1. Introduction
The healthcare sector is known to be a large contributor to environmental pollution. On average, 5.5% of the total national carbon footprint of countries originates from the healthcare sector [
1]. The healthcare sectors of developed countries such as the United States (US), Belgium, and Japan are in the lead, being accountable for 7.6 to 8.1% of carbon output [
1]. In 2013, the global disease burden due to the environmental impact of the US healthcare sector was calculated to be 614,000 disability-adjusted life years (DALY) annually [
2]. This paradox, where healthcare has indirect adverse effects on public health, calls for action to improve environmental performance of the healthcare sector through energy savings and a reduction in environmental pollution and waste generation [
3,
4].
Healthcare waste (HCW) and its disposal cause pollution and consequently pose health risks that may result in disease and premature death [
5,
6]. Being one of the largest industries in the world, healthcare generates a vast amount of waste, which is expected to increase in the coming decades due to a growing number of healthcare interventions, as a result of global population growth and increased life expectancy [
6]. Producing 8.4 kg/bed/day, resulting in three billion kilograms of waste annually, the US is momentarily ranks first in the world with regard to HCW generation [
7].
The World Health Organization (WHO) estimates that 85% of HCW is non-hazardous waste, while the remaining is either infectious, toxic, or radioactive [
5]. The most common methods of disposal of HCW are incineration and landfill, both of which can lead to the production of hazardous chemicals and pollutants [
6]. Not only because of its environmental impact but also given the financial consequences and health hazards, it is of the utmost importance to reduce the generation of HCW.
Hospitals are known large polluters; in developed countries, they generate 1% of a nation’s solid waste [
8]. Being resource intensive, it is estimated that up to 33% of all hospital waste is generated in operating rooms (ORs) [
8]. In their study on the carbon footprint of three Western academic hospitals, MacNeill et al. found that a single operation yields up to an average of 16 kg of solid waste [
9].
Addressing waste generation in an operating room setting can be very challenging for a number of reasons. Firstly, in recent decades there has been an emphasis on the employment of single-use items, which by definition generate a lot of waste. Secondly, a portion of operating room waste consists of hazardous waste. Proper segregation of this waste stream from the non-hazardous waste is desirable because the non-hazardous waste contains a fraction of important recyclable material [
10]. In practice, this waste segregation has proven to be complicated mainly due to a lack of knowledge on the work floor, and because OR waste contains contaminated materials [
11,
12]. As with waste reduction in general, the cornerstones for waste reduction in the OR are ‘reduce’, ‘reuse’, and ‘recycle’ [
13].
A reduction in surgical waste can be achieved by preventing wastage. During surgical procedures, there is often overage in the form of disposable sterile materials and instruments that are opened but not used [
14,
15,
16,
17]. Additionally, disposable custom packs (sets of disposable products pre-packaged for specific procedures) frequently contain unnecessary materials [
18]. Hygiene regulations dictate that these unused instruments and materials may not be used for another patient and must therefore be discarded. Preventing these forms of wastage not only benefits the environment, but also increases cost efficiency.
Reusing instruments, gowns, and drapes instead of using disposable alternatives can provide significant waste reduction in the OR [
12]. Using reusable sterile gowns instead of disposable gowns resulted in 84% less waste [
19]. Blue wrap, a single use polypropylene wrap for sterile surgical instruments, is a major source of surgical waste [
20]. Estimates suggest that 115 million kilograms of blue wrap is discarded on a yearly basis in the US alone [
21]. Reusable rigid aluminum containers are a good alternative to blue wrap, as instead of utilizing a single-use wrapper, surgical instruments are sterilized in a reusable aluminum case. A comparative Life Cycle Assessment (LCA) of these two packaging systems showed that the carbon footprint of the aluminum containers is 85% less than that of blue wrap [
22].
Recycling is an important way to ensure that raw materials are not wasted in a circular economy. In part due to the fact that many discarded materials are contaminated, only 20–25% of OR waste is eligible for recycling [
10]. This potentially recyclable fraction mainly concerns paper and plastic packaging, because catheters, syringes, etc., are not suitable for recycling. Recycling is frequently considered to be the primary solution to reducing OR waste [
20,
23,
24]. However, from an environmental point of view, it is often preferable to address waste output in the OR by considering ‘reduce’ and ‘reuse’ first, since in recycling, energy has to be added to produce new products, and in many cases the quality of the raw material decreases (downcycling).
All of these different approaches to addressing OR waste can ensure that the environmental sustainability of the OR is improved. However, not every strategy is equally eco-effective, and frequently it is not obvious which waste results in the largest environmental burden. For example, reducing the number of redundant cotton gauzes from a custom pack has a much greater environmental impact than recycling polypropylene items from the same kit [
18]. A classical LCA can reveal where environmental hotspots are in operating room waste. However, it takes a lot of time and effort to perform a full LCA for every single disposable item in the OR. An alternative is to look at the environmental impact of waste itself. By using Department for Environment, Food and Rural Affairs (DEFRA) greenhouse gas life cycle conversion factors, MacNeill et al. calculated the carbon footprints of surgical waste based on the material composition of waste streams in the operating room [
9]. DEFRA conversion factors take into account greenhouse gas emissions that are generated both upstream (in the supply chain) and downstream (during disposal) [
25].
Many studies on reducing OR waste focus on a particular source of OR waste, or on a single solution such as reducing overage or recycling [
10,
14,
15,
20,
23,
26,
27,
28]. However, with this practice, it is not clear that the approach chosen is most effective in addressing environmental impact from OR waste as a whole. A well-structured, multidisciplinary approach to waste inventory and the implementation of solutions is expected to yield better results.
In the context of increasing patient safety, DeRosier et al. described a prospective risk analysis tool with which healthcare processes can be analyzed to identify and address patient hazards [
29]. This Healthcare Failure Mode and Effect Analysis (HFMEA) is a structured method in which a multidisciplinary team goes through a step-by-step process that is characterized by the use of a flow diagram, a hazard analysis, and a decision tree with which critical and relevant parts of the process are identified for improvement [
29]. Evaluation of the HFMEA has shown that although it is a time- and resource-intensive method, it is useful for assessing and improving the safety of healthcare processes [
30,
31,
32]. The HFMEA has proven successful for improving patient safety in processes such as blood transfusions, drug administration, and in the introduction of new surgical techniques [
33,
34,
35].
The primary research question for this study was whether it is possible to transform the HFMEA into a tool for identifying and addressing the environmental impact of OR waste. As far as we know, to date, no comparable structured, multidisciplinary approach has been described in the literature to address the OR waste problem in such a comprehensive way. As a secondary research question, we investigated whether the application of this novel method, the Healthcare Sustainability Mode and Effect Analysis (HSMEA), could identify carbon hotspots in surgical waste and provide solutions for improvement.
2. Materials & Methods
2.1. Healthcare Sustainability Mode and Effect Analysis (HSMEA)
The Failure Mode and Effect Analysis (FMEA) is a risk assessment tool that is frequently used in the manufacturing industry. Its purpose is to prospectively identify the ways in which a process may fail (failure mode) and examine their consequences (effect analysis). In order to apply this method to healthcare processes for improving patient safety, the Healthcare FMEA (HFMEA) was created [
29]. The HFMEA is a structured step-by-step method characterized by the key elements listed in
Table 1.
A multidisciplinary team of 6–8 people carries out the five analytical steps (
Table 2) of this method in a series of 4–6 meetings. The five steps that comprise the HFMEA were taken as a template for the Healthcare Sustainability Mode and Effect Analysis tool [
29].
Step 1: Topic definition
In order to perform a focused analysis of the subject, a very precise topic needs to be chosen. This will provide guidance to the team performing the HSMEA analysis. In the context of patient safety, the HFMEA recommends topics that are in a high-risk or high-vulnerability area. By analogy, healthcare processes that have a large environmental impact (e.g., greenhouse gas emissions, surface water pollution) can be a topic for review using the HSMEA. This research focuses on waste production from the OR, but other topics in the areas of energy consumption, water consumption, use of pharmaceuticals, etc., are eligible, as long as they are topics that can potentially increase the sustainability of healthcare, that are readily quantifiable, and for which opportunities for improvement exist.
Step 2: Team assembly
For this step, a multidisciplinary team is assembled, and meetings are scheduled in which the various process steps will be completed. Since the processes under investigation are often complex in nature, where no one person has all the knowledge about all aspects, it is important to assemble a team that is multidisciplinary. Team members should include subject matter experts, outsiders, and a leader. Subject matter experts have specific knowledge of (parts of) the process being studied. Outsiders, on the other hand, are healthcare professionals from other fields who are unfamiliar with the process being studied, potentially favoring an unbiased outcome. The role of the team leader is crucial for the successful completion of a HFMEA [
31]. The team leader must be someone with leadership skills who preferably has experience with previous FMEAs. The team leader’s role is to maintain an overview, monitor the process, guide the team, and ultimately ensure a final result. The optimal size of a multidisciplinary FMEA team is 6–10 members. The team must be large enough to have sufficient expertise regarding all facets of the process, and small enough to ensure that meetings can be attended by a sufficient number of individuals [
30]. The number of meetings advised is 4–6, each lasting 2–3 h, thus being long and often enough to allow for progress, but with attention to feasibility, and the focus and enthusiasm of the team [
30].
Step 3: Process flowchart
A graphical representation of the entire process provides not only an overview, but also insight into the various sub-processes. The purpose of the flowchart is to be complete, to prevent parts of the process from being overlooked, and further, to guide the team so that they are not overwhelmed by the complexity of the process [
29]. In order to obtain a detailed understanding of the process of waste generation, the team investigate what kind of products and materials are disposed of. Every group of items that is disposed of is called a sub-step (for example, the disposal of 10 identical cotton gauzes counts as 1 item). They then investigate which waste streams they are disposed of through, and how this waste stream is handled. This is described graphically by means of a flowchart.
Step 4: Hazard analysis
In the original HFMEA, this step identifies all the possible failure modes of the sub-steps, and a hazard score (a measure of the impact on patients if the error occurs) is calculated. This hazard score is displayed in a matrix to provide an overview of the severity and probability of the potential error.
In our HSMEA, the environmental hazard of all sub-steps (items that are disposed of) identified in Step 3 are quantified in Step 4 by means of the amount of waste (in kg) produced, and the carbon footprint of the waste stream it is disposed of through (kg CO
2 equivalents). In order to calculate the carbon footprint, DEFRA greenhouse gas life cycle conversion factors for waste disposal are used (
Table 3).
These conversion factors take into account greenhouse gas emissions generated both upstream (production, transport) and downstream (transport, disposal). MacNeill et al., used this method to quantify the carbon footprint of surgical waste in their study on carbon footprinting operating theaters in three health systems [
9].
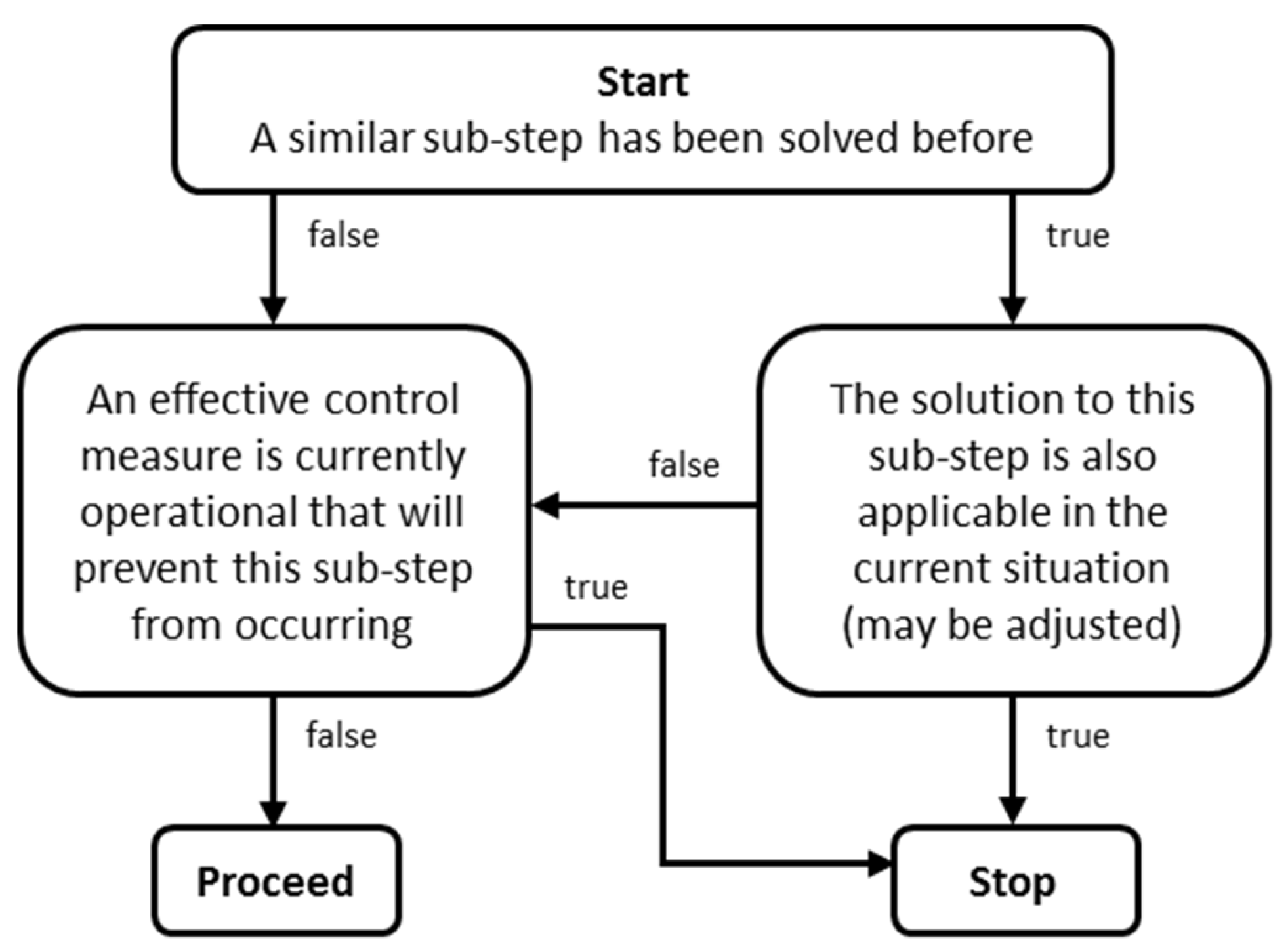
Furthermore, in Step 4, a decision tree is applied to each sub-step. The decision tree serves as a triaging function. It ensures that if a solution to a similar problem has been encountered in a previous HSMEA, this process does not have to be gone through again. The decision tree then determines whether the HSMEA process should continue for the sub-step (‘proceed’) or should be terminated (‘stop’) (
Figure 1).
Step 5: Actions and outcome measures
For every sub-step (items that are disposed of), as identified in Step 3, that passes through the decision tree, the team members now have to identify a sustainable solution. Here, the cornerstones for waste reduction in the OR (‘reduce’, ‘reuse’, and ‘recycle’) are applied [
13]. These classic three Rs of waste minimization strategies have been supplemented with ‘rethink’, ‘refuse’ and ‘refrain’ from action. ‘Rethink’ to consider alternatives for the item instead waste disposal, ‘refuse’ if the item turns out to be redundant and can be omitted, and ‘refrain’ if some sub-steps cannot be made more sustainable at the moment.
After selecting one of these six Rs as a solution for each item, the tool automatically recalculates the new environmental hazard (carbon footprint) using the revised weight and emission factor. The environmental hazard of an item may decrease as a result of it being less present (fewer kilograms) in the waste after the chosen solution (refuse, reduce, reuse, rethink), or because it is disposed of in a different waste stream with a lower carbon footprint, such as when plastic is separated for recycling (2.1 kg CO2-eq/kg) instead of entering the MSW stream (4.4 kg CO2-eq/kg). It is also checked for every sub-step whether it would have an impact on stakeholder safety. Now, the hotspots for sustainable intervention can be determined by comparing the baseline situation from Step 4 to the new situation from Step 5. By categorizing the proposed solutions, it becomes apparent which solution category has the largest impact on the carbon footprint. These categories are called hotspots and are prioritized to implement in daily practice.
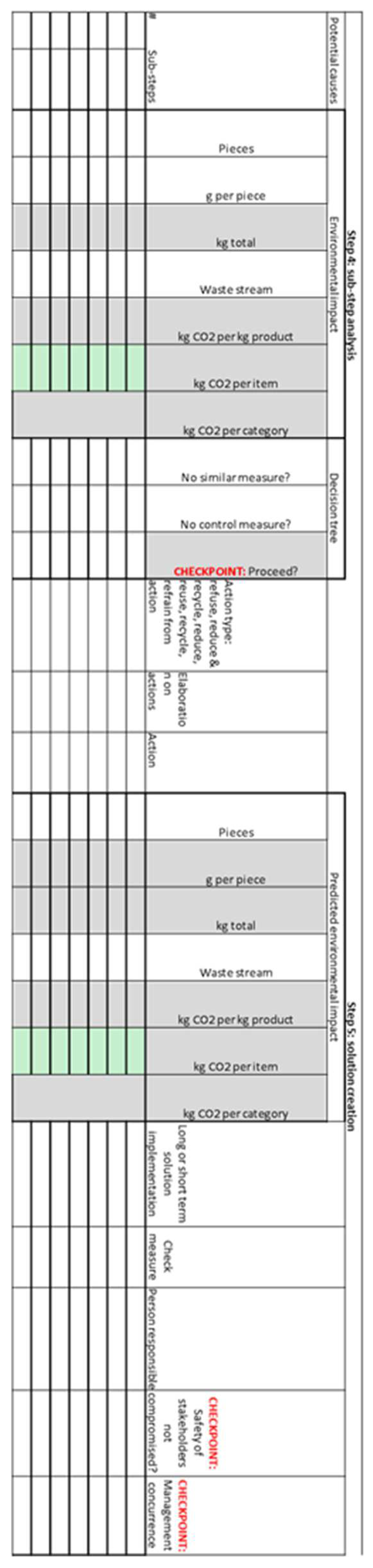
Spreadsheet
All of the calculations for Steps 4 and 5 are conducted in a spreadsheet. For Step 4, the number, weight, and waste stream of the items that are discarded must be entered. The spreadsheet then calculates the carbon footprint of each sub-step, and color-coding is used to indicate whether it represents a carbon hotspot. For Step 5, one of the 6 sustainable solutions must be selected, for which the spreadsheet calculates the new carbon footprint. A screenshot of the spreadsheet is presented in
Appendix A.
2.2. Validation Study
After the HSMEA was designed, it was validated with a group of potential users at the Leiden University Medical Centre (LUMC) to assure it was suitable in a clinical setting. Three sessions of 1.5 h were organized over an eight-week period, in which the HSMEA was finalized for a case study. For the validation sessions, five potential users with different backgrounds were invited. Two medical specialists, one being the leader of the Green Team and the other a specialist regarding the investigated procedures, attended the meetings. Also in attendance was one OR nurse, who was also a member of the Green Team; the head of the sterilization department of the LUMC, as she had extensive experience and knowledge about HFMEA; and lastly, the primary investigator of the study, who was the team leader.
During the first validation session, the HSMEA tool was explained step-by-step to the members of the group on the basis of a fictitious case study by means of a PowerPoint presentation. The topic for the validation session (Step 1) was determined beforehand by the team leader and concerned the reduction of waste generated in the preparation room for a fictional but realistic procedure. In this first session, the team created the flowchart of Step 3 by writing the individual steps on Post-It sticky notes and creating graphical representation of the entire process on a A3 format paper.
At the second validation session, Step 4 and Step 5 of the tool were completed by the team. All the weights and the waste streams of all the pieces that are discarded during the procedure were determined. During the completion of Step 5, several suggestions were made by the team on how this step could be improved. For example, categorizing the solutions as long- or short-term implementation could help the team to have a better overview of the solutions. Furthermore, they suggested that waste handling costs should be implemented as well to provide a more complete overview of the implications of the solutions proposed in Step 5.
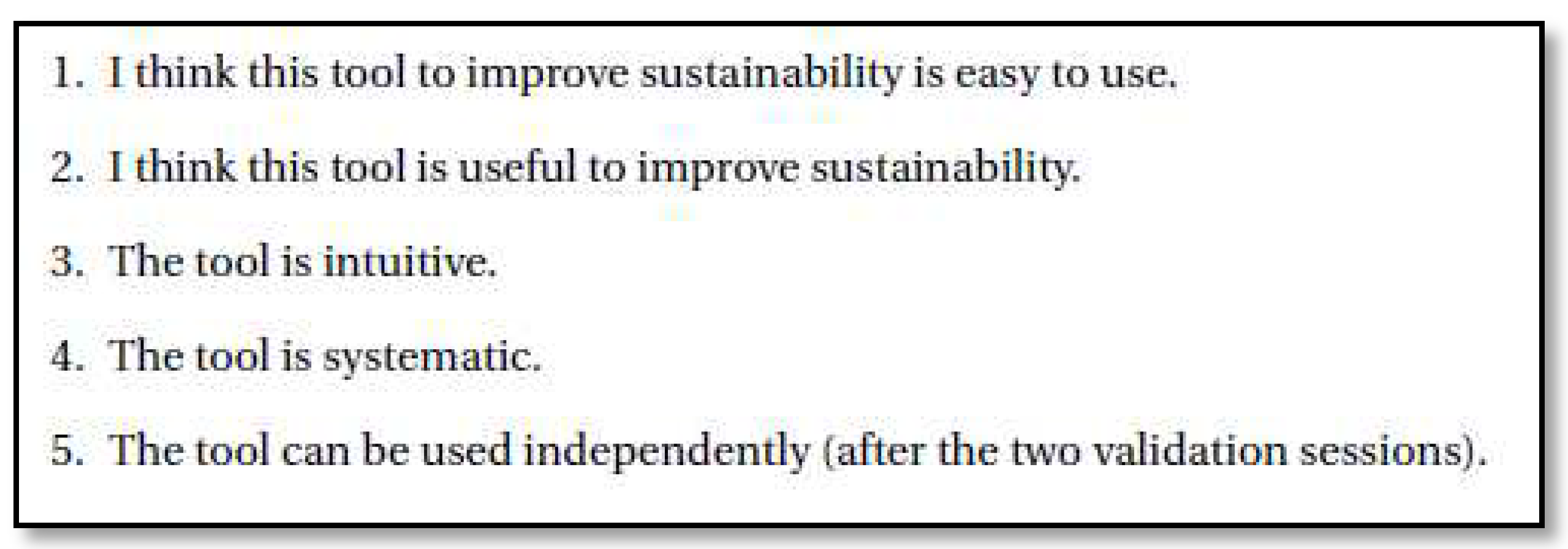
During the third validation session, the fulfilment of the method’s requirements (easy to use, systematic, resulting in improvement of environmental impact) was tested by means of a concise questionnaire. The questions from the survey can be found in
Figure 2. All questions required an answer on a scale from 1–5, with 1 being ‘Do not agree at all’ and 5 being ‘Agree completely’. For every item, an average score of 3.5 was considered as positive fulfilment of the requirement. When a participant gave an item a score of 3 or lower, this was discussed with this participant to find out why this score was awarded and how this could be improved.
Following these validation sessions, a case study was conducted of surgical waste produced in three Cesarean section procedures in a two-week study period to assess the applicability of the HSMEA in a clinical setting.
3. Results
Step 1: Topic definition
For the case study, the topic was defined as: lowering the carbon footprint from the surgical waste generated in the preparation room and OR during a caesarean section. We choose the caesarean section (C-section) for the validation since it is a very common procedure. In LUMC, all members of the OR team were familiar with the procedure and it is highly standardized, which means that there is virtually no variation in the amount of disposable and reusable products used during surgery. This made this operation ideal for investigating whether the HSMEA could improve its environmental sustainability.
Step 2: Team assembly
The team performing the HSMEA consisted of six people: two medical specialists (one being an expert regarding the studied procedure, the other the leader of the OR Green Team), one OR nurse (expert regarding the waste generation process), one manager of the Department of Operating Rooms of the LUMC (expert regarding HFMEA), one coordinator of the waste handling department of the LUMC (expert regarding waste management and recycling), and the project leader.
Step 3: Process flowchart
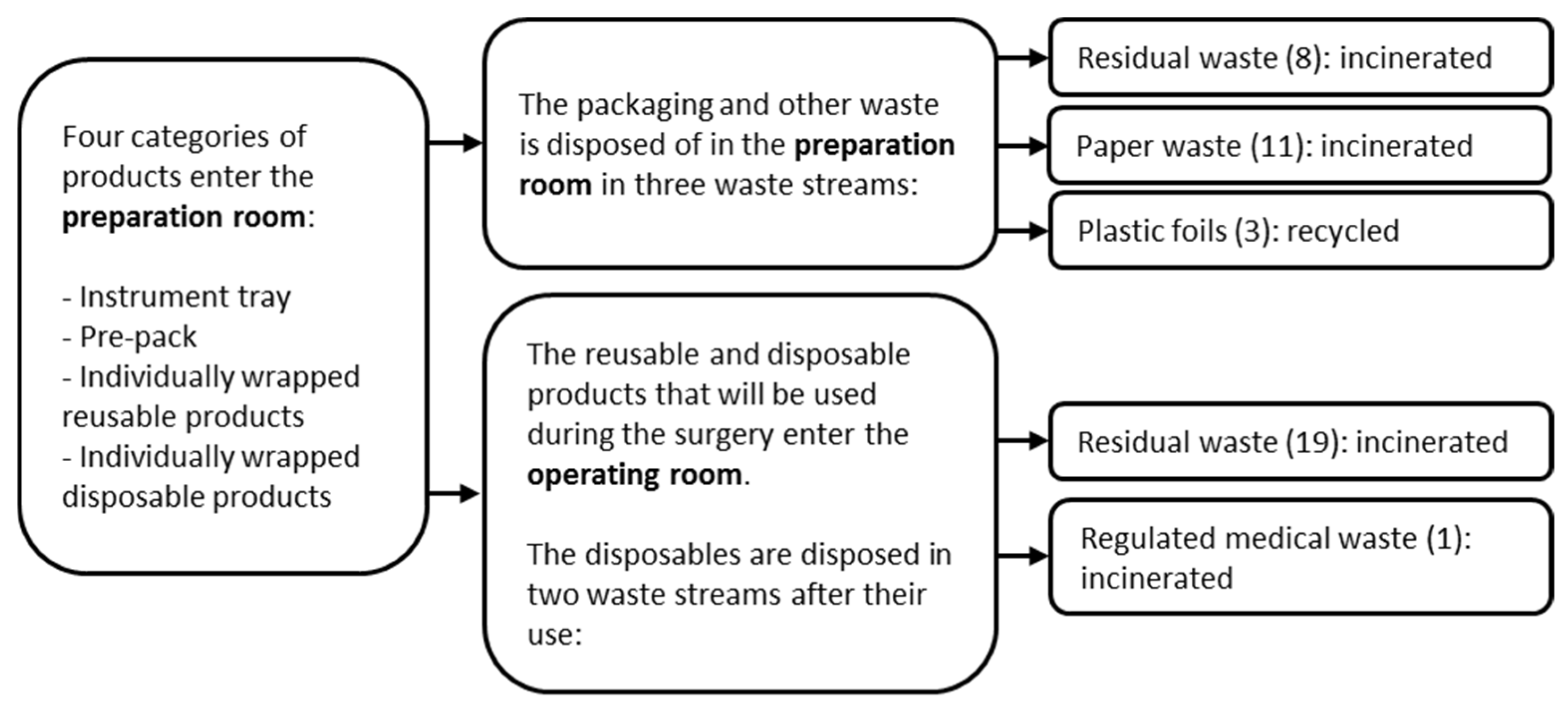
The flowchart, as presented in
Figure 3, was created during the first meeting. Here the waste stream of the identified products was determined. The number of sub-steps (items) that contributed to the generation of each waste stream is indicated in parentheses.
The first block represents the items that are brought into the preparation room. The instrument tray contains the reusable surgical instruments that are used during the procedure. This tray originates from the Central Sterile Supply Department within the hospital and is packed in polypropylene blue wrap. Apart from the instrument tray, a custom pack is used for every C-section. This is a pre-packed tray with sterile disposable items assembled especially for a specific kind of surgery. Furthermore, individually wrapped disposable and reusable products can be collected separately when requested by the surgeon.
The second two blocks represent the preparation room and the OR. In these two areas, waste is allocated to different waste streams. In the preparation room, the packaging of the four categories from block 1 is disposed of. Other waste, such as protection caps or superfluous products, is disposed of here as well. The products that are needed for the surgery are brought into the OR, and they are disposed of inside the OR after use.
Disposal in the preparation room occurs in three separate waste streams (MSW, paper waste, and plastic foils). Twenty-two items were identified that are disposed of in this area. Eight items are disposed of as MSW, which is incinerated. Eleven items are disposed of as paper waste. These items are collected separately but are all treated as MSW by the waste handling company and incinerated. Three items are disposed of as plastic foils and will be recycled. In the OR, most items (19 out of 20) are disposed of as MSW and incinerated. The remaining item is disposed of as Regulated Medical Waste (RMW) and incinerated as well, but at a different waste incineration plant.
Step 4: Hazard analysis
The baseline carbon footprint was calculated for each item by multiplying its weight by the appropriate conversion factor from
Table 3. The amount of waste and emissions created in both the preparation room and the OR for the baseline situation can be found in
Table 4. From these baseline data, hotspots of environmental burden could be identified. In the preparation room, the item with the highest carbon footprint (0.45 kg CO
2-eq) was the polypropylene blue wrap used to package the reusable instrument trays. Its carbon footprint accounts for 48% of all items disposed of in the preparation room. Inside the OR, the disposal of sterile gauzes (2.0 kg CO
2-eq) and the four sterile surgical gowns (2.0 kg CO
2-eq) are responsible for the highest proportion of the carbon footprint of all items disposed of, each representing 19%.
Step 5: Actions and outcome measures
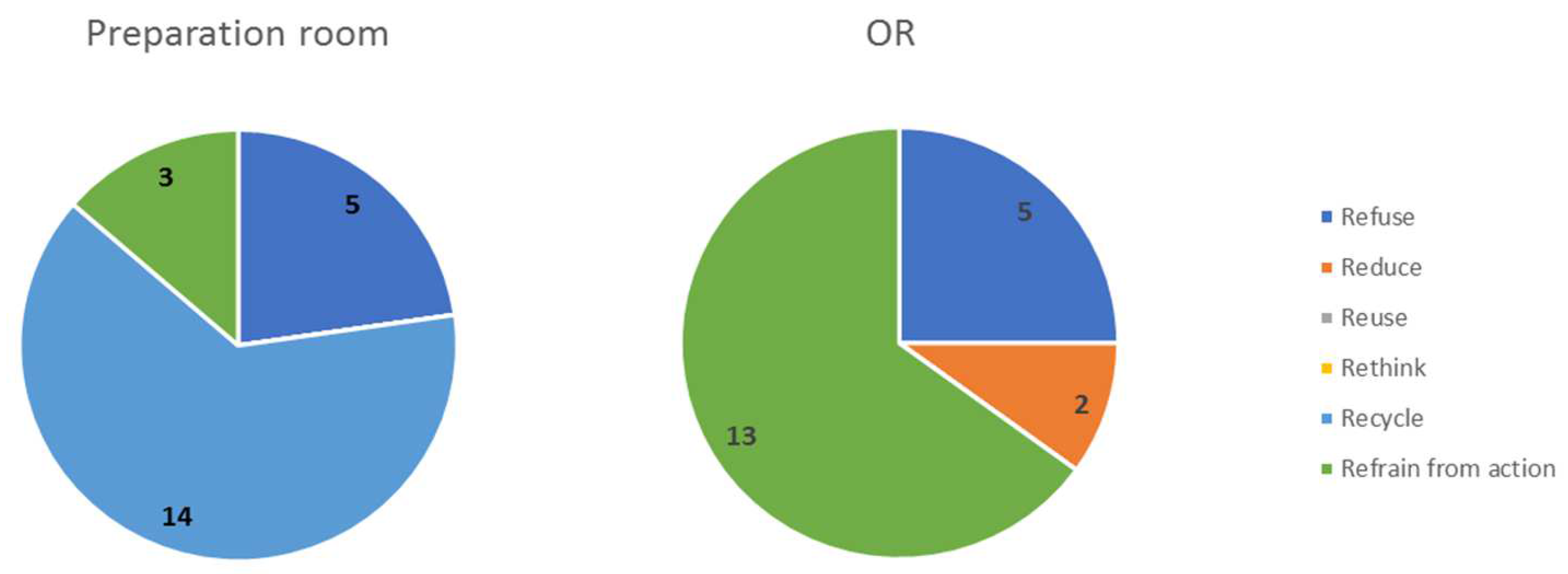
All sub-steps (items) passed through the decision tree (
Figure 1) and were assigned a sustainable solution using the 6 Rs. In the preparation room, 14 items were recycled, and for 8 items there was no sustainable solution possible (‘refuse’/’refrain from action’). In the OR, two items could be ‘reduced’ by leaving them out of the custom pack, and for 18 items no sustainable solution was possible at this time. All solutions were discussed among the team to determine whether they compromise stakeholder safety. This was not the case for any assigned solution. An overview of the sustainable solutions assigned to each sub-step in the preparation room and OR can be found in
Figure 4.
For the polypropylene blue wrap, the sub-step with the highest carbon footprint in the preparation room, the solution ‘refrain from action’ was chosen. The use of this wrapping is necessary in order to maintain the sterility of the instrument tray. The blue wrap is currently not accepted for recycling by the waste handler. The alternative of a reusable rigid container has too many implications for business operations to be a realistic option in the short term.
To the sub-steps with the highest carbon footprint in the OR, the following solutions were assigned. For the disposal of four surgical gowns, the solution ‘reduce’ was chosen. One of these four gowns was disposed of unused. This gown is included in the custom pack in case a fourth assistant (intern) joins the operation. However, this is the fact in only a minority of cases. Therefore, this gown should be removed from the custom pack and wrapped individually for use when an intern is present. Two packages of sterile gauzes were present in the custom pack. For the package of small gauzes, ‘refuse’ was chosen since the 10 large gauzes proved to be sufficient for the entire operation.
The overall result of the implementation of sustainable solutions in the preparation room and the OR for the C-section was a waste reduction of 600 g (−22%) and a carbon footprint reduction of 2.5 kg CO2-eq (−22%).
Practical implications
After the HSMEA was completed, the team started with implementing the proposed recycling solutions into daily practice in the OR department. Now, the paper waste stream is recycled, as is all plastic waste. The different trash bags are consistently color-coded throughout the OR complex. For each trash bag, written instructions are present which aid the personnel with choosing the correct trash bag. In order to improve the workflow, it was decided to collect all types of plastic in one trash bag, instead of collecting every type of plastic separately (e.g., plastic foils, hard plastics). This was deemed the most appropriate solution in this situation after consultation with operating nurses and the waste handling department. Now, a waste collection station with three trash bags is present in the preparation room, collecting paper, plastic, and MSW.
Revising the custom pack was identified as having a major environmental impact for both the preparation room and the OR. Of the total CO2-footprint reduction, 98% was attributable to the revision of the custom pack, while only 2% resulted from paper and plastic recycling. The custom pack revision included the removal of 11 items that that turned out to be superfluous. Two items that were always used during the operation but were delivered separately were added to the package, which meant less packaging material was needed.
HSMEA user feedback
For survey questions 1 (I think this tool to improve sustainability is easy to use), 2 (I think this tool is useful to improve sustainability), and 4 (The tool is systematic), the participants scored an average of more than 3.5 out of 5, which was interpreted as a sign of a positive fulfilment of the tool’s requirement. On the question of whether this tool was intuitive, respondents answered with an average score of 3.3 (range 3–4). To improve this, the spreadsheet was modified in a number of respects in consultation with the users. When asked whether the tool could be used independently in a subsequent HSMEA, the average score was 2.5 (grades 1–4). The most important factor here was that the team leader should be familiar with the HSMEA tool. A possible solution was to educate someone from the LUMC to be a process leader for HSMEAs.
4. Discussion
Healthcare waste and its disposal cause pollution and consequently pose health risks that may result in disease and premature death [
5,
6]. The fact that operating rooms are responsible for up to 33% of all hospital solid waste makes this an important issue to address [
8]. Addressing this problem of healthcare waste requires quantifying its impact on the environment and finding solutions to reduce it.
To address the primary research question of this study, it was found that it was possible to successfully transform a method of identifying hazards in healthcare processes (HFMEA) into the novel HSMEA to quantify and systematically reduce the carbon hotpots of healthcare waste. In the first three steps, the topic is specified, a multidisciplinary team is assembled, and the generated waste is accurately mapped. In the fourth step, the original hazard analysis of the HFMEA is replaced by an environmental hazard calculation based on the carbon footprint of waste streams. Identifying carbon footprint hotspots makes it possible to focus on projects that will yield the most potent effect in reduction initiatives. In the last step, sustainable solutions are applied by preventing the generation of waste (refuse, reduce, reuse, rethink) or by depositing the waste in a waste stream with a lower carbon footprint (recycle).
To assess the applicability of the HSMEA, and in doing so answer the secondary research question, a caesarean section was used as a template to reduce the carbon footprint of surgical waste generated during this procedure. Several carbon footprint hotspots were identified during the sub-step analysis of the surgical C-section waste. The most environmentally harmful item in the preparation room was the blue wrap that is used to pack surgical instruments. The use of blue wrap as packaging material for sterile surgical instruments is known to be a major contributor to OR waste. Estimates are that 115 million kilograms of blue wrap is discarded on a yearly basis in the US alone [
21]. It is a multilayer non-woven packaging material made from polypropylene that is used in many sterilization departments in the world. After unpacking sterile surgical instruments blue wrap packaging is discarded, making up 11.5% of total OR waste [
10]. We were not able to find a sustainable solution in our hospital for blue wrap, which was a carbon footprint hotspot in the preparation room waste. Possible solutions are recycling blue wrap, or the use of a reusable rigid container that can be considered as a packaging system for sterile instruments [
22].
In the operating room itself, cotton gauzes and disposable surgical gowns that were in the custom pack caused the most environmental burden. Polypropylene is the most common material of disposables used in custom packs for operations. However, when the life cycle of the items in disposables custom packs for a traditional vaginal childbirth were studied, cotton gauzes were found to have the biggest environmental impact [
18]. Adjusting the composition of the custom pack yielded by far the greatest environmental gain in our HSMEA of the C-section (98%), which involved removing unnecessary items such as small cotton gauzes and a spare disposable surgical gown.
During the process of solution creation, it became clear that recycling had only a very limited impact on the reduction of the carbon footprint of surgical waste generation. Inside the OR, recycling was not a solution due to the risk of contamination with infectious materials. In the preparation room, even though recycling was 14 out of 21 times the chosen solution, it was only responsible for 2 percent of the overall reduction in carbon footprint. Recycling is an important way to ensure that raw materials are not wasted in a circular economy. However, recycling is difficult to achieve in an OR setting with potential infectious waste. Also, it is much better to ensure that waste is not created in the first place by refusing, reducing, reusing, and rethinking materials.
In their systematic evaluation of user feedback from 13 HFMEA analyses, Habraken et al. showed that its multidisciplinary, systematic, and stepwise approach, which are also tenets underlying the HSMEA, are the strengths of this method [
31]. As a result, this method provides insight into the entire process from different perspectives and is very detailed and comprehensive. User feedback showed that the HSMEA is perceived as a systematic approach that is easy to use and promotes sustainability. However, when asked if a subsequent project could be conducted independently, the HSMEA scored less than desired. The importance of having a skilled and effective the team leader has also been mentioned previously in evaluations of the HFMEA. A facilitator with knowledge and overview of the process is critical to the success of HFMEA [
31,
32].
The weakness of the HSMEA, like its predecessor (HFMEA), lies in the fact that is a resource-intensive and time-consuming method. The case study of the C-section involved six healthcare professionals who completed three one-and-a-half hour sessions with each other. These drawbacks are also known issues with the HFMEA and must be weighed against the aforementioned benefits [
31].
Limitations
In order to make the HSMEA method broad and easy to apply, a number of shortcomings of the carbon footprint tool have been accepted. Firstly, only the global warming potential (carbon footprint) is calculated and all other environmental effects like acidification, eutrophication etc., as well as materials depletion, are not taken into account. The advantage of expressing environmental damage in the form of a carbon footprint is that it is a concept that has become understandable to the general public. Secondly, the carbon footprint was calculated from waste streams instead of doing Life Cycle Assessments of all materials present. The latter is an extremely long and labor-intensive process compared to the identification and weighing of waste. Using DEFRA greenhouse gas life cycle conversion factors for waste disposal is permitted, as the majority of OR waste is composed of a mixture of different plastics [
9]. The HSMEA analysis could be supplemented by other methods that do take the aforementioned factors into account by performing a Life Cycle Assessment with, for example, ReCiPe 2016 [
36]. However, this will be at the expense of user friendliness, while the present results appear to be in line with previous studies [
18].
In the validation study, we did not include all waste generated during the C-section, as anesthetic waste was not taken into account. Waste from anesthetic practice contributes substantially to OR waste. McGain et al. showed that 25% of total operating room waste came from anesthesia [
37]. In the future application of the HSMEA, however, this can certainly be included in the research given the similarities in the materials found in both surgical and anesthetic waste.
Another possible limitation is that the validation was limited to the C-section. This procedure was selected because it is always performed in the same way at the LUMC and therefore there is little or no variation in waste production. When different surgeries are studied, more waste audits will be needed to ensure a good understanding of the waste produced. However, this should not be an obstacle to applying this newly introduced method.
Future research
One strength of the HSMEA lies in the structured analysis and quantification of the environmental impact of a process by a multidisciplinary team, after which sustainable solutions are sought for carbon hotspots. Future research should focus, in addition to OR waste, on the application of HSMEA to other resource-intensive areas of healthcare, such as the Intensive Care, Cath labs, and Dialysis units.
Apart from application to waste from other hospital departments, this method could also be used in areas such as water and electricity savings. Specific topics such as, for example, water consumption for hand washing can be the subject of a HSMEA. The process can be mapped and the various sustainable solutions to save water (water saving taps, critical appraisal of the handwashing protocol, etc.) investigated, implemented, and its environmental benefits quantified. Similarly, energy consumption in the OR department, or any other section of the hospital, can be chosen as a topic with energy-saving measures or the use of renewable energy as sustainable solutions.