Abstract
The continuous expansion of the nursing scope of practice, the undeniable growth of the nurses’ role in the healthcare crisis, the shortage of labor, especially in rural areas and marginalized urban csommunities, and last but not least, the lack of literature on Romanian nursing autonomy are some of the background factors in this study. This study’s purpose is to assess nurses’ perceptions of their medical care independence. The main hypothesis is that more advanced levels of education generate a greater inclination toward autonomous interventions. The quantitative research is based on a survey using a self-designed questionnaire as a tool (based on a nurse-focused structure and process indicators following the Donabedian model) applied in a Romanian clinical hospital. Based on a literature review, three composite indicators were developed and tested for reliability using the Cronbach alpha coefficient. These indicators reflect autonomy from three perspectives: clinical practice independence, autonomy in relation to work, and autonomy through digitalization. This scientific approach revealed a major impact of the regulatory framework on nurses’ perceptions of their autonomy, below the expectations of use, and the acceptance of digital technologies among nurses. Finally, it was observed that college graduate nurses perceive lower levels of independence than post-secondary ones.
1. Introductions
The International Year of the Nurse and Midwife—Florence Nightingale’s date of birth bicentenary, 2020—was profoundly marked by the fight against the COVID-19 pandemic. At that time, the too-often veiled role and the ever-increasing complexity of nurses’ duties came to light. As shown below, in crisis situations, nurses assume more responsibilities, autonomy, and, consequently, more risks. Yet, the line of demarcation between autonomous and delegated nursing interventions is not uniformly established. It differs from one country to another and from urban to rural areas, and it depends on the nurses’ education and professional training, legislation, institutional procedures, interpersonal relations, etc. Against the background of nurses’ expanding role, research on factors affecting their autonomy is gaining increasing importance. This is a time when nurse-led care models are promoted as a means of compensating for the lack of physicians in rural areas and marginalized urban communities. This study is important for a better understanding of the extent to which Romanian nurses are capitalizing on their full professional potential, acting at their full scope of practice, and wishing to pursue these two goals through higher autonomy.
Our purpose is to assess Romanian nurses’ perceptions of their autonomy and advocate for the recognition of their central role in the healthcare system. A more advanced level of education generates a greater inclination toward autonomous activities: this is our main hypothesis. This study aims to compensate for the scarcity of research that uses nursing-focused process indicators. Our scientific interest is focused on continuous nursing education and professional training (including capitalizing on the advantages of digitalization) as means of gaining more clinical and work-related autonomy. The innovative component is the system of autonomy-related indicators designed and applied as a questionnaire in a Romanian clinical hospital.
Literature review. Worldwide, in 2018, nurses amounted to 27.9 million, being the most important occupational group among health professionals (59%). There are significant differences between regions in terms of the average densities of practicing nurses and nursing graduates. The Americas lead the world ranking by far, especially when it comes to the number of university degree holders. Regional gaps are even more obvious if reported according to income levels. The relatively small number of graduates in high-income countries (compared to nurse density per capita) is mainly driven by labor migration from low-income countries [1].
Romania is one of the few countries in the European Union (EU) with limited staffing capacity for both practicing doctors and nurses. Romania reported approximately 3.1 doctors per 1000 population, below the EU average of 3.8, and 7.2 nurses per 1000 population, compared to an average of 8.2 in the EU. In Europe, Norway benefits from the highest density of nurses (17.7 per 1000 population) [2]. In Romania, the ratio of nurses to doctors was 2.4 in 2018, compared to an average of 2.3 in the EU, with Finland in the top ranking with an average of 4.4 nurses for each doctor [2,3]. In 2021, Romania’s ratio of nurses to doctors decreased to 2.3 [3]. It is stated that the poor availability of nurses has a negative impact on the resilience of the public health system. Hence, nurses should play a more important role both at the organizational decision-making level and at the national one by contributing to the conceptualization of nursing policies [2].
Nurses’ role. The nurses’ critical role in direct care and health status monitoring under safe conditions is highlighted [4]. In addition to their role in the prevention and treatment of a whole series of ailments, nurses have an essential role in monitoring the patient’s condition, reporting medical errors, perceiving the weaknesses of the health system, and responding to medical emergencies, epidemics, disasters, or humanitarian crises. Moreover, nurse-led primary care services sometimes lead to better outcomes than other models of care. The existence of advanced practice roles in nursing contributes to the increasing access of vulnerable (especially rural) and urban marginalized populations to primary healthcare. This is only possible when nurses are encouraged to practice at their full scope of practice. In this way, nurses develop into a means of ensuring universal access to healthcare services [5,6,7,8,9,10]. In Romania, 92.1% of doctors (excluding dentists) and 96.6% of nurses with higher education worked in urban areas in 2021. Of the total number of health personnel with secondary education, 89.4% practiced in urban areas [11].
Nurses’ holistic knowledge of the patient allows for the swift identification of medical care’s adverse effects. Guided by their moral obligations, nurses have an important role in reporting medical errors, and advanced practice registered nurses (APRNs) were found to be more inclined to communicate such errors [12].
Nurses believe that the presence of motivational factors such as better working conditions or salary incentives could create the basis for taking on more responsibilities, even those traditionally reserved for physicians [13]. The progressive shift from physician-led to nurse-led medical care models accelerated during the COVID-19 pandemic in different countries, where a series of strategies and regulations were adopted to recognize nurses’ critical role [14]. As nurses assumed additional responsibilities in times of crises, it becomes obvious that specialized education and training is imperative [15].
In Romania, the nurse’s role is described by Law No. 278/2015. Provisions related to independent nursing interventions appear, with insufficient clarity, in establishing the patient’s need for nursing care, in performing quality analysis to improve professional practice, and in crisis/disaster situations. Actually, it is a proven fact that high-risk conditions impart more professional autonomy to a nurse. On the other hand, the previously mentioned Law clearly states that “protecting and improving health” is to be performed “by administering the treatment according to the doctor’s prescriptions” [16]. In Poland, the latest legislative changes offer nurses the opportunity to carry out independent activities in many health areas [17]. In addition, in this country, amid the more and more common appearance of burnout, researchers are finding that nurses perceive that management positions provide better work conditions [18].
The importance of the nurses’ role and the clarity of its definition in the US is noted [14]. Not coincidentally, in the US, the nursing profession ranked first in terms of ethics and honesty for the 20th consecutive year [19]. At the opposite pole, Romanian hospitals managed to grasp the last place in the population’s confidence, with a percentage of only 15% [20].
Autonomy. In contrast to Isabel Hampton Robb’s (early leader of nursing education) opinion that a nurse is just a physician’s subservient who has to “remember to do what she is told to do, and no more…”, Florence Nightingale advocated for educated nurses, and she envisioned their further expanding role and autonomy [21]. The nursing profession “has evolved from total dependence, to autonomy and independence...” [22]. Autonomy can be defined as the nurse’s freedom to act in accordance with her/his professional training. However, autonomy depends not only on the individual but also on the complex and dynamic decision-making framework established within the health unit and/or at the government level. The world is going through a period of transition characterized by the development and highlighting of the leadership component in nursing [23], even if this profession was not initially regarded as self-standing. In Japan, all nurses are expected to be able to think and act independently [24].
Autonomy takes two distinct forms, namely, clinical practice autonomy and autonomy in relation to work. The characteristics of working conditions can be grouped into several categories, among which autonomy occupies an important place alongside nurse participation, supportive managers, collaborative relationships with physicians, decentralization, etc. [25]. The most attractive working conditions (expressed through increased labor stability) are found in so-called “magnet hospitals”, where better results for patients are reported [26,27,28]. The main findings of studies carried out in such hospitals show that autonomy, an appropriate level of staffing, and the quality of professional relationships have become standards of good practice. The need for future research on correlations between nursing autonomy, the extent to which this autonomy is supported by nurse managers, and the way physicians encourage/disapprove of independence is emphasized [27]. Studies on working conditions in “magnet hospitals” show that autonomy is a key factor affecting the quality of medical care. Nurses practicing in such hospitals benefit from greater autonomy and higher job satisfaction. Licensed nurses have better outcomes due, in part, to an increased willingness to exercise decision-making authority in patient care [29]. To this end, “nurses should be fully supported with robust education, resources, and autonomy” [10].
Evidence shows that countries with fewer physicians have more APRNs. It follows that nurses’ autonomy increases as, through public policies, solutions are sought to counteract the shortage of physicians. This calls for additional nurse-managed health centers [30]. In certain countries, investments are being made to increase the number of APRNs. In others, public policies generate the replacement of advanced-education employees with nurses having less professional training and, consequently, lower salaries. This happens despite the fact that, as is demonstrated, education and autonomy show negative correlations with indicators such as the mortality rate in the first 30 days after admission and Failure to Rescue (FTR) [29,31]. On the other hand, it was found that in medical units promoting nurses’ autonomy, there is greater job satisfaction, a lower probability of burnout and compassion fatigue syndromes, higher staffing stability, better teamwork, and increased healthcare quality. Poor working conditions and a lack of proper furnishing, cleaning, and equipment are factors negatively affecting job satisfaction in Romanian hospitals [32].
Thus, for a nurse, autonomy can be defined as the ability to implement professional knowledge for the patient’s benefit and to make decisions destined to increase the quality of healthcare services. One way of expressing autonomy is independence. Yet, one of the literature’s main findings is that the concept of autonomy in nursing is insufficiently clarified [33,34,35,36].
Education. The duration of schooling and curricula differ geographically, with most countries having their own standards. Commonly, the minimum duration is three years, while the Americas benefit from the highest percentage of graduates with five-year degrees. Advanced studies (master’s, doctoral, and postdoctoral degrees) call for new curricula, specialized teaching staff, research components focused on critical thinking, and, last but not least, a prepared health system to capitalize on such skills. It is found that nurses with four years of education are significantly more able to identify medical emergencies [37]. Patients cared for by licensed nurses have lower mortality rates, shorter hospital stays, and, consequently, lower care expenditures. An expanding scope of practice is closely correlated with the skills acquired through education. Although, since the beginning of the pandemic, research nurses have contributed numerous practical solutions, a lack of nurse-led studies related to COVID-19 has been noted.
Continuous professional training allows nurses to grow independently through reflection [24]. Nurses are facing challenges with an aging population, a decrease in the birth rate, the development of medical technologies, changes in the manifestations of diseases, patients’ increasing awareness of their legal rights, and more restrictive malpractice regulations. Therefore, there is a need for increased skills and, consequently, for a growing number of nursing universities with diversified and flexible curricula adapted to the new conditions imposed by the pandemic [10,24,38]. The education system should train nurses “to respond autonomously to the problems of an individual” [39].
The American Association of Colleges of Nursing (AACN) has developed common core curricula and identified the competencies required for baccalaureate, master’s, Doctor of Nursing Practice (practice-focused), and PhD degrees in nursing (research- and education-focused) [40]. In the EU, the process of harmonizing nursing degrees and the university curricula began at the end of the 1970s. Currently, a standard set of nursing competencies is defined [41], but the provision of eHealth services raises new issues related to professional qualifications such as the integration of digital skills and the use of digital technologies in nursing education [38].
In Romania, the multi-annual Strategy for the Development of Healthcare Human Resources 2022–2030 (Government Decision No. 854/2022) recognizes the need to update undergraduate and graduate education based on competencies (Direction of Action 6.3.). Subsumed to this desire, there is a need to “Reform the nurses’ … training process” (Specific Objective 6.3.3.) [42]. From this perspective, a particularly relevant indicator, not found in the reviewed literature, could be the ratio of nursing graduate professors to medical graduate professors in nursing education. This indicator could provide valuable information regarding the importance given to the nursing profession in the academic environment and beyond.
Romania has the lowest ratio of nursing professionals to nurses (0.11 in 2020) due, mainly, to a very low number of nursing professionals (82 per 100,000 population) [43]. In 2021, this ratio improved slightly (to 0.13) [3], but it is still very far from the optimal unit ratio, when all nurses are professionals who “assume responsibility for the planning and management of the care of patients, including the supervision of other health care workers, working autonomously or in teams with medical doctors and others in the practical application of preventive and curative measures” [44]. At the same time, in 2020, Romania benefited from an impressive number of nursing graduates (99.95 graduates per 100,000 population), being exceeded only by Switzerland (111.88) [45]. The corroboration of the two statistics reveals the truth about nurses’ migration from Romania to countries where their true value is recognized. It is no less true that Romania had the lowest number of professional nursing graduates per 100,000 population among European countries.
Regulation. Amid the diversification of nursing curricula and the increase in the number of medical specialties, nurses’ autonomy calls for an increasingly robust regulatory framework. This framework and proper training on legislation should enable nurses to act to their full scope of practice [46]. The National Council of State Boards of Nursing, through the Global Regulatory Atlas, identifies at least 144 nurse categories worldwide [47]. In the US, according to the National Council of State Boards of Nursing, APRNs assess, diagnose, and manage patients’ medical problems, order tests, and prescribe medications (as of January 2021, in 23 US states) [48]. However, in 27 US states, nurse practitioners do not have full practice authority [10]. The staffing structure in medical centers and nurses’ turnover by education degree are also regulation-dependent. Further research is needed to assess the impact of legislation on APRNs’ teamwork.
Nursing regulation characteristics are influenced by the presence, at the government level, of a chief nurse position to promote leadership programs and APRNs’ involvement at all decision-making levels, on equal footing with other healthcare employees. Countries in North America and Western Europe benefit from better-defined regulatory systems [1]. It is noted that there is still a long way to go until the legislation will enable nurses to act to their full scope of practice [1,10]. Most countries have an institution responsible for nursing regulation. In Romania, the Ministry of Health has no specialized commission in nursing; the Order of Nurses and Midwives of Romania is the regulatory body. In the Republic of Moldova, the Ministry of Health, Labor and Social Protection, by Order 867/2020, provided for the existence of the Nursing Commission [49].
Scope-of-practice regulations can limit the healthcare efficiency growth afforded by the full capitalization of nurses’ knowledge potential [50]. The nursing regulation diversity and complexity generated a scarcity of literature studying its impact on nurse autonomy.
The American Association of Nurse Practitioners classifies the states into states with independent practice and prescriptive authority; states where a collaborative agreement with a physician is required for at least one of the independent activities; and states that only allow physician-delegated activities [7]. It was found that, in the US, states that grant more authority by expanding the scope of practice have seen increases in nurse densities per capita. In these states, both the interest in professional training (30% increase in enrolments in advanced education programs for the right to independent practice and 13% increase in prescriptive authority) and the availability to practice in rural areas (by 1.5 times) have increased.
Digitalization. The literature focuses mainly on two directions. The first refers to digital technology categories and how these technologies help decision making in nursing [51]. For example, eHealth platforms enable the objective assessment of severity and the real-time identification of the most affected communities according to the speed and propagation patterns of different pandemics. Information and Communication Technologies (ICTs) are also used to monitor various chronic and/or rare diseases. Although nurses are among the main users of digital platforms, they are rarely asked to participate in their design. The second research direction considers the benefits of/barriers to using ICTs [1,52,53,54,55,56,57]. The COVID-19 pandemic has contributed substantially to overcoming these limitations. The need for social distancing, the reduction in unnecessary exposures to infections, and the lack of personal protective equipment required new solutions to promote eHealth.
For several decades, APRNs have been playing a central role in eHealth services in countries such as Finland and the US [38,58]. Through their experience in using digital technologies and knowledge on governing regulations, APRNs can strengthen their leadership role in education and health systems. As early as 1992, the American Nurses Association (ANA) established the specialization in nursing informatics, and since 1995, the American Nurses Credentialing Center (ANCC) has granted a certificate in nursing informatics [57]. More and more used in the educational system, virtual reality brings nurses closer to the concepts of leadership, communication, decision-making systems, critical thinking, inclusivity, health appraisal, and disaster triage [59]. In other countries, although nursing education has remained unchanged for over half a century, the pandemic forced the entry of modern technologies [60]. From this perspective, Romania was, in 2018, in last place in Europe regarding the use of computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET), with only 38 such investigations per 1000 population (while the EU average was 204) [2].
Regulations aimed at expanding the scope of practice and the rapid development of eHealth in response to the pandemic have allowed nurses to carry out their work to the full extent of their education and professional training.
Autonomy is a very important component of work conditions and a means of transforming nursing resources into high-quality medical services. However, the impact of ICTs on nurses’ autonomy is scarcely mentioned in the dedicated literature. Hence, there is a need for an in-depth assessment of the impact of ICTs on autonomy and, consequently, the mandatory inclusion of ICT skills in the nursing curricula [10,58,61,62,63] because, as long as the medical education system fails to keep up with the evolution of digital technologies, we will not be able to accurately measure the extent to which these technologies affect nurses’ autonomy.
Nursing-Sensitive Indicators (NSIs). A 1997–2017 systematic literature review contains mostly articles developed in the US (74%), 69% of which include applications for general hospitals [31]. The ambiguous, even elusive character of many NSIs poses important problems in their classification, use, and interpretation. Research is focused on analyzing the categories, content, and utility of NSIs, starting from Donabedian’s model. The Donabedian model of the knowledge, evaluation, and improvement of healthcare quality studies the dynamic cycle of interdependencies between the healthcare structure, processes, and results, attaching a distinct series of indicators to each of the three components [64,65].
The structural component includes variables related to patients or nurses (number, density per patient, skill level, and professional experience) and the organizational characteristics of the health facility/system (work schedule and environment and autonomy granted to nurses). The process indicators consider autonomous, delegated, and interprofessional activities (nursing/intervention-focused). These indicators strictly pertain to medical acts, namely, treatment and care procedures, pain management, the maintenance of skin, integrity, and patient education. In addition, process indicators can be divided into two categories. The first includes nursing-related indicators (any intervention based on the nurse’s judgment and knowledge to improve the patient’s condition). The second is work-related and considers nursing care plan development procedures [66]. Finally, results indicators describe changes in the nurse or patient status. Nurse-focused indicators include nurses’ job satisfaction, nurse-reported quality of care, nurse burnout, nurse turnover, etc. [31]. Still, it is obvious that, among results indicators, the most frequently used are patient-focused indicators.
NSIs can also be categorized according to four other coordinates: the nursing practice environment; nurses’ education level and skills; hospital structure/setting; and nurse models/nurse organization [67].
The radical changes imposed by the pandemic required the adaptation of NSI systems and the review of nurse responsibilities [14]. Over time, the Donabedian model was enriched with a whole series of variables specific to nursing activity, leading to the creation of the Nursing Role Effectiveness Model [68]. In this model, the structural variables include aspects of nurse independence. The performance achieved by expressing an autonomous role is quantified using indicators that reflect the patient’s perception of healthcare quality. The interprofessional role performance is estimated based on the nurse’s perception of communication and coordination quality in care activities [69]. Particularly important is that results indicators (including the costs incurred by the adoption of a certain care plan) are divided according to the type of role (autonomous, delegated, or interprofessional) [70,71]. Similarly, process indicators differ according to the role they describe: autonomous (triage and assessment activities, self-care assistance, addiction management, and patient education), delegated (coordination of care, assessment of treatment response, medication administration, and use of clinical judgment), or interprofessional (quality of communication and coordination of the care process).
The World Health Organization [1] analyzes nursing performance using indicators drawn from the National Health Workforce: A Handbook [72]. The autonomy indicators are “national chief nurse (or equivalent) role”; “national leadership development opportunities”; and “existence of advanced nursing roles (nurse practitioner/advanced practice nurse)”.
Nurses’ autonomy can be assessed using the Clinical Nursing Competence Self-Assessment Scale, which includes “coordinating care environment and teamwork” indicators such as “risk management”, “care coordination”, and “nursing management/fulfillment roles” [24].
The Nursing Care Performance Framework is a network of indicators reflecting three subsystems (nursing resources, nursing services, and patients’ conditions) to assess the impact of ICTs on nursing performance indicators [61].
One of the most used indicator systems for analyzing nurses’ working environment [25,27,29] is the Nursing Work Index (NWI), developed in 1989 in the US and based on research carried out in a “magnet hospital”. The system was continuously adapted (NWI-Revised), with most of the questionnaires being applied in hospitals using the Likert scale. NWI-R contains 57 items grouped into four theoretical categories: control over practice, autonomy, doctor–nurse relationship, and organizational support.
Slater et al. and Rao et al. [27,29] used five NWI-R items to create an autonomy subscale. Common indicators used in both studies include “nursing controls its own practice”, “freedom to make important patient care and work decisions”, and “not being placed in a position of having to do things that are against my nursing judgment”. In addition to these three common items, Slater et al. chose two more: “managerial staffs are supportive of nurses” and “a nurse manager backs up the nursing staff in decision making, even if the conflict is with a doctor”. Rao et al. selected other additional indicators to evaluate autonomy: “support for new and innovative ideas about patient care” and “involvement of staff nurses in the internal governance of the hospital”. The questionnaire responses were aggregated at the hospital level and then averaged to obtain a hospital-level autonomy score.
A healthcare system’s performance analysis based on NSIs helps establish a scientific basis for a correct and autonomous decision-making process. NSIs are useful for conducting research on the nurses’ role throughout all structure–process–result interdependencies. However, it is noted that NSIs measure predominantly nursing failures, and less so their positive impacts. The explanation follows logically from the available statistical information in medical records [4]. A very limited number of studies target nurse-focused outcomes. Furthermore, the scarcity of studies on nursing-focused processes/interventions, especially those aimed at patient care models, stands out. The lack of standards on nursing processes’ evaluation, the absence of an integrated understanding of these processes, and the rarity of process–result interdependency studies are highlighted [66]. In fact, Donabedian himself wrote, 55 years ago, that research should move from understanding the quality of the medical process to understanding the medical process itself [73]. It was too early yet for him to predict the impact of digitalization, its risks, and its opportunities for the healthcare system [74].
The main aim of this study is to assess nurses’ independence in Romania while understanding autonomy as a whole and as a tridimensional concept made of clinical practice independence, autonomy in relation to work, and autonomy through digitalization. In close correlation with theoretical support, the specific objectives aim, on the one hand, to determine the influence of education on autonomy and, on the other hand, to assess the degree of the acceptance of, use of, and interest in eHealth applications. Based on the established objectives and the reviewed literature, the following hypotheses were formulated: nurses appreciate that they have a moderate degree of autonomy in their clinical practice; the level of education in nursing is a determining factor affecting the perception of autonomy in relation to work; and the integration of digital applications in current practice is insufficient.
One of our main conclusions is that, besides the level of education, which clearly influences the perceived degree of clinical autonomy, professional experience is a key factor to consider. Regarding autonomy in relation to work, future studies should study whether work conditions meet the expectations of college graduates. These studies would explain the relatively low score given by undergraduate nurses to this category of autonomy. Of great importance is to assess the ability of nursing universities to provide their graduates with the theoretical and practical knowledge necessary to carry out safe autonomous activities. We also found that the use and acceptance of digital technologies scored lower than anticipated, hence the need for digitalization policies to raise awareness of the benefits and to counter lagging behind developed states. The major impact of regulation and managerial attitude toward autonomy should be emphasized. Our research, carried out in a Romanian clinical hospital, revealed that college graduates represent, contrary to the initial assumptions, the nurse category with the lowest score of professional autonomy perception.
2. Materials and Methods
Between August and October 2022, a questionnaire-based survey was conducted among nurses from the cardiology, urology, internal medicine, day hospitalization, and oncology wards of the Clinical Hospital “Prof. Dr. Theodor Burghele”, Bucharest. The questionnaire was delivered in person along with informed consent forms and details about the main aims of the study.
The questionnaire was developed using the NWI-R indicators applied by Slater et al. and Rao et al., and additional process items of our own conception, to capture nurses’ perceptions of their autonomy. The first section of the questionnaire comprises structural indicators on the respondents’ age, gender, net monthly income (including increments), and level of education in nursing. As a result of the selective research, 65 questionnaires were returned, accounting for 81.3% of those distributed. Data preprocessing for analysis and the conversion of analog to digital responses were accomplished using Microsoft Excel. The second part of the questionnaire comprises 12 nursing process items using a four-point Likert scale. For these items, respondents evaluated each question using one of the following statements: “Very true” (score = 4), “Rather true” (score = 3), “Rather untrue” (score = 2), and “Completely untrue” (score = 1) or “Very satisfied” (score = 4), “Rather satisfied” (score = 3), “Rather dissatisfied” (score = 2), and “Completely dissatisfied” (score = 1) [75,76].
Missing data in Likert-scale questionnaires are handled in different ways, including imputing and filling in missing responses based on the occurrence frequency of an expected response or deleting unanswered questions. Missing data can be divided into three categories based on their random distribution: missing at random (MAR), missing completely at random (MCAR), and missing non-ignorable data (MNAR) [77]. The objective analysis revealed that missing values were at random, with no correlation between the frequency of the occurrence of blank questions, so a total of 15 questionnaires were excluded from our analysis. As a result, 50 valid questionnaires were used for further analysis.
The grouping of items using a Likert scale into composite variables generally requires a step-by-step methodology, beginning with an internal consistency evaluation and then regrouping the composite variables’ items to maximize the Cronbach alpha internal consistency coefficient [78]. The Cronbach alpha coefficient for each of the three proposed composite variables is determined using the next formula:
where N represents the number of items considered for the construction of a new composite variable, is the average inter-item covariance, and is their average variance.
Usually, a Cronbach alpha coefficient exceeding 0.07 supports the reliability of internal consistency, but this coefficient is extremely sensitive if composite indicators include a smaller number of items—less than 10 [79]. Recent studies [80,81] show that a Cronbach alpha of 0.5–0.6 may be an acceptable threshold in these circumstances, given that the average inter-item correlation ranges between 0.15 and 0.5 [82].
Our research illustrates autonomy in clinical practice, in relation to work, and in the use and acceptance of digital healthcare technologies. The methodology described above was used to group the 12 process items of the questionnaire into three distinct composite variables (Table 1).

Table 1.
Grouping nurses’ asutonomy questionnaire items into composite variables.
The Cronbach alpha reliability coefficient analysis, the model viability assessment, and descriptive statistics were performed in IBM SPSS Statistics for Windows, Version 27.0 [83].
3. Results
More than half of the respondents fall between the ages of 36 and 50, the majority of the studied population is female, and 96% of respondents have revenues between 3000 and 5000 RON (USD 600 and USD 1000) per month. As to the respondents’ levels of education, a certain state of balance (23 respondents with higher education and 27 with post-secondary education) is noted. The sample contains 34% college undergraduates, 8% master’s degree holders, and 4% PhD graduates. Figure 1 depicts the distribution of the 50 respondents based on the above-mentioned structural criteria.
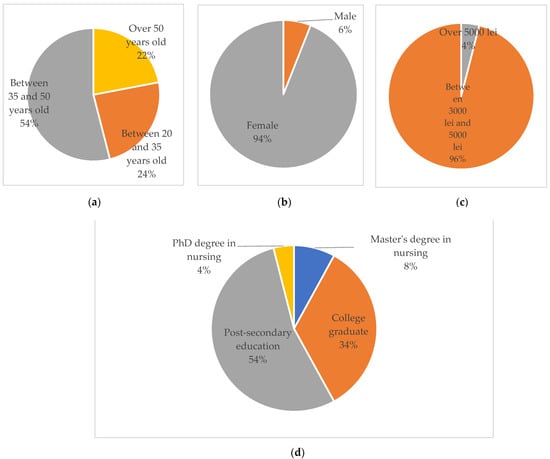
Figure 1.
Distribution of the sample population, after checking the validity of the questionnaires, based on the established socio-demographic criteria: (a) population by age, (b) population by sex, (c) population by net monthly income (including increments), and (d) population by level of nursing education.
The overall Cronbach alpha coefficient (Table 2) is 0.787, above the 0.7 threshold, thus indicating the viability of the 12 considered autonomy items. The average item correlation is significantly positive (0.239) and situated in the acceptable range of 0.15–0.5.

Table 2.
Reliability of the nurses’ autonomy analysis model, based on the 12 items of the questionnaire.
The items’ central trend (expressed as a median value) per nursing education level is presented in Figure 2. In terms of freedom to make important patient-related decisions, graduates of advanced studies (master’s or PhD degree in nursing) are clustered around the maximum values. They are, at the same time, the category of respondents who claim to participate on their own in continuing nursing education programs. Graduates of advanced studies consider that regulation provides rather adequate support for independence in patient-related decisions. Post-secondary employees and university undergraduates perceive that the current legislation does not allow for enough autonomy. It is also noted that the majority of respondents do not consider that they have the autonomy to participate in organizational decision making, although they perceive that their nursing education is capitalized to the scope of practice.
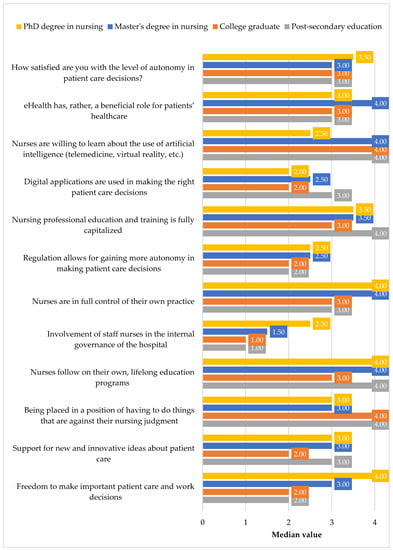
Figure 2.
Central tendency, by education, for the autonomy items of the questionnaire.
The grouping of the twelve items into composite variables includes the assessment of the viability of the construction model and the expression of each composite variable in terms of average scores for the constituent items.
The degree of professional autonomy in clinical practice arises from the freedom to make important decisions related to the care of patients, the ability of respondents to comply with the rules of professional ethics and deontology, the independent establishment of the diagnosis of care, the perception of the respondents regarding the capacity of the legislative framework to ensure nurses’ independence in clinical practice, and the satisfaction of the respondents with regard to the level of autonomy in patient-related decision making. The Cronbach alpha coefficient calculated for this first set of items (0.698) indicates the suitable reliability of the internal consistency (Table 3).

Table 3.
Reliability of the professional autonomy analysis model in clinical practice, based on the five items considered.
The correlation between the items considered for this composite variable ranges between −0.399 (correlation between professional deontology and the freedom to independently establish a diagnosis) and 0.711 (correlation between the adequacy of legislative support for ensuring autonomy and the freedom to make important decisions regarding patient care) (Table 4).

Table 4.
Correlation matrix of the items considered for the calculation of the variable capturing the degree of professional autonomy in clinical practice.
We found that the average of the correlations between the items in the first variable (0.272) is situated within the reliable range.
The significant correlation between professional deontology and decision-making freedom in patient care shows that actions that contravene the nurse’s judgment have a significant negative effect on the freedom of decision making regarding the care of patients.
The degree of autonomy in relation to the conditions, the work environment, and lifelong professional training was expressed according to the respondents’ perceptions regarding the support received for the application of innovative ideas, their interest in continuous professional training, the possibility of being involved in decisions regarding the management of the hospital, and the appreciation of the capitalization of nursing knowledge. The Cronbach alpha coefficient calculated for the second set of items of the questionnaire is 0.616 (Table 5).

Table 5.
Reliability of the autonomy analysis model in relation to the conditions, the working environment, and lifelong professional training, based on the 4 items considered.
The correlation matrix (Table 6) between the elements of the second composite variable indicates moderate positive correlations for all the items considered. The average correlation is 0.276, within the range of 0.15 and 0.5, thus demonstrating the reliability of the variable construction.

Table 6.
Correlation matrix of the items considered for the calculation of the variable degree of autonomy in relation to the conditions, the work environment, and lifelong professional training.
We emphasize that the best inter-item correlation (0.574) is between support for innovative ideas and knowledge capitalization, and the lowest correlation (0.093) is between “Lifelong learning” and “Management decisions”. The latter illustrates that a greater openness of the respondents to undertake continuous education programs would contribute very little to their involvement in the hospital’s management decision-making processes.
The use and acceptance of digital technologies in clinical practice was assessed based on responses to the items on the use of digital applications for patient care decisions, their willingness to participate in education programs in the field of the use of artificial intelligence, and the responsdents’ perception of the impact of digitalization on patients’ health. The Cronbach alpha coefficient for the last composite variable is 0.649 (Table 7).

Table 7.
Reliability of the analysis model of the use and acceptance of digital technologies in clinical practice, based on the three items considered.
The average correlation between these items (0.385) proves the variable’s construction reliability. The correlation matrix of the third composite variable is presented in Table 8. We observe moderate correlations between all three constituent items.

Table 8.
Correlation matrix of items considered for the calculation of the variable use and acceptance of digital technologies in clinical practice.
Respondents’ perception of health digitalization benefits has a significant positive correlation with the use of digital applications (0.509). So, the more they use patient-related digital technologies, the more nurses realize the importance of eHealth and therefore are more open to participating in artificial intelligence education programs.
Figure 3 shows the average values of the three composite variables by education level. None of these variables amounts to the maximum scale of “4”, validating our first hypothesis and demonstrating that the majority of respondents consider themselves to have a low to medium degree of autonomy. It is important to acknowledge that the degree of professional autonomy in clinical practice and the degree of autonomy in relation to work are significantly higher for advanced-education nurses. Thus, the level of nursing education is a determining factor for autonomy. On the other hand, the use and acceptance of digital technologies is quite low, suggesting a certain reluctance to embrace these new technologies.
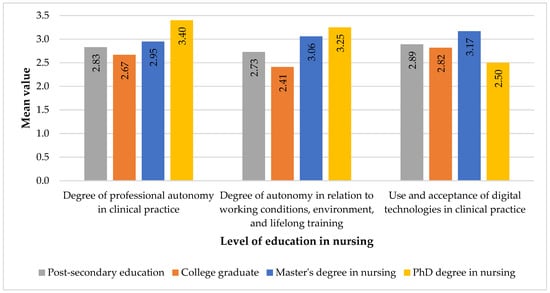
Figure 3.
Average split of autonomy (based on the three composite indicators) by level of education in nursing.
Figure 4 depicts the average level of autonomy as calculated across the entire set of questionnaire items.
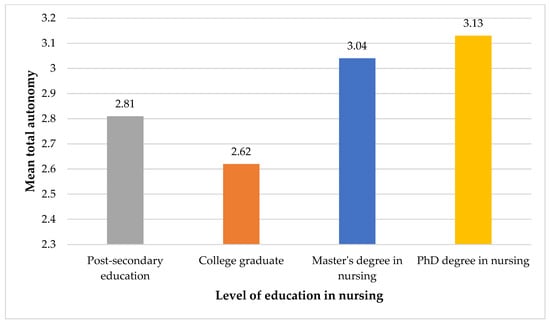
Figure 4.
Average overall autonomy (based on the twelve questionnaire items) by level of education in nursing.
As to the overall nurses’ autonomy (according to the twelve items of the questionnaire), the results are consistent with the hypothesis that education is positively correlated with the respondents’ perceptions of their degree of independence.
4. Discussion
The central tendency for the questionnaire items by education level (Figure 2) highlights a series of relevant conclusions on nurses’ autonomy. Thus, for clinical practice autonomy, it should be emphasized that nurses with post-secondary education and college undergraduates more often report situations where they are put in a position to take actions that contradict their professional judgments. In addition, autonomy in diagnosis confirms the initial hypotheses, as it is closely correlated with the respondents’ levels of professional education. Regarding autonomy in relation to work, nurses with post-secondary education are the only ones who are satisfied with their professional knowledge capitalization, while college undergraduates rank last. The lowest autonomy scores from the entire set of questionnaire items are found in decision-making processes at the hospital level, a confirmation of the hypothesis that Romania is experiencing important gaps in promoting nursing leadership. The respondents consider that regulation does not stimulate nurses’ independent medical interventions. From the perspective of digital autonomy, contrary to expectations, nurses with post-secondary education declare the most intense use of digital technologies in patient care decisions. However, the use of ICTs is relatively low among all respondents. On the other hand, nurses with a master’s degree recognize, to the greatest extent, the benefits of digital applications. We emphasize the willingness of all nurse categories (except PhDs, which were poorly represented in our sample) to follow eHealth education programs.
The results of the Inter-Item Correlation Matrix (Table 4, Table 6, and Table 8) also reveal a number of conclusive aspects. Thus, for clinical practice autonomy, regulation has a significant impact on all components of this composite indicator, especially on care decisions and clinical satisfaction. From the perspective of autonomy in relation to work, the most significant correlation appears between the degree of professional knowledge capitalization and support for the application of new, innovative care solutions. This reflects the nurse-perceived importance of managerial and physicians’ involvement in promoting professional independence. Our study confirms that the perception of the beneficial role of digitalization is the main trigger for the use of eHealth technologies.
With the distribution of the 12 questionnaire items into 3 composite variables (clinical practice autonomy, autonomy in relation to work, and digital autonomy), the obtained results fit, in general, the research hypotheses. For clinical practice autonomy, it is observed that nurses with advanced education report the highest autonomy scores, with an important increase from master’s graduates to PhDs. However, there is a lower degree of autonomy among college undergraduates compared to post-secondary nurses. This is explained by the lack of experience among undergraduates, given that nursing university studies have a relatively recent history in Romania. We reiterate that our research is limited to the evaluation of the subjective perception of autonomy. For autonomy in relation to work, the situation is repeated, with the indication that college undergraduates experience even lower autonomy scores compared to the other nurse categories. With respect to the use and acceptance of digital technologies, graduates with master’s degrees have a higher autonomy score than those with post-secondary and undergraduate education. However, we note the small differences between the last two categories of nurses, a fact that can be attributed to an insufficient presence of the digital component in the university curriculum (Figure 3).
If we consider the global autonomy score that includes all three previous composite components, our outcomes reveal a similar situation (Figure 4). In other words, the hypothesis that the education level induces greater autonomy is only valid for nurses with advanced education. College undergraduates perceive less autonomy than nurses with post-secondary degrees. This result calls for further research on education interdependencies with professional experience, university training quality, and the inclusion of nursing digitalization.
The limitations of our study are related to the fact that the respondents belong to a single hospital, so in the future, we will extend the research to other health units. In addition, the analysis of perceived autonomy can be structured based on different medical specialties.
Author Contributions
Conceptualization, M.B., I.P.I., J.A., I.R. and D.A.C., methodology M.B., I.P.I., J.A., D.A.C., C.J. and I.R.; validation, formal analysis, and investigation, M.B., I.P.I., J.A., D.A.C., C.J., L.-I.G. and I.R.; data curation, I.R. and C.J. writing—original draft preparation, M.B., I.P.I., J.A., D.A.C., C.J., L.-I.G. and I.R.; writing—review and editing, M.B., I.P.I., J.A., D.A.C., C.J., L.-I.G. and I.R.; project administration, M.B., I.P.I. and I.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Clinical Hospital “Theodor Burghele” (protocol code 7371/24 August 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. State of the World’s Nursing 2020: Investing in Education, Jobs and Leadership; World Health Organization: Geneva, Switzerland, 2020; ISBN 978-92-4-000327-9. [Google Scholar]
- OECD; European Union. Health at a Glance: Europe 2020: State of Health in the EU Cycle; OECD: Paris, France, 2020; ISBN 978-92-64-36564-3. [Google Scholar]
- Personalul Medico-Sanitar pe Categorii, Forme de Proprietate, Sexe, Macroregiuni, Regiuni de Dezvoltare și Județe. Available online: http://statistici.insse.ro:8077/tempo-online/#/pages/tables/insse-table (accessed on 15 October 2022).
- Savitz, L.A.; Jones, C.B.; Bernard, S. Quality Indicators Sensitive to Nurse Staffing in Acute Care Settings. In Advances in Patient Safety: From Research to Implementation (Volume 4: Programs, Tools, and Products); Henriksen, K., Battles, J.B., Marks, E.S., Lewin, D.I., Eds.; Advances in Patient Safety; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2005. [Google Scholar]
- Crevacore, C.; Jacob, E.; Coventry, L.L.; Duffield, C. Integrative Review: Factors Impacting Effective Delegation Practices by Registered Nurses to Assistants in Nursing. J. Adv. Nurs. 2022. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Strategy on Human Resources for Health: Workforce 2030; World Health Organization: Geneva, Switzerland, 2016; ISBN 978-92-4-151113-1. [Google Scholar]
- Xue, Y.; Ye, Z.; Brewer, C.; Spetz, J. Impact of State Nurse Practitioner Scope-of-Practice Regulation on Health Care Delivery: Systematic Review. Nurs. Outlook 2016, 64, 71–85. [Google Scholar] [CrossRef] [PubMed]
- Spetz, J.; Skillman, S.M.; Andrilla, C.H.A. Nurse Practitioner Autonomy and Satisfaction in Rural Settings. Med. Care Res. Rev. 2017, 74, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Neprash, H.T.; Smith, L.B.; Sheridan, B.; Moscovice, I.; Prasad, S.; Kozhimannil, K. Nurse Practitioner Autonomy and Complexity of Care in Rural Primary Care. Med. Care Res. Rev. 2021, 78, 684–692. [Google Scholar] [CrossRef] [PubMed]
- Committee on the Future of Nursing 2020–2030; National Academy of Medicine; National Academies of Sciences, Engineering, and Medicine. The Future of Nursing 2020–2030: Charting a Path to Achieve Health Equity; Wakefield, M.K., Williams, D.R., Menestrel, S.L., Flaubert, J.L., Eds.; National Academies Press: Washington, DC, USA, 2021; p. 25982. ISBN 978-0-309-68506-1. [Google Scholar]
- Pisică, S.; Ioniță, A.; Rădoi, S.; Gusicov, D.M.; Militaru, A. Activitatea Rețelei Sanitare și de Ocrotire a Sănătății în Anul 2021; National Institute of Statistics: Bucharest, Romania, 2022. [Google Scholar]
- Vaismoradi, M.; Vizcaya-Moreno, F.; Jordan, S.; Gåre Kymre, I.; Kangasniemi, M. Disclosing and Reporting Practice Errors by Nurses in Residential Long-Term Care Settings: A Systematic Review. Sustainability 2020, 12, 2630. [Google Scholar] [CrossRef]
- Karimi-Shahanjarini, A.; Shakibazadeh, E.; Rashidian, A.; Hajimiri, K.; Glenton, C.; Noyes, J.; Lewin, S.; Laurant, M.; Colvin, C.J. Barriers and Facilitators to the Implementation of Doctor-Nurse Substitution Strategies in Primary Care: A Qualitative Evidence Synthesis. Cochrane Database Syst. Rev. 2019, 2019. [Google Scholar] [CrossRef]
- Barchielli, C.; Rafferty, A.M.; Vainieri, M. Integrating Key Nursing Measures into a Comprehensive Healthcare Performance Management System: A Tuscan Experience. Int. J. Environ. Res. Public. Health 2022, 19, 1373. [Google Scholar] [CrossRef]
- Navales, J.V.; Jallow, A.W.; Lai, C.Y.; Liu, C.Y.; Chen, S.W. Relationship between Quality of Nursing Work Life and Uniformed Nurses’ Attitudes and Practices Related to COVID-19 in the Philippines: A Cross-Sectional Study. Int. J. Environ. Res. Public. Health 2021, 18, 9953. [Google Scholar] [CrossRef]
- LEGE Nr. 278/2015 din 12 Noiembrie 2015 Pentru Modificarea şi Completarea Ordonanţei de Urgenţă a Guvernului nr. 144/2008 Privind Exercitarea Profesiei de Asistent Medical Generalist, a Profesiei de Moaşă şi a Profesiei de Asistent Medical, Precum şi Organizarea şi Funcţionarea Ordinului Asistenţilor Medicali Generalişti, Moaşelor şi Asistenţilor Medicali din România. Available online: https://www.oamr.ro/wp-content/uploads/2016/01/Legea-278_2015-1.pdf (accessed on 10 February 2022).
- Harpula, K.; Bartosiewicz, A.; Krukowski, J. Polish Nurses’ Opinions on the Expansion of Their Competences—Cross-Sectional Study. Nurs. Rep. 2021, 11, 301–310. [Google Scholar] [CrossRef]
- Misiak, B.; Sierżantowicz, R.; Krajewska-Kułak, E.; Lewko, K.; Chilińska, J.; Lewko, J. Psychosocial Work-Related Hazards and Their Relationship to the Quality of Life of Nurses—A Cross-Sectional Study. Int. J. Environ. Res. Public. Health 2020, 17, 755. [Google Scholar] [CrossRef]
- Saad, L. Military Brass, Judges Among Professions at New Image Lows. Available online: https://news.gallup.com/poll/388649/military-brass-judges-among-professions-new-image-lows.aspx (accessed on 15 October 2022).
- Pompierii și SMURD, Două Instituții Controlate de Raed Arafat, în Topul Încrederii Românilor. Available online: https://www.g4media.ro/exclusiv-sondaj-avangarde-pompierii-si-smurd-doua-institutii-controlate-de-raed-arafat-in-topul-increderii-romanilor-in-trecut-primele-locuri-erau-ocupate-de-armata-si-biserica.html (accessed on 15 October 2022).
- Selanders, L.; Crane, P. The Voice of Florence Nightingale on Advocacy. OJIN Online J. Issues Nurs. 2012, 17, 1. [Google Scholar] [CrossRef] [PubMed]
- Marcean, C.; Ghinoiu, C. Tratat de Nursing: Îngrijirea Omului Sănătos şi Bolnav; Ediţie Îngrijită; Editura Medicală: Bucureşti, Romania, 2010; ISBN 978-973-39-0704-6. [Google Scholar]
- Rosser, E.; Westcott, L.; Ali, P.A.; Bosanquet, J.; Castro-Sanchez, E.; Dewing, J.; McCormack, B.; Merrell, J.; Witham, G. The Need for Visible Nursing Leadership During COVID-19. J. Nurs. Scholarsh. 2020, 52, 459–461. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, Y.; Okuda, R.; Fukada, M. Factors Affecting Clinical Nursing Competency: A Cross Sectional Study. Yonago Acta Med. 2021, 64, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Norman, R.M.; Sjetne, I.S. Measuring Nurses’ Perception of Work Environment: A Scoping Review of Questionnaires. BMC Nurs. 2017, 16, 66. [Google Scholar] [CrossRef]
- Lasater, K.B.; Germack, H.D.; Small, D.S.; McHugh, M.D. Hospitals Known for Nursing Excellence Perform Better on Value Based Purchasing Measures. Policy Polit. Nurs. Pract. 2016, 17, 177–186. [Google Scholar] [CrossRef]
- Slater, P.; O’Halloran, P.; Connolly, D.; McCormack, B. Testing of the Factor Structure of the Nursing Work Index-Revised. Worldviews Evid. Based Nurs. 2010, 7, 123–134. [Google Scholar] [CrossRef]
- Hara, Y.; Asakura, K.; Asakura, T. The Impact of Changes in Professional Autonomy and Occupational Commitment on Nurses’ Intention to Leave: A Two-Wave Longitudinal Study in Japan. Int. J. Environ. Res. Public. Health 2020, 17, 6120. [Google Scholar] [CrossRef]
- Rao, A.D.; Kumar, A.; McHugh, M. Better Nurse Autonomy Decreases the Odds of 30-Day Mortality and Failure to Rescue: Nurse Autonomy. J. Nurs. Scholarsh. 2017, 49, 73–79. [Google Scholar] [CrossRef]
- Auerbach, D.I.; Chen, P.G.; Friedberg, M.W.; Reid, R.; Lau, C.; Buerhaus, P.I.; Mehrotra, A. Nurse-Managed Health Centers and Patient-Centered Medical Homes Could Mitigate Expected Primary Care Physician Shortage. Health Aff. (Millwood) 2013, 32, 1933–1941. [Google Scholar] [CrossRef]
- Oner, B.; Zengul, F.D.; Oner, N.; Ivankova, N.V.; Karadag, A.; Patrician, P.A. Nursing-sensitive Indicators for Nursing Care: A Systematic Review (1997–2017). Nurs. Open 2021, 8, 1005–1022. [Google Scholar] [CrossRef]
- Ionel, I.P.; Armean, P.; Furtunescu, F.L. Assessment of Stress and Satisfaction in Nurses, as Part of Hospital Accreditation. Acta Med. Transilv. 2017, 22, 11–13. [Google Scholar]
- Rouhi-Balasi, L.; Elahi, N.; Ebadi, A.; Jahani, S.; Hazrati, M. Professional Autonomy of Nurses: A Qualitative Meta-Synthesis Study. Iran. J. Nurs. Midwifery Res. 2020, 25, 273. [Google Scholar] [CrossRef] [PubMed]
- Nibbelink, C.W.; Brewer, B.B. Decision-Making in Nursing Practice: An Integrative Literature Review. J. Clin. Nurs. 2018, 27, 917–928. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.; De Gagne, J.C. Autonomy of Nurse Practitioners in Primary Care: An Integrative Review. J. Am. Assoc. Nurse Pract. 2016, 28, 170–174. [Google Scholar] [CrossRef] [PubMed]
- Oshodi, T.O.; Bruneau, B.; Crockett, R.; Kinchington, F.; Nayar, S.; West, E. Registered Nurses’ Perceptions and Experiences of Autonomy: A Descriptive Phenomenological Study. BMC Nurs. 2019, 18, 51. [Google Scholar] [CrossRef]
- Pantazopoulos, I.; Tsoni, A.; Kouskouni, E.; Papadimitriou, L.; Johnson, E.O.; Xanthos, T. Factors Influencing Nurses’ Decisions to Activate Medical Emergency Teams: MET Activation. J. Clin. Nurs. 2012, 21, 2668–2678. [Google Scholar] [CrossRef]
- Directorate—General for Health and Food Safety (European Commission); EY; Open Evidencce; Politécnica LifeStech. Study on Health Data, Digital Health and Artificial Intelligence in Healthcare; Publications Office of the EU: Luxembourg, 2022. [Google Scholar]
- Titircă, L.; Gal, G.; Seuchea, M. Tehnici de Evaluare şi Îngrijiri Acordate de Asistenţii Medicali: Ghid de Nursing; Ediţia a 7-a.; Viaţa Medicală Românească: Bucureşti, Romania, 2008; ISBN 978-973-160-010-9. [Google Scholar]
- The Essentials: Core Competencies for Professional Nursing education. Available online: https://www.aacnnursing.org/AACN-Essentials (accessed on 7 October 2022).
- DIRECTIVE 2013/55/EU OF THE EUROPEAN PARLIAMENT AND OF THE COUNCIL of 20 November 2013 Amending Directive 2005/36/EC on the Recognition of Professional Qualifications and Regulation (EU) No 1024/2012 on Administrative Cooperation through the Internal Market Information System (‘the IMI Regulation’). Available online: https://eur-lex.europa.eu (accessed on 15 October 2022).
- Hotărâre Privind Aprobarea Strategiei Multianuale Pentru Dezvoltarea Resurselor Umane în Sănătate 2022—2030. Available online: https://rohealthreview.ro/wp-content/uploads/2022/07/Monitorul-Oficial-Partea-I-nr.-663.pdf (accessed on 15 October 2022).
- Nursing and Caring Professionals. Available online: https://ec.europa.eu/eurostat/databrowser/view/HLTH_RS_PRSNS/default/table?lang=en&category=hlth.hlth_care.hlth_res.hlth_staff (accessed on 15 October 2022).
- Structure, Group Definitions and Correspondence Tables; International Labour Office: Geneva, Switzerland, 2012; ISBN 978-92-2-125953-4.
- Health Graduates. Available online: https://ec.europa.eu/eurostat/databrowser/view/HLTH_RS_GRD__custom_3593049/default/table?lang=en (accessed on 15 October 2022).
- Ionel, I.P.; Armean, P.; Furtunescu, F.L. Hospitals Accreditation: How Well We Understand the Process? Acta Med. Transilv. Public Health Manag. 2015, 20, 22–23. [Google Scholar]
- Nursing Regulation around the World. Available online: https://regulatoryatlas.com/ (accessed on 3 August 2022).
- APRNs in the U.S. Available online: https://www.ncsbn.org/nursing-regulation/practice/aprn.page (accessed on 8 March 2022).
- Ordinul Ministrului Sănătății, Muncii și Protecției Sociale nr.867 din 23 octombrie 2020. Available online: https://msmps.gov.md/wp-content/uploads/2020/10/Ordin-MSMPS-nr.-867-din-23.09.2020-Comisii-de-specialitate.pdf (accessed on 3 August 2022).
- Park, J.; Athey, E.; Pericak, A.; Pulcini, J.; Greene, J. To What Extent Are State Scope of Practice Laws Related to Nurse Practitioners’ Day-to-Day Practice Autonomy? Med. Care Res. Rev. 2018, 75, 66–87. [Google Scholar] [CrossRef]
- Krick, T.; Huter, K.; Domhoff, D.; Schmidt, A.; Rothgang, H.; Wolf-Ostermann, K. Digital Technology and Nursing Care: A Scoping Review on Acceptance, Effectiveness and Efficiency Studies of Informal and Formal Care Technologies. BMC Health Serv. Res. 2019, 19, 400. [Google Scholar] [CrossRef]
- Ross, J.; Stevenson, F.; Lau, R.; Murray, E. Exploring the Challenges of Implementing E-Health: A Protocol for an Update of a Systematic Review of Reviews. BMJ Open 2015, 5, e006773. [Google Scholar] [CrossRef]
- Scott Kruse, C.; Karem, P.; Shifflett, K.; Vegi, L.; Ravi, K.; Brooks, M. Evaluating Barriers to Adopting Telemedicine Worldwide: A Systematic Review. J. Telemed. Telecare 2018, 24, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Mair, F.S.; May, C.; O’Donnell, C.; Finch, T.; Sullivan, F.; Murray, E. Factors That Promote or Inhibit the Implementation of E-Health Systems: An Explanatory Systematic Review. Bull. World Health Organ. 2012, 90, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Russo, J.E.; McCool, R.R.; Davies, L. VA Telemedicine: An Analysis of Cost and Time Savings. Telemed. E-Health 2016, 22, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Jedamzik, S. Digitale Gesundheit und Pflege: Die Zukunft ist jetzt. Unfallchirurg 2019, 122, 670–675. [Google Scholar] [CrossRef] [PubMed]
- Onu, F.U.; Agbo, I.S. Factors That Affect the Use of Ict in Nursing Profession in Ebonyi State Nigeria. J. Inf. Eng. Appl. 2013, 3, 63–69. [Google Scholar]
- Rutledge, C.M.; O’Rourke, J.; Mason, A.M.; Chike-Harris, K.; Behnke, L.; Melhado, L.; Downes, L.; Gustin, T. Telehealth Competencies for Nursing Education and Practice: The Four P’s of Telehealth. Nurse Educ. 2021, 46, 300–305. [Google Scholar] [CrossRef]
- Chen, F.-Q.; Leng, Y.-F.; Ge, J.-F.; Wang, D.-W.; Li, C.; Chen, B.; Sun, Z.-L. Effectiveness of Virtual Reality in Nursing Education: Meta-Analysis. J. Med. Internet Res. 2020, 22, e18290. [Google Scholar] [CrossRef]
- Geng, Y.; Huang, P.-S.; Huang, Y.-M. Crowdsourcing in Nursing Education: A Possibility of Creating a Personalized Online Learning Environment for Student Nurses in the Post-COVID Era. Sustainability 2021, 13, 3413. [Google Scholar] [CrossRef]
- Rouleau, G.; Gagnon, M.-P.; Côté, J.; Payne-Gagnon, J.; Hudson, E.; Dubois, C.-A. Impact of Information and Communication Technologies on Nursing Care: Results of an Overview of Systematic Reviews. J. Med. Internet Res. 2017, 19, e122. [Google Scholar] [CrossRef]
- Fagerström, C.; Tuvesson, H.; Axelsson, L.; Nilsson, L. The Role of ICT in Nursing Practice: An Integrative Literature Review of the Swedish Context. Scand. J. Caring Sci. 2017, 31, 434–448. [Google Scholar] [CrossRef]
- Button, D.; Harrington, A.; Belan, I. E-Learning & Information Communication Technology (ICT) in Nursing Education: A Review of the Literature. Nurse Educ. Today 2014, 34, 1311–1323. [Google Scholar] [CrossRef] [PubMed]
- Donabedian, A. The Definition of Quality and Approaches to Its Assessment; His Explorations in Quality Assessment and Monitoring; Health Administration Press: Ann Arbor, MI, USA, 1980; ISBN 978-0-914904-47-2. [Google Scholar]
- Donabedian, A. The Quality of Care. How Can It Be Assessed? JAMA J. Am. Med. Assoc. 1988, 260, 1743–1748. [Google Scholar] [CrossRef]
- Heslop, L.; Lu, S.; Xu, X. Nursing-sensitive Indicators: A Concept Analysis. J. Adv. Nurs. 2014, 70, 2469–2482. [Google Scholar] [CrossRef] [PubMed]
- Needleman, J.; Kurtzman, E.T.; Kizer, K.W. Performance Measurement of Nursing Care. Med. Care Res. Rev. 2007, 64, 10S–43S. [Google Scholar] [CrossRef] [PubMed]
- Lukewich, J.A.; Tranmer, J.E.; Kirkland, M.C.; Walsh, A.J. Exploring the Utility of the Nursing Role Effectiveness Model in Evaluating Nursing Contributions in Primary Health Care: A Scoping Review. Nurs. Open 2019, 6, 685–697. [Google Scholar] [CrossRef] [PubMed]
- Doran, D.I.; Sidani, S.; Keatings, M.; Doidge, D. An Empirical Test of the Nursing Role Effectiveness Model. J. Adv. Nurs. 2002, 38, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Irvine, D.; Sidani, S.; Hall, L.M. Linking Outcomes to Nurses’ Roles in Health Care. Nurs. Econ. 1998, 16, 58–64, 87. [Google Scholar] [PubMed]
- Irvine, D.; Sidani, S.; Hall, L.M. Finding Value in Nursing Care: A Framework for Quality Improvement and Clinical Evaluation. Nurs. Econ. 1998, 16, 110–116, 131. [Google Scholar]
- World Health Organization. National Health Workforce Accounts: A Handbook; World Health Organization: Geneva, Switzerland, 2017; ISBN 978-92-4-151311-1. [Google Scholar]
- Donabedian, A. Evaluating the Quality of Medical Care. Milbank Mem. Fund Q. 1966, 44, 166–206. [Google Scholar] [CrossRef]
- Berwick, D.; Fox, D.M. “Evaluating the Quality of Medical Care”: Donabedian’s Classic Article 50 Years Later: “Evaluating the Quality of Medical Care”. Milbank Q. 2016, 94, 237–241. [Google Scholar] [CrossRef]
- Rubin, R.B.; Sypher, H.E.; Palmgreen, P. (Eds.) Communication Research Measures, 1st ed.; Communication studies; 1. publ. in paperback; Routledge: New York, NY, USA, 2009; ISBN 978-0-415-87146-4. [Google Scholar]
- University of Lincoln. Guides: MASH Guide: Home. Available online: https://guides.library.lincoln.ac.uk/c.php?g=110730 (accessed on 10 October 2022).
- Mirzaei, A.; Carter, S.R.; Patanwala, A.E.; Schneider, C.R. Missing Data in Surveys: Key Concepts, Approaches, and Applications. Res. Soc. Adm. Pharm. 2022, 18, 2308–2316. [Google Scholar] [CrossRef] [PubMed]
- Morgan, G.A. IBM SPSS for Introductory Statistics: Use and Interpretation, 6th ed.; Routledge: New York, NY, USA, 2020; ISBN 978-1-138-57822-7. [Google Scholar]
- Pallant, J. SPSS Survival Manual: A Step by Step Guide to Data Analysis Using IBM SPSS, 7th ed.; Routledge: New York, NY, USA, 2020; ISBN 978-1-00-311745-2. [Google Scholar]
- Creswell, J.W. Educational Research: Planning, Conducting, and Evaluating Quantitative and Qualitative Research, 4th ed.; Pearson: Boston, MA, USA, 2012; ISBN 978-0-13-136739-5. [Google Scholar]
- Hanapiah, K.S.; Hashim, A.; Karim, Z.A. Validity and Reliability of Tactical Skills Assessment Instrument for Talent Identification among Malaysian Male Young Football Players. Int. J. Acad. Res. Bus. Soc. Sci. 2019, 9, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Clark, L.A.; Watson, D. Constructing Validity: Basic Issues in Objective Scale Development. Psychol. Assess. 1995, 7, 309–319. [Google Scholar] [CrossRef]
- IBM Corp. Released 2020. IBM SPSS Statistics for Windows; Version 27.0; IBM Corp: Armonk, NY, USA, 2020. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).