Social Infrastructure During the COVID-19 Pandemic: Evaluating the Impact of Outdoor Recreation on Pandemic Dynamics in Europe
Abstract
1. Introduction
2. Literature Review
3. Materials and Methods
3.1. Sampling Procedure and Research Timeframe
3.2. Measures of Variables
- Visitation trends: In response to the primary aim of this study, in order to assess the changes in public demand for social infrastructures driven by the COVID-19 pandemic. This study thereby recognizes the increase and decline in the six studied social infrastructure visitations to pre-pandemic visitation levels. The Google mobility report was thus assigned to indicate the visitation trends in social infrastructures based on the baseline for mobility changes (median value for the corresponding day of the week during 3 January–6 February 2020) [55].
- Infection rate: Taking into account variations in a country’s size and scale characteristics, disease transmission is interpreted through its propagation rate rather than using absolute case numbers. In epidemiology, rates are employed to quantify how frequent specific events occur within a designated population over a particular timeframe [56]. This method is admitted to address how the pandemic impacted social infrastructure demands. Consequently, the infection rate is determined by the number of daily new cases per million inhabitants [57].
- NPI stringency index: In order to track the effect of public health interventions on parks and open space visitations, this study employed the scoring system developed by the Oxford COVID-19 Pandemic Government Response Tracker (OxCGRT) from Oxford University in order to determine the stringency index of implemented public health measures amid the observed trends of increased and declined visitations. This index measures the intensity of ‘lockdown-type’ policies that mainly limit public behavior. It combines nineteen response indicators, such as school and workplace closures, as well as travel restrictions, into a composite measure. This stringency index is scaled from 0 to 100, where higher values represent more severe restrictions (with 100 being the most stringent) [58].
- Duration of behavioral change: This variable is essential in determining whether the period exhibiting a specific visitation trend holds an impact on the following trend in terms of visitation levels, i.e., whether prolonged visitation declines that are forced by implemented public health interventions might have provoked significant increased visitations towards parks and open spaces once the restrictions were eased. Therefore, durations of visitation increases and declines are demonstrated as , respectively.
- Visitation magnitude: The inclusion of this variable was to determine the visitation magnitude that is reached during both behavioral trends (increases and declines). Therefore, visitation magnitudes for visitation increases and declines are demonstrated as , respectively.
3.3. Data Quality and Limitations
- World Health Organization’s dashboard: This data source enables comprehensive cross-national analysis of COVID-19 patterns, providing standardized metrics for infection rates and temporal trends. However, significant data quality limitations exist as case detection, testing strategies, and reporting practices vary across jurisdictions. These variations, stemming from differences in healthcare systems, testing capacities, and case definitions among countries, affect data consistency. Additionally, true case counts may be under- or overestimated due to testing availability constraints, varying reporting protocols, and healthcare system capacity limitations during peak infection periods.
- Google Community Mobility Reports: These reports provide valuable high-frequency data on population movement patterns, enabling detailed analysis of behavioral changes during the pandemic. The data allow for comparative analysis across different location types and temporal patterns. However, the data represent only users with enabled Google location history on their devices, introducing potential selection bias. This limitation may underrepresent certain demographic groups, particularly those less likely to use smartphone technology or Google services.
- Oxford COVID-19 Government Response Tracker (OxCGRT): This tracker offers systematic and comparable data on policy responses across jurisdictions, enabling quantitative analysis of intervention strategies. The Oxford Stringency Index provides standardized metrics for cross-national comparison of policy measures. However, the index faces limitations in capturing implementation nuances. While it effectively records the presence and strictness of policies, it cannot account for actual enforcement levels, public compliance variations, or local policy adaptations.
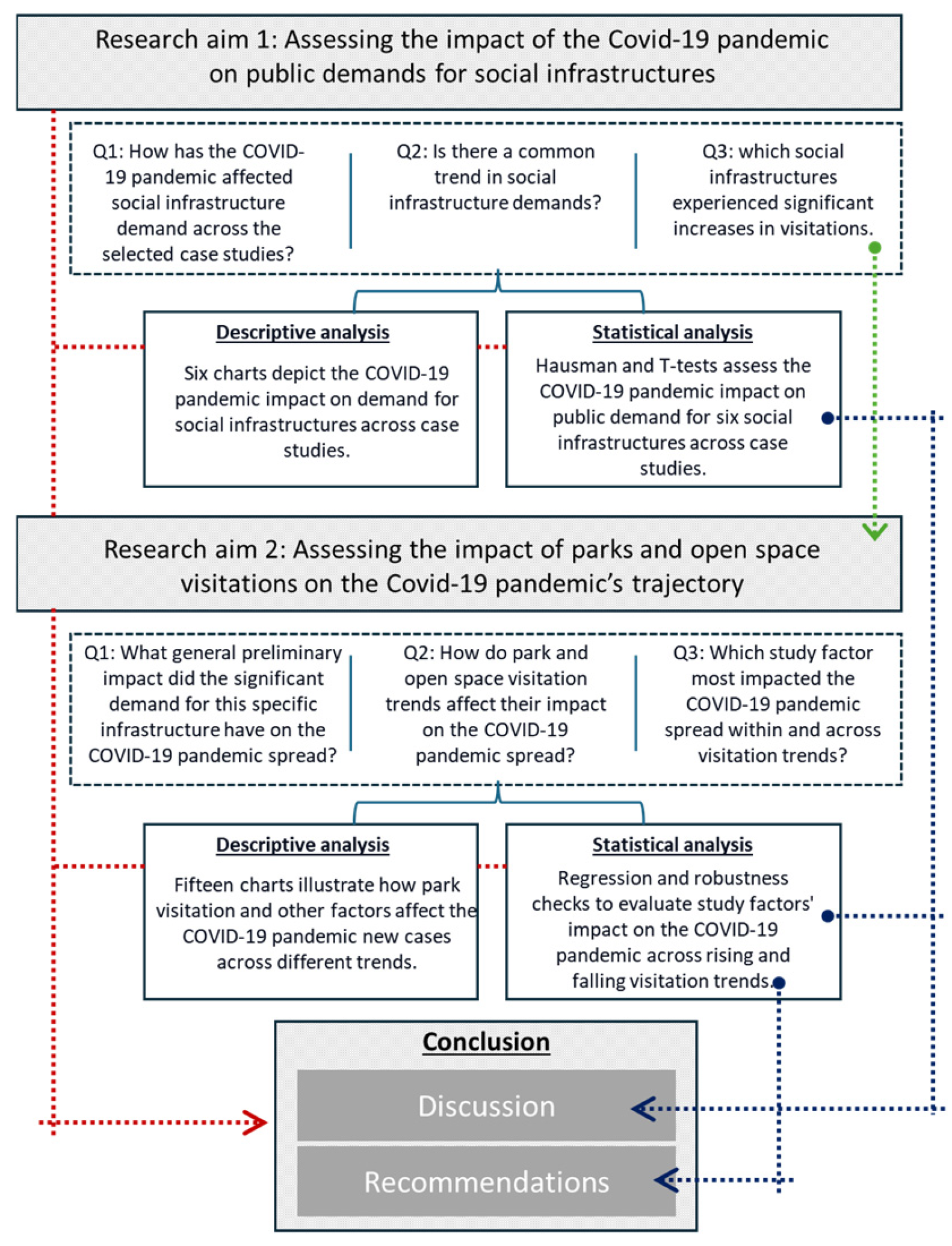
3.4. Methodology and Analytical Framework
- Hausman test: This test was applied to determine the most appropriate model (fixed or random effects) for analyzing the impact of the new COVID-19 pandemic cases on demands for various social infrastructures, with separate tests conducted for each infrastructure type. Fixed-effects models (used when p < 0.05) focused on how changes in the COVID-19 pandemic cases relate to changes in visitation within specific infrastructures over time, controlling for time-invariant characteristics. Random-effects models (used when p > 0.05) examined how differences in the COVID-19 pandemic cases relate to differences in visitation both within and between time periods, allowing for broader generalization across similar infrastructure types. This approach allows for tailored analysis of each infrastructure type, acknowledging potential variations in how daily the COVID-19 pandemic new cases affect visitation trends across different social infrastructures.
- t-test: This test was conducted to check for the significant effect of the new COVID-19 pandemic cases on the six social infrastructures studied.
- Regression analysis and robustness checks: A combination of multiple and linear regression analyses was performed to assess the impact of various study factors influencing the dramatic increase in visitations to parks and open spaces relative to the new COVID-19 pandemic cases, from the presented Equation (1). And to model the relationships between different visitation trend factors in order to identify underlying influential variables, utilizing Equation (2). Then, multiple tests were carried out to verify the reliability and validity of the regression results, ensuring that the conclusions are not sensitive to specific conditions or outliers.
- β0: Intercept (baseline level of new infections when all XXX factors are zero).
- β1, β2, β3, …: Coefficients representing the effect of each study factor on new infections.
- X: The chosen and most influential study factors.
- β0,i is the intercept for each specific factor’s effect during declines.
- β1,i is the coefficient indicating the impact of each study factor during increases on its corresponding factor during declines.
- FI represents the value of the study factor during the increased visitation trend.
- FD represents the value of the study factor during the declined visitation trend.
- ϵi is the error term capturing unobserved influences and random variation.
4. Data Collection and Analysis
4.1. The Impact of the COVID-19 Pandemic on Social Infrastructure Demands
4.1.1. The Impact of the COVID-19 Pandemic on Demand for Residential Places
4.1.2. The Impact of the COVID-19 Pandemic on Demand for Retail and Indoor Recreation Places
4.1.3. The Impact of the COVID-19 Pandemic on Demand for Groceries and Pharmacies
4.1.4. The Impact of the COVID-19 Pandemic on Demand for Transit Stations
4.1.5. The Impact of the COVID-19 Pandemic on Demand for Workplaces
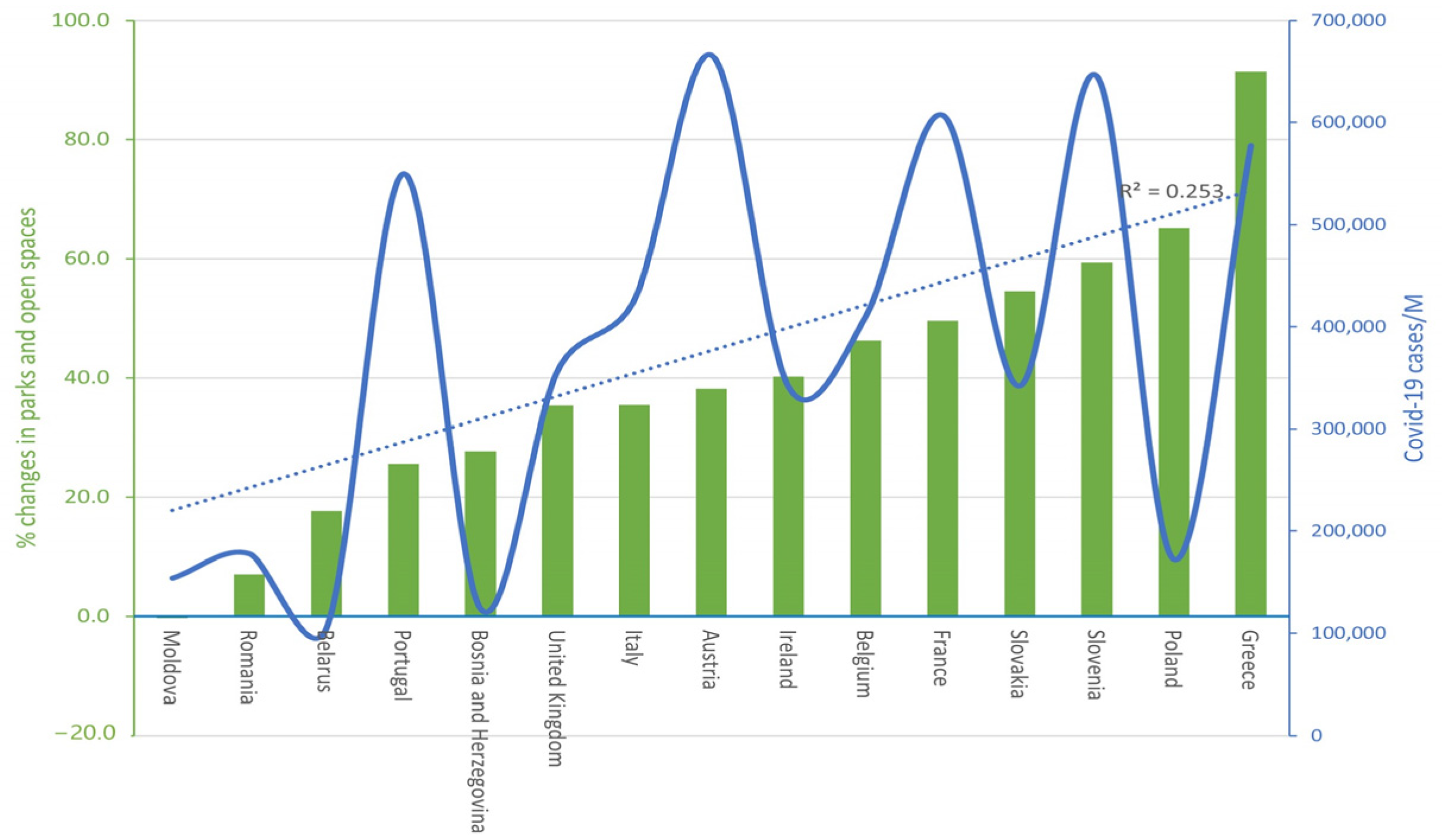
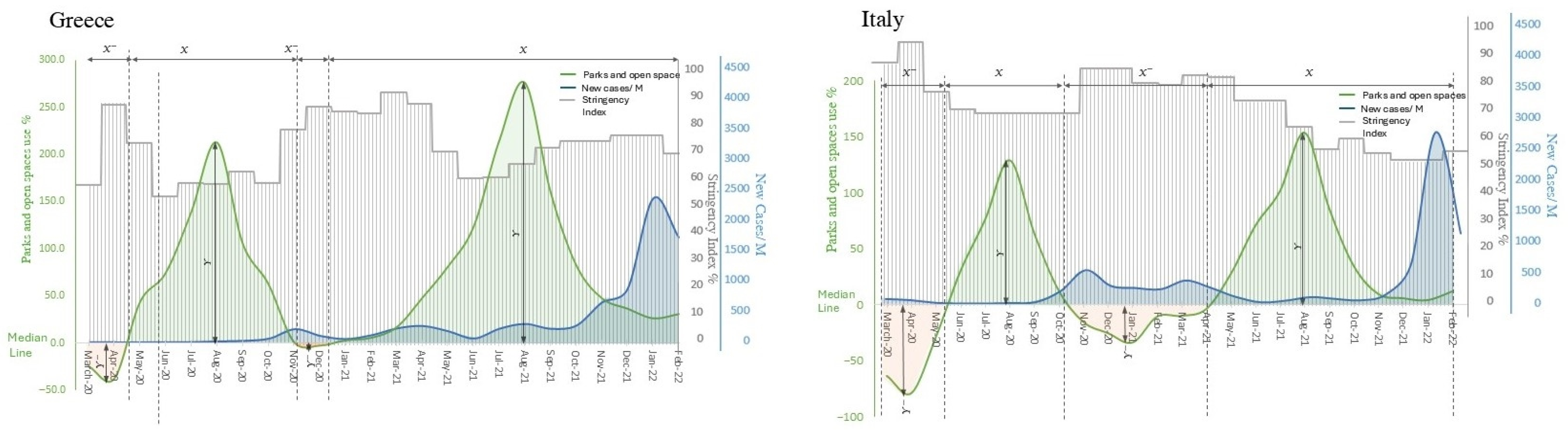
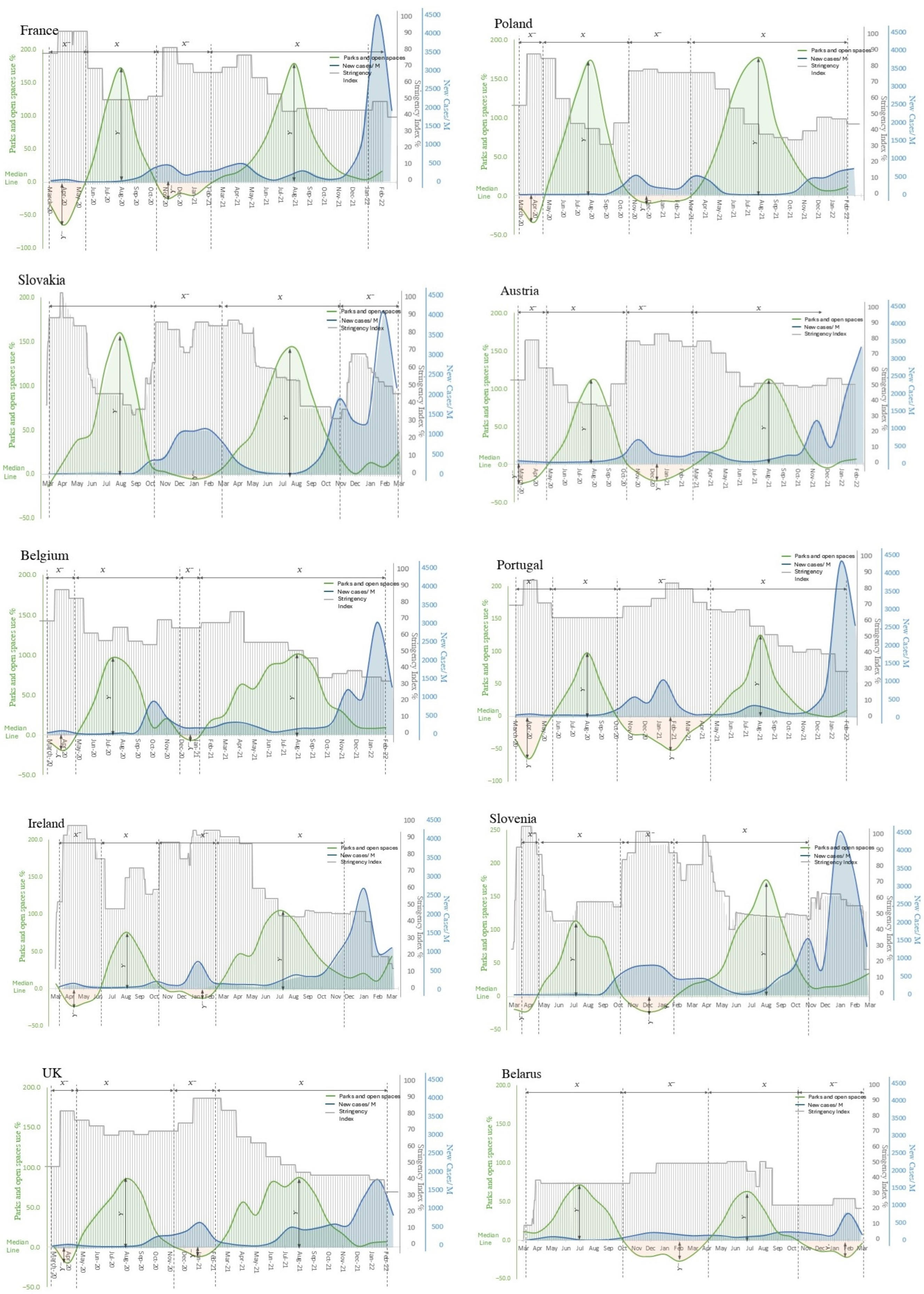
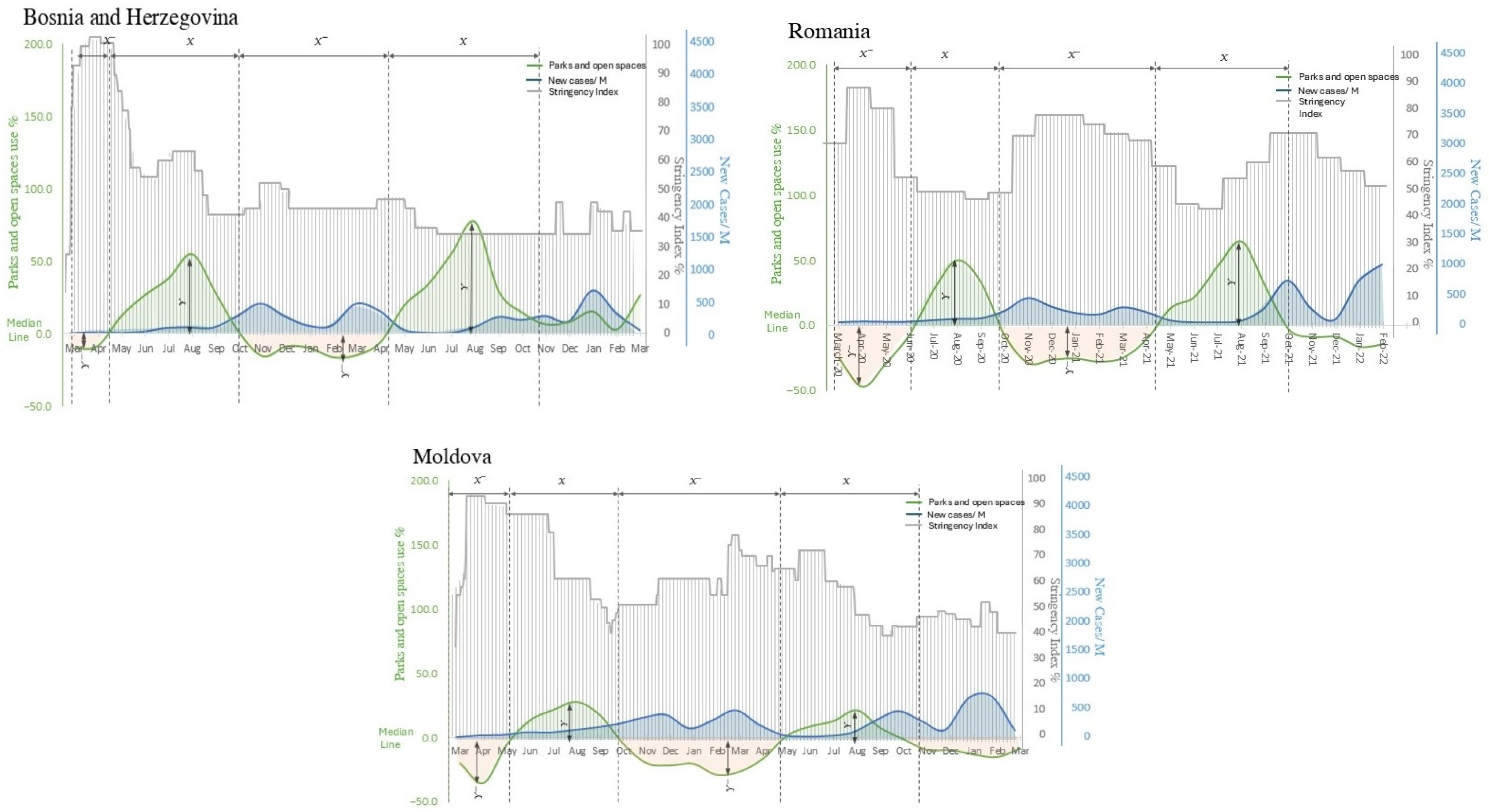
4.1.6. The Impact of the COVID-19 Pandemic on Demands for Parks and Open Spaces
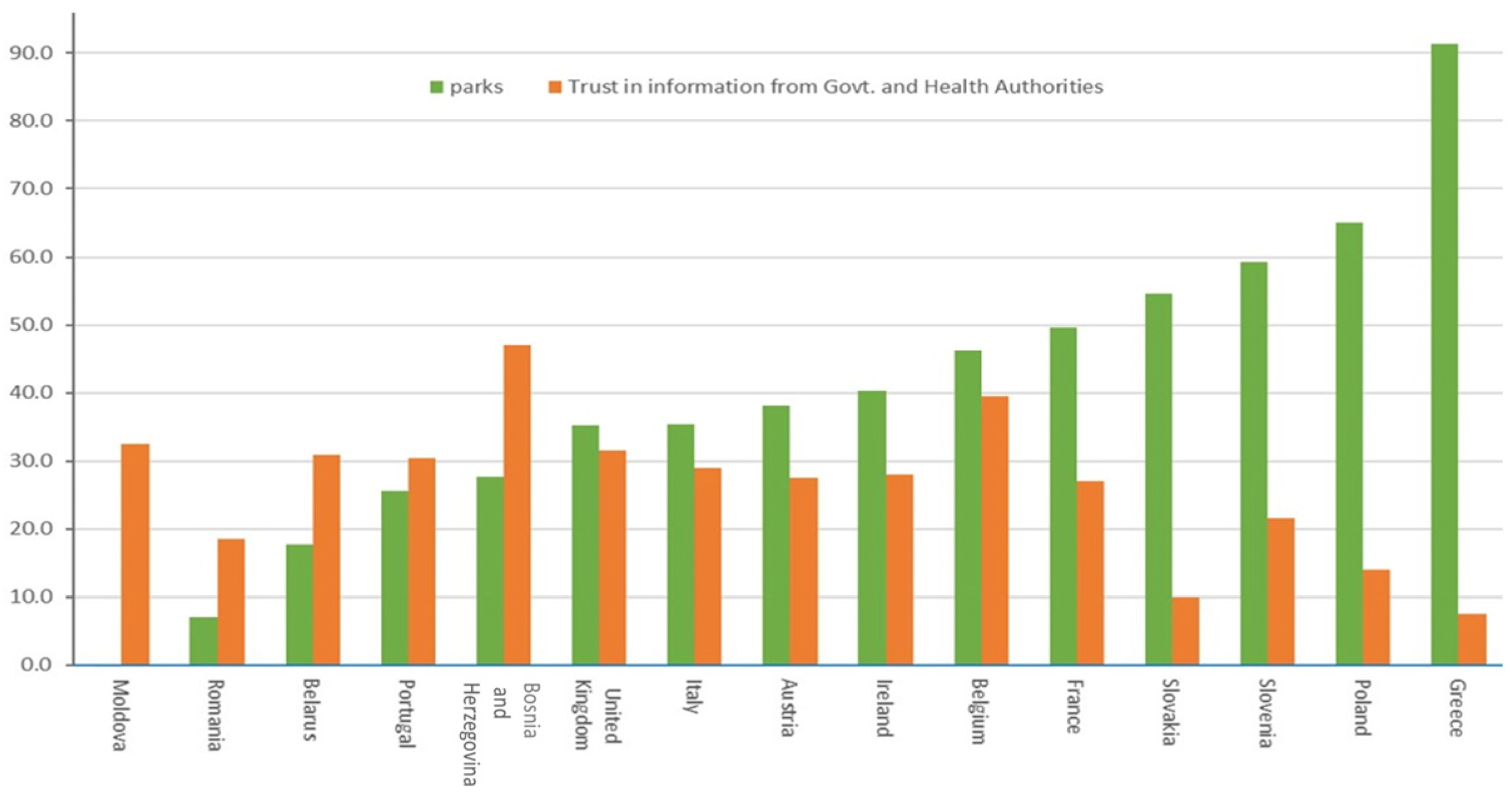
4.2. The Impact of Parks and Open Spaces on the COVID-19 Pandemic
Factors Affecting Park and Open Space Visitation During the COVID-19 Pandemic
5. Results
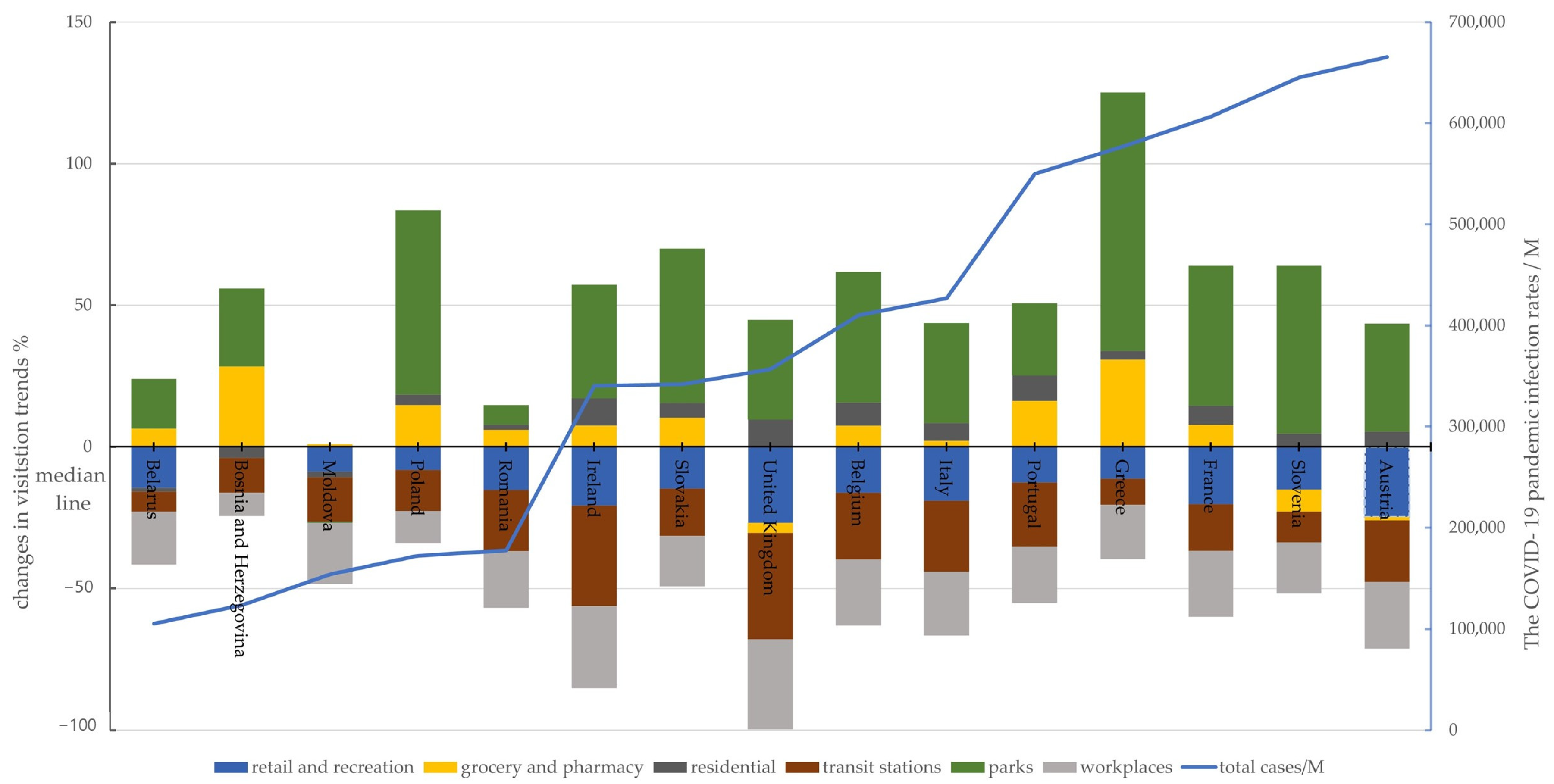
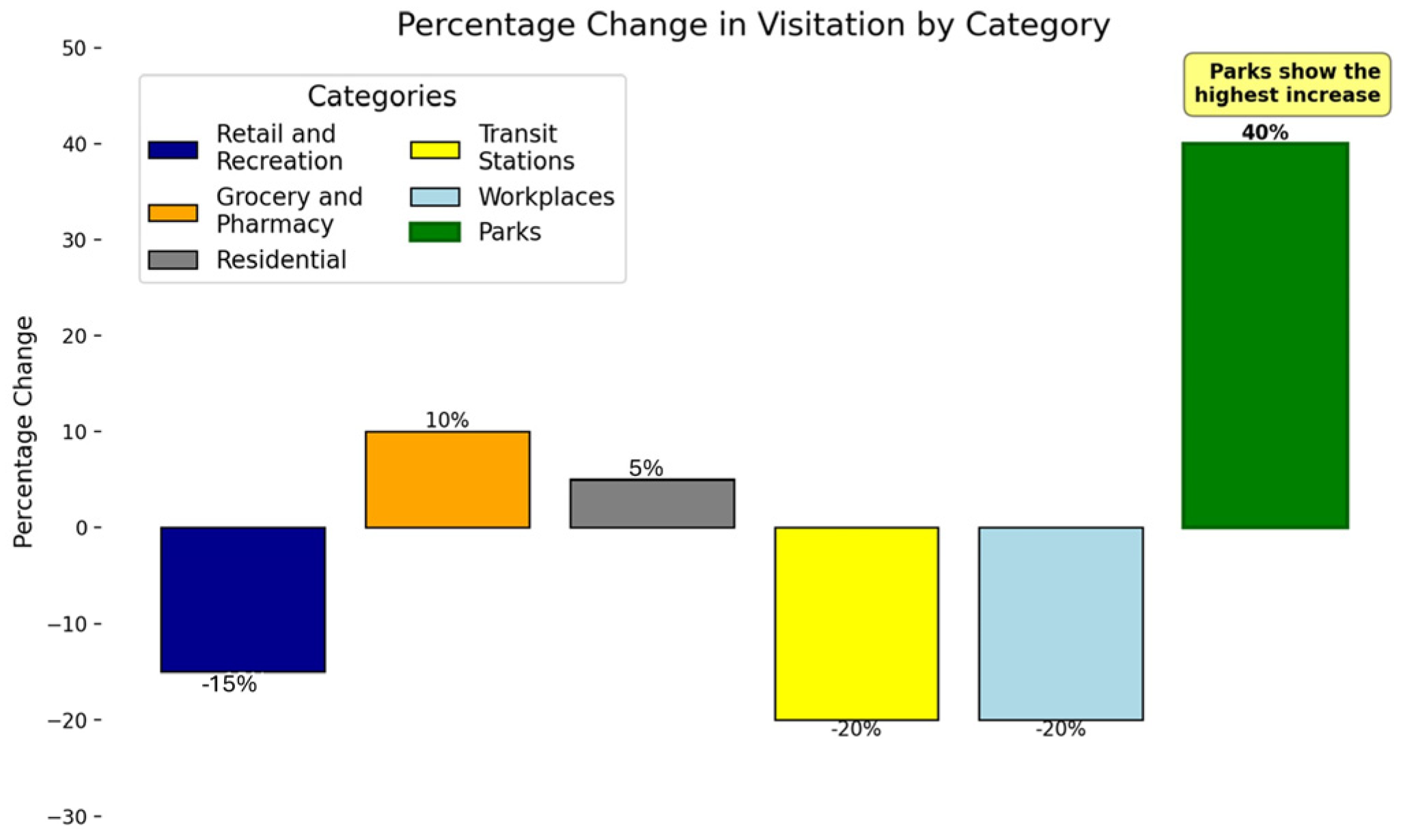
5.1. The Impact of the COVID-19 Pandemic on Behavioral Shifts Towards Social Infrastructures
- For the impact of the new COVID-19 pandemic cases on retail and recreation, the fixed effects panel data model was deemed appropriate. A significant negative effect was observed with a p-value of 0.00 (p < 0.05) and an estimated coefficient of B = −15.49.
- For the impact of the new COVID-19 pandemic cases on groceries and pharmacies, the random effects panel data model was deemed appropriate. A significant positive effect was observed with a p-value of 0.00 (p < 0.05) and an estimated coefficient of B = 7.42.
- For the impact of the new COVID-19 pandemic cases on residential areas, the fixed effects panel data model was deemed appropriate. A significant positive effect was observed with a p-value of 0.00 (p < 0.05) and an estimated coefficient of B = 4.16.
- For the impact of the new COVID-19 pandemic cases on transit stations, the fixed effects panel data model was deemed appropriate. A significant negative effect was observed with a p-value of 0.00 (p < 0.05) and an estimated coefficient of B = −19.73.
- For the impact of the new COVID-19 pandemic cases on workplaces, the fixed effects panel data model was deemed appropriate. A significant negative effect was observed with a p-value of 0.00 (p < 0.05) and an estimated coefficient of B = −20.94.
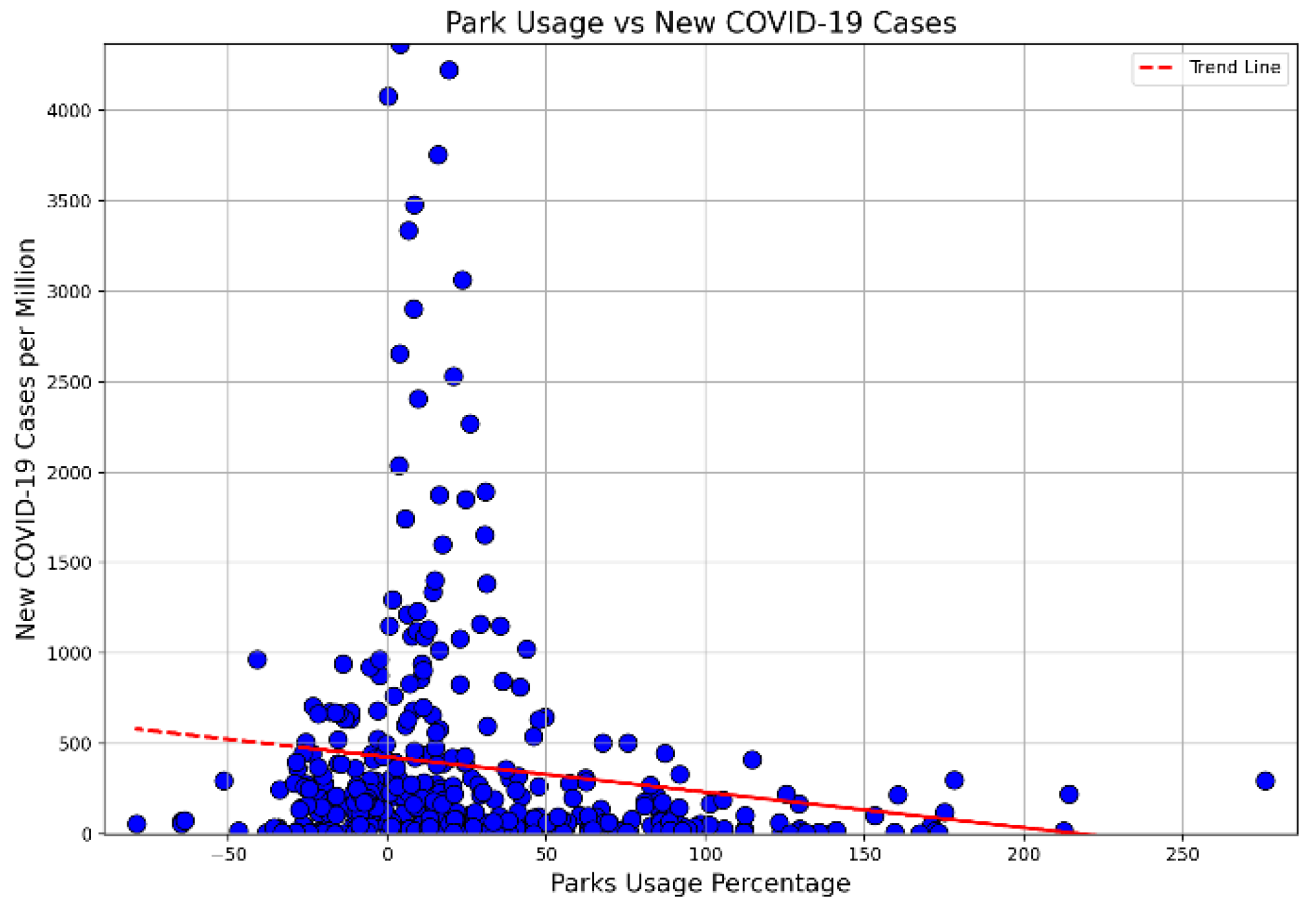
- For the impact of the new COVID-19 pandemic cases on parks, the fixed effects panel data model was deemed appropriate. A significant positive effect was observed with a p-value of 0.00 (p < 0.05) and an estimated coefficient of B = 41.17.
5.2. The Impact of Parks and Open Spaces on the COVID-19 Pandemic
5.2.1. ANOVA and Post Hoc Test
- The visitation magnitude factor showed a highly significant effect on the visitation trends, with an F-statistic of 171.0662 and a p-value of 0.0. This suggests that changes in visitation magnitudes were a key driver of the observed trends.
- Visitation duration was another significant factor, with an F-statistic of 29.5272 and a p-value of 0.0. This suggests that the length of time (in months) was an important differentiator between the groups, contributing to the trends observed.
- Public health stringency also showed a significant effect, with an F-statistic of 26.8124 and a p-value of 0.0. This indicates that the level of public health measures was a significant factor in differentiating the groups, impacting the trends.
- The factor of new infections per million was not statistically significant, with an F-statistic of 1.3991 and a p-value of 0.2417. This suggests that infection rates did not strongly differentiate between the groups and were not a key driver of the trends.
- Park and open space visitations with increasing trends showed significantly higher visitation magnitude values (MD = 143.15, p < 0.001), with an average of 143.15 percentage points higher than in the visitation decline trend. The tight confidence interval [121.24, 165.06] indicates that this is a very reliable difference.
- Park and open space visitations with increasing trends demonstrated significantly lower public health stringency measures (MD = −16.49, p < 0.001), with stringency levels 16.49 percentage points lower than in locations with declining visitation trends. The narrow confidence interval [−22.87, −10.12] confirms this inverse relationship was consistent.
- Park and open space visitations with increasing trends maintained significantly longer durations (MD = 4.23, p < 0.001), extending to 4.23 months longer than in declining visitation trends. The narrow confidence interval [2.67, 5.79] demonstrates that this is a reliable pattern.
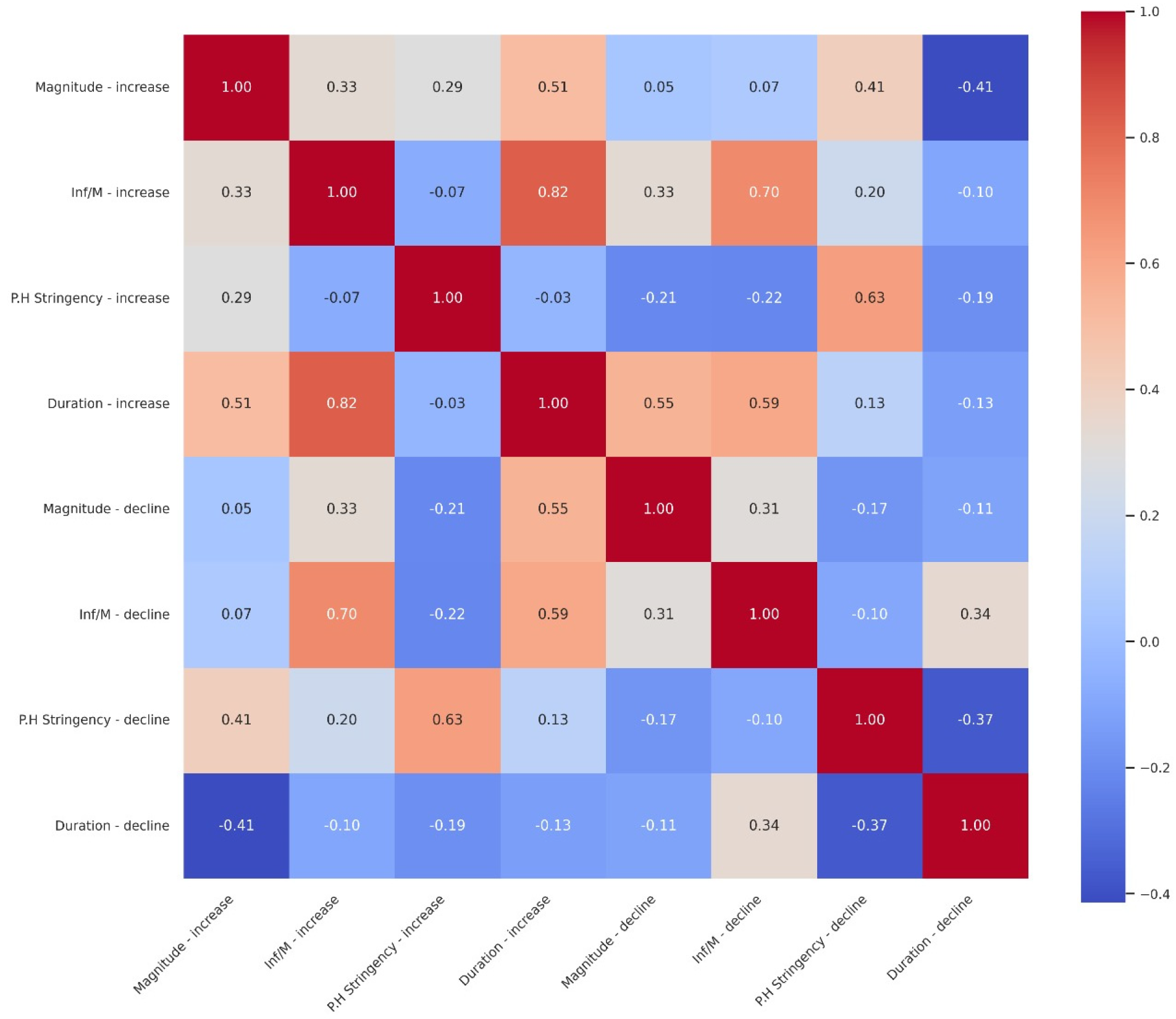
5.2.2. Correlation Analysis
- Infection rates during increased visitation periods strongly correlated with the duration (x) of the same visitation trend (r = 0.82), suggesting that longer visitation periods during increased visitation trends correlated with higher infection rates.
- Infection rates showed strong consistency between increase and decline periods (r = 0.70), indicating persistent infection patterns across both visitation trends.
- Public health measures maintained a strong correlation between increase and decline visitation trends (r = 0.63), reflecting consistent policy implementation.
- Visitation magnitude during increased visitation trends (y) moderately correlated with visitation duration (x) of the same trend (r = 0.51), showing that higher visitation magnitudes tended to last longer, also possibly reflecting that a longer period of increased visitations had an impact on increasing the total number of visits.
- Visitation duration during the increased trend (x) showed a moderate relationship with the visitation magnitude of the following declined trend (y−) (r = 0.55), suggesting that the longer the increased trend persisted, the lower the visitations that occurred in the opposing trend, likely due to the stringent implementation of public health measures.
- Visitation magnitude during the increased trend (y) showed moderate correlation with stringent public health measures implemented in the visitation decline trend (r = 0.41), likely indicating the counter effect of implementing stringent public health attempting to suppress visitation levels on the visitation flows once restrictions were eased.
- Visitation magnitude during increased visitation trends (y−) negatively correlated with visitation duration of the opposing trend (x−) (r = −0.41), indicating that shorter visitation decline periods triggered higher rebound levels of visitation surges when implemented restrictions were eased.
- The stringency of implemented public health measures during visitation decline trends negatively correlated with the corresponding visitation duration of the same trend (r = −0.37), suggesting that stricter measures may have shortened visitation decline phases.
5.2.3. Regression Analysis
- The independent variables (implemented public health measure, visitation duration, and visitation magnitude) managed to explain 69.2% of the variance in dependent variables (associated new infections/M).
- There was a significant effect of visitation duration when p-value < 0.05.
- There was no significant effect of visitation magnitudes when p-value > 0.05. This outcome could have been due to the nature of parks and open spaces, which typically have ample airflow that minimizes disease transmission, making the number of visitors less impactful. Additionally, the factor of parks and open space size was not considered.
- There was no significant effect of implemented public health measures when p-value > 0.05. This lack of significance could have been due to the study’s timeframe, which included both the pre- and post-vaccination periods.
- Jarque–Bera test (for normality of residuals): The JB statistic: 0.4013 with p-value: 0.8182. The high p-value (>0.05) indicates that the residuals were likely normally distributed.
- Breusch–Pagan test (for heteroscedasticity): The BP statistic: 5.2061 with p-value: 0.1573. The p-value was greater than 0.05, indicating that there was no strong evidence of heteroscedasticity in the model.
- The independent variables (implemented public health measure, visitation duration, and visitation magnitude) managed to explain 29% of the variance in the dependent variable (associated new infections/M).
- There was a significant effect of visitation duration when p-value < 0.05.
- There was a significant effect of visitation magnitude when p-value < 0.05.
- There was no significant effect of implemented public health measures when p-value > 0.05. This lack of significance could have been due to the study’s timeframe, which included both the pre- and post-vaccination periods.
- There was no significant effect for applied public health measures when p-value > 0.05.
- Jarque–Bera test (for Box–Cox normality of residuals): The high p-value (>0.05) indicated that the residuals were likely normally distributed.
- Breusch–Pagan test (for Box–Cox heteroscedasticity): The high p-value (>0.05) indicated that there was no strong evidence of heteroscedasticity in the model.
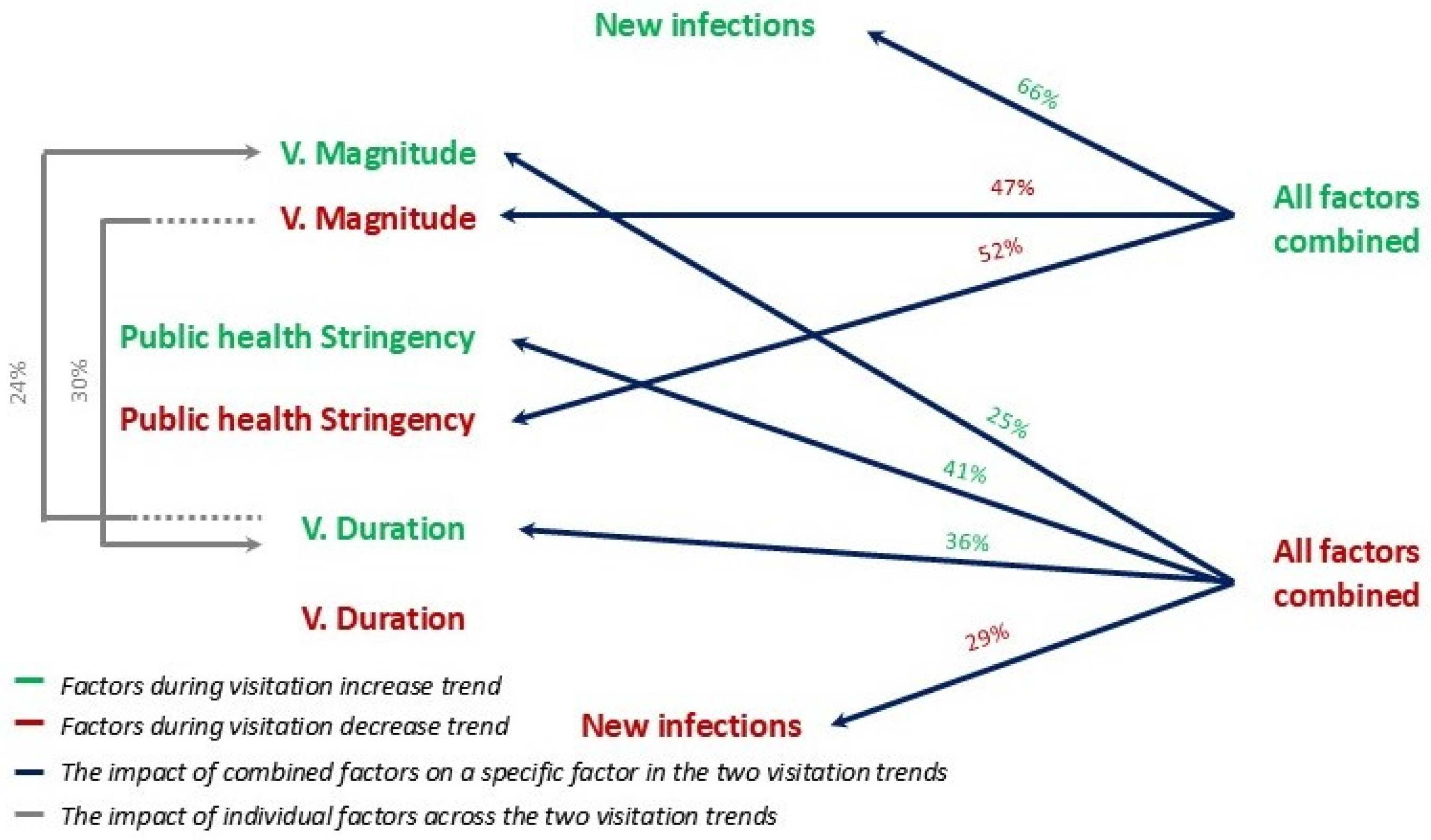
- Visitation magnitude during visitation decline trends (y−) positively explained 30.2% of the variance in visitation duration of the contrasting trend (x).
- Applied public health measures during visitation decline trends managed to explain 17% of the variance in visitation magnitude of the contrasting trend (x).
- The duration of visitations declines managed to also explain 17% of the variance in visitation magnitude of the contrasting trend (x).
- All study factors during visitation decline periods (except infection rates) managed to explain 25% of the variance in visitation magnitudes of the opposing visitation trend (y).
- All study factors during visitation decline periods (except infection rates) managed to explain 35.5% of the variance in visitation duration of the opposing visitation trend (x).
- All study factors during increased visitations (except infection rates) managed to explain 47% of the variance in visitation magnitudes of the opposing visitation trend (y−).
6. Discussion and Conclusions
6.1. Discussion
6.2. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Countries | Residential | Retail and Recreation | Grocery and Pharmacy | Transit Stations | Workplaces | Parks and Open Spaces | Total Cases/M |
|---|---|---|---|---|---|---|---|
| Austria | 5.4 | −24.8 | −1.2 | −21.7 | −23.6 | 38.1 | 665,539 |
| Slovenia | 4.7 | −15.2 | −7.7 | −10.9 | −17.8 | 59.3 | 645,148 |
| France | 6.6 | −20.3 | 7.8 | −16.5 | −23.3 | 49.6 | 606,726 |
| Greece | 3.0 | −11.3 | 30.8 | −9.2 | −19.2 | 91.4 | 576,922 |
| Portugal | 9.1 | −12.6 | 16.1 | −22.6 | −19.9 | 25.6 | 549,775 |
| Italy | 6.2 | −19.0 | 2.1 | −25.1 | −22.5 | 35.4 | 427,082 |
| Belgium | 8.1 | −16.3 | 7.5 | −23.5 | −23.3 | 46.2 | 410,241 |
| UK | 9.6 | −26.8 | −3.7 | −37.5 | −31.7 | 35.3 | 356,927 |
| Slovakia | 5.2 | −14.7 | 10.2 | −16.8 | −17.7 | 54.6 | 341,743 |
| Ireland | 9.7 | −20.7 | 7.5 | −35.6 | −28.9 | 40.2 | 340,411 |
| Romania | 1.7 | −15.2 | 6.0 | −21.6 | −19.9 | 7.0 | 177,649 |
| Poland | 3.8 | −8.2 | 14.7 | −14.5 | −11.4 | 65.1 | 172,131 |
| Moldova | −2.0 | −8.7 | 0.9 | −15.7 | −21.6 | −0.4 | 153,952 |
| Bosnia and Herzegovina | −3.9 | 0.1 | 28.2 | −12.4 | −8.2 | 27.7 | 123,742 |
| Belarus | −1.4 | −14.5 | 6.3 | −7.1 | −18.5 | 17.6 | 105,381 |
| Country | Outdoor Visitation Increase Trend | Outdoor Visitation Decline Trend | ||||||
|---|---|---|---|---|---|---|---|---|
| Magnitude % | New Inf. /M | Public Health Stringency % | Duration (M) | Magnitude % | New Inf. /M | Public Health Stringency % | Duration (M) | |
| Greece | 212.6 | 46.7 | 61.1 | 7.0 | −38.0 | 4.7 | 75.5 | 2.0 |
| 276.0 | 521.4 | 72.1 | 14.0 | −3.0 | 104.3 | 83.5 | 1.0 | |
| Austria | 112.2 | 52.1 | 46.0 | 6.0 | −26.0 | 34.7 | 74.1 | 2.0 |
| 112.5 | 721.9 | 57.8 | 12.0 | −21.6 | 349.7 | 72.7 | 4.0 | |
| France | 170.8 | 117.1 | 52.0 | 5.0 | −64.8 | 37.9 | 81.0 | 3.0 |
| 178.2 | 782.9 | 49.3 | 12.0 | −23.6 | 300.5 | 68.3 | 4.0 | |
| Slovenia | 111.9 | 83.6 | 49.9 | 6.0 | −20.7 | 13.4 | 74.6 | 2.0 |
| 175.0 | 881.2 | 51.1 | 13.0 | −23.4 | 677.4 | 81.8 | 3.0 | |
| Portugal | 98.1 | 68.9 | 61.1 | 5.0 | −64.7 | 38.0 | 73.7 | 3.0 |
| 125.4 | 823.9 | 48.7 | 10.0 | −51.4 | 371.6 | 72.6 | 6.0 | |
| Belgium | 92.9 | 211.5 | 59.2 | 7.0 | −19.0 | 75.6 | 72.8 | 2.0 |
| 101.3 | 620.9 | 46.5 | 13.0 | −5.3 | 183.8 | 60.4 | 2.0 | |
| Slovakia | 159.4 | 88.1 | 53.4 | 8.0 | −14.0 | 2.9 | 68.1 | 1.0 |
| 141.0 | 762.7 | 48.7 | 12.0 | −5.4 | 921.6 | 68.2 | 3.0 | |
| Ireland | 76.0 | 58.2 | 57.5 | 4.0 | −21.6 | 43.9 | 74.6 | 4.0 |
| 105.3 | 597.8 | 48.4 | 12.0 | −11.5 | 258.4 | 82.6 | 4.0 | |
| Italy | 128.6 | 49.0 | 67.0 | 5.0 | −78.9 | 48.6 | 82.7 | 3.0 |
| 153.1 | 158.1 | 75.1 | 11.0 | −33.9 | 312.2 | 78.9 | 7.0 | |
| UK | 85.8 | 100.9 | 68.6 | 7.0 | −19.4 | 47.1 | 63.4 | 2.0 |
| 87.2 | 567.3 | 49.4 | 12.0 | −11.7 | 411.8 | 82.2 | 3.0 | |
| Romania | 50.1 | 55.8 | 48.0 | 3.0 | −46.7 | 11.7 | 71.8 | 4.0 |
| 64.4 | 60.1 | 51.6 | 5.0 | −28.6 | 366.9 | 65.4 | 12.0 | |
| Belarus | 72.1 | 42.2 | 28.1 | 8.0 | −27.0 | 150.5 | 41.0 | 7.0 |
| 63.0 | 137.6 | 33.7 | 6.0 | −21.7 | 287.8 | 20.9 | 4.0 | |
| Bosnia | 54.6 | 80.9 | 54.9 | 6.0 | −10.2 | 9.8 | 78.3 | 2.0 |
| 76.7 | 176.3 | 37.3 | 10.0 | −16.2 | 252.1 | 44.3 | 6.0 | |
| Moldova | 27.7 | 112.4 | 63.3 | 4.0 | −35.6 | 28.0 | 77.9 | 3.0 |
| 21.1 | 87.7 | 54.6 | 5.0 | −29.3 | 342.6 | 50.9 | 12.0 | |
| Poland | 172.0 | 47.3 | 49.2 | 6.0 | −33.1 | 5.7 | 69.0 | 2.0 |
| 173.3 | 254.8 | 46.3 | 11.0 | −9.6 | 323.8 | 73.3 | 5.0 | |
References
- Venter, Z.S.; Barton, D.N.; Gundersen, V.; Figari, H.; Nowell, M.S. Back to nature: Norwegians sustain increased recreational use of urban green space months after the COVID-19 outbreak. Landsc. Urban Plan. 2021, 214, 104175. [Google Scholar] [CrossRef]
- Lu, Y.; Zhao, J.; Wu, X.; Lo, S.M. Escaping to nature during a pandemic: A natural experiment in Asian cities during the COVID-19 pandemic with big social media data. Sci. Total Environ. 2021, 777, 146092. [Google Scholar] [CrossRef]
- Beery, T.; Olsson, M.R.; Vitestam, M. COVİD-19 and outdoor recreation management: Increased participation, connection to nature, and a look to climate adaptation. J. Outdoor Recreat. Tour. 2021, 36, 100457. [Google Scholar] [CrossRef] [PubMed]
- Bulfone, T.C.; Malekinejad, M.; Rutherford, G.W.; Razani, N. Outdoor Transmission of SARS-CoV-2 and Other Respiratory Viruses: A Systematic Review. J. Infect. Dis. 2021, 223, 550–561. [Google Scholar] [CrossRef] [PubMed]
- Okech, E.A.; Nyadera, I.N. Urban green spaces in the wake of COVID-19 pandemic: Reflections from Nairobi, Kenya. GeoJournal 2022, 87, 4931–4945. [Google Scholar] [CrossRef]
- da Schio, N.; Phillips, A.; Fransen, K.; Wolff, M.; Haase, D.; Ostoić, S.K.; Živojinović, I.; Vuletić, D.; Derks, J.; Davies, C.; et al. The impact of the COVID-19 pandemic on the use of and attitudes towards urban forests and green spaces: Exploring the instigators of change in Belgium. Urban For. Urban Green. 2021, 65, 127305. [Google Scholar] [CrossRef]
- Berdejo-Espinola, V.; Suárez-Castro, A.F.; Amano, T.; Fielding, K.S.; Oh, R.R.Y.; Fuller, R.A. Urban green space use during a time of stress: A case study during the COVID-19 pandemic in Brisbane, Australia. People Nat. 2021, 3, 597–609. [Google Scholar] [CrossRef]
- Fagerholm, N.; Eilola, S.; Arki, V. Outdoor recreation and nature’s contribution to well-being in a pandemic situation—Case Turku, Finland. Urban For. Urban Green. 2021, 64, 127257. [Google Scholar] [CrossRef]
- Burnett, H.; Olsen, J.R.; Nicholls, N.; Mitchell, R. Change in time spent visiting and experiences of green space following restrictions on movement during the COVID-19 pandemic: A nationally representative cross-sectional study of UK adults. BMJ Open 2021, 11, e044067. [Google Scholar] [CrossRef]
- Venter, Z.S.; Barton, D.N.; Gundersen, V.; Figari, H.; Nowell, M. Urban nature in a time of crisis: Recreational use of green space increases during the COVID-19 outbreak in Oslo, Norway. Environ. Res. Lett. 2020, 15, 104075. [Google Scholar] [CrossRef]
- AbouKorin, S.A.A.; Han, H.; Mahran, M.G.N. Role of urban planning characteristics in forming pandemic resilient cities—Case study of COVID-19 impacts on European cities within England, Germany and Italy. Cities 2021, 118, 103324. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.E.; Mahmud, A.S.; Miller, I.F.; Rajeev, M.; Rasambainarivo, F.; Rice, B.L.; Takahashi, S.; Tatem, A.J.; Wagner, C.E.; Wang, L.-F.; et al. Infectious disease in an era of global change. Nat. Rev. Microbiol. 2021, 20, 193–205. [Google Scholar] [CrossRef] [PubMed]
- Grubaugh, N.D.; Ladner, J.T.; Lemey, P.; Pybus, O.G.; Rambaut, A.; Holmes, E.C.; Andersen, K.G. Tracking virus outbreaks in the twenty-first century. Nat. Microbiol. 2018, 4, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Piret, J.; Boivin, G. Pandemics Throughout History. Front. Microbiol. 2021, 11, 631736. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wang, T. Urban resilience under the COVID-19 pandemic: A quantitative assessment framework based on system dynamics. Cities 2023, 136, 104265. [Google Scholar] [CrossRef]
- Zhen, Q.; Zhang, A.; Huang, Q.; Li, J.; Du, Y.; Zhang, Q. Overview of the Role of Spatial Factors in Indoor SARS-CoV-2 Transmission: A Space-Based Framework for Assessing the Multi-Route Infection Risk. Int. J. Environ. Res. Public Health 2022, 19, 11007. [Google Scholar] [CrossRef]
- Oakman, J.; Lambert, K.A.; Weale, V.P.; Stuckey, R.; Graham, M. Employees Working from Home: Do Leadership Factors Influence Work-Related Stress and Musculoskeletal Pain? Int. J. Environ. Res. Public Health 2023, 20, 3046. [Google Scholar] [CrossRef]
- Pierce, M.; Hope, H.; Ford, T.; Hatch, S.; Hotopf, M.; John, A.; Kontopantelis, E.; Webb, R.; Wessely, S.; McManus, S.; et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020, 7, 883–892. [Google Scholar] [CrossRef]
- Xu, T.; Shao, M.; Liu, R.; Wu, X.; Zheng, K. Risk Perception, Perceived Government Coping Validity, and Individual Response in the Early Stage of the COVID-19 Pandemic in China. Int. J. Environ. Res. Public Health 2023, 20, 1982. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Lippi, G.; Henry, B.M.; Sanchis-Gomar, F. Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID-19). Eur. J. Prev. Cardiol. 2020, 27, 906–908. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Xu, R.; Schwartz, M.; Ghosh, D.; Chen, X. COVID-19 and Retail Grocery Management: Insights from a Broad-Based Consumer Survey. IEEE Eng. Manag. Rev. 2020, 48, 202–211. [Google Scholar] [CrossRef]
- Rosemberg, M.A.S.; Adams, M.; Polick, C.; Li, W.V.; Dang, J.; Tsai, J.H.C. COVID-19 and mental health of food retail, food service, and hospitality workers. J. Occup. Environ. Hyg. 2021, 18, 169–179. [Google Scholar] [CrossRef] [PubMed]
- Kwok, K.O.; Li, K.K.; Chan, H.H.H.; Yi, Y.Y.; Tang, A.; Wei, W.I.; Wong, S.Y.S. Community Responses during Early Phase of COVID-19 Epidemic, Hong Kong. Emerg. Infect. Dis. 2020, 26, 1575–1579. [Google Scholar] [CrossRef] [PubMed]
- Conrow, L.; Campbell, M.; Kingham, S. Transport changes and COVID-19: From present impacts to future possibilities. N. Z. Geogr. 2021, 77, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Hu, S.; Chen, P. Who left riding transit? Examining socioeconomic disparities in the impact of COVID-19 on ridership. Transp. Res. Part D Transp. Environ. 2021, 90, 102654. [Google Scholar] [CrossRef]
- Jiang, S.; Cai, C. Unraveling the dynamic impacts of COVID-19 on metro ridership: An empirical analysis of Beijing and Shanghai, China. Transp. Policy 2022, 127, 158–170. [Google Scholar] [CrossRef]
- Donkin, R. The Future of Work; Springer: Berlin/Heidelberg, Germany, 2009; pp. 1–272. [Google Scholar] [CrossRef]
- Florida, R.; Rodríguez-Pose, A.; Storper, M. Cities in a post-COVID world. Urban Stud. 2021, 60, 1509–1531. [Google Scholar] [CrossRef]
- Barath, M.; Schmidt, D.A. Offices after the COVID-19 Pandemic and Changes in Perception of Flexible Office Space. Sustainability 2022, 14, 11158. [Google Scholar] [CrossRef]
- Kassem, M.A.; Radzi, A.R.; Pradeep, A.; Algahtany, M.; Rahman, R.A. Impacts and Response Strategies of the COVID-19 Pandemic on the Construction Industry Using Structural Equation Modeling. Sustainability 2023, 15, 2672. [Google Scholar] [CrossRef]
- Ikegami, K.; Ando, H.; Mafune, K.; Tsuji, M.; Tateishi, S.; Odagami, K.; Muramatsu, K.; Fujino, Y.; Ogami, A. Job stress and work from home during the COVID-19 pandemic among Japanese workers: A prospective cohort study. Health Psychol. Behav. Med. 2023, 11, 2163248. [Google Scholar] [CrossRef] [PubMed]
- Qosaj, F.A.; Weine, S.M.; Sejdiu, P.; Hasani, F.; Statovci, S.; Behluli, V.; Arenliu, A. Prevalence of Perceived Stress, Anxiety, and Depression in HCW in Kosovo during the COVID-19 Pandemic: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2022, 19, 16667. [Google Scholar] [CrossRef] [PubMed]
- Sikos, T.T.; Molnár, D.; Kovács, A. The impact of COVID-19 pandemic on the retail sector: Policy-strategy-innovation. Észak-Mo. Stratég. Füzetek 2022, 19, 76–85. [Google Scholar] [CrossRef]
- AbouKorin, S.A.A.; Han, H.; Mahran, M.G.N. Pandemic resilience planning: NPI measures and COVID-19 impacts in UK, Germany, and Italy. Cities 2023, 143, 104621. [Google Scholar] [CrossRef]
- Harris, P.; Harris-Roxas, B.; Prior, J.; Morrison, N.; McIntyre, E.; Frawley, J.; Adams, J.; Bevan, W.; Haigh, F.; Freeman, E.; et al. Respiratory pandemics, urban planning and design: A multidisciplinary rapid review of the literature. Cities 2022, 127, 103767. [Google Scholar] [CrossRef]
- CMS. Nursing Home Visitation—COVID-19 (REVISED). 8 May 2023. Available online: https://www.cms.gov/medicare/provider-enrollment-and-certification/surveycertificationgeninfo/policy-and-memos-states/nursing-home-visitation-covid-19-revised (accessed on 23 August 2024).
- Alba, C.; Pan, B.; Yin, J.; Rice, W.L.; Mitra, P.; Lin, M.S.; Liang, Y. COVID-19’s impact on visitation behavior to US national parks from communities of color: Evidence from mobile phone data. Sci. Rep. 2022, 12, 13398. [Google Scholar] [CrossRef]
- Pan, J.; Bardhan, R.; Jin, Y. Spatial distributive effects of public green space and COVID-19 infection in London. Urban For. Urban Green. 2021, 62, 127182. [Google Scholar] [CrossRef]
- Lee, K.O.; Mai, K.M.; Park, S. Green space accessibility helps buffer declined mental health during the COVID-19 pandemic: Evidence from big data in the United Kingdom. Nat. Ment. Health 2023, 1, 124–134. [Google Scholar] [CrossRef]
- Geng, D.C.; Innes, J.; Wu, W.; Wang, G. Impacts of COVID-19 pandemic on urban park visitation: A global analysis. J. For. Res. 2021, 32, 553–567. [Google Scholar] [CrossRef]
- Wang, J.; Wu, X.; Wang, R.; He, D.; Li, D.; Yang, L.; Yang, Y.; Lu, Y. Review of Associations between Built Environment Characteristics and Severe Acute Respiratory Syndrome Coronavirus 2 Infection Risk. Int. J. Environ. Res. Public Health 2021, 18, 7561. [Google Scholar] [CrossRef]
- Rice, W.L.; Pan, B. Understanding changes in park visitation during the COVID-19 pandemic: A spatial application of big data. Wellbeing Space Soc. 2021, 2, 100037. [Google Scholar] [CrossRef] [PubMed]
- Stock, S.; Bu, F.; Fancourt, D.; Mak, H.W. Longitudinal associations between going outdoors and mental health and wellbeing during a COVID-19 lockdown in the UK. Sci. Rep. 2022, 12, 10580. [Google Scholar] [CrossRef] [PubMed]
- Slater, S.J.; Christiana, R.W.; Gustat, J. Recommendations for Keeping Parks and Green Space Accessible for Mental and Physical Health During COVID-19 and Other Pandemics. Prev. Chronic Dis. 2020, 17, E59. [Google Scholar] [CrossRef] [PubMed]
- Csomós, G.; Borza, E.M.; Farkas, J.Z. Exploring park visitation trends during the COVID-19 pandemic in Hungary by using mobile device location data. Sci. Rep. 2023, 13, 11078. [Google Scholar] [CrossRef] [PubMed]
- Godfrey, D. No COVID-19-Related Park Closures Expected in Burnaby—Burnaby Now. 2020. Available online: https://www.burnabynow.com/local-news/no-covid-19-related-park-closures-expected-in-burnaby-3119960 (accessed on 8 November 2023).
- Rose, A. National Park Visitors Surge as COVID-19 Pandemic Restrictions Wane|CNN. CNN. 2021. Available online: https://www.cnn.com/travel/article/national-park-visitors-surge/index.html (accessed on 8 November 2023).
- Pouso, S.; Borja, Á.; Fleming, L.E.; Gómez-Baggethun, E.; White, M.P.; Uyarra, M.C. Contact with blue-green spaces during the COVID-19 pandemic lockdown beneficial for mental health. Sci. Total Environ. 2021, 756, 143984. [Google Scholar] [CrossRef]
- Alizadehtazi, B.; Tangtrakul, K.; Woerdeman, S.; Gussenhoven, A.; Mostafavi, N.; Montalto, F.A. Urban Park Usage During the COVID-19 Pandemic. J. Extrem. Events 2020, 7, 2150008. [Google Scholar] [CrossRef]
- Johnson, T.F.; Hordley, L.A.; Greenwell, M.P.; Evans, L.C. Associations between COVID-19 transmission rates, park use, and landscape structure. Sci. Total Environ. 2021, 789, 148123. [Google Scholar] [CrossRef]
- Spano, G.; D’este, M.; Giannico, V.; Elia, M.; Cassibba, R.; Lafortezza, R.; Sanesi, G. Association between indoor-outdoor green features and psychological health during the COVID-19 lockdown in Italy: A cross-sectional nationwide study. Urban For. Urban Green. 2021, 62, 127156. [Google Scholar] [CrossRef]
- Kinzig, A.P.; Ehrlich, P.R.; Alston, L.J.; Arrow, K.; Barrett, S.; Buchman, T.G.; Daily, G.C.; Levin, B.; Levin, S.; Oppenheimer, M.; et al. Social Norms and Global Environmental Challenges: The Complex Interaction of Behaviors, Values, and Policy. Bioscience 2013, 63, 164–175. [Google Scholar] [CrossRef]
- Casari, M.; Tagliapietra, C. Group size in social-ecological systems. Proc. Natl. Acad. Sci. USA 2018, 115, 2728–2733. [Google Scholar] [CrossRef]
- COVID-19 Community Mobility Reports. Available online: https://www.google.com/covid19/mobility/ (accessed on 15 September 2024).
- Center for Disease Control and Prevention (CDC). Principles of Epidemiology in Public Health Practice; CDC: Atlanta, Georgia, 2006. [Google Scholar]
- Mathieu, E.; Ritchie, H.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Hasell, J.; Macdonald, B.; Dattani, S.; Beltekian, D.; Ortiz-Ospina, E.; et al. Coronavirus Pandemic (COVID-19). Our World in Data. 8 March 2020. Available online: https://ourworldindata.org/coronavirus (accessed on 23 August 2024).
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef] [PubMed]
- Real Estate News—KPMG Slovakia. Available online: https://kpmg.com/sk/en/home/industries/real-estate.html (accessed on 26 April 2023).
- UN-Habitat’s COVID-19 Response Plan|UN-Habitat. Available online: https://unhabitat.org/un-habitat-covid-19-response-plan (accessed on 26 April 2023).
- Arafat, S.M.Y.; Kar, S.K.; Marthoenis, M.; Sharma, P.; Apu, E.H.; Kabir, R. Psychological underpinning of panic buying during pandemic (COVID-19). Psychiatry Res. 2020, 289, 113061. [Google Scholar] [CrossRef] [PubMed]
- McKinsey. European Consumer Pessimism Intensifies in the Face of Rising Prices|McKinsey. Available online: https://www.mckinsey.com/capabilities/growth-marketing-and-sales/our-insights/survey-european-consumer-sentiment-during-the-coronavirus-crisis (accessed on 7 May 2023).
- Ahrendt, D.; Cabrita, J.; Clerici, E.; Hurley, J.; Leončikas, T.; Mascherini, M.; Riso, S.; Sándor, E. Living, Working and COVID-19; Eurofound: Dublin, Ireland, 2020; p. 66. [Google Scholar]
- Huynh, N.N.Y.; Nguyen, D.D.; Ta, N.H.; Nguyen, M.T.; Van Nguyen, T.; Dang, H.T.; Vo, T.K.C.; Le, N.T. COVID-19 Clusters at Workplaces and its Transmission into Communities in Vietnam: A Novel Emerging Occupational Risk Factor at Work Due to Coronavirus Infection. Asian Pacific J. Environ. Cancer 2020, 3, 27–33. [Google Scholar] [CrossRef]
- Telework in the EU Before and After the COVID-19: Where We Were, Where We Head to. Available online: https://joint-research-centre.ec.europa.eu/document/download/1ccf7717-ab52-4215-b14a-08d74e9d44fc_en (accessed on 29 April 2023).
- The Future of the Office Has Arrived: It’s Hybrid. Available online: https://www.gallup.com/workplace/511994/future-office-arrived-hybrid.aspx (accessed on 13 September 2024).
- COVID Behaviors Dashboard—Johns Hopkins Center for Communication Programs. Available online: https://ccp.jhu.edu/kap-covid/ (accessed on 23 May 2023).
- Nanath, K.; Balasubramanian, S.; Shukla, V.; Islam, N.; Kaitheri, S. Developing a mental health index using a machine learning approach: Assessing the impact of mobility and lockdown during the COVID-19 pandemic. Technol. Forecast. Soc. Chang. 2022, 178, 121560. [Google Scholar] [CrossRef] [PubMed]
- Larson, L.R.; Zhang, Z.; Oh, J.I.; Beam, W.; Ogletree, S.S.; Bocarro, J.N.; Lee, K.J.; Casper, J.; Stevenson, K.T.; Hipp, J.A.; et al. Urban Park Use During the COVID-19 Pandemic: Are Socially Vulnerable Communities Disproportionately Impacted? Front. Sustain. Cities 2021, 3, 710243. [Google Scholar] [CrossRef]
- Niță, M.R.; Arsene, M.; Barbu, G.; Cus, A.G.; Ene, M.; Serban, R.M.; Stama, C.M.; Stoia, L.N. Using Social Media Data to Evaluate Urban Parks Use during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 10860. [Google Scholar] [CrossRef]
- Freeman, S.; Eykelbosh, A. COVID-19 and Outdoor Safety Considerations for Use of Outdoor Recreational Spaces; National Collaborating Centre for Environmental Health: Vancouver, BC, Canada, 2020; Available online: https://www.scirp.org/reference/referencespapers?referenceid=2872772 (accessed on 13 September 2024).
- Volenec, Z.M.; Abraham, J.O.; Becker, A.D.; Dobson, A.P. Public parks and the pandemic: How park usage has been affected by COVID-19 policies. PLoS ONE 2021, 16, e0251799. [Google Scholar] [CrossRef]
- Tully, M.A.; McMaw, L.; Adlakha, D.; Blair, N.; McAneney, J.; McAneney, H.; Carmichael, C.; Cunningham, C.; Armstrong, N.C.; Smith, L. The effect of different COVID-19 public health restrictions on mobility: A systematic review. PLoS ONE 2021, 16, e0260919. [Google Scholar] [CrossRef]
- Shoari, N.; Ezzati, M.; Baumgartner, J.; Malacarne, D.; Fecht, D. Accessibility and allocation of public parks and gardens in England and Wales: A COVID-19 social distancing perspective. PLoS ONE 2020, 15, e0241102. [Google Scholar] [CrossRef]
| Dependent Variables | Housman Test | Variable | Panel Data Model | ||||
|---|---|---|---|---|---|---|---|
| Value | Model | Coeff. | S.E. | t-Test | p-Value | ||
| Retail and recreation | 4.61 ** | Fixed | c | −15.49 | 0.218 | −71.13 | 0.00 |
| New cases | 0.00 | 0.00 | 9.67 | 0.00 | |||
| Groceries and pharmacies | 0.0258 | Random | c | 7.42 | 0.19 | 38.75 | 0.00 |
| New cases | 0.00 | 0.00 | 10.09 | 0.00 | |||
| Residential | 6.86 ** | Fixed | c | 4.16 | 0.06 | 60.08 | 0.00 |
| New cases | −0.00 | 0.00 | −2.00 | 0.04 | |||
| Transit station | 63.97 ** | Fixed | c | −19.73 | 0.20 | −97.14 | 0.00 |
| New cases | 0.00 | 0.00 | 6.48 | 0.00 | |||
| Workplaces | 28.53 ** | Fixed | c | −20.94 | 0.13 | −159.13 | 0.00 |
| New cases | 0.00 | 0.00 | 7.82 | 0.00 | |||
| Parks and open spaces | 12.23 ** | Fixed | c | 41.17 | 0.524 | 78.56 | 0.00 |
| New cases | −0.00 | 0.00 | −4.56 | 0.00 | |||
| Study Factors | F-Statistic | p-Value |
|---|---|---|
| Visitation magnitudes (y, y−) | 171.06 | 0.00 ** |
| New infections | 1.39 | 0.24 |
| Public health measures | 26.81 | 0.00 ** |
| Visitation duration (x, x−) | 29.53 | 0.00 ** |
| Study Factors | MD | p-Value | CI Lower | CI Upper |
|---|---|---|---|---|
| Visitation magnitudes (y, y−) | 143.15 | 0.00 ** | 121.24 | 165.06 |
| Public health measures | −16.49 | 0.00 ** | −22.87 | −10.12 |
| Visitation duration (x, x−) | 4.23 | 0.00 ** | 2.67 | 5.79 |
| Statistic | Value | |
| R-squared | 0.6923 | |
| Adjusted R-squared | 0.6568 | |
| F-statistic | 19.5002 | |
| Prob (F-statistic) | 0.0000 | |
| Log-likelihood | −194.5399 | |
| AIC | 397.0797 | |
| BIC | 402.6845 | |
| Jarque–Bera (JB) | 0.4013 | |
| Prob (JB) | 0.8182 | |
| Breusch–Pagan | 5.2061 | |
| Prob (BP) | 0.1573 | |
| Variable | Coefficient | p > |t| |
| Const | −272.956 | 0.156689 |
| Visitation duration | 78.28554 | 2.93 × 10−7 |
| Visitation magnitude | −0.64762 | 0.358323 |
| Public health stringency | −0.23226 | 0.943786 |
| OLS Coef | OLS p-Value | Box-Cox Coef | Box-Cox p-Value | |
|---|---|---|---|---|
| Const | 54.37 | 0.8130 | 5.54 | 0.1127 |
| Duration (x−) | 34.48 | 0.0295 | 0.72 | 0.0033 |
| Magnitude (y−) | 4.45 | 0.0403 | 0.07 | 0.0368 |
| Public health stringency | 1.89 | 0.5206 | 0.01 | 0.7340 |
| R-squared | 0.25 | - | 0.36 | - |
| Adj. R-squared | 0.16 | - | 0.29 | - |
| F-statistic | 2.8995 | 0.0540 | 4.9297 | 0.0077 |
| JB p-value | 0.00 | - | 0.67 | - |
| BP p-value | 0.54 | - | 0.53 | - |
| Box–Cox Lambda | - | - | 0.19 | - |
| Periods of Visitation Increase | |||||||
|---|---|---|---|---|---|---|---|
| Magnitude | Infection/M | Stringency | Duration | All | |||
| Periods of Visitation Declines | Magnitude | R-squared | 0.002 | 0.106 | 0.045 | 0.302 | 0.470 |
| p value | 0.802 | 0.078 | 0.260 | 0.001 *** | 0.002 ** | ||
| Infection/M | R-squared | 0.004 | 0.492 | 0.047 | 0.352 | 0.546 | |
| p value | 0.720 | 0.000 ** | 0.248 | 0.000 *** | 0.000 ** | ||
| Stringency | R-squared | 0.168 | 0.041 | 0.396 | 0.018 | 0.522 | |
| p value | 0.024 | 0.278 | 0.000 ** | 0.489 | 0.000 | ||
| Duration | R-squared | 0.172 | 0.010 | 0.037 | 0.016 | 0.189 | |
| p value | 0.022 ** | 0.598 | 0.309 | 0.493 | 0.245 | ||
| All | R-squared | 0.2535 | 0.177 | 0.4084 | 0.3551 | ||
| p value | 0.0517 ** | 0.159 | 0.00305 *** | 0.00883 *** | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahran, M.G.N.; Han, H.; Mabrouk, M.; AbouKorin, S.A.A. Social Infrastructure During the COVID-19 Pandemic: Evaluating the Impact of Outdoor Recreation on Pandemic Dynamics in Europe. Sustainability 2024, 16, 10343. https://doi.org/10.3390/su162310343
Mahran MGN, Han H, Mabrouk M, AbouKorin SAA. Social Infrastructure During the COVID-19 Pandemic: Evaluating the Impact of Outdoor Recreation on Pandemic Dynamics in Europe. Sustainability. 2024; 16(23):10343. https://doi.org/10.3390/su162310343
Chicago/Turabian StyleMahran, Mahran Gamal N., Haoying Han, Mahmoud Mabrouk, and Salma Antar A. AbouKorin. 2024. "Social Infrastructure During the COVID-19 Pandemic: Evaluating the Impact of Outdoor Recreation on Pandemic Dynamics in Europe" Sustainability 16, no. 23: 10343. https://doi.org/10.3390/su162310343
APA StyleMahran, M. G. N., Han, H., Mabrouk, M., & AbouKorin, S. A. A. (2024). Social Infrastructure During the COVID-19 Pandemic: Evaluating the Impact of Outdoor Recreation on Pandemic Dynamics in Europe. Sustainability, 16(23), 10343. https://doi.org/10.3390/su162310343









