Association between Atrial Fibrillation Incidence and Temperatures, Wind Scale and Air Quality: An Exploratory Study for Shanghai and Kunming
Abstract
1. Introduction
2. Literature Review and Research Gap
3. Materials and Methods
3.1. Data Collection and Resources
3.2. Research Logic and Data Curation
3.3. Binary Logistic Regression
3.4. Model Tests
4. Results
4.1. Qualitative Models’ Results
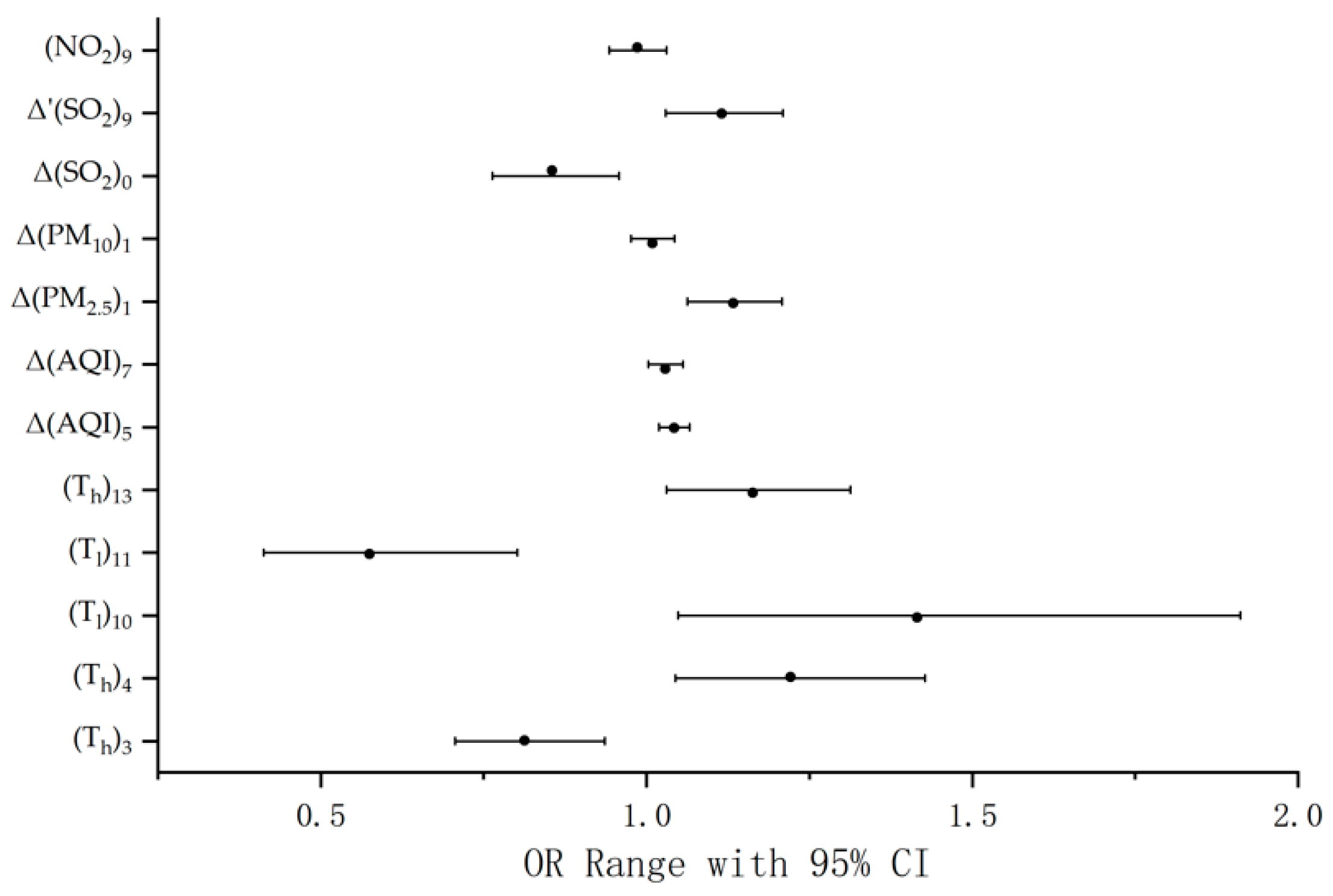
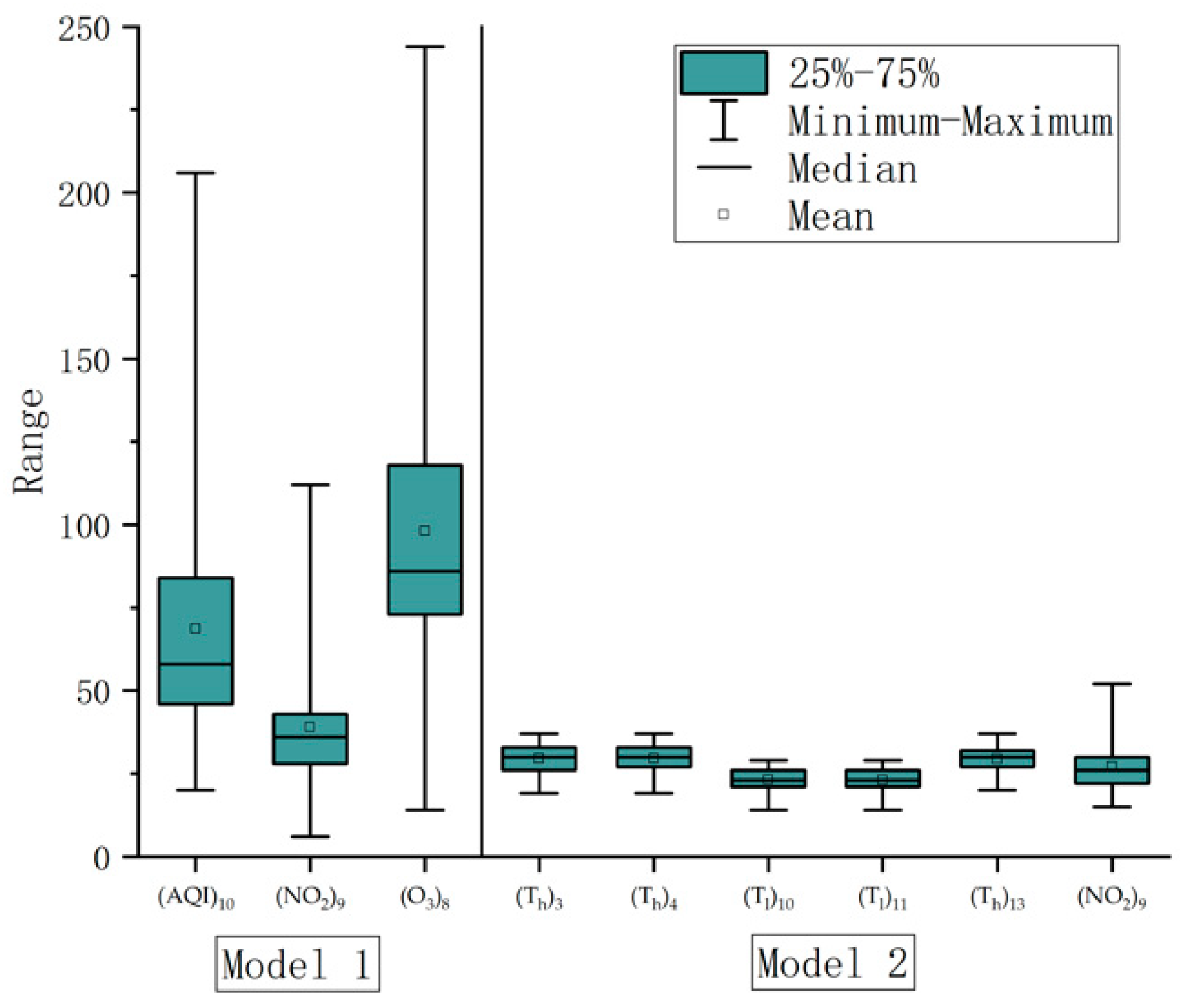
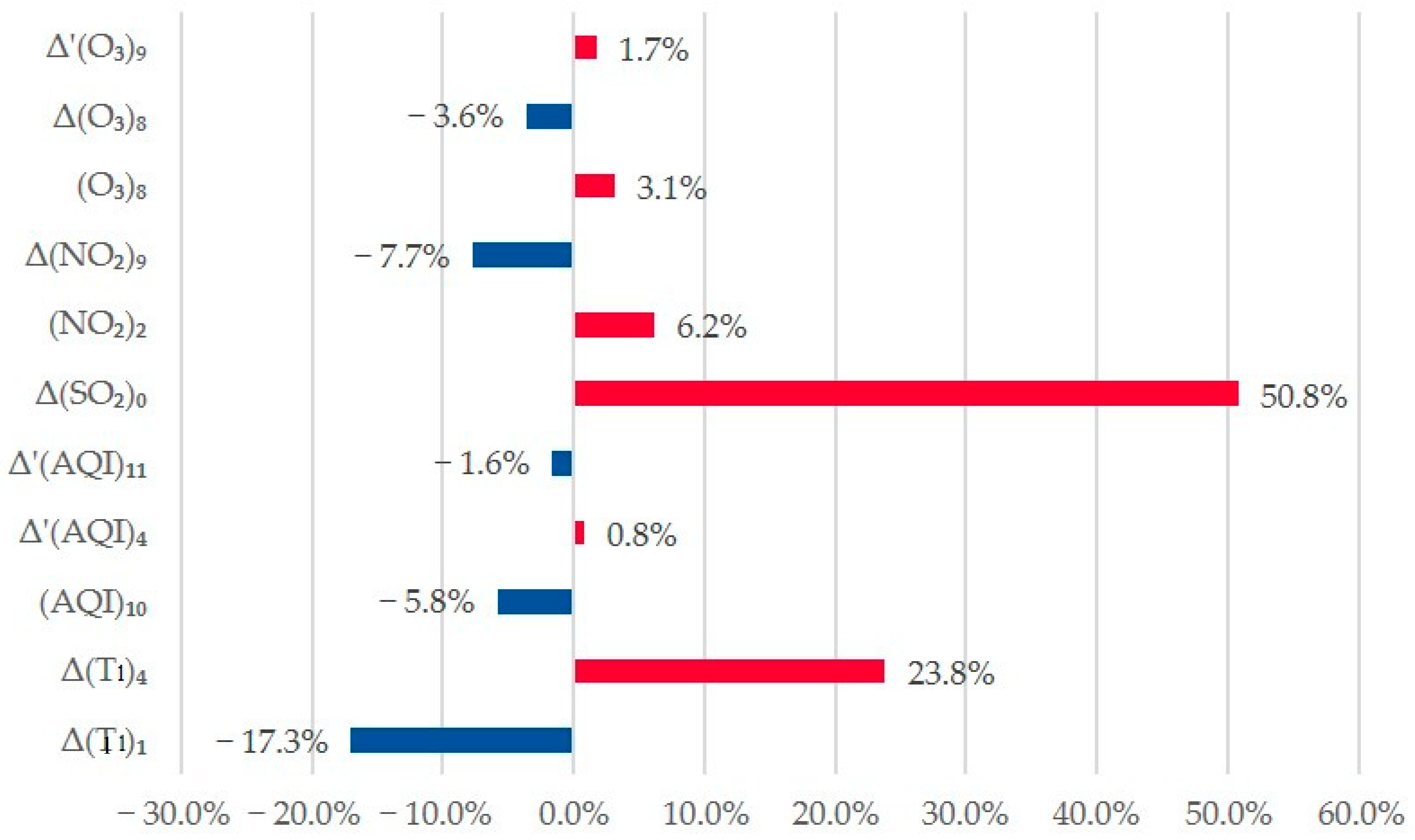
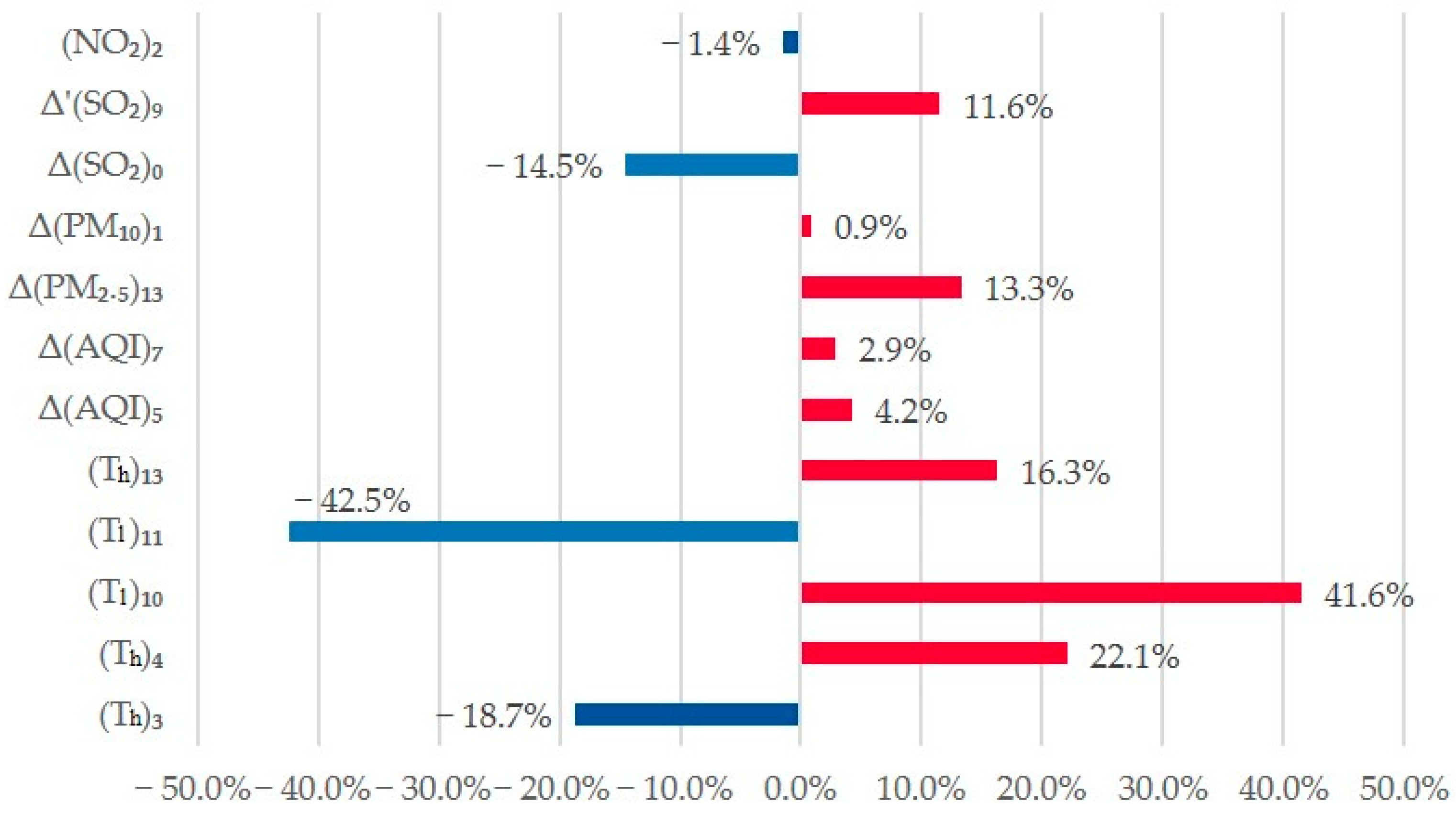
4.2. Quantitative Models Results
4.3. Epidemicical Results
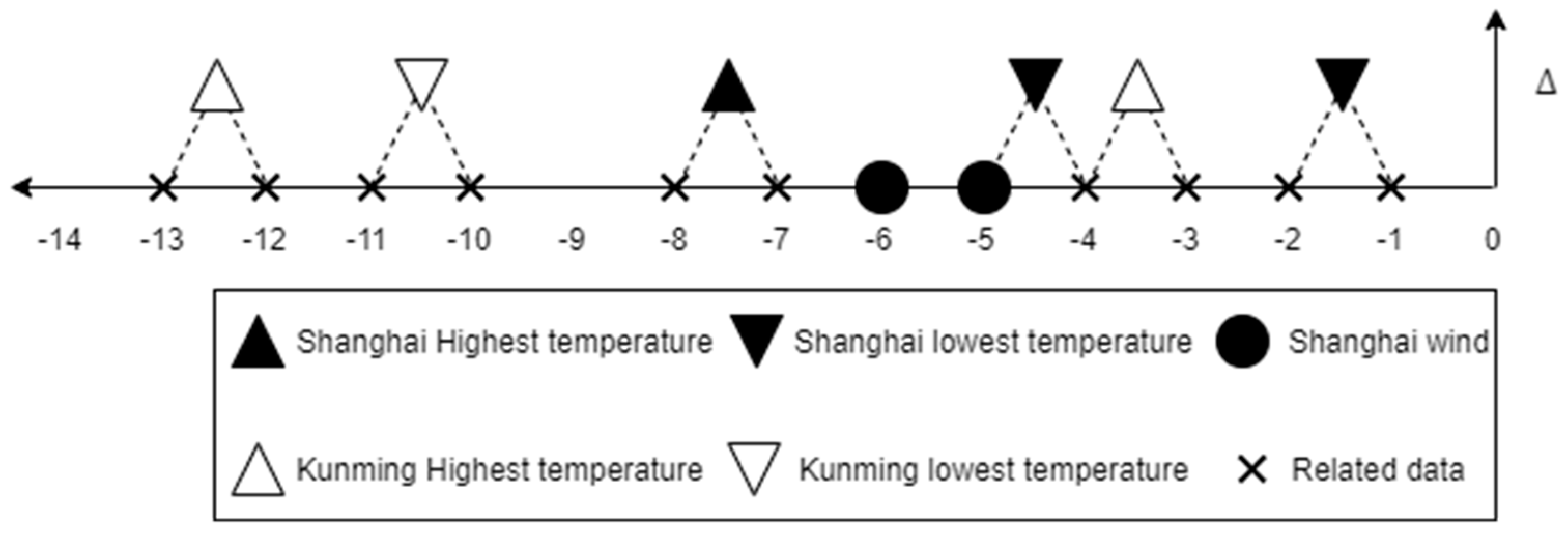
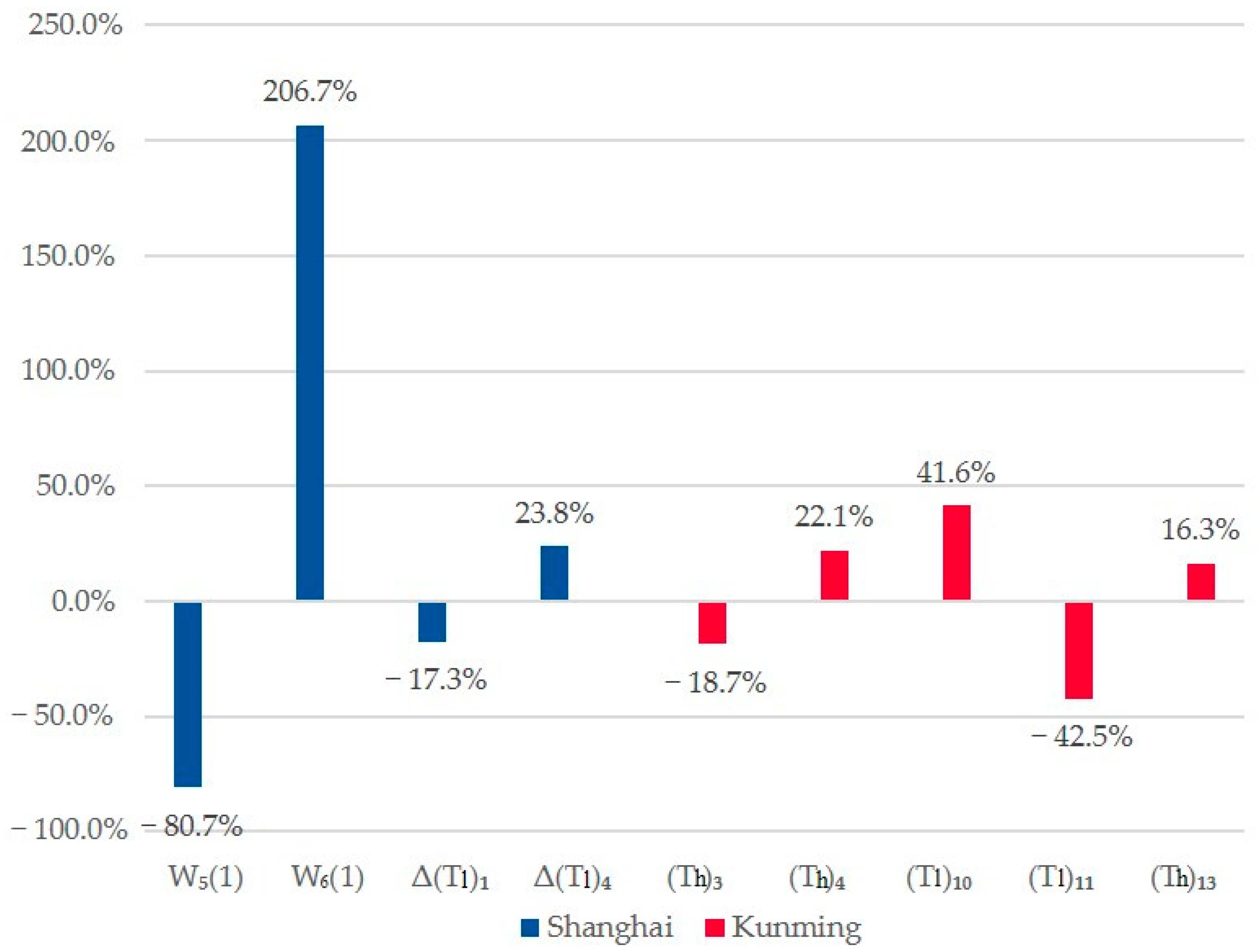
4.4. Geographical Results
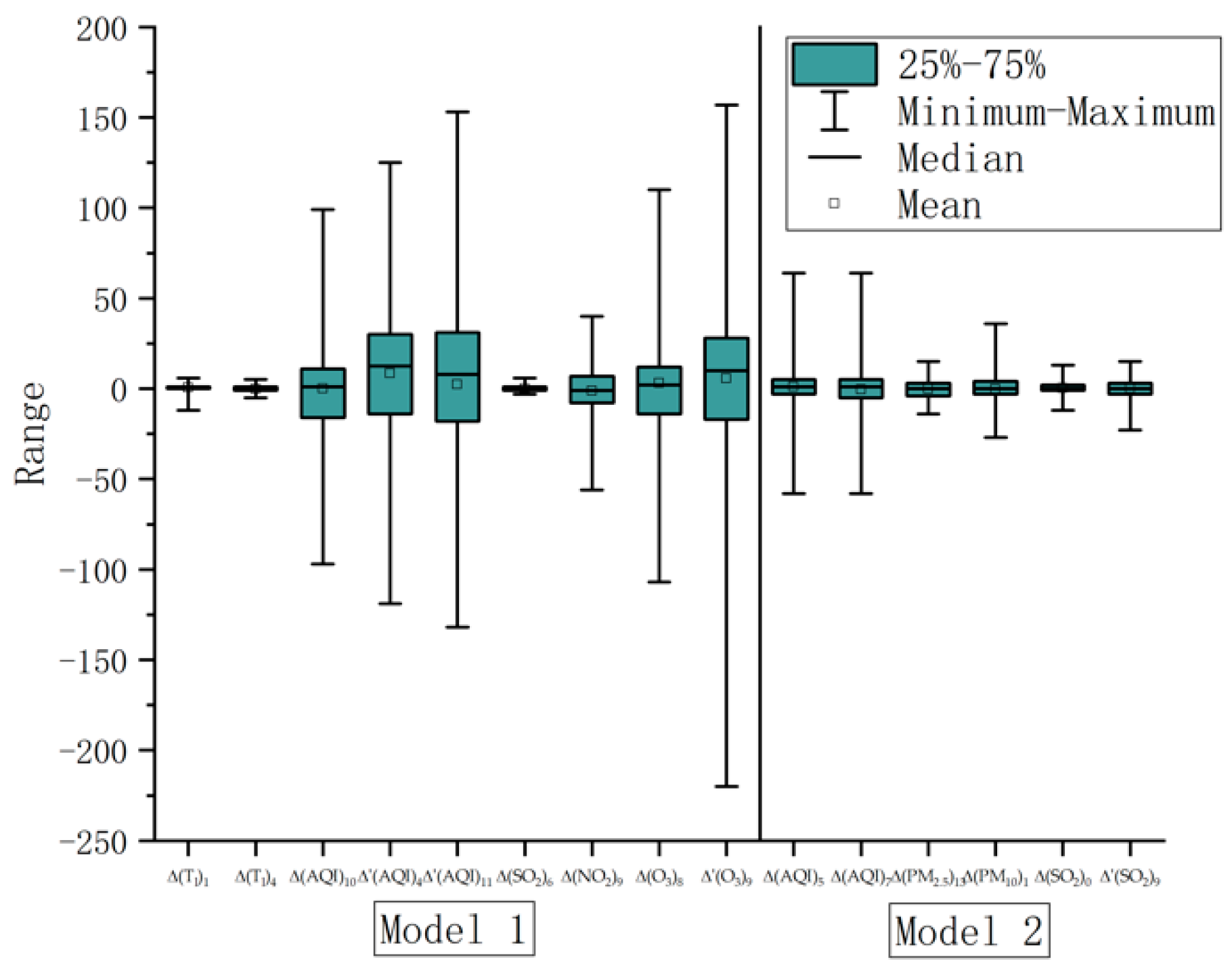
4.5. Pollution’s Lag-Pattern Impact
5. Discussion
5.1. The Influence of Air Pollution Factors on AF
5.2. AF Risk Factors Are Variable in Different Cities
5.3. The Impact’s Lag-Affect Pattern
5.4. Research Significance, Limitations and Prospects
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Description | Variables | Shanghai | Kunming | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β 1 | Std. 2 | Sig. 3 | OR | OR 4 95% CI | β | Std. | Sig. | OR | OR 4 95% CI | ||||
| Lower Bound | Upper Bound | Lower Bound | Upper Bound | ||||||||||
| Wind | W5(1) | −2.900 | 0.760 | 0.000 | 0.055 | 0.012 | 0.244 | ||||||
| W6(1) | 2.498 | 0.552 | 0.000 | 12.162 | 4.119 | 35.917 | |||||||
| Temperature | Δ(Tl)1 | −1.213 | 0.439 | 0.006 | 0.297 | 0.126 | 0.703 | ||||||
| Δ(Tl)4 | 1.999 | 0.455 | 0.000 | 7.378 | 3.022 | 18.013 | |||||||
| (Th)7 | 1.662 | 0.454 | 0.000 | 5.267 | 2.162 | 12.833 | |||||||
| Δ(Th)3 | −0.906 | 0.370 | 0.014 | 0.404 | 0.196 | 0.835 | |||||||
| Δ(Tl)10 | 1.095 | 0.336 | 0.001 | 2.988 | 1.545 | 5.777 | |||||||
| Δ(Th)12 | −1.983 | 0.541 | 0.000 | 0.138 | 0.048 | 0.397 | |||||||
| AQI | Δ(AQI)5 | 0.763 | 0.309 | 0.014 | 2.144 | 1.170 | 3.928 | ||||||
| Δ(AQI)7 | −1.105 | 0.346 | 0.001 | 0.331 | 0.168 | 0.652 | |||||||
| Δ(AQI)12 | −1.857 | 0.453 | 0.000 | 0.156 | 0.064 | 0.379 | |||||||
| Δ′(AQI)4 | 1.935 | 0.445 | 0.000 | 6.925 | 2.893 | 16.578 | |||||||
| Δ′(AQI)11 | −1.834 | 0.477 | 0.000 | 0.160 | 0.063 | 0.407 | |||||||
| TSP | Δ(PM2.5)5 | 0.926 | 0.422 | 0.028 | 2.525 | 1.105 | 5.770 | ||||||
| Δ(PM2.5)13 | 0.827 | 0.316 | 0.009 | 2.285 | 1.230 | 4.246 | |||||||
| Δ′(PM10)2 | 0.770 | 0.345 | 0.026 | 2.160 | 1.098 | 4.248 | |||||||
| SO2 | Δ(SO2)0 | −1.156 | 0.372 | 0.002 | 0.315 | 0.152 | 0.652 | ||||||
| Δ(SO2)10 | 1.305 | 0.424 | 0.002 | 3.686 | 1.606 | 8.457 | |||||||
| Δ′(SO2)7 | 1.960 | 0.416 | 0.000 | 7.102 | 3.142 | 16.056 | |||||||
| Δ′(SO2)9 | 0.763 | 0.345 | 0.027 | 2.145 | 1.091 | 4.218 | |||||||
| NO2 | Δ(NO2)9 | −1.264 | 0.349 | 0.000 | 0.283 | 0.143 | 0.560 | ||||||
| Δ′(NO2)10 | −1.419 | 0.430 | 0.001 | 0.242 | 0.104 | 0.562 | |||||||
| O3 | Δ′(O3)9 | 0.913 | 0.425 | 0.032 | 2.491 | 1.083 | 5.726 | ||||||
| Δ′(O3)12 | −1.363 | 0.437 | 0.002 | 0.256 | 0.109 | 0.603 | |||||||
| Constant | c | −4.222 | 0.854 | 0.000 | 0.015 | −3.773 | 0.579 | 0.000 | 0.023 | ||||
References
- Camm, A.J.; Kirchhof, P.; Lip, G.Y.H.; Schotten, U.; Savelieva, I.; Ernst, S.; Van Gelder, I.C.; Al Attar, N.; Hindricks, G.; Prendergast, B.; et al. Guidelines for the management of atrial fibrillation: The Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur. Heart J. 2010, 31, 2369–2429. [Google Scholar]
- Guo, Y.; Tian, Y.; Wang, H.; Si, Q.; Wang, Y.; Lip, G.Y.H. Prevalence, incidence, and lifetime risk of atrial fibrillation in China: New insights into the global burden of atrial fibrillation. Chest 2015, 147, 109–119. [Google Scholar] [CrossRef]
- Wang, Z.; Chen, Z.; Wang, X.; Zhang, L.; Li, S.; Tian, Y.; Shao, L.; Hu, H.; Gao, R. The Disease Burden of Atrial Fibrillation in China from a National Cross-sectional Survey. Am. J. Cardiol. 2018, 122, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Hu, D. An epidemiological study on the prevalence of atrial fibrillation in the Chinese population of mainland China. J. Epidemiol. 2008, 18, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Friberg, L.; Rosenqvist, M.; Lip, G.Y.H. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: The Swedish Atrial Fibrillation cohort study. Eur. Heart J. 2012, 33, 1500–1510. [Google Scholar] [CrossRef]
- Gao, H.; Yang, W.; Wang, J.; Zheng, X. Analysis of the Effectiveness of Air Pollution Control Policies based on Historical Evaluation and Deep Learning Forecast: A Case Study of Chengdu-Chongqing Region in China. Sustainability 2021, 13, 206. [Google Scholar] [CrossRef]
- Liu, H.; Liu, J.; Yang, W.; Chen, J.; Zhu, M. Analysis and Prediction of Land Use in Beijing-Tianjin-Hebei Region: A Study Based on the Improved Convolutional Neural Network Model. Sustainability 2020, 12, 3002. [Google Scholar] [CrossRef]
- Andrew, N.E.; Thrift, A.G.; Cadilhac, D.A. The prevalence, impact and economic implications of atrial fibrillation in stroke: What progress has been made? Neuroepidemiology 2013, 40, 227–239. [Google Scholar] [CrossRef]
- Kim, H.; Kim, Y.; Hong, Y.-C. The lag-effect pattern in the relationship of particulate air pollution to daily mortality in Seoul, Korea. Int. J. Biometeorol. 2003, 48, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Khajavi, A.; Khalili, D.; Azizi, F.; Hadaegh, F. Impact of temperature and air pollution on cardiovascular disease and death in Iran: A 15-year follow-up of Tehran Lipid and Glucose Study. Sci. Total Environ. 2019, 661, 243–250. [Google Scholar] [CrossRef]
- Shen, X.; Yang, W.; Sun, S. Analysis of the Impact of China’s Hierarchical Medical System and Online Appointment Diagnosis System on the Sustainable Development of Public Health: A Case Study of Shanghai. Sustainability 2019, 11, 6564. [Google Scholar] [CrossRef]
- Li, Y.; Yang, W.; Shen, X.; Yuan, G.; Wang, J. Water environment management and performance evaluation in central China: A research based on comprehensive evaluation system. Water 2019, 11, 2472. [Google Scholar] [CrossRef]
- Yang, W.; Yuan, G.; Han, J. Is China’s air pollution control policy effective? Evidence from Yangtze River Delta cities. J. Clean. Prod. 2019, 220, 110–133. [Google Scholar] [CrossRef]
- Jiang, B.; Li, Y.; Yang, W. Evaluation and Treatment Analysis of Air Quality Including Particulate Pollutants: A Case Study of Shandong Province, China. Int. J. Environ. Res. Public Health 2020, 17, 9476. [Google Scholar] [CrossRef] [PubMed]
- Wordley, J.; Walters, S.; Ayres, J.G. Short term variations in hospital admissions and mortality and particulate air pollution. Occup. Environ. Med. 1997, 54, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Sun, Q.; Hong, X.; Wold, L.E. Cardiovascular Effects of Ambient Particulate Air Pollution Exposure. Circulation 2010, 121, 2755–2765. [Google Scholar] [CrossRef] [PubMed]
- Balakrishnan, K.; Dey, S.; Gupta, T.; Dhaliwal, R.S.; Brauer, M.; Cohen, A.J.; Stanaway, J.D.; Beig, G.; Joshi, T.K.; Aggarwal, A.N.; et al. The impact of air pollution on deaths, disease burden, and life expectancy across the states of India: The Global Burden of Disease Study 2017. Lancet Planet. Health 2019, 3, e26–e39. [Google Scholar] [CrossRef]
- Newell, K.; Kartsonaki, C.; Lam, K.B.H.; Kurmi, O.P. Cardiorespiratory health effects of particulate ambient air pollution exposure in low-income and middle-income countries: A systematic review and meta-analysis. Lancet Planet. Health 2017, 1, e360–e367. [Google Scholar] [CrossRef]
- Neophytou, A.M.; Yiallouros, P.; Coull, B.A.; Kleanthous, S.; Pavlou, P.; Pashiardis, S.; Dockery, D.W.; Koutrakis, P.; Laden, F. Particulate matter concentrations during desert dust outbreaks and daily mortality in Nicosia, Cyprus. J. Expo. Sci. Environ. Epidemiol. 2013, 23, 275–280. [Google Scholar] [CrossRef]
- Kim, H.; Kim, J.; Kim, S.; Kang, S.; Kim, H.; Kim, H.; Heo, J.; Yi, S.; Kim, K.; Youn, T.; et al. Cardiovascular Effects of Long-Term Exposure to Air Pollution: A Population-Based Study With 900 845 Person-Years of Follow-up. J. Am. Heart Assoc. 2017, 6, e007170. [Google Scholar] [CrossRef] [PubMed]
- Brook, R.D.; Rajagopalan, S.; Pope, C.A., 3rd; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A.; et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 2010, 121, 2331–2378. [Google Scholar] [CrossRef] [PubMed]
- Kim, I.; Yang, P.; Lee, J.; Yu, H.T.; Kim, T.; Uhm, J.; Pak, H.; Lee, M.; Joung, B. Long-term exposure of fine particulate matter air pollution and incident atrial fibrillation in the general population: A nationwide cohort study. Int. J. Cardiol. 2019, 283, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Qian, Z.; Howard, S.W.; Vaughn, M.G.; Fan, S.; Liu, K.; Dong, G. Global association between ambient air pollution and blood pressure: A systematic review and meta-analysis. Environ. Pollut. 2018, 235, 576–588. [Google Scholar] [CrossRef]
- Chen, R.; Yin, P.; Meng, X.; Liu, C.; Wang, L.; Xu, X.; Ross, J.A.; Tse, L.A.; Zhao, Z.; Kan, H.; et al. Fine Particulate Air Pollution and Daily Mortality. A Nationwide Analysis in 272 Chinese Cities. Am. J. Respir. Crit. Care Med. 2017, 196, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Liu, C.; Meng, X.; Niu, Y.; Lin, Z.; Liu, Y.; Liu, J.; Qi, J.; You, J.; Tse, L.A.; et al. Associations between short-term exposure to ambient sulfur dioxide and increased cause-specific mortality in 272 Chinese cities. Environ. Int. 2018, 117, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Yin, P.; Chen, R.; Meng, X.; Wang, L.; Niu, Y.; Lin, Z.; Liu, Y.; Liu, J.; Qi, J.; et al. Ambient carbon monoxide and cardiovascular mortality: A nationwide time-series analysis in 272 cities in China. Lancet Planet. Health 2018, 2, e12–e18. [Google Scholar] [CrossRef]
- Chen, R.; Yin, P.; Meng, X.; Wang, L.; Liu, C.; Niu, Y.; Lin, Z.; Liu, Y.; Liu, J.; Qi, J.; et al. Associations Between Ambient Nitrogen Dioxide and Daily Cause-specific Mortality: Evidence from 272 Chinese Cities. Epidemiology 2018, 29, 482–489. [Google Scholar] [CrossRef] [PubMed]
- Yin, P.; Chen, R.; Wang, L.; Meng, X.; Liu, C.; Niu, Y.; Lin, Z.; Liu, Y.; Liu, J.; Qi, J.; et al. Ambient Ozone Pollution and Daily Mortality: A Nationwide Study in 272 Chinese Cities. Environ. Health Perspect. 2017, 125, 117006. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Peel, J.L.; Hannigan, M.P.; Dutton, S.J.; Sheppard, L.; Clark, M.L.; Vedal, S. The temporal lag structure of short-term associations of fine particulate matter chemical constituents and cardiovascular and respiratory hospitalisations. Environ. Health Perspect. 2012, 120, 1094–1099. [Google Scholar] [CrossRef]
- Staniswalis, J.G.; Yang, H.; Li, W.; Kelly, K.E. Using a continuous time lag to determine the associations between ambient PM2.5 hourly levels and daily mortality. J. Air Waste Manag. Assoc. 2009, 59, 1173–1185. [Google Scholar] [CrossRef]
- Ma, Y.; Zhang, H.; Zhao, Y.; Zhou, J.; Yang, S.; Zheng, X.; Wang, S. Short-term effects of air pollution on daily hospital admissions for cardiovascular diseases in western China. Environ. Sci. Pollut. Res. 2017, 24, 14071–14079. [Google Scholar] [CrossRef]
- Su, C.; Breitner, S.; Schneider, A.; Liu, L.; Franck, U.; Peters, A.; Pan, X. Short-term effects of fine particulate air pollution on cardiovascular hospital emergency room visits: A time-series study in Beijing, China. Int. Arch. Occup. Environ. Health 2016, 89, 641–657. [Google Scholar] [CrossRef] [PubMed]
- Ghanizadeh, G.; Heidari, M.; Seifi, B.; Jafari, H.; Pakjouei, S. The effect of climate change on cardiopulmonary disease—A systematic review. J. Clin. Diagn. Res 2017, 11, IE01–IE04. [Google Scholar] [CrossRef]
- Das, D.; Bakal, J.A.; Westerhout, C.M.; Hernandez, A.F.; O’Connor, C.M.; Atar, D.; McMurray, J.J.V.; Armstrong, P.W.; Ezekowitz, J.A. The association between meteorological events and acute heart failure: New insights from ASCEND-HF. Int. J. Cardiol. 2014, 177, 819–824. [Google Scholar] [CrossRef]
- Guzder, R.N.; Gatling, W.; Mullee, M.A.; Byrne, C.D. Impact of metabolic syndrome criteria on cardiovascular disease risk in people with newly diagnosed type 2 diabetes. Diabetologia 2006, 49, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Amiri, M.; Majid, H.A.; Hairi, F.; Thangiah, N.; Bulgiba, A.; Su, T.T. Prevalence and determinants of cardiovascular disease risk factors among the residents of urban community housing projects in Malaysia. BMC Public Health 2014, 14 (Suppl. 3), S3. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Yang, W.; Chen, H.; Li, Y. China’s energy whistleblowing and energy supervision policy: An evolutionary game perspective. Energy 2020, 213, 118774. [Google Scholar] [CrossRef]
- Bhatnagar, A. Cardiovascular pathophysiology of environmental pollutants. Am J Physiol. Heart Circ. Physiol. 2004, 286, H479. [Google Scholar] [CrossRef] [PubMed]
- Tertre, A.L.; Medina, S.; Samoli, E.; Forsberg, B.; Katsouyanni, K. Short-term effects of particulate air pollution on cardiovascular diseases in eight european cities. J. Epidemiol. Community Health 2002, 56, 773–779. [Google Scholar] [CrossRef]
- Münzel, T.; Steven, S.; Frenis, K.; Hahad, O.; Daiber, A. Environmental factors such as noise and air pollution and vascular disease. Antioxid. Redox Signal. 2020, 33, 581–601. [Google Scholar] [CrossRef]
- Chin, M.T. Basic mechanisms for adverse cardiovascular events associated with air pollution. Heart 2015, 101, 253–256. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Yang, Y. Research on Air Pollution Control in China: From the Perspective of Quadrilateral Evolutionary Games. Sustainability 2020, 12, 1756. [Google Scholar] [CrossRef]
- Khorasani, Z.M.; Bagheri, R.K.; Yaghoubi, M.A.; Chobkar, S.; Aghaee, M.A.; Abbaszadegan, M.R.; Sahebkar, A. The association between serum irisin levels and cardiovascular disease in diabetic patients. Diabetes Metab. Syndr. 2019, 13, 786–790. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.X.; Li, L.G. Efficiency evaluation of industrial waste gas control in China: A study based on data envelopment analysis (DEA) model. J. Clean. Prod. 2018, 179, 1–11. [Google Scholar] [CrossRef]
- Ware, L.J.; Rennie, K.L.; Kruger, H.S.; Kruger, I.M.; Greeff, M.; Fourie, C.M.T.; Huisman, H.W.; Scheepers, J.D.W.; Uys, A.S.; Kruger, R.; et al. Evaluation of waist-to-height ratio to predict 5 year cardiometabolic risk in sub-Saharan African adults. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 900–907. [Google Scholar] [CrossRef]
- Shi, Z.; Tuomilehto, J.; Kronfeld Schor, N.; Alberti, G.K.; Stern, N.; El Osta, A.; Bilu, C.; Einat, H.; Zimmet, P. The circadian syndrome predicts cardiovascular disease better than metabolic syndrome in Chinese adults. J. Intern. Med. 2020, 12, 13204. [Google Scholar] [CrossRef]
- Barton, T.J.; Low, D.A.; Bakker, E.A.; Janssen, T.; de Groot, S.; van der Woude, L.; Thijssen, D.H.J. Traditional Cardiovascular Risk Factors Strongly Underestimate the 5-Year Occurrence of Cardiovascular Morbidity and Mortality in Spinal Cord Injured Individuals. Arch. Phys. Med. Rehabil. 2021, 102, 27–34. [Google Scholar] [CrossRef]
- Liu, X.; Kong, D.; Liu, Y.; Fu, J.; Gao, P.; Chen, T.; Fang, Q.; Cheng, K.; Fan, Z. Effects of the short-term exposure to ambient air pollution on atrial fibrillation. Pacing Clin. Electrophysiol. 2018, 41, 1441–1446. [Google Scholar] [CrossRef]
- Chiu, H.; Tsai, S.; Weng, H.; Yang, C. Short-term effects of fine particulate air pollution on emergency room visits for cardiac arrhythmias: A case-crossover study in Taipei. J. Toxicol. Environ. Health A 2013, 76, 614–623. [Google Scholar] [CrossRef]
- Rich, D.Q.; Mittleman, M.A.; Link, M.S.; Schwartz, J.; Luttmann-Gibson, H.; Catalano, P.J.; Speizer, F.E.; Gold, D.R.; Dockery, D.W. Increased Risk of Paroxysmal Atrial Fibrillation Episodes Associated with Acute Increases in Ambient Air Pollution. Environ. Health Perspect. 2006, 114, 120–123. [Google Scholar] [CrossRef]
- Delfino, R.J.; Gillen, D.L.; Tjoa, T.; Staimer, N.; Polidori, A.; Arhami, M.; Sioutas, C.; Longhurst, J. Electrocardiographic ST-segment depression and exposure to traffic-related aerosols in elderly subjects with coronary artery disease. Environ. Health Perspect. 2011, 119, 196–202. [Google Scholar] [CrossRef]
- Korantzopoulos, P.; Kolettis, T.M.; Galaris, D.; Goudevenos, J.A. The role of oxidative stress in the pathogenesis and perpetuation of atrial fibrillation. Int. J. Cardiol. 2007, 115, 135–143. [Google Scholar] [CrossRef]
- Pekkanen, J.; Peters, A.; Hoek, G.; Tiittanen, P.; Brunekreef, B.; de Hartog, J.; Heinrich, J.; Ibald-Mulli, A.; Kreyling, W.G.; Lanki, T.; et al. Particulate air pollution and risk of ST-segment depression during repeated submaximal exercise tests among subjects with coronary heart disease: The Exposure and Risk Assessment for Fine and Ultrafine Particles in Ambient Air (ULTRA) study. Circulation 2002, 106, 933–938. [Google Scholar] [CrossRef] [PubMed]
- Peters, A.; Fröhlich, M.; Döring, A.; Immervoll, T.; Wichmann, H.E.; Hutchinson, W.L.; Pepys, M.B.; Koenig, W. Particulate air pollution is associated with an acute phase response in men; results from the MONICA-Augsburg Study. Eur. Heart J. 2001, 22, 1198–1204. [Google Scholar] [CrossRef] [PubMed]
- Fabritz, L.; Guasch, E.; Antoniades, C.; Bardinet, I.; Benninger, G.; Betts, T.R.; Brand, E.; Breithardt, G.; Bucklar-Suchankova, G.; Camm, A.J.; et al. Expert consensus document: Defining the major health modifiers causing atrial fibrillation: A roadmap to underpin spersonalised prevention and treatment. Nat. Rev. Cardiol. 2016, 13, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Chen, Y.; Lin, Y.; Chen, S. Inflammation and the pathogenesis of atrial fibrillation. Nat. Rev. Cardiol. 2015, 12, 230–243. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez, A.; Van Wagoner, D.R. Oxidant and Inflammatory Mechanisms and Targeted Therapy in Atrial Fibrillation: An Update. J. Cardiovasc. Pharmacol. 2015, 66, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Chung, M.K.; Martin, D.O.; Sprecher, D.; Wazni, O.; Kanderian, A.; Carnes, C.A.; Bauer, J.A.; Tchou, P.J.; Niebauer, M.J.; Natale, A.; et al. C-reactive protein elevation in patients with atrial arrhythmias: Inflammatory mechanisms and persistence of atrial fibrillation. Circulation 2001, 104, 2886–2891. [Google Scholar] [CrossRef]
- Huang, C.; Barnett, A.G.; Wang, X.; Tong, S. The impact of temperature on years of life lost in Brisbane, Australia. Nat. Clim. Chang. 2012, 2, 265–270. [Google Scholar] [CrossRef]
- Watanabe, E.; Kuno, Y.; Takasuga, H.; Tong, M.; Sobue, Y.; Uchiyama, T.; Kodama, I.; Hishida, H. Seasonal variation in paroxysmal atrial fibrillation documented by 24-h Holter electrocardiogram. Heart Rhythm 2007, 4, 27–31. [Google Scholar] [CrossRef]
- Chen, R.; Kan, H.; Chen, B.; Huang, W.; Bai, Z.; Song, G.; Pan, G. Association of particulate air pollution with daily mortality: The China Air Pollution and Health Effects Study. Am. J. Epidemiol. 2012, 175, 1173–1181. [Google Scholar] [CrossRef] [PubMed]
- Spengos, K.; Vemmos, K.; Tsivgoulis, G.; Manios, E.; Zakopoulos, N.; Mavrikakis, M.; Vassilopoulos, D. Diurnal and seasonal variation of stroke incidence in patients with cardioembolic stroke due to atrial fibrillation. Neuroepidemiology 2003, 22, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.; Uhm, T.; Han, J.; Won, K.-M.; Choe, J.C.; Shin, J.Y.; Park, J.S.; Lee, H.W.; Oh, J.-H.; Choi, J.H.; et al. Meteorological Factors and Air Pollutants Contributing to Seasonal Variation of Acute Exacerbation of Atrial Fibrillation: A Population-Based Study. J. Occup. Environ. Med. 2018, 60, 1082–1086. [Google Scholar] [CrossRef] [PubMed]
- Shiue, I.; Perkins, D.R.; Bearman, N. Relationships of physiologically equivalent temperature and hospital admissions due to I30-I51 other forms of heart disease in Germany in 2009–2011. Environ. Sci. Pollut. Res. Int. 2016, 23, 6343–6352. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Martens, W.J.M. Climate change, thermal stress and mortality changes. Soc. Sci. Med. 1998, 46, 331–344. [Google Scholar] [CrossRef]


| Description | Variables | Shanghai | Kunming | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Β 1 | Std. 2 | Sig. 3 | OR | OR 4 95% CI | β | Std. | Sig. | OR | OR 4 95% CI | ||||
| Lower Bound | Upper Bound | Lower Bound | Upper Bound | ||||||||||
| wind | W5(1) | −1.645 | 0.649 | 0.011 | 0.193 | 0.054 | 0.689 | ||||||
| W6(1) | 1.121 | 0.426 | 0.009 | 3.067 | 1.330 | 7.076 | |||||||
| Temperature | (Th)3 | −0.207 | 0.072 | 0.004 | 0.813 | 0.706 | 0.936 | ||||||
| (Th)4 | 0.200 | 0.080 | 0.012 | 1.221 | 1.044 | 1.427 | |||||||
| (Tl)10 | 0.347 | 0.153 | 0.023 | 1.416 | 1.048 | 1.911 | |||||||
| (Tl)11 | −0.553 | 0.170 | 0.001 | 0.575 | 0.412 | 0.802 | |||||||
| (Th)13 | 0.151 | 0.062 | 0.015 | 1.163 | 1.030 | 1.313 | |||||||
| Δ(Tl)1 | −0.190 | 0.093 | 0.041 | 0.827 | 0.689 | 0.992 | |||||||
| Δ(Tl)4 | 0.214 | 0.120 | 0.075 | 1.238 | 0.978 | 1.567 | |||||||
| AQI | (AQI)10 | −0.060 | 0.018 | 0.001 | 0.942 | 0.909 | 0.975 | ||||||
| Δ(AQI)5 | 0.041 | 0.011 | 0.000 | 1.042 | 1.019 | 1.066 | |||||||
| Δ(AQI)7 | 0.029 | 0.013 | 0.030 | 1.029 | 1.003 | 1.056 | |||||||
| Δ′(AQI)4 | 0.008 | 0.005 | 0.089 | 1.008 | 0.999 | 1.018 | |||||||
| Δ′(AQI)11 | −0.016 | 0.008 | 0.047 | 0.984 | 0.968 | 1.000 | |||||||
| TSP | Δ(PM2.5)13 | 0.125 | 0.033 | 0.000 | 1.133 | 1.062 | 1.208 | ||||||
| Δ(PM10)1 | 0.009 | 0.017 | 0.602 | 1.009 | 0.976 | 1.043 | |||||||
| SO2 | Δ(SO2)0 | −0.157 | 0.058 | 0.007 | 0.855 | 0.763 | 0.958 | ||||||
| Δ(SO2)6 | 0.411 | 0.130 | 0.002 | 1.508 | 1.168 | 1.947 | |||||||
| Δ′(SO2)9 | 0.109 | 0.041 | 0.008 | 1.116 | 1.029 | 1.209 | |||||||
| NO2 | (NO2)2 | 0.060 | 0.020 | 0.002 | 1.062 | 1.021 | 1.104 | −0.014 | 0.023 | 0.531 | 0.986 | 0.943 | 1.031 |
| Δ(NO2)9 | −0.080 | 0.020 | 0.000 | 0.923 | 0.887 | 0.960 | |||||||
| O3 | (O3)8 | 0.031 | 0.009 | 0.000 | 1.031 | 1.014 | 1.049 | ||||||
| Δ(O3)8 | −0.037 | 0.016 | 0.024 | 0.964 | 0.933 | 0.995 | |||||||
| Δ′(O3)9 | 0.017 | 0.009 | 0.044 | 1.017 | 1.000 | 1.034 | |||||||
| Constant | c | −4.008 | 0.874 | 0.000 | 0.018 | −3.098 | 1.478 | 0.036 | 0.045 | ||||
| Location | Omnibus Tests of Model Coefficients | Hosmer and Lemeshow Test | ||||
|---|---|---|---|---|---|---|
| Chi-Square | df | Sig. | Chi-Square | df | Sig. | |
| Shanghai | 63.89 | 14 | 0 | 15.394 | 8 | 0.052 |
| Kunming | 44.41 | 12 | 0 | 10.039 | 8 | 0.262 |
| Location | Area | Std. Error | Asymptotic Sig. | Asymptotic 95% Confidence Interval | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| Shanghai | 0.824 | 0.027 | 0 | 0.771 | 0.877 |
| Kunming | 0.756 | 0.034 | 0 | 0.689 | 0.822 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, S.; Zhao, Y.; Chen, Z.; Dou, M.; Zhang, Q.; Yang, W. Association between Atrial Fibrillation Incidence and Temperatures, Wind Scale and Air Quality: An Exploratory Study for Shanghai and Kunming. Sustainability 2021, 13, 5247. https://doi.org/10.3390/su13095247
Lu S, Zhao Y, Chen Z, Dou M, Zhang Q, Yang W. Association between Atrial Fibrillation Incidence and Temperatures, Wind Scale and Air Quality: An Exploratory Study for Shanghai and Kunming. Sustainability. 2021; 13(9):5247. https://doi.org/10.3390/su13095247
Chicago/Turabian StyleLu, Sha, Yiyun Zhao, Zhouqi Chen, Mengke Dou, Qingchun Zhang, and Weixin Yang. 2021. "Association between Atrial Fibrillation Incidence and Temperatures, Wind Scale and Air Quality: An Exploratory Study for Shanghai and Kunming" Sustainability 13, no. 9: 5247. https://doi.org/10.3390/su13095247
APA StyleLu, S., Zhao, Y., Chen, Z., Dou, M., Zhang, Q., & Yang, W. (2021). Association between Atrial Fibrillation Incidence and Temperatures, Wind Scale and Air Quality: An Exploratory Study for Shanghai and Kunming. Sustainability, 13(9), 5247. https://doi.org/10.3390/su13095247






