Predictors of Post-Traumatic Stress Symptoms in Nurses during COVID-19 Pandemic: The Role of Occupational Stressors, Personality Traits, and Availability of Protective Equipment
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
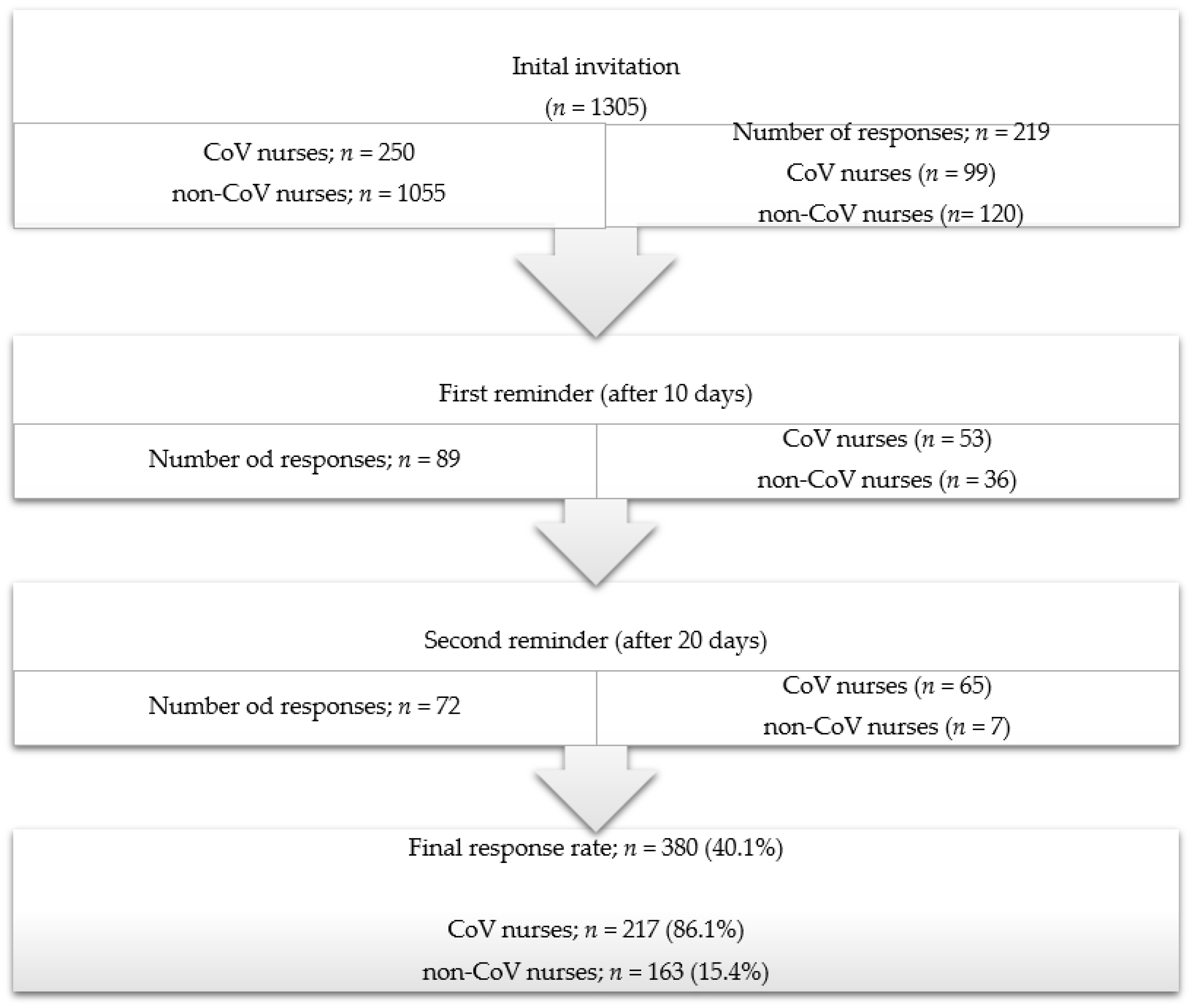
2.2. Participants
2.3. Outcomes of the Study
2.4. Study Instruments
2.4.1. Demographic Information
2.4.2. The Big Five Inventory
2.4.3. Post-Traumatic Stress Disorder Checklist (PCL-5)
2.4.4. Questionnaire on Workplace Stressors for Hospital Workers
2.5. Statistical Analysis
3. Results
3.1. Demographic Data of the Participants
3.2. Descriptive Results on the Observed Factors
3.3. Results of Multiple Regression Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dolić, M.; Antičević, V.; Dolić, K.; Pogorelić, Z. Questionnaire for assessing social contacts of nurses who worked with coronavirus patients during the first wave of the COVID-19 pandemic. Healthcare 2021, 9, 930. [Google Scholar] [CrossRef]
- Xiong, N.; Fritzsche, K.; Pan, Y.; Löhlein, J.; Leonhart, R. The psychological impact of COVID-19 on Chinese healthcare workers: A systematic review and meta-analysis. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 1515–1529. [Google Scholar] [CrossRef]
- Teo, I.; Chay, J.; Cheung, Y.B.; Sung, S.C.; Tewani, K.G.; Yeo, L.F.; Yang, G.M.; Pan, F.T.; Ng, J.Y.; Abu Bakar Aloweni, F.; et al. Healthcare worker stress, anxiety, and burnout during the COVID-19 pandemic in Singapore: A 6-month multi-centre prospective study. PLoS ONE 2021, 16, e0258866. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Lee, E.H.; Park, N.R.; Choi, Y.H. Mental health of nurses working at a government-designated hospital during a MERS-CoV outbreak: A cross-sectional study. Arch. Psychiatr. Nurs. 2018, 32, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Bassi, M.; Negri, L.; Delle Fave, A.; Accardi, R. The relationship between post-traumatic stress and positive mental health symptoms among health workers during COVID-19 pandemic in Lombardy, Italy. J. Affect. Disord. 2021, 280, 1–6. [Google Scholar] [CrossRef]
- Stafseth, S.K.; Skogstad, L.; Ræder, J.; Hovland, I.S.; Hovde, H.; Ekeberg, Ø.; Lie, I. Symptoms of anxiety, depression, and post-traumatic stress disorder in health care personnel in Norwegian ICUs during the first wave of the COVID-19 pandemic, a prospective, observational cross-sectional study. Int. J. Environ. Res. Public Health 2022, 19, 7010. [Google Scholar] [CrossRef] [PubMed]
- Shan, Y.; Shang, J.; Yan, Y.; Lu, G.; Hu, D.; Ye, X. Mental workload of frontline nurses aiding in the COVID-19 pandemic: A latent profile analysis. J. Adv. Nurs. 2021, 77, 2374–2385. [Google Scholar] [CrossRef]
- Smallwood, N.; Karimi, L.; Bismark, M.; Putland, M.; Johnson, D.; Dharmage, S.C.; Barson, E.; Atkin, N.; Long, C.; Ng, I.; et al. High levels of psychosocial distress among Australian frontline healthcare workers during the COVID-19 pandemic: A cross-sectional survey. Gen. Psychiatry 2021, 34, e100577. [Google Scholar] [CrossRef]
- Yunitri, N.; Chu, H.; Kang, X.L.; Jen, H.J.; Pien, L.C.; Tsai, H.T.; Kamil, A.R.; Chou, K.R. Global prevalence and associated risk factors of posttraumatic stress disorder during COVID-19 pandemic: A meta-analysis. Int. J. Nurs. Stud. 2022, 126, 104136. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, C.; Pan, W.; Zheng, J.; Gao, J.; Huang, X.; Cai, S.; Zhai, Y.; Latour, J.M.; Zhu, C. Stress, burnout, and coping strategies of frontline nurses during the COVID-19 epidemic in Wuhan and Shanghai, China. Front. Psychiatry 2020, 11, 565520. [Google Scholar] [CrossRef]
- Shahrour, G.; Dardas, L.A. Acute stress disorder, coping self-efficacy and subsequent psychological distress among nurses amid COVID-19. J. Nurs. Manag. 2020, 28, 1686–1695. [Google Scholar] [CrossRef] [PubMed]
- Gohar, B.; Larivière, M.; Lightfoot, N.; Wenghofer, E.; Larivière, C.; Nowrouzi-Kia, B. Understanding sickness absence in nurses and personal support workers: Insights from frontline staff and key informants in Northeastern Ontario. Work 2020, 66, 755–766. [Google Scholar] [CrossRef] [PubMed]
- Dolić, M.; Antičević, V.; Dolić, K.; Pogorelić, Z. The impact of sociodemographic characteristics on coping strategies used by nurses working at COVID and non-COVID hospital departments during COVID-19 pandemic: A cross-sectional study. Healthcare 2022, 10, 1144. [Google Scholar] [CrossRef]
- Friganovic, A.; Režić, S.; Kurtović, B.; Vidmanić, S.; Zelenikova, R.; Rotim, C.; Konjevoda, V.; Režek, B.; Piškor, S. Nurses’ perception of implicit nursing care rationing in Croatia-A cross-sectional multicentre study. J. Nurs. Manag. 2020, 28, 2230–2239. [Google Scholar] [CrossRef] [PubMed]
- Gohar, B.; Larivière, M.; Lightfoot, N.; Larivière, C.; Wenghofer, E.; Nowrouzi-Kia, B. Demographic, lifestyle, and physical health predictors of sickness absenteeism in nursing: A meta-analysis. Saf. Health Work 2021, 12, 536–543. [Google Scholar] [CrossRef]
- Crocamo, C.; Bachi, B.; Calabrese, A.; Callovini, T.; Cavaleri, D.; Cioni, R.M.; Moretti, F.; Bartoli, F.; Carrà, G. Some of us are most at risk: Systematic review and meta-analysis of correlates of depressive symptoms among healthcare workers during the SARS-CoV-2 outbreak. Neurosci. Biobehav. Rev. 2021, 131, 912–922. [Google Scholar] [CrossRef] [PubMed]
- Ding, S.; Deng, S.; Zhang, Y.; Wang, Q.; Liu, Z.; Huang, J.; Yang, X. Experiences and needs of front-line nurses during the COVID-19 pandemic: A systematic review and qualitative meta-synthesis. Front. Public Health 2022, 10, 805631. [Google Scholar] [CrossRef]
- Gómez-Urquiza, J.L.; De la Fuente-Solana, E.I.; Albendín-García, L.; Vargas-Pecino, C.; Ortega-Campos, E.M.; Cañadas-De la Fuente, G.A. Prevalence of burnout syndrome in emergency nurses: A meta-analysis. Crit. Care Nurse 2017, 37, e1–e9. [Google Scholar] [CrossRef]
- Hickling, M.T.; Barnett, S.D. Psychological impact of COVID-19 on nursing personnel: A regional online survey. J. Adv. Nurs. 2022, 78, 3025–3033. [Google Scholar] [CrossRef]
- Dolić, M.; Antičević, V.; Dolić, K.; Pogorelić, Z. Difference in pandemic-related experiences and factors associated with sickness absence among nurses working in COVID-19 and non-COVID-19 departments. Int. J. Environ. Res. Public Health 2022, 19, 1093. [Google Scholar] [CrossRef]
- Warshaw, E.M.; Schlarbaum, J.P.; Silverberg, J.I.; DeKoven, J.G.; Maibach, H.I.; Sasseville, D.; Fowler, J.F., Jr.; Marks, J.G., Jr.; Belsito, D.V.; Reeder, M.J.; et al. Safety equipment: When protection becomes a problem. Contact Dermat. 2019, 81, 130–132. [Google Scholar] [CrossRef]
- Simonovich, S.D.; Aquino, E.; Lattner, C.; Soco, C.; Ponder, T.N.; Amer, L.; Howard, S.; Nwafor, G.; Shah, P.; Badowski, D.; et al. US nurses’ challenges with personal protective equipment during COVID-19: Interview findings from the frontline workforce. Psych 2022, 4, 226–237. [Google Scholar] [CrossRef]
- World Health Organization. Shortage of Personal Protective Equipment Endangering Health Workers Worldwide; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- John, O.P.; Donahue, E.M.; Kentle, R.L. The Big Five Inventory—Versions 4a and 54; University of California, Berkeley, Institute of Personality and Social Research: Berkeley, CA, USA, 1991. [Google Scholar]
- Kardum, I.; Gračanin, A.; Hudek-Knežević, J. Dimenzije ličnosti i religioznost kao prediktori socioseksualnosti kod žena i muškaraca. Druš. Istraž. 2008, 17, 505–528. [Google Scholar]
- Ito, M.; Takebayashi, Y.; Suzuki, Y.; Horikoshi, M. Posttraumatic stress disorder checklist for DSM-5: Psychometric properties in a Japanese population. J. Affect. Disord. 2019, 247, 11–19. [Google Scholar] [CrossRef]
- Milošević, M.G.R.; Mustajbegović, J.; Knežević, B.; Juras, K.; Bubaš, M. Validacija upitnika o stresorima na radnom mjestu bolničkih zdravstvenih djelatnika. Sigurnost 2009, 51, 75–84. [Google Scholar]
- Rajčáni, J.; Vytykačová, S.; Botíková, V.; Šuhajdová, B. Predictors of traumatic stress in nurses during the COVID-19 pandemic. Československá Psychol. 2022, 66, 17–29. [Google Scholar] [CrossRef]
- Si, M.Y.; Su, X.Y.; Jiang, Y.; Wang, W.J.; Gu, X.F.; Ma, L.; Li, J.; Zhang, S.K.; Ren, Z.F.; Ren, R.; et al. Psychological impact of COVID-19 on medical care workers in China. Infect. Dis. Poverty 2020, 9, 113. [Google Scholar] [CrossRef]
- Bohlken, J.; Schömig, F.; Lemke, M.R.; Pumberger, M.; Riedel-Heller, S.G. COVID-19 pandemic: Stress experience of healthcare workers—A short current review. Psychiatr. Prax. 2020, 47, 190–197. [Google Scholar]
- Steudte-Schmiedgen, S.; Stieler, L.; Erim, Y.; Morawa, E.; Geiser, F.; Beschoner, P.; Jerg-Bretzke, L.; Albus, C.; Hiebel, N.; Weidner, K. Correlates and predictors of PTSD symptoms among healthcare workers during the COVID-19 pandemic: Results of the egePan-VOICE study. Front. Psychiatry 2021, 12, 686667. [Google Scholar] [CrossRef]
- Carmassi, C.; Foghi, C.; Dell’Oste, V.; Cordone, A.; Bertelloni, C.A.; Bui, E.; Dell’Osso, L. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: What can we expect after the COVID-19 pandemic. Psychiatry Res. 2020, 292, 113312. [Google Scholar] [CrossRef]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Ge, J.; Yang, M.; Feng, J.; Qiao, M.; Jiang, R.; Bi, J.; Zhan, G.; Xu, X.; Wang, L.; et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. 2020, 88, 916–919. [Google Scholar] [CrossRef] [PubMed]
- Pogorelić, Z.; Anand, S.; Artuković, L.; Krishnan, N. Comparison of the outcomes of testicular torsion among children presenting during the Coronavirus Disease 2019 (COVID-19) pandemic versus the pre-pandemic period: A systematic review and meta-analysis. J. Pediatr. Urol. 2022, 18, 202–209. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Anand, S.; Žuvela, T.; Singh, A.; Križanac, Z.; Krishnan, N. Incidence of complicated appendicitis during the COVID-19 pandemic versus the pre-pandemic period: A systematic review and meta-analysis of 2782 pediatric appendectomies. Diagnostics 2022, 12, 127. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Milanović, K.; Veršić, A.B.; Pasini, M.; Divković, D.; Pavlović, O.; Lučev, J.; Žufić, V. Is there an increased incidence of orchiectomy in pediatric patients with acute testicular torsion during COVID-19 pandemic?—A retrospective multicenter study. J. Pediatr. Urol. 2021, 17, 479.e1–479.e6. [Google Scholar] [CrossRef] [PubMed]
- Lange, S.J.; Ritchey, M.D.; Goodman, A.B.; Dias, T.; Twentyman, E.; Fuld, J.; Schieve, L.A.; Imperatore, G.; Benoit, S.R.; Kite-Powell, A.; et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions—United States, January–May 2020. Am. J. Transplant. 2020, 69, 795–800. [Google Scholar]
- Arnetz, J.E.; Goetz, C.M.; Sudan, S.; Arble, E.; Janisse, J.; Arnetz, B.B. Personal protective equipment and mental health symptoms among nurses during the COVID-19 pandemic. J. Occup. Environ. Med. 2020, 62, 892–897. [Google Scholar] [CrossRef]
- Galanis, P.; Vraka, I.; Fragkou, D.; Bilali, A.; Kaitelidou, D. Impact of personal protective equipment use on health care workers’ physical health during the COVID-19 pandemic: A systematic review and meta-analysis. Am. J. Infect. Control 2021, 49, 1305–1315. [Google Scholar] [CrossRef]
| Variable | SD | |
|---|---|---|
| Stigmatization and misunderstanding | 3.698 | 0.946 |
| Social distancing | 3.229 | 0.874 |
| Fear of infection | 3.995 | 0.943 |
| Extraversion | 3.736 | 0.562 |
| Comfort | 4.089 | 0.505 |
| Conscientiousness | 4.328 | 0.504 |
| Neuroticism | 2.266 | 0.712 |
| Openness | 3.513 | 0.489 |
| PCL-5 in total | 24.861 | 16.082 |
| Public criticism | 3.379 | 1.070 |
| Dangerous and harmful conditions at work | 3.012 | 1.019 |
| Conflicts and communication at work | 3.282 | 1.056 |
| Shift work | 3.615 | 1.089 |
| Professional and intellectual requirements | 3.331 | 0.981 |
| Predictors | B | β | t | p |
|---|---|---|---|---|
| (Constant) | −24.367 | −2.891 | 0.004 | |
| BFI-Extraversion | −5.016 | −0.175 | −4.234 | 0.000 |
| BFI-Agreeableness | −0.162 | −0.005 | −0.112 | 0.911 |
| BFI-Conscientiousness | 0.566 | 0.018 | 0.375 | 0.708 |
| BFI-Neuroticism | 12.328 | 0.546 | 12.339 | 0.000 |
| BFI-Openness | 6.151 | 0.187 | 4.450 | 0.000 |
| Public criticism | 2.374 | 0.158 | 3.081 | 0.002 |
| Dangers and harms at work | −1.987 | −0.126 | −2.464 | 0.014 |
| Conflicts and communication at work | 3.830 | 0.251 | 5.641 | 0.000 |
| Shift work | 0.065 | 0.004 | 0.104 | 0.917 |
| Professional and intellectual work demands | 1.035 | 0.063 | 1.378 | 0.169 |
| Worked in a COVID-19 department during the pandemic | −2.888 | −0.089 | −2.578 | 0.010 |
| Pandemic-Related Stressors | Direct Effects on Criterion | Indirect Effects on Criterion | Total Effects | |
|---|---|---|---|---|
| (SE) | 95% CI | (95% CI) | (SE) | |
| Stigmatization and misunderstanding | 4.421 (0.843) | 2.764–6.078 | −0.1360 (−0.469–0.090) | 4.421 (0.843) |
| Social distancing | 6.748 (0.878) | 5.022–8.473 | 0.079 (−0.108–0.356) | 6.748 (0.878) |
| Fear of infection | 3.112 (0.861) | 1.419–4.806 | 0.109 (−0.072–0.414) | 3.112 (0.861) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dolić, M.; Antičević, V.; Dolić, K.; Pogorelić, Z. Predictors of Post-Traumatic Stress Symptoms in Nurses during COVID-19 Pandemic: The Role of Occupational Stressors, Personality Traits, and Availability of Protective Equipment. Sustainability 2023, 15, 9555. https://doi.org/10.3390/su15129555
Dolić M, Antičević V, Dolić K, Pogorelić Z. Predictors of Post-Traumatic Stress Symptoms in Nurses during COVID-19 Pandemic: The Role of Occupational Stressors, Personality Traits, and Availability of Protective Equipment. Sustainability. 2023; 15(12):9555. https://doi.org/10.3390/su15129555
Chicago/Turabian StyleDolić, Matea, Vesna Antičević, Krešimir Dolić, and Zenon Pogorelić. 2023. "Predictors of Post-Traumatic Stress Symptoms in Nurses during COVID-19 Pandemic: The Role of Occupational Stressors, Personality Traits, and Availability of Protective Equipment" Sustainability 15, no. 12: 9555. https://doi.org/10.3390/su15129555
APA StyleDolić, M., Antičević, V., Dolić, K., & Pogorelić, Z. (2023). Predictors of Post-Traumatic Stress Symptoms in Nurses during COVID-19 Pandemic: The Role of Occupational Stressors, Personality Traits, and Availability of Protective Equipment. Sustainability, 15(12), 9555. https://doi.org/10.3390/su15129555







