environmental impact, as it is a natural and renewable food that requires no fuel, no water for cleaning, and no waste.
As it requires no production, packaging, or transport, it leaves no carbon footprint on the environment. A UK study [18] showed that breastfeeding for six months saves 95–153 kg of CO2 per baby compared to formula feeding, which is equivalent to taking 50,000–77,500 cars off the road each year.
Another study showed that, in the USA alone, more than 32 million kW of energy is used annually to process, package, and transport infant formula, and 550 million cans, 86,000 tonnes of metal, and 364,000 kg of paper are sent to the landfill each year [19]. Formula milk contributes to environmental degradation and climate change, so promoting breastfeeding is essential for the environment [20].
1.3. Factors That Determine Breastfeeding Success
Several psychosocial factors can affect the success or failure of breastfeeding. These include advice and experiences during pregnancy and childbirth, acceptance of community or family norms, physical difficulties, or problems at work [17]. The early initiation of breastfeeding increases the success of breastfeeding. In the first hour after birth, the infant has very sensitive reflexes and tactile areola stimulation (sensitive period) [21]. For this reason, it is recommended that the baby is placed on the mother’s abdomen within half an hour of birth to ensure uninterrupted skin-to-skin contact [22]. A strong affectionate bond develops between the two, and the newborn’s metabolic capacity develops through this type of contact and postnatal breastfeeding.
The most common reason for breastfeeding failure among mothers is a drop in milk production. This is often due to the mother’s subjective thinking, which is mistakenly attributed to the baby’s hunger, or a loss of motivation to breastfeed, which she tries to justify with a lack of secretion [11].
During pregnancy, attendance at breastfeeding counselling and support from health care providers are the most important factors in initiating breastfeeding [11]. The decision to breastfeed is usually made in the first trimester of pregnancy. However, many mothers decide to breastfeed late in pregnancy or after giving birth [17,21]. Sayres and Visentin [23] show that the rate of breastfeeding doubles if the mother has received advice from the midwife during pregnancy, so it is important to address issues such as nipple care, the benefits of breastfeeding, and correct maternal feeding [21].
The characteristics of women in society, such as their cultural environment, education, social class, and work, influence the decision to breastfeed [23]. The role of the partner is very important in this decision. If the partner is not supportive, breastfeeding will not even be considered, or weaning will occur prematurely.
Despite the multiple benefits of breastfeeding for both mother and child, as well as for the environment, many mothers decide not to breastfeed or to stop breastfeeding before their newborns are 6 months old. Therefore, the aim of this study was to analyse the levels of self-efficacy in breastfeeding and the factors that cause early abandonment, determining the degree of mothers’ satisfaction with exclusive breastfeeding, and analysing the reasons for abandonment and the socio-cultural characteristics associated with the duration of breastfeeding.
2. Materials and Methods
A descriptive, observational, and retrospective self-report survey study was carried out using an accidental sample of all breastfeeding women attending the nursing consultation (midwife) of different Primary Health Care services or the paediatric telephone consultation during the study period who consented to participate by signing the informed consent form. The centres where the study was carried out included the Algemesí Health Center of the La Ribera Health Department (Valencia), the Xiprerets, Manises, Quart de Poblet and Mislata Health Centers, and the maternity and delivery ward of the Manises Hospital of the Manises Health Department (Valencia) and the Gandía Health Department (Valencia).
Inclusion criteria were women over 18 years of age who started breastfeeding after childbirth, who could speak and read Spanish without difficulty, and whose infants were aged between 6 and 24 months. Exclusion criteria included breastfeeding women with preterm infants, multiple births, mothers with mental disabilities, or mothers or children with medical problems that prevent or seriously hinder breastfeeding.
During the data collection period, the average number of births in the study centres was 1620 per year. The sample of 96 breastfeeding women in this study therefore represents 5.93% of the annual average. The sample size was calculated using the G*Power software v.3.1.9.6 [24]. Thus, for between-participant comparisons, a minimum sample size of 54 is suggested to ensure a large effect in nonparametric comparisons, or 52 if a parametric approach is chosen, both with 80% statistical power.
Data collection took place between December 2020 and January 2021. Information was collected by personal or telephone interview in view of the pandemic situation during the study.
2.1. Variables
Sociodemographic and obstetric variables were collected (age, nationality, marital status, whether she has a stable partner, whether her partner supports exclusive breastfeeding, level of education, profession, current occupation, number of children, order of children, whether she had previous children who were breastfed and for how long, type of delivery, birth preparation assistance, whether she was given information at her health centre about breastfeeding during pregnancy). In addition, a validated Spanish version of the Breastfeeding Self-efficacy Scale-Short Form (BSES-SF) was used [25]. This is a self-administered instrument that measures breastfeeding self-efficacy. It has 14 items that are rated on a 5-point Likert scale, so the total score ranges from 14 to 70. The 14 questions are divided into two distinct domains: intrapersonal thoughts (Q1, Q2, Q3, Q4, Q9 and Q14) and breastfeeding techniques (Q5, Q6, Q7, Q8, Q10, Q11, Q12 and Q13). A higher score corresponds to better breastfeeding self-efficacy. The timing of BSES measurement varies in the literature, including antenatal, hospital, and up to several months postpartum. Responses were the retrospective view of the respondent of the first six months after birth. In this study, the internal consistency of the BSES-SF was confirmed by Cronbach’s alpha 0.86.
2.2. Statistical Analysis
For the presentation of descriptive data, central tendency and dispersion statistics are used for continuous variables. Qualitative variables are expressed as case values and percentages. Data from the BSES-SF scale are presented as a percentile. The normality of the distributions was analysed using the Shapiro–Wilk test. The Mann–Whitney test was used to compare two independent samples and the Kruskal–Wallis test was used to compare three or more. A logistic regression model was performed to analyse the probability of early breastfeeding cessation using socio-demographic variables as predictors. For this purpose, the early cessation of breastfeeding was dichotomised by setting the cut-off point at 4 months, since, in Spain, maternity leave after childbirth lasts 16 weeks. The Nagelkerke R-squared was used as a measure of overall predictive performance. Calibration was assessed using the Hosmer–Lemeshow goodness-of-fit test. The area under the ROC curve (AUC) reflects the discrimination of the resulting model. All socio-demographic variables that were significant in the univariate analysis were added to the model. The categories used as a reference were those that the literature review indicates to be a protective factor for exclusive breastfeeding. A significance level of 0.05 was used for all tests.
2.3. Ethical Approval and Consent to Participate
The study was conducted in accordance with the principles set out in the Declaration of Helsinki. Approval was obtained from the Ethics Committee of the Hospital de la Fe (approval code 2018/0091, dated 11 April 2018), and informed consent was obtained from all participants.
3. Results
The final analysed sample comprised 96 lactating women. The mean age was 33.0 years (SD = 4.49), with a range between 19 and 43 years. Table 1 describes the socio-demographic characteristics of the sample.

Table 1.
Socio-demographic characteristics of the sample.
The mean duration of breastfeeding is 69.56 days (SD = 54.28) and 50% of women breastfeed less than 60 days. We observed a lot of variability, with a maximum reported value of 180 days and a minimum of 1 day. The Shapiro–Wilk test allows us to state that the distribution of duration does not conform to the normal distribution (p < 0.05). Table 2 shows the analysis of the duration of breastfeeding in the first 6 months of life of the newborn according to the different socio-demographic variables.

Table 2.
Duration of breastfeeding according to sociodemographic variables.
We found statistically significant relationships in the duration of breastfeeding according to marital status, stable partner, partner support, educational attainment, type of delivery, and attendance at antenatal classes. We see that married women breastfeed longer than divorced or single women. Women who have a stable partner and are supported by their partner breastfeed longer. Mothers with a tertiary education have a shorter duration than those with an intermediate education. Those who had their babies by normal birth have a longer duration of breastfeeding than those who had their babies through a dictocic birth or caesarean section, and finally, those who attended antenatal classes have a much longer duration of breastfeeding than those who did not.
The median score of the BSES-SF Scale was 60.0, with an Interquartile Range (IQR) between 16.5 and 112.5. Table 3 shows the analysis of maternal satisfaction according to socio-demographic variables:

Table 3.
BSES-SF score according to sociodemographic variables.
We found no statistically significant differences between the questionnaire scores and the analysed variables, except for the type of delivery. Mothers with natural or instrumental delivery were significantly more satisfied with breastfeeding than those who delivered by caesarean section.
Table 4 analyses the association between all the answers to the questionnaire and the duration of breastfeeding to detect possible reasons for abandonment.

Table 4.
Association between responses to the BSES-SF questionnaire and breastfeeding duration.
In Table 4, we can observe a significantly longer duration in six questions, three from the Intrapersonal Thoughts domain (Q2, Q4 and Q9) and three from the Breastfeeding Technique domain (Q7, Q8, and Q13). These results, which show higher scores for mothers who breastfeed for longer, reveal positive attitudes towards the act of breastfeeding itself, such as the desire to breastfeed, personal satisfaction, readiness to breastfeed when the baby needs it, confidence in the correctness of the process, a sense of comfort in the act itself, and a positive attitude towards life in general.
A binary logistic regression model was performed, using all socio-demographic variables that were significant in the univariate analysis as predictors of a longer duration of breastfeeding. The results of the model are presented in Table 5.

Table 5.
Logistic regression model for early breastfeeding cessation.
The explained variance of the model was 62.7%. The model showed adequate calibration (Chi2 = 4.409 df = 8; p = 0.818) and good discrimination (AUC = 0.845; 95% CI 0.741–0.949) (Figure 1). We found that the increase in the probability of dropping out is related to higher educational attainment. On the other hand, having a stable partner and attending childbirth preparation is associated with a longer duration of breastfeeding.
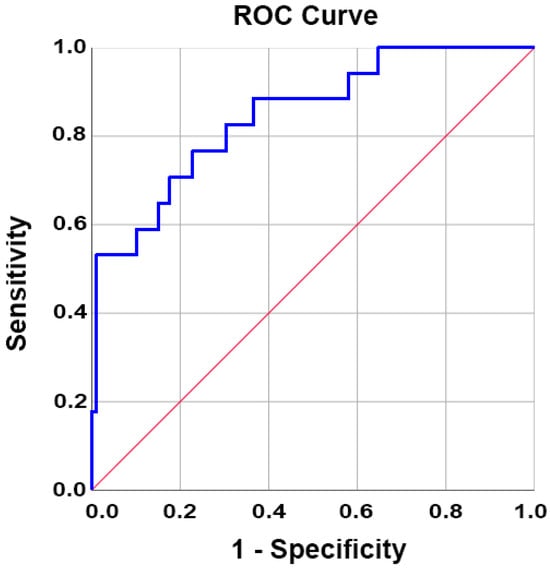
Figure 1.
Receiver operating characteristic (ROC) curve of the model of early breastfeeding cessation as a function of socio-demographic variables. The diagonal line indicates no discrimination above chance.
4. Discussion
Although the WHO, the AEP, and other associations recommend exclusive breastfeeding for up to 6 months [10,26], our study shows that the average does not exceed 70 days and half of the women breastfeed for less than 60 days, which is well below these recommendations. This is not an isolated finding; a study carried out in Guipúzcoa [27] shows that while a high percentage of women start breastfeeding, after the first 4 months, this percentage drops from 84.8% to 53.7%. Other studies report percentages of initiation that are below this, with a considerable decrease after the third month of breastfeeding [6,28,29,30], which is more similar to the results found in our study.
A total of 76.1% of the mothers in this study are over 30 years of age. The mean age of mothers who breastfeed their children was 33 years (SD 4.49), slightly higher than that reported by the 2010 project of the Child and Perinatal Health Observatory (OSIP) [29], a project of the Dirección General de Salud Pública de la Conselleria de Sanitat de la Comunitat Valenciana, which aims to provide information and public dissemination on child health; this put the mean age of mothers at 31 years. According to the National Institute of Statistics (INE) [31], the average age of mothers at the national level is 32.08 years and at the level of the province of Valencia the average is 32.32 years, very similar values to those found in our study. We found no statistically significant differences in the sociodemographic factor age. However, some studies [27,28,32,33,34,35] identify that the older the mother, the longer the duration of BF, with older mothers being those who breastfeed the longest.
In the literature, we find that the initiation and abandonment of BF is related to maternal factors (lack of knowledge, lack of adequate counselling, age, insecurity when breastfeeding, etc.) and other community factors also play a role, whether at the level of the family, the health system, etc. [28,33]. In the present study, we found an association between satisfaction with breastfeeding and the type of delivery. We observed that women who gave birth naturally were much more satisfied with BF than those who delivered by instrumental delivery or caesarean section. We have also seen that women who give birth naturally have a significantly longer duration of lactation than women who give birth by instrumental delivery or caesarean section. Other studies [36,37] support these findings and show that caesarean delivery is a factor that has a negative influence on the timing of BF. On the other hand, Cakmak and Kuguoglu [38] try to respond to this fact by stating that mothers who give birth by caesarean section need more help with the initiation of breastfeeding after delivery and this seems to influence the subsequent duration of breastfeeding.
In terms of duration, it has been observed that the presence of a stable partner and the receipt of support from the partner have a direct impact on the duration of breastfeeding. This may be the reason why married women breastfeed for significantly longer than single or divorced women. Other studies [39,40] confirm this assertion, as mothers who are divorced or single are more likely to give up breastfeeding early due to a lack of emotional stability, fatigue, and lack of support. Similarly, in the present study, we found that the women who are more satisfied with BF are married, although the differences with respect to single or divorced women are not statistically significant. In the model of early breastfeeding cessation, we also found that partner stability is a protective factor for breastfeeding, consistent with the work of Littman et al. [41], who found that mothers whose partners were supportive of breastfeeding were more likely to breastfeed for longer.
There is evidence that mothers who have had antenatal classes have a much longer duration of breastfeeding than those who have not. We have also seen that they are generally more satisfied, according to the results of the BSES-SF scale. However, this difference is not statistically significant. On the other hand, in the model of early breastfeeding cessation, we have seen that support for childbirth preparation is a protective model. This is mainly due to the counselling provided by health professionals, which makes breastfeeding safer and more comfortable. In addition, Alus et al. [42] state that the success of BF requires a great deal of preparation and support from skilled personnel from the very beginning.
Surprisingly, we have observed in our study that mothers with a tertiary level of education have a shorter duration than mothers with an intermediate level of education. Furthermore, we have seen in the model that an increase in the educational level of breastfeeding mothers is a risk factor for the abandonment of breastfeeding. This is consistent with the study by Chen et al. [43], which showed that infants whose mothers had higher education were more likely to experience breastfeeding cessation. A plausible explanation could be that mothers with higher levels of education tend to have higher levels of employment and demand, which may contribute to their early cessation of breastfeeding, as Cooklin et al. note [44]. In contrast, other recent studies, such as Aidam’s [37], show that mothers with higher levels of education continue breastfeeding longer because they are more aware of its benefits for the baby’s health and for themselves. Other studies find no association between breastfeeding duration and the mother’s level of education [45,46,47].
In our study, we found that the desire to breastfeed, personal satisfaction, willingness to breastfeed when the baby needs it, confidence in the correctness of the process, and a sense of comfort are the causes of early cessation of breastfeeding, making discomfort and insecurity risk factors for breastfeeding. The most dissatisfied women surveyed were those who had not attended antenatal classes, most likely due to lack of information and support. Nursan et al. [48] disagree with these findings and state that there is no significant relationship between maternal satisfaction and previous antenatal education classes. However, the findings of Pinilla et al. [49] are consistent with ours. Effective breastfeeding requires the establishment of policies and a breastfeeding-friendly environment, as well as the development of personal skills through information, education, and training. It is essential that mothers have the knowledge to increase their milk production and that they are well supported by trained staff, which reduces their sense of insecurity.
It should be recalled that, in 2016, breastfeeding was recognized as a human right for babies and mothers that should be promoted and protected, according to a statement issued by the United Nations (UN) Human Rights Council in Geneva [50]. No other health behaviour has such a broad and long-lasting impact on public health. Protecting, supporting, and promoting breastfeeding helps to safeguard planetary and human health by minimising environmental damage [51].
Limitations
The limitations of the present study include the small sample size. This may limit the generalizability of the results. The aim of this research was to achieve a larger number of face-to-face interviews to obtain an optimal sample size. However, given the circumstances of the global pandemic, sample collection was hampered by many telephone visits. Many mothers refused to be interviewed because they wanted to spend as little time as possible at the health centre. On the other hand, given the pandemic situation, it is likely that concerns about the transmission of the virus through breastfeeding may have also contributed to the reduction in breastfeeding. Finally, although the results of this study seem to indicate that satisfaction levels may be associated with a longer duration of breastfeeding, the limitations of the sampling and the retrospective questionnaire response design mentioned above preclude broad generalisation of the results, although these findings suggest the need for individual assessment and intervention to support breastfeeding women.
5. Conclusions
A high level of education, lack of preparation for childbirth, instrumental delivery or caesarean section, lack of security, feeling uncomfortable breastfeeding in the presence of others, and low maternal satisfaction were factors associated with early breastfeeding cessation among mothers in the study. Women in the study who are married are significantly more satisfied with exclusive breastfeeding and breastfeed longer than single and divorced women.
Effective breastfeeding requires the establishment of policies and a breastfeeding-friendly environment. It also requires the development of personal skills through information, education, and training. It is essential that mothers have the knowledge to increase their milk production and that they are adequately supervised by qualified and well-trained personnel, which will reduce their sense of insecurity, increasing advocacy efforts among mothers with higher education.
Based on this analysis, it is important to propose further research with new intervention strategies in the future to contribute to the social normalisation of breastfeeding and to help many breastfeeding mothers avoid early cessation of breastfeeding, which will contribute to the protection of planetary and human health by minimising environmental damage. Adequate and protocolised care must be provided. Education and support for parents on optimal breastfeeding and the environmental impact of formula feeding is essential.
Author Contributions
Conceptualization, M.T.M.-L., A.A.-C. and M.P.-B.; methodology, M.T.M.-L. and M.P.-B.; software, M.P.-B.; validation, M.T.M.-L.; formal analysis, M.P.-B.; investigation, A.A.-C., J.P.-M., A.P.-F., M.E.L.-G., F.L.-C. and F.T.-A.; data curation, M.P.-B.; writing—original draft preparation, M.T.M.-L., A.A.-C., J.P.-M., A.P.-F., M.E.L.-G., F.L.-C., F.T.-A. and M.P.-B.; writing—review and editing, M.T.M.-L., A.A.-C., J.P.-M. and M.P.-B.; supervision, M.T.M.-L. All authors have read and agreed to the published version of the manuscript.
Funding
The publication costs of this work have been financed by the Catholic University of Valencia under grant 2023-275-001.
Institutional Review Board Statement
The study was conducted in accordance with the principles set out in the Declaration of Helsinki. Approval was obtained from the Ethics Committee of the Hospital de la Fe of Valencia (Spain). (Approval code 2018/0091 dated 11 April 2018).
Informed Consent Statement
Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Yi, D.Y.; Kim, S.Y. Human Breast Milk Composition and Function in Human Health: From Nutritional Components to Microbiome and MicroRNAs. Nutrients 2021, 13, 3094. [Google Scholar] [CrossRef] [PubMed]
- Nyqvist, K.H.; Häggkvist, A.P.; Hansen, M.N.; Kylberg, E.; Frandsen, A.L.; Maastrup, R.; Ezeonodo, A.; Hannula, L.; Koskinen, K.; Haiek, L.N. Expansion of the ten steps to successful breastfeeding into neonatal intensive care: Expert group recommendations for three guiding principles. J. Hum. Lact. 2012, 28, 289–296. [Google Scholar] [CrossRef]
- Britton, C.; McCormick, F.M.; Renfrew, M.J.; Wade, A.; King, S.E. Support for breastfeeding mothers. Cochrane Database Syst. Rev. 2007, 1, CD001141, Erratum in Cochrane Database Syst. Rev. 2012, 5, CD001141. [Google Scholar]
- Stelmach, I.; Kwarta, P.; Jerzynska, J.; Stelmach, W.; Krakowiak, J.; Karbownik, M.; Podlecka, D.; Hanke, W.; Polanska, K. Duration of breastfeeding and psychomotor development in 1-year-old children-Polish Mother and Child Cohort Study. Int. J. Occup. Med. Environ. Health 2019, 32, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, R.A.; Lawrence, R.M. Breastfeeding. A Guide for the Medical Profession, 8th ed.; Elsevier: Philadelphia, PA, USA, 2016. [Google Scholar]
- Vila-Candel, R.; Soriano-Vidal, F.J.; Murillo-Llorente, M.; Pérez-Bermejo, M.; Castro-Sánchez, E. Maintenance of exclusive breastfeeding after three months postpartum: An experience in a health department of a Valencian Community. Aten. Primaria 2019, 51, 91–98. [Google Scholar] [CrossRef] [PubMed]
- WHO Infant and Young Child Nutrition (Progress and Evaluation Report); and Status of Implementation of the International Code of Marketing of Breast-Milk Substitutes Promoting the Infant-Feeding Ideal. Available online: https://iris.who.int/bitstream/handle/10665/170799/EB89_R18_eng.pdf?sequence=1&isAllowed=y (accessed on 3 December 2023).
- UNICEF Innocenti Declaration 2005 on Infant and Young Child Feeding. Available online: https://www.unicef-irc.org/publications/435-innocenti-declaration-2005-on-infant-and-young-child-feeding.html (accessed on 3 December 2023).
- UNICEF Breastfeeding. A Mother’s Gift, for Every Child. Available online: https://www.unicef.org/media/48046/file/UNICEF_Breastfeeding_A_Mothers_Gift_for_Every_Child.pdf (accessed on 3 December 2023).
- WHO Exclusive Breastfeeding for Optimal Growth, Development and Health of Infants. Available online: https://www.who.int/tools/elena/interventions/exclusive-breastfeeding (accessed on 3 December 2023).
- Estévez González, M.; Martell Cebrián, D.; Medina Santana, R.; García Villanueva, E.; Saavedra Santana, P. Factors associated with discontinuance of breastfeeding. An. Esp. Pediatr. 2002, 56, 144–150. [Google Scholar] [CrossRef]
- García García, N.; Fernández Gutiérrez, P. Mothers’ knowledge and attitudes towards breastfeeding in an IHAN hospital. Metas Enferm. Feb. 2018, 21, 50–58. [Google Scholar] [CrossRef]
- Parsa, P.; Masoumi, Z.; Parsa, N.; Parsa, B. Parents’ Health Beliefs Influence Breastfeeding Patterns among Iranian Women. Oman Med. J. 2015, 30, 187–192. [Google Scholar] [CrossRef]
- The Breastfeeding Committee (AEP). Clinical Practice Guideline on Breastfeeding. Available online: https://www.aeped.es/sites/default/files/guia_de_lactancia_materna.pdf (accessed on 3 December 2023).
- Mangesi, L.; Zakarija-Grkovic, I. Treatments for breast engorgement during lactation. Cochrane Database Syst. Rev. 2016, 2016, CD006946. [Google Scholar] [CrossRef]
- Crepinsek, M.A.; Taylor, E.A.; Michener, K.; Stewart, F. Interventions for preventing mastitis after childbirth. Cochrane Database Syst. Rev. 2020, 9, CD007239. [Google Scholar] [CrossRef]
- The Breastfeeding Committee (AEP). Protection, Promotion and Support of Breastfeeding in Europe: Strategic Plan. Available online: https://www.aeped.es/sites/default/files/5-europe_a_blueprint_for_action.pdf (accessed on 3 December 2023).
- Karlsson, J.O.; Garnett, T.; Rollins, N.C.; Röös, E. The carbon footprint of breastmilk substitutes in comparison with breastfeeding. J. Clean. Prod. 2019, 222, 436–445. [Google Scholar] [CrossRef]
- Coutsoudis, A.; Coovadia, H.M.; King, J. The breastmilk brand: Promotion of child survival in the face of formula-milk marketing. Lancet 2009, 374, 423–425. [Google Scholar] [CrossRef]
- Joffe, N.; Webster, F.; Shenker, N. Support for breastfeeding is an environmental imperative. BMJ 2019, 367, l5646. [Google Scholar] [CrossRef]
- Sayres, S.; Visentin, L. Breastfeeding: Uncovering barriers and offering solutions. Curr. Opin. Pediatr. 2018, 30, 591–596. [Google Scholar] [CrossRef]
- Pallás, C.R. Promocion de la Lactancia Materna. Programa de Actividades Preventivas y de Promoción de la Salud (PAPPS). Available online: https://www.aeped.es/sites/default/files/4-promocion_de_lactancia_previnfad.pdf (accessed on 6 December 2023).
- Bengough, T.; Dawson, S.; Cheng, H.L.; McFadden, A.; Gavine, A.; Rees, R.; Sacks, E.; Hannes, K. Factors that influence women’s engagement with breastfeeding support: A qualitative evidence synthesis. Matern. Child Nutr. 2022, 18, e13405. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Marco Alegría, T.D.; Martínez Martínez, D.; Muñoz Gómez, M.J.; Sayas Ortiz, I.; Oliver-Roig, A.; Richart-Martínez, M. Spanish reference values for the Breastfeeding Self-Efficacy Scale-Short Form BSES-SF. An. Sist. Sanit. Navar. 2014, 37, 203–211. [Google Scholar] [CrossRef]
- AEP Spanish Association of Paediatrics. Breastfeeding Committee. Recommendations on Breastfeeding. Available online: https://www.aeped.es/sites/default/files/201202-recomendaciones-lactancia-materna.pdf (accessed on 3 December 2023).
- Oribe, M.; Lertxundi, A.; Basterrechea, M.; Begiristain, H.; Santa Marina, L.; Villar, M.; Dorronsoro, M.; Amiano, P.; Ibarluzea, J. Prevalence of factors associated with the duration of exclusive breastfeeding during the first 6 months of life in the INMA birth cohort in Gipuzkoa. Gac. Sanit. 2015, 29, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Espinoza Cadima, C.; Zamorano Jiménez, C.A.; Graham Pontones, S.; Gutierrez Orozco, A. Factors determining the duration of breastfeeding during the first three months of life. An. Med. 2014, 59, 120–126. [Google Scholar]
- Observatorio de Salud Infantil y Perinatal Child and Perinatal Health Observatory. Situación de la Salud Infantil y Perinatal en la Comunitat Valenciana en 2009. Available online: http://www.sogcv.com/archivos/boletin_conselleria_sanidad_salud_perinatal.pdf (accessed on 3 December 2023).
- Ortega García, J.A.; Pastor Torres, E.; Martínez Lorente, I.; Bosch Giménez, V.; Quesada López, J.J.; Hernández Ramón, F.; Alcaráz Quiñonero, M.; Llamas del Castillo, M.M.; Torres Cantero, A.M.; García de León González, R.; et al. Malama project in the Region of Murcia (Spain): Environment and breastfeeding. An. Pediatr. 2008, 68, 447–453. [Google Scholar] [CrossRef] [PubMed][Green Version]
- INE National Statistics Institute. Type of Breastfeeding According to Sex and Autonomous Community. Population Aged 6 Months to 4 Years. Available online: http://www.ine.es/jaxi/Datos.htm?path=/t15/p419/a2006/p07/l0/&file=03111.px (accessed on 3 December 2023).
- Rosa Niño, M.; Gioconda Silva, E.; Eduardo Atalah, S. Factors associated with exclusive breastfeeding. Rev. Chil. Pediatric. 2012, 82, 161–169. [Google Scholar]
- Yngve, A.; Sjöström, M. Breasfeeding determinants and a suggested framework for action in Europe. Public Health Nutr. 2001, 4, 729–739. [Google Scholar] [CrossRef] [PubMed]
- Prendes Labrada, M.C.; Vianco del Río, M.; Gutiérrez González, R.M.; Guibert Reyes, W. Maternal factors associated with the duration of breastfeeding in Santos Suárez. Rev. Cubana Med. Gen. Integr. 1999, 15, 397–402. [Google Scholar]
- Escribá Agaúir, V.; Más Pons, R.; Colomer Revuelta, C. Duration of breastfeeding and work activity. An. Esp. Pediatr. 1996, 44, 437–441. [Google Scholar]
- Ruiz Pizzi, C.V. Motivations of Mothers of Infants under 6 Months Attending the Ñuñoa Milk League to Practice Effective Exclusive Breastfeeding. Ph.D. Thesis, Faculty of Medicine, University of Chile, Santiago, Chile, 2015. [Google Scholar]
- Aidam, B.A.; Pérez-Escamilla, R.; Lartey, A.; Aidam, J. Factors associated with exclusive breastfeeding in Accra, Ghana. Eur. J. Clin. Nutr. 2005, 59, 789–796. [Google Scholar] [CrossRef][Green Version]
- Cakmak, H.; Kuguoglu, S. Comparison of the breastfeeding patterns of mothers who delivered their babies per vagina and via cesarean section: An observational study using the LATCH breastfeeding charting system. Int. J. Nurs. Stud. 2007, 44, 1128–1137. [Google Scholar] [CrossRef]
- Mateu Céscar, C.; Vila Candel, R.; Bellvis Vázquez, E.; Planells López, E.; Martinez Ballester, A.; Gómez Sánchez, M.J.; Espuig Sebastián, R. Duration of breastfeeding at 3 months postpartum. Enfermería Integr. 2016, 113, 64–70. [Google Scholar]
- Linares, B.; Bonilla, J.A.; Vergara, E. Maternal factors associated with duration of breastfeeding in a regional hospital. Pediatría de México. 2009, 11, 15–19. [Google Scholar]
- Littman, H.; Medendorp, S.V.; Goldfarb, J. The decision to breastfeed: The importance of fathers’ approval. Clin. Pediatr. 1994, 33, 214–219. [Google Scholar] [CrossRef]
- Alus Tokat, M.; Okumus, H.; Dennis, C.L. Translation and psychometric assessment of the Breast-feeding Self-Efficacy Scale-Short Form among pregnant and postnatal women in Turkey. Midwifery 2010, 26, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Cheng, G.; Pan, J. Socioeconomic status and breastfeeding in China: An analysis of data from a longitudinal nationwide household survey. BMC Pediatr. 2019, 19, 167. [Google Scholar] [CrossRef] [PubMed]
- Cooklin, A.R.; Donath, S.M.; Amir, L.H. Maternal employment and breastfeeding: Results from the longitudinal study of Australian children. Acta Paediatr. 2008, 97, 620–623. [Google Scholar] [CrossRef]
- Colodro-Conde, L.; Sánchez-Romera, J.F.; Tornero-Gómez, M.J.; Pérez-Riquelme, F.; Polo-Tomás, M.; Ordoñana, J.R. Relationship between level of education and breastfeeding duration depends on social context: Breastfeeding trends over a 40-year period in Spain. J. Hum. Lact. 2011, 27, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Durán Menéndez, R.; Villegas Cruz, D.; Sobrado Rosales, Z.; Almanza Mas, M. Psychosocial factors that influence the abandonment of breastfeeding. Rev. Cubana Pediatr. 1999, 71, 72–79. [Google Scholar]
- Sacristán, A.; Lozano, J.; Gil, M.; Vega, A. Current situation and factors conditioning breastfeeding in Castilla y León. Rev. Pediatría Atenció Primaria 2011, 13, 33–46. [Google Scholar]
- Nursan, C.; Dilek, K.; Sevin, A. Breastfeeding Self-efficacy of Mothers and the Affecting Factors. Aquichan 2014, 14, 327–335. [Google Scholar] [CrossRef]
- Pinilla Gómez, E.; Dominguez Nariño, C.C.; García Rueda, A. Adolescent mothers, a challenge facing the factors that influence exclusive breastfeeding. Enferm. Glob. 2014, 13, 59–70. [Google Scholar]
- United Nations. Joint Statement by the UN Special Rapporteurs on the Right to Food, Right to Health, the Working Group on Discrimination against Women in Law and in Practice, and the Committee on the Rights of the Child in Support of Increased Efforts to Promote, Support and Protect Breast-Feeding. Available online: https://www.ohchr.org/en/statements/2016/11/joint-statement-un-special-rapporteurs-right-food-right-health-working-group?LangID=E&NewsID=20871 (accessed on 3 December 2023).
- UNICEF Breastfeeding and Climate Change. A Case Study by the Baby Friendly Initiative. Available online: https://www.unicef.org.uk/babyfriendly/breastfeeding-and-climate-change/#:~:text=Breastmilk%20requires%20no%20packaging%2C%20shipping,helps%20to%20minimise%20environmental%20impact (accessed on 3 December 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).