E-Health Research in Southeast Asia: A Bibliometric Review
Abstract
1. Introduction
- How is research on eHealth in Southeast Asia distributed over time and geographical sources?
- What authors and documents have evidenced the most significant citation impact in the literature on eHealth in Southeast Asia?
- What is the intellectual structure of the knowledge base on eHealth in Southeast Asia?
- What topics have attracted the most significant attention from scholars on eHealth in Southeast Asia over time?
2. Methods
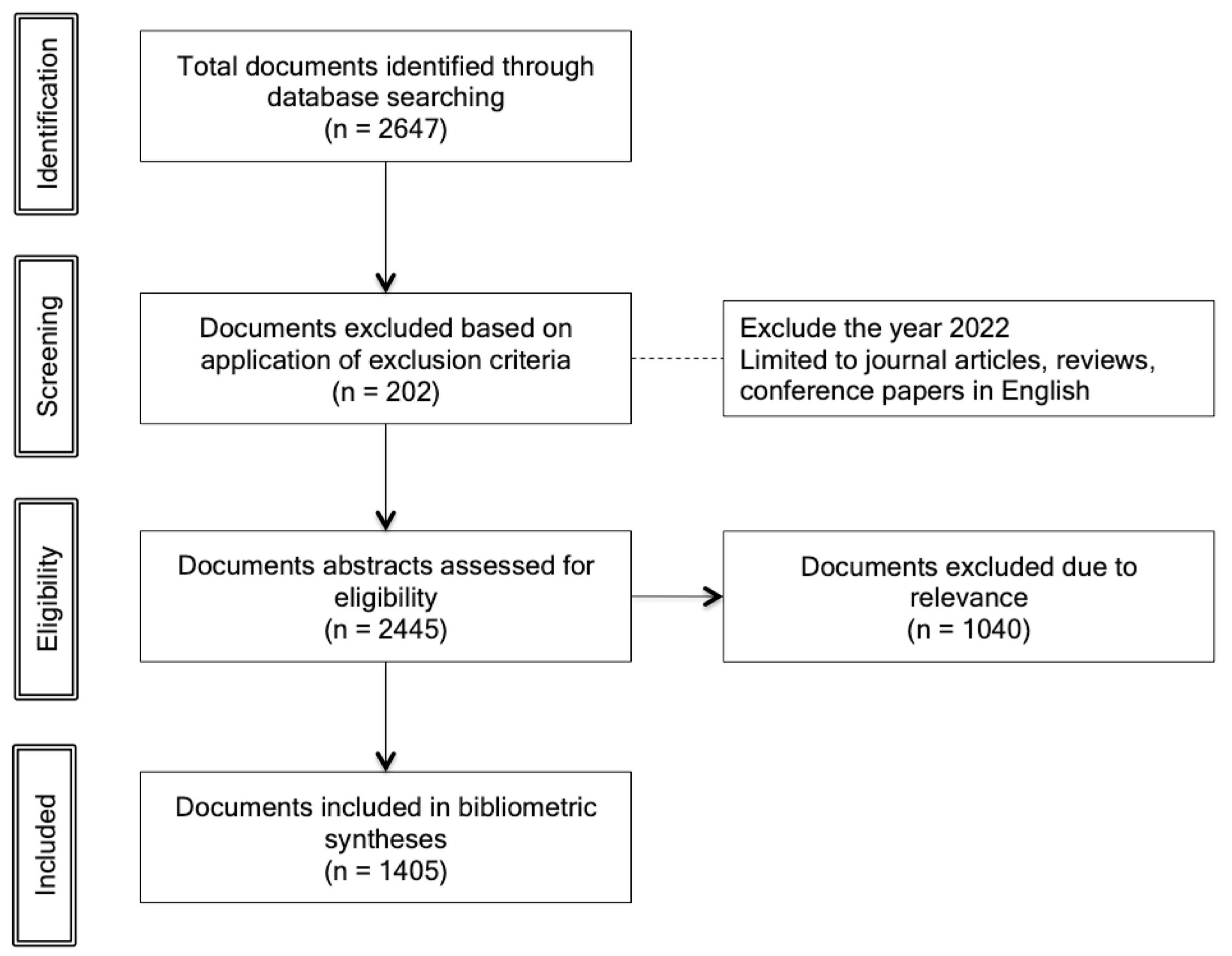
2.1. Identification of Sources for the Review
2.2. Data Analysis
3. Results
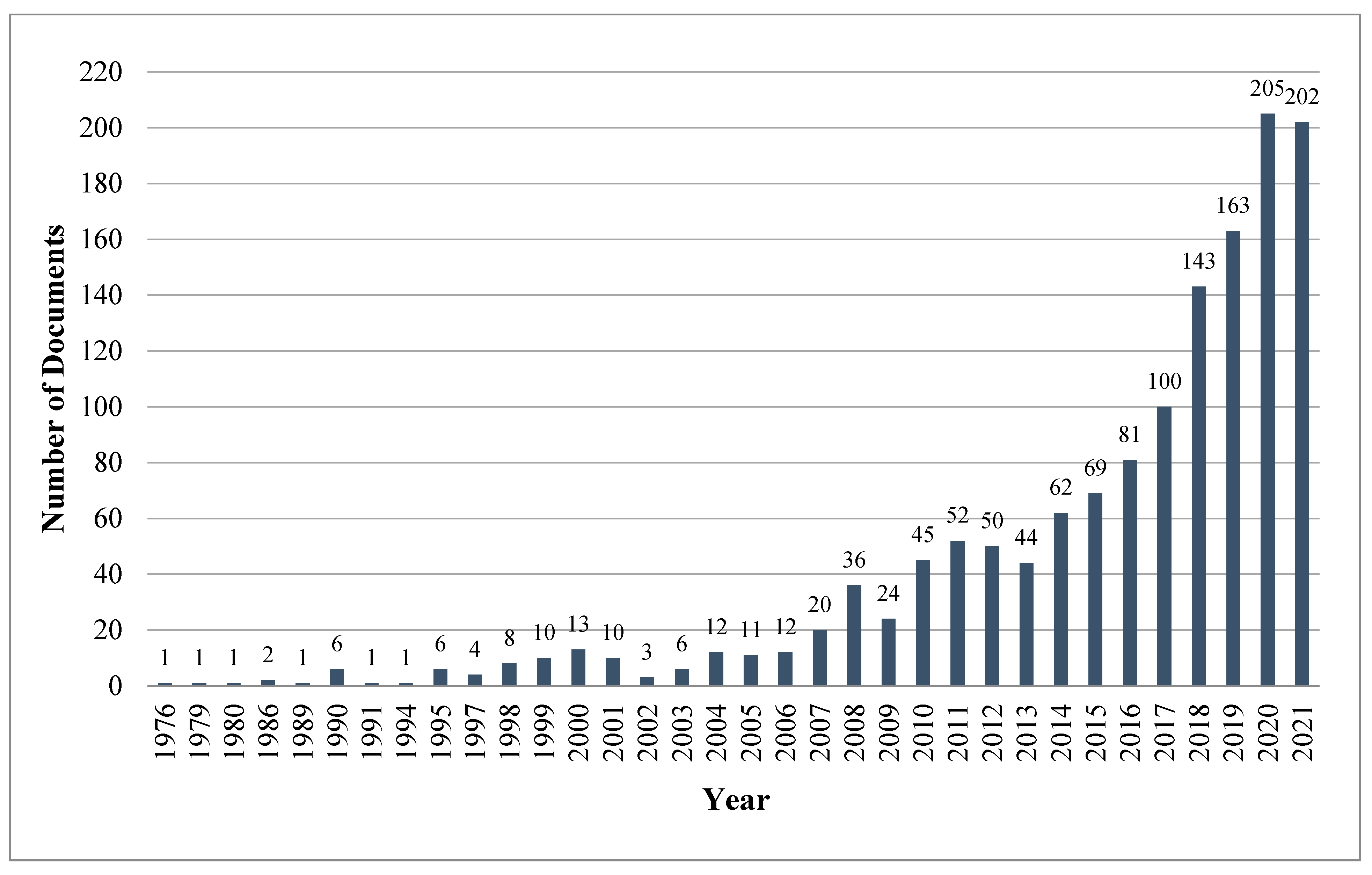
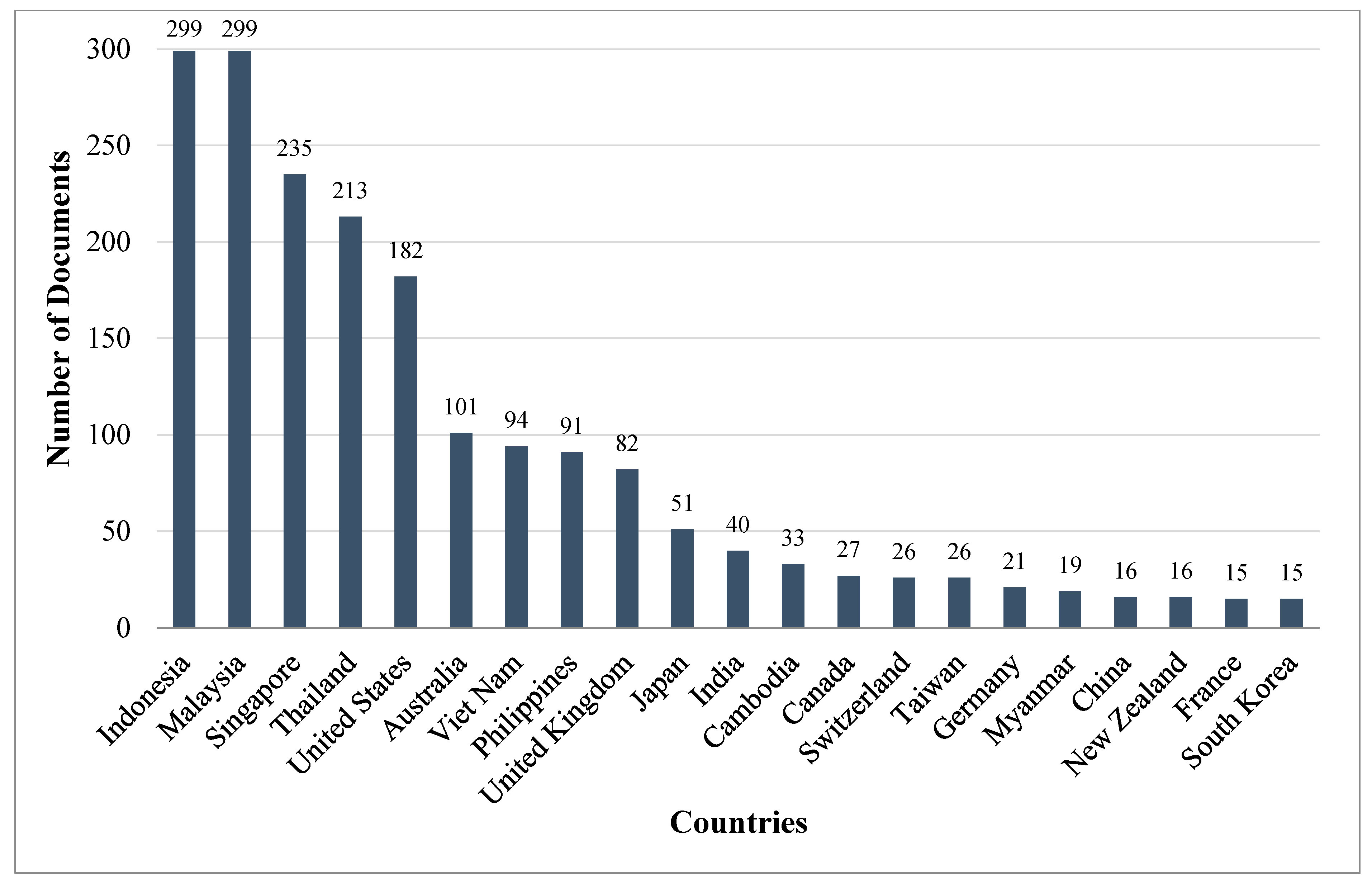
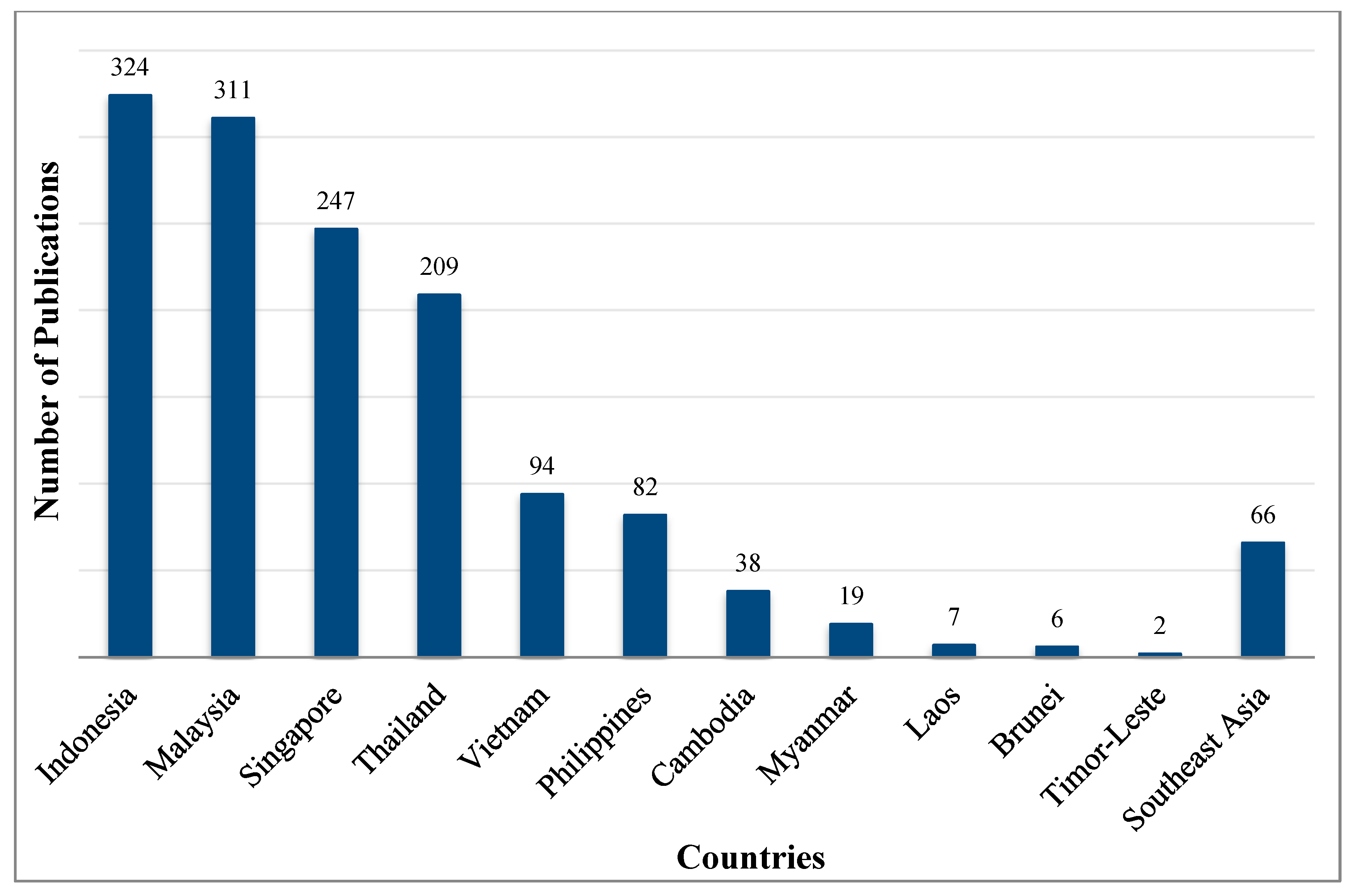
3.1. Analysis of the Descriptive Trends of the Literature on eHealth in Southeast Asia
3.2. Analysis of the Key Authors and Documents on eHealth in Southeast Asia
3.2.1. Key Authors
3.2.2. Key Documents
| Rank | Document | Nation a | Type of Document | Topical Focus | Scopus Citations |
|---|---|---|---|---|---|
| 1 | Kijsanayotin et al., (2009) [35] | TH b | Empirical | Hospital Information System | 343 |
| 2 | S. Lim et al., (2011) [43] | SG c | Empirical | m-Health | 126 |
| 3 | Ahmadi et al., (2015) [42] | UK d | Empirical | Hospital Information System | 85 |
| 4 | Xue et al., (2012) [46] | SG c | Empirical | m-Health | 80 |
| 5 | Lee et al., (1998) [47] | US e | Empirical | Telehealth | 80 |
| 6 | Son and Tuan (2016) [48] | VT f | Empirical | Data Mining | 74 |
| 7 | Fabrlzio et al., (2000) [39] | US e | Empirical | Telehealth | 74 |
| 8 | Ahmadi et al., (2017) [45] | UK d | Empirical | Hospital Information System | 71 |
| 9 | Nguyen et al., (2016) [49] | CA g | Empirical | Telehealth | 71 |
| 10 | Roffeei et al., (2015) [50] | MY h | Empirical | Telehealth | 66 |
| 11 | Yeung and Gourlay (2012) [51] | SG c | Empirical | Geographic Information System | 65 |
| 12 | Chaikaew et al., (2009) [52] | TH b | Review | Telehealth | 65 |
| 13 | Kittayapong et al., (2008) [53] | TH b | Empirical | Geographic Information System | 63 |
| 14 | Entwisle et al., (1997) [54] | US e | Empirical | Geographic Information System | 60 |
| 15 | Mohan and Yaacob (2004) [55] | MY h | Conceptual | Telehealth | 58 |
| 16 | Müller et al., (2016) [56] | SG c | Empirical | m-Health | 56 |
| 17 | Miles et al., (2017) [57] | UK d | Review | m-Health | 55 |
| 18 | Chib and Chen (2011) [58] | SG c | Empirical | m-Health | 54 |
| 19 | Smith et al., (2015) [59] | UK d | Empirical | m-Health | 52 |
| 20 | Zaidan et al., (2015) [60] | MY h | Conceptual | Telehealth | 52 |
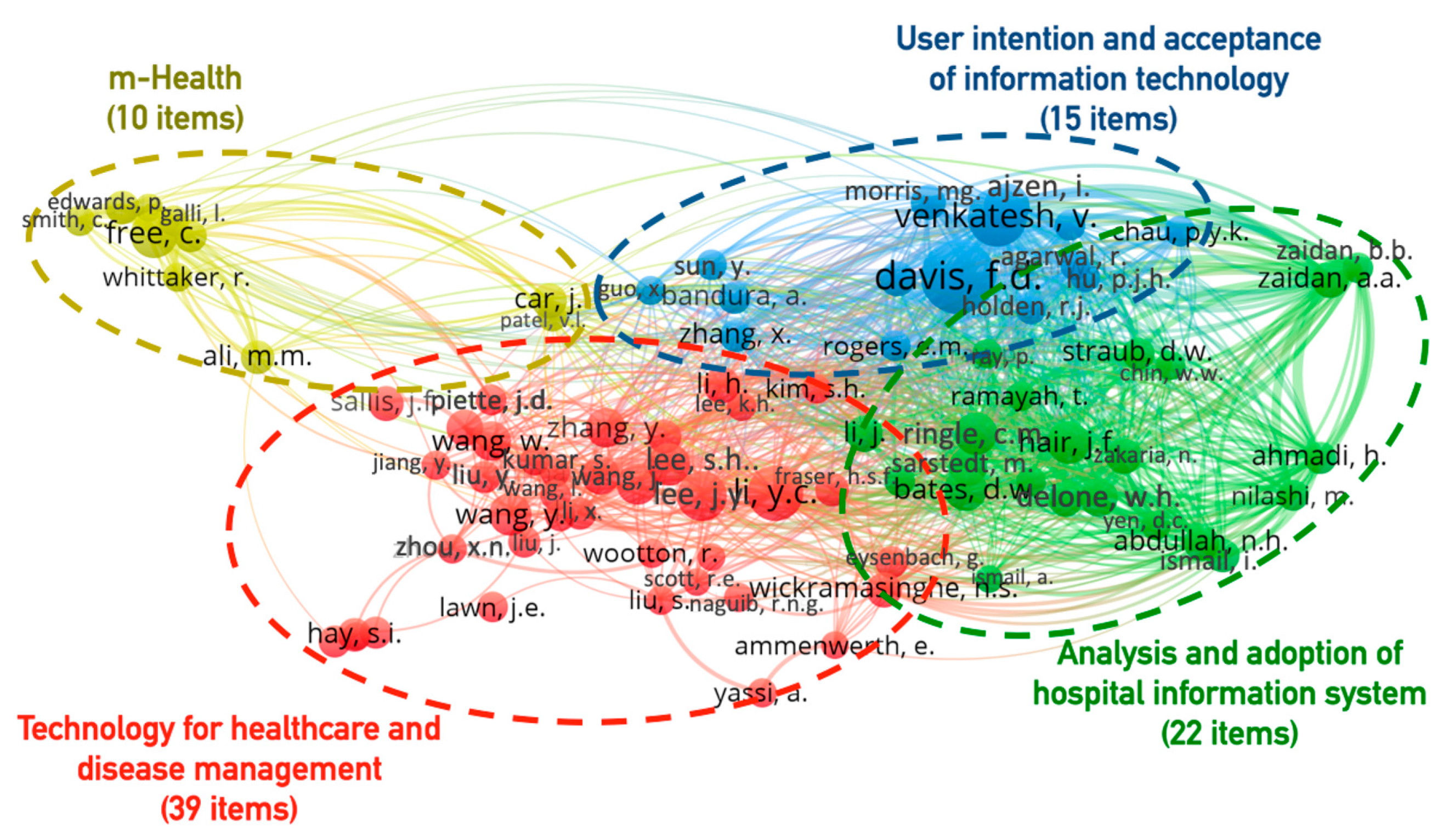
3.3. Intellectual Structure of the eHealth Literature in Southeast Asia
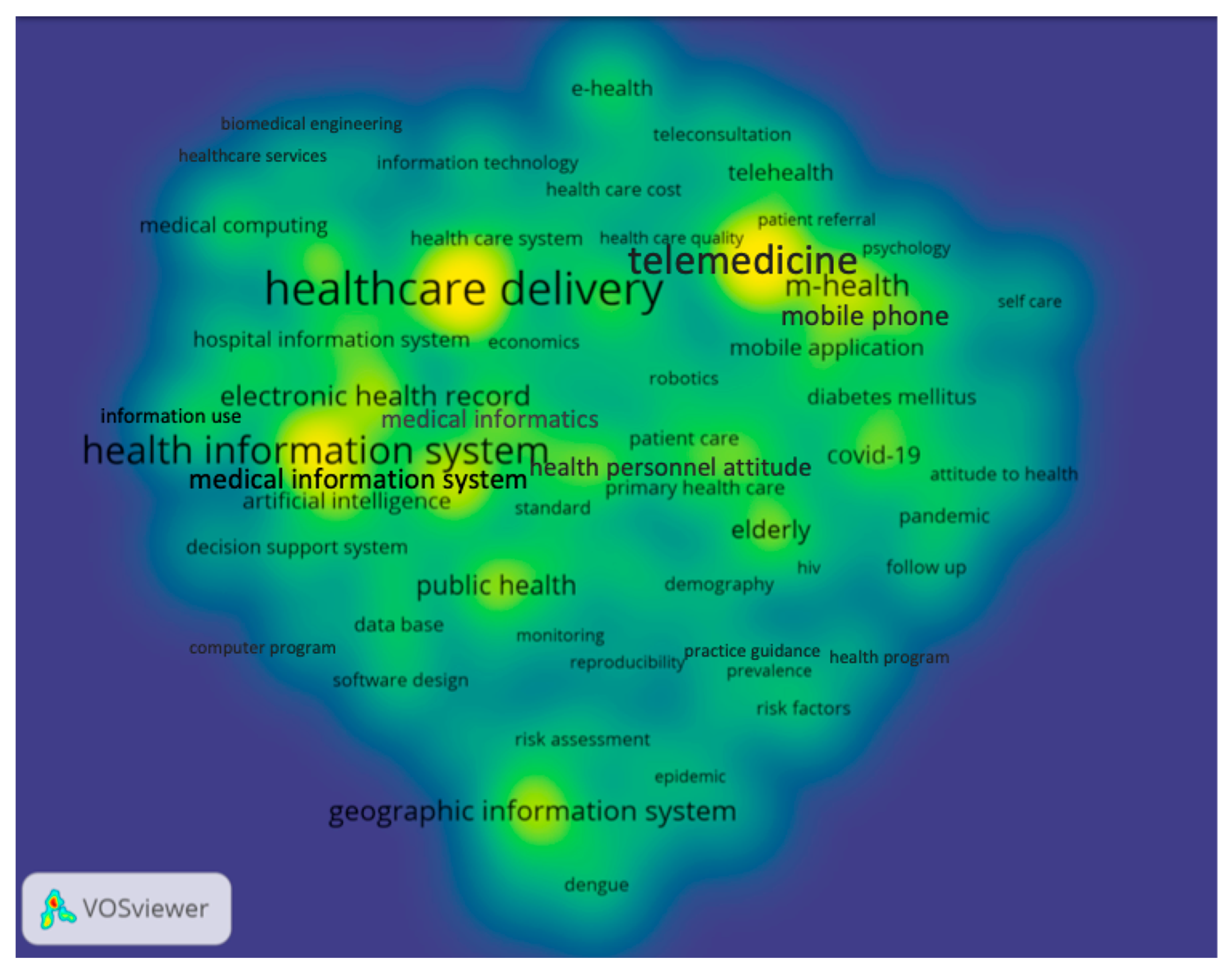
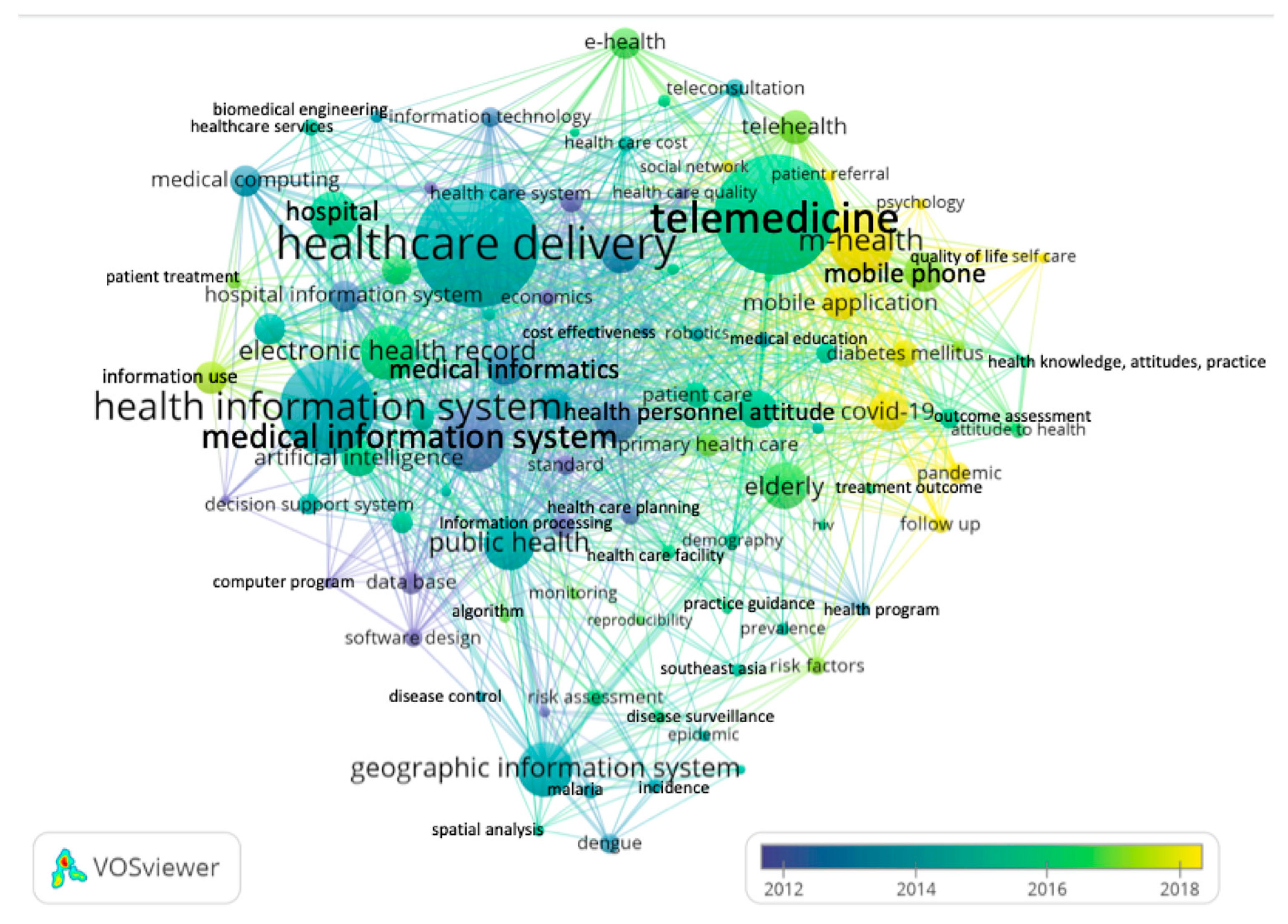
3.4. Topical Foci of the eHealth in Southeast Asia Knowledge Base
4. Discussion
4.1. Limitations
4.2. Interpretation of the Findings
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Awad, A.; Trenfield, S.J.; Pollard, T.D.; Ong, J.J.; Elbadawi, M.; McCoubrey, L.E.; Goyanes, A.; Gaisford, S.; Basit, A.W. Connected healthcare: Improving patient care using digital health technologies. Adv. Drug Deliv. Rev. 2021, 178, 113958. [Google Scholar] [CrossRef] [PubMed]
- Punnakitikashem, P.; Hallinger, P. Bibliometric Review of the Knowledge Base on Healthcare Management for Sustainability, 1994–2018. Sustainability 2019, 12, 205. [Google Scholar] [CrossRef]
- World Health Organization. Global Strategy on Digital Health 2020–2025. 2020. Available online: https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf (accessed on 2 January 2021).
- Novillo-Ortiz, D.; Marin, H.D.F.; Saigí-Rubió, F. The role of digital health in supporting the achievement of the Sustainable Development Goals (SDGs). Int. J. Med. Inform. 2018, 114, 106–107. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, R.C. The promise of e-Health–A Canadian perspective. eHealth Int. 2002, 1, 4. [Google Scholar] [CrossRef] [PubMed]
- Black, A.D.; Car, J.; Pagliari, C.; Anandan, C.; Cresswell, K.; Bokun, T.; McKinstry, B.; Procter, R.; Majeed, A.; Sheikh, A. The Impact of eHealth on the Quality and Safety of Health Care: A Systematic Overview. PLoS Med. 2011, 8, e1000387. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.; Jadad, A.; Rizo, C.; Enkin, M.; Powell, J.; Pagliari, C. What Is eHealth (3): A Systematic Review of Published Definitions. J. Med Internet Res. 2005, 7, e110. [Google Scholar] [CrossRef]
- Luk, C.Y. The impact of digital health on traditional healthcare systems and doctor-patient relationships: The case study of Singapore. In Innovative Perspectives on Public Administration in the Digital Age; IGI Global: Hershey, PA, USA, 2018; pp. 143–167. [Google Scholar]
- Penedo, F.J.; Oswald, L.B.; Kronenfeld, J.P.; Garcia, S.F.; Cella, D.; Yanez, B. The increasing value of eHealth in the delivery of patient-centred cancer care. Lancet Oncol. 2020, 21, e240–e251. [Google Scholar] [CrossRef]
- Brørs, G.; Norman, C.D.; Norekvål, T.M. Accelerated importance of eHealth literacy in the COVID-19 outbreak and beyond. Eur. J. Cardiovasc. Nurs. 2020, 19, 458–461. [Google Scholar] [CrossRef]
- Watson, A.R.; Wah, R.; Thamman, R. The Value of Remote Monitoring for the COVID-19 Pandemic. Telemed. e-Health 2020, 26, 1110–1112. [Google Scholar] [CrossRef]
- Koonin, L.M.; Hoots, B.; Tsang, C.A.; Leroy, Z.; Farris, K.; Jolly, B.; Antall, P.; McCabe, B.; Zelis, C.B.; Tong, I. Trends in the Use of Telehealth during the Emergence of the COVID-19 Pandemic—United States, January–March 2020. Morb. Mortal. Wkly. Rep. Cent. Dis. Control. Prev. 2020, 69, 1595–1599. Available online: https://www.cdc.gov/mmwr/volumes/69/wr/mm6943a3.htm (accessed on 8 July 2022). [CrossRef]
- Monaghesh, E.; Hajizadeh, A. The role of telehealth during COVID-19 outbreak: A systematic review based on current evidence. BMC Public Health 2020, 20, 1193. [Google Scholar] [CrossRef] [PubMed]
- Wosik, J.; Fudim, M.; Cameron, B.; Gellad, Z.F.; Cho, A.; Phinney, D.; Curtis, S.; Roman, M.; Poon, E.G.; Ferranti, J. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Inform. Assoc. 2020, 27, 957–962. [Google Scholar] [CrossRef] [PubMed]
- The ASEAN Secretariat. Master Plan on ASEAN Connectivity 2025; The ASEAN Secretariat: Jakarta, Indonesia, 2016. [Google Scholar]
- Ang, I.Y.H.; Tan, K.X.Q.; Tan, C.; Tan, C.H.; Kwek, J.W.M.; Tay, J.; Toh, S.A. A Personalized Mobile Health Program for Type 2 Diabetes During the COVID-19 Pandemic: Single-Group Pre–Post Study. JMIR Diabetes 2021, 6, e25820. [Google Scholar] [CrossRef] [PubMed]
- Le, H.T.; Nguyen, D.N.; Beydoun, A.S.; Le, X.T.T.; Nguyen, T.T.; Pham, Q.T.; Ta, N.T.K.; Nguyen, Q.T.; Nguyen, A.N.; Hoang, M.T.; et al. Demand for Health Information on COVID-19 among Vietnamese. Int. J. Environ. Res. Public Health 2020, 17, 4377. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.M.; Teo, C.H.; Ng, C.J.; Chiew, T.K.; Ng, W.L.; Abdullah, A.; Hadi, H.A.; Liew, C.S.; Chan, C.S. An Automated Patient Self-Monitoring System to Reduce Health Care System Burden During the COVID-19 Pandemic in Malaysia: Development and Implementation Study. JMIR Public Health Surveill. 2021, 9, e23427. [Google Scholar] [CrossRef] [PubMed]
- Teh, H.L.; Suan, M.A.M.; Mohammed, N.S. Geriatric Telemedicine: Ensuring continuity of healthcare services to the older patients in Kedah, Malaysia during the COVID-19 pandemic. Med J. Malays. 2021, 76, 562–564. [Google Scholar]
- Fatehi, F.; Wootton, R. Telemedicine, telehealth or e-health? A bibliometric analysis of the trends in the use of these terms. J. Telemed. Telecare 2012, 18, 460–464. [Google Scholar] [CrossRef]
- Müller, A.M.; A Maher, C.; Vandelanotte, C.; Hingle, M.; Middelweerd, A.; Lopez, M.L.; Desmet, A.; E Short, C.; Nathan, N.; Hutchesson, M.J.; et al. Physical Activity, Sedentary Behavior, and Diet-Related eHealth and mHealth Research: Bibliometric Analysis. J. Med. Internet Res. 2018, 20, e122. [Google Scholar] [CrossRef]
- Welsh, T.S. The literature of telemedicine: A bibliometric study. Sci. Technol. 2005, 25, 21–34. [Google Scholar] [CrossRef]
- Zupic, I.; Čater, T. Bibliometric methods in management and organization. Organ. Res. Methods 2015, 18, 429–472. [Google Scholar] [CrossRef]
- Falagas, M.E.; Pitsouni, E.I.; Malietzis, G.; Pappas, G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: Strengths and weaknesses. FASEB J. 2007, 22, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Hallinger, P.; Kovačević, J. A Bibliometric Review of Research on Educational Administration: Science Mapping the Literature, 1960 to 2018. Rev. Educ. Res. 2019, 89, 335–369. [Google Scholar] [CrossRef]
- Hallinger, P.; Wang, R. The Evolution of Simulation-Based Learning Across the Disciplines, 1965–2018: A Science Map of the Literature. Simul. Gaming 2019, 51, 9–32. [Google Scholar] [CrossRef]
- Mongeon, P.; Paul-Hus, A. The journal coverage of Web of Science and Scopus: A comparative analysis. Scientometrics 2016, 106, 213–228. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Agustina, R.; Dartanto, T.; Sitompul, R.; Susiloretni, K.A.; Suparmi; Achadi, E.L.; Taher, A.; Wirawan, F.; Sungkar, S.; Sudarmono, P.; et al. Universal health coverage in Indonesia: Concept, progress, and challenges. Lancet 2018, 393, 75–102. [Google Scholar] [CrossRef] [PubMed]
- Gros, D.F.; Yoder, M.; Tuerk, P.W.; Lozano, B.E.; Acierno, R. Exposure Therapy for PTSD Delivered to Veterans via Telehealth: Predictors of Treatment Completion and Outcome and Comparison to Treatment Delivered in Person. Behav. Ther. 2011, 42, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Van Eck, N.J.; Waltman, L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics 2010, 84, 523–538. [Google Scholar] [CrossRef]
- Chua, S.G.; Dobberstein, N. The ASEAN Digital Revolution. Kearney. 2015, pp. 1–46. Available online: https://www.kearney.com/documents/20152/5364057/The+ASEAN+digital+revolution.pdf/625da4b5-8d05-6798-004a-e49a59e8d817?t=1581504740845 (accessed on 11 August 2022).
- Erh, J. Assessing Digital Economy Policies in Six Southeast Asian Countries. © ISEAS Yusof Ishak Institute 2021. Available online: http://hdl.handle.net/11540/13645 (accessed on 11 August 2022).
- Friede, A.; Blum, H.L.; McDonald, M. Public health informatics: How information-age technology can strengthen public health. Annu. Rev. Public Health 1995, 16, 239–252. [Google Scholar] [CrossRef]
- Kijsanayotin, B.; Pannarunothai, S.; Speedie, S.M. Factors influencing health information technology adoption in Thailand’s community health centers: Applying the UTAUT model. Int. J. Med. Inform. 2009, 78, 404–416. [Google Scholar] [CrossRef]
- Ong, M.E.H.; Tan, E.H.; Yan, X.; Anushia, P.; Lim, S.H.; Leong, B.S.-H.; Ong, V.Y.K.; Tiah, L.; Yap, S.; Overton, J.; et al. An observational study describing the geographic-time distribution of cardiac arrests in Singapore: What is the utility of geographic information systems for planning public access defibrillation? (PADS Phase I). Resuscitation 2008, 76, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Singhasivanon, P. Malaria, Multi-Drug Resistance and Economic Development in the Greater Mekong Subregion of Southeast Asia-Incorporating geographical information systems databases. Southeast Asian J. Trop. Med. Public Health 1999, 30 (Suppl. 4), 97–101. Available online: https://www.scopus.com/inward/record.uri?eid=2-s2.0-29744468239&partnerID=40&md5=7a8068a447dfbd87e0c580f5805e9aa9 (accessed on 30 August 2022).
- Detmer, D.E.; Shortliffe, E.H. Clinical informatics: Prospects for a new medical subspecialty. JAMA 2014, 311, 2067–2068. [Google Scholar] [CrossRef] [PubMed]
- Fabrlzio, M.D.; Lee, B.R.; Chan, D.Y.; Stoianovici, D.; Jarrett, T.W.; Yang, C.; Kavoussi, L.R. Effect of Time Delay on Surgical Performance During Telesurgical Manipulation. J. Endourol. 2000, 14, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Gorny, A.W.; Liew, S.J.; Tan, C.S.; Müller-Riemenschneider, F. Fitbit charge HR wireless heart rate monitor: Validation study conducted under free-living conditions. JMIR mHealth uHealth 2017, 5, e8233. [Google Scholar] [CrossRef]
- Rim, T.H.; Da Soh, Z.; Tham, Y.-C.; Yang, H.H.S.; Lee, G.; Kim, Y.; Nusinovici, S.; Ting, D.S.W.; Wong, T.Y.; Cheng, C.-Y. Deep Learning for Automated Sorting of Retinal Photographs. Ophthalmol. Retin. 2020, 4, 793–800. [Google Scholar] [CrossRef]
- Ahmadi, H.; Nilashi, M.; Ibrahim, O. Organizational decision to adopt hospital information system: An empirical investigation in the case of Malaysian public hospitals. Int. J. Med. Inform. 2015, 84, 166–188. [Google Scholar] [CrossRef]
- Lim, S.; Xue, L.; Yen, C.C.; Chang, L.; Chan, H.C.; Tai, B.C.; Duh, H.B.L.; Choolani, M. A study on Singaporean women’s acceptance of using mobile phones to seek health information. Int. J. Med. Inform. 2011, 80, e189–e202. [Google Scholar] [CrossRef]
- Schüll, N.D. Data for life: Wearable technology and the design of self-care. Biosocieties 2016, 11, 317–333. [Google Scholar] [CrossRef]
- Ahmadi, H.; Nilashi, M.; Shahmoradi, L.; Ibrahim, O. Hospital Information System adoption: Expert perspectives on an adoption framework for Malaysian public hospitals. Comput. Hum. Behav. 2017, 67, 161–189. [Google Scholar] [CrossRef]
- Xue, L.; Yen, C.C.; Chang, L.; Chan, H.C.; Tai, B.C.; Tan, S.B.; Duh, H.B.L.; Choolani, M. An exploratory study of ageing women’s perception on access to health informatics via a mobile phone-based intervention. Int. J. Med. Inform. 2012, 81, 637–648. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.R.; Bishoff, J.T.; Janetschek, G.; Bunyaratevej, P.; Kamolpronwijit, W.; Cadeddu, J.A.; Ratchanon, S.; O’Kelley, S.; Kavoussi, L.R. A novel method of surgical instruction: International telementoring. World J. Urol. 1998, 16, 367–370. [Google Scholar] [CrossRef] [PubMed]
- Son, L.H.; Tuan, T.M. A cooperative semi-supervised fuzzy clustering framework for dental X-ray image segmentation. Expert Syst. Appl. 2016, 46, 380–393. [Google Scholar] [CrossRef]
- Nguyen, H.V.; Tan, G.S.W.; Tapp, R.J.; Mital, S.; Ting, D.S.W.; Wong, H.T.; Tan, C.S.; Laude, A.; Tai, E.S.; Tan, N.C.; et al. Cost-effectiveness of a National Telemedicine Diabetic Retinopathy Screening Program in Singapore. Ophthalmology 2016, 123, 2571–2580. [Google Scholar] [CrossRef]
- Roffeei, S.H.M.; Abdullah, N.; Basar, S.K.R. Seeking social support on Facebook for children with Autism Spectrum Disorders (ASDs). Int. J. Med. Inform. 2015, 84, 375–385. [Google Scholar] [CrossRef]
- Yeung, B.P.M.; Gourlay, T. A technical review of flexible endoscopic multitasking platforms. Int. J. Surg. 2012, 10, 345–354. [Google Scholar] [CrossRef]
- Chaikaew, N.; Tripathi, N.K.; Souris, M. Exploring spatial patterns and hotspots of diarrhea in Chiang Mai, Thailand. Int. J. Health Geogr. 2009, 8, 36. [Google Scholar] [CrossRef]
- Kittayapong, P.; Bhumiratana, A.; Yoksan, S.; Chansang, U.; Chansang, C. Suppression of Dengue Transmission by Application of Integrated Vector Control Strategies at Sero-Positive GIS-Based Foci. Am. J. Trop. Med. Hyg. 2008, 78, 70–76. [Google Scholar] [CrossRef]
- Entwisle, B.; Rindfuss, R.R.; Walsh, S.J.; Evans, T.P.; Curran, S.R. Geographic information systems, spatial network analysis, and contraceptive choice. Demography 1997, 34, 171–187. [Google Scholar] [CrossRef]
- Mohan, J.; Yaacob, R.R.R. The Malaysian telehealth flagship application: A national approach to health data protection and utilisation and consumer rights. Int. J. Med. Inform. 2004, 73, 217–227. [Google Scholar] [CrossRef]
- Müller, A.M.; Khoo, S.; Morris, T. Text Messaging for Exercise Promotion in Older Adults from an Upper-Middle-Income Country: Randomized Controlled Trial. J. Med. Internet Res. 2016, 18, e5. [Google Scholar] [CrossRef] [PubMed]
- Miles, C.; Arden-Close, E.; Thomas, M.; Bruton, A.; Yardley, L.; Hankins, M.; Kirby, S.E. Barriers and facilitators of effective self-management in asthma: Systematic review and thematic synthesis of patient and healthcare professional views. npj Prim. Care Respir. Med. 2017, 27, 57. [Google Scholar] [CrossRef] [PubMed]
- Chib, A.; Chen, V.H.H. Midwives with mobiles: A dialectical perspective on gender arising from technology introduction in rural Indonesia. New Media Soc. 2011, 13, 486–501. [Google Scholar] [CrossRef]
- Smith, C.; Ngo, T.D.; Gold, J.; Edwards, P.; Vannak, U.; Sokhey, L.; Machiyama, K.; Slaymaker, E.; Warnock, R.; McCarthy, O.; et al. Effect of a mobile phone-based intervention on post-abortion contraception: A randomized controlled trial in Cambodia. Bull. World Health Organ. 2015, 93, 842A–850A. [Google Scholar] [CrossRef]
- Zaidan, B.B.; Al-Haiqi, A.; Zaidan, A.A.; Abdulnabi, M.; Kiah, M.L.M.; Muzamel, H. A Security Framework for Nationwide Health Information Exchange based on Telehealth Strategy. J. Med Syst. 2015, 39, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Sweileh, W.M.; Al-Jabi, S.W.; AbuTaha, A.S.; Zyoud, S.H.; Anayah, F.; Sawalha, A.F. Bibliometric analysis of worldwide scientific literature in mobile-health: 2006–2016. BMC Med. Inform. Decis. Mak. 2017, 17, 72. [Google Scholar] [CrossRef] [PubMed]
- Üsdiken, B.; Pasadeos, Y. Organizational analysis in North America and Europe: A comparison of co-citation networks. Organ. Stud. 1995, 16, 503–526. [Google Scholar] [CrossRef]
- Small, H. Co-citation in the scientific literature: A new measure of the relationship between two documents. J. Am. Soc. Inf. Sci. 1973, 24, 265–269. [Google Scholar] [CrossRef]
- Li, Y.-C.; Hung, M.-C.; Hsiao, S.-J.; Tsai, K.-D.; Chang, M.-M. An Assessment of Patient Safety in Acupuncture Process Under EMR Support. J. Med. Syst. 2010, 35, 1447–1453. [Google Scholar] [CrossRef]
- Li, Y.-C.; Chang, I.-C.; Hung, W.-F.; Fu, H.-K. The Critical Factors Affecting Hospital Adoption of Mobile Nursing Technologies in Taiwan. In Proceedings of the 38th Annual Hawaii International Conference on System Sciences, Big Island, HI, USA, 6 January 2005; p. 157b. [Google Scholar]
- Jaana, M.; Sicotte, C.; Paré, G. Exploring Health Information Technology Innovativeness and its Antecedents in Canadian Hospitals. Methods Inf. Med. 2010, 49, 28–36. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, Z. Automatic detecting indicators for quality of health information on the Web. Int. J. Med. Inform. 2007, 76, 575–582. [Google Scholar] [CrossRef] [PubMed]
- Wickramasinghe, N. IS/IT as a tool to achieve goal alignment. Int. J. Health Technol. Manag. 2000, 2, 163. [Google Scholar] [CrossRef]
- Wickramasinghe, N.; Misra, S.K. A wireless trust model for healthcare. Int. J. Electron. Health 2004, 1, 60–77. [Google Scholar] [CrossRef] [PubMed]
- Bates, D.W.; Gawande, A.A. Improving safety with information technology. N. Engl. J. Med. Mass Med. Soc. 2003, 348, 2526–2534. [Google Scholar] [CrossRef]
- Delone, W.H.; McLean, E.R. The DeLone and McLean Model of Information Systems Success: A Ten-Year Update. J. Manag. Inf. Syst. 2003, 19, 9–30. [Google Scholar]
- Ismail, A.; Jamil, A.T.; Rahman, A.F.A.; Bakar, J.M.A.; Saad, N.M.; Saadi, H. The implementation of Hospital Information System (HIS) in tertiary hospitals in malaysia: A qualitative study. Malays. J. Public. Health Med. 2010, 10, 16–24. [Google Scholar]
- Hair, J.F. Multivariate Data Analysis: A Global Perspective, 7th ed.; Prentice Hall: Upper Saddle River, NJ, USA, 2009. [Google Scholar]
- Agarwal, R.; Prasad, J. The antecedents and consequents of user perceptions in information technology adoption. Decis. Support Syst. 1998, 22, 15–29. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Fishbein, M.; Ajzen, I. Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research. Philos. Rhetor. 1977, 6, 244–245. [Google Scholar]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User acceptance of information technology: Toward a unified view. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Chib, A.; van Velthoven, M.H.; Car, J. mHealth Adoption in Low-Resource Environments: A Review of the Use of Mobile Healthcare in Developing Countries. J. Health Commun. 2014, 20, 4–34. [Google Scholar] [CrossRef] [PubMed]
- Free, C.; Phillips, G.; Galli, L.; Watson, L.; Felix, L.; Edwards, P.; Patel, V.; Haines, A. The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review. PLoS Med. 2013, 10, e1001362. [Google Scholar] [CrossRef]
- Whittaker, R.; McRobbie, H.; Bullen, C.; Rodgers, A.; Gu, Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst. Rev. 2016, 4, CD006611. [Google Scholar] [CrossRef] [PubMed]
- Van Do, V.; Spears, C.A.; Van Minh, H.; Huang, J.; Redmon, P.B.; Long, N.X.; Eriksen, M.P. Perceptions about mindfulness and text messaging for smoking cessation in Vietnam: Results from a qualitative study. JMIR mHealth uHealth 2020, 8, e17337. [Google Scholar]
- Bal, P.; Shamsir, S.; Warid, N.; Yahya, A.; Yunus, J.; Supriyanto, E.; Ngim, C.F. MHealth application: Mobile thalassemia patient management application. In Proceedings of the 2014 IEEE Conference on Biomedical Engineering and Sciences (IECBES), Kuala Lumpur, Malaysia, 8–10 December 2014; IEEE: Piscataway, NJ, USA, 2014; pp. 792–796. [Google Scholar]
- DeSilva, M.; Vu, C.N.; Bonawitz, R.; Hai, L.T.; Van Lam, N.; Yen, L.T.; Gifford, A.L.; Haberer, J.; Linh, D.T.; Sabin, L. The Supporting Adolescent Adherence in Vietnam (SAAV) study: Study protocol for a randomized controlled trial assessing an mHealth approach to improving adherence for adolescents living with HIV in Vietnam. Trials 2019, 20, 150. [Google Scholar] [CrossRef] [PubMed]
- Liverani, M.; Ir, P.; Wiseman, V.; Perel, P. User experiences and perceptions of health wearables: An exploratory study in Cambodia. Glob. Health Res. Policy 2021, 6, 33. [Google Scholar] [CrossRef] [PubMed]
- Suwanthara, J.; Noinongyao, A.; Vittayakorn, S. WiseMed: Medication reminder for seniors. In Proceedings of the 2019 23rd International Computer Science and Engineering Conference (ICSEC), Phuket, Thailand, 30 October–1 November 2019; IEEE: Piscataway, NJ, USA, 2019; pp. 409–414. [Google Scholar]
- Becker, S.; Miron-Shatz, T.; Schumacher, N.; Krocza, J.; Diamantidis, C.; Albrecht, U.-V. mHealth 2.0: Experiences, possibilities, and perspectives. JMIR mHealth uHealth 2014, 2, e3328. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.; Li, T.; Wang, X.; Yang, X.; Yu, Z. Visualizing the intellectual structure and evolution of electronic health and telemedicine research. Int. J. Med. Inform. 2019, 130, 103947. [Google Scholar] [CrossRef]
- Giansanti, D. The Role of the mHealth in the Fight against the COVID-19: Successes and Failures. Healthcare 2021, 9, 58. [Google Scholar] [CrossRef]
- Paul, J.; Criado, A.R. The art of writing literature review: What do we know and what do we need to know? Int. Bus. Rev. 2020, 29, 101717. [Google Scholar] [CrossRef]
- World Bank. The Digital Economy in Southeast Asia: Strengthening the Foundations for Future Growth. World Bank. 2019. Available online: https://documents1.worldbank.org/curated/en/328941558708267736/pdf/The-Digital-Economy-in-Southeast-Asia-Strengthening-the-Foundations-for-Future-Growth.pdf (accessed on 2 January 2021).
- Uribe-Toril, J.; Ruiz-Real, J.L.; Nievas-Soriano, B.J. A study of eHealth from the perspective of social sciences. Healthcare 2021, 9, 108. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, Q.A.; Shah, B.; Kundi, G.M.; Nawaz, A.; Miankhel, A.K.; Chishti, K.A.; Qureshi, N.A. Infrastructural barriers to e-health implementation in developing countries. Eur. J. Sustain. Dev. 2013, 2, 163. [Google Scholar]
| Rank | Author | Nation | Documents | Scopus Citation | CPD a | Topical Focus |
|---|---|---|---|---|---|---|
| 1 | Pannarunothai, S. | Thailand | 5 | 374 | 75 | Public Health Informatics |
| 2 | Kijsanayotin, B. | Thailand | 9 | 373 | 41 | Public Health Informatics |
| 3 | Speedie, S.M. | US b | 4 | 351 | 88 | Public Health Informatics |
| 4 | Choolani, M. | Singapore | 3 | 223 | 74 | m-Health |
| 5 | Ong, M.E.H | Singapore | 10 | 222 | 22 | Public Health Informatics |
| 6 | Nilashi, M. | Malaysia | 5 | 210 | 42 | HIS d |
| 7 | Ibrahim, O. | Malaysia | 4 | 209 | 52 | HIS d |
| 8 | Tai, B.C. | Singapore | 3 | 208 | 69 | m-Health |
| 9 | Chan, H.C. | Singapore | 2 | 206 | 103 | m-Health |
| 10 | Chang, L. | Singapore | 2 | 206 | 103 | m-Health |
| 11 | Duh, H.B.L. | Singapore | 2 | 206 | 103 | m-Health |
| 12 | Xue, L. | Singapore | 2 | 206 | 103 | m-Health |
| 13 | Yen, C.C. | Singapore | 2 | 206 | 103 | m-Health |
| 14 | Lee, B.R. | US b | 4 | 185 | 46 | Clinical Informatics |
| 15 | Kavoussi, L.R. | US b | 3 | 183 | 61 | Clinical Informatics |
| 16 | Ahmadi, H. | UK c | 4 | 177 | 44 | HIS d |
| 17 | Wong, T.Y. | Singapore | 8 | 177 | 22 | Clinical Informatics |
| 18 | Singhasivanon, P. | Thailand | 5 | 171 | 34 | Public Health Informatics |
| 19 | Tan, C.S. | Singapore | 7 | 167 | 24 | Clinical Informatics |
| 20 | Ngo, T.D. | UK c | 7 | 146 | 21 | m-Health |
| Rank | Author | Nation | Co-Citation | Topical Focus |
|---|---|---|---|---|
| 1 | Davis, F.D. | United States | 112 | User intention and acceptance of IT |
| 2 | Venkatesh, V. | United States | 75 | User intention and acceptance of IT |
| 3 | Li, Y.C. | Taiwan | 70 | Technology for healthcare and disease management |
| 4 | Lee, J.Y. | United States | 58 | Technology for healthcare and disease management |
| 5 | Free, C. | United Kingdom | 53 | m-Health |
| 6 | Ajzen, I. | United States | 50 | User intention and acceptance of IT |
| 7 | Hair, J.F. | United States | 46 | Analysis and adoption of hospital information system |
| 8 | Ringle, C.M. | Germany | 45 | Analysis and adoption of hospital information system |
| 9 | Bates, D.W. | United States | 44 | Analysis and adoption of hospital information system |
| 10 | Lee, S.H. | United Kingdom | 44 | Technology for healthcare and disease management |
| 11 | Wang, Y. | Canada | 44 | Technology for healthcare and disease management |
| 12 | Wang, J. | United States | 42 | Technology for healthcare and disease management |
| 13 | Wang, W. | Singapore | 41 | Technology for healthcare and disease management |
| 14 | Zhang, Y. | China | 41 | Technology for healthcare and disease management |
| 15 | Delone, W.H. | United States | US | Analysis and adoption of hospital information system |
| 16 | Sarstedt, M. | Germany | 39 | Analysis and adoption of hospital information system |
| 17 | Zhang, J. | Singapore | 38 | Technology for healthcare and disease management |
| 18 | Li, H. | Finland | 36 | Technology for healthcare and disease management |
| 19 | Li, J. | Australia | 36 | Technology for healthcare and disease management |
| 20 | Zaidan, A.A. | Malaysia | 36 | Analysis and adoption of hospital information system |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lwin, H.N.N.; Punnakitikashem, P.; Thananusak, T. E-Health Research in Southeast Asia: A Bibliometric Review. Sustainability 2023, 15, 2559. https://doi.org/10.3390/su15032559
Lwin HNN, Punnakitikashem P, Thananusak T. E-Health Research in Southeast Asia: A Bibliometric Review. Sustainability. 2023; 15(3):2559. https://doi.org/10.3390/su15032559
Chicago/Turabian StyleLwin, Hnin Nu Nu, Prattana Punnakitikashem, and Trin Thananusak. 2023. "E-Health Research in Southeast Asia: A Bibliometric Review" Sustainability 15, no. 3: 2559. https://doi.org/10.3390/su15032559
APA StyleLwin, H. N. N., Punnakitikashem, P., & Thananusak, T. (2023). E-Health Research in Southeast Asia: A Bibliometric Review. Sustainability, 15(3), 2559. https://doi.org/10.3390/su15032559






