1. Introduction
Information System in healthcare, also known as Health Information System (HIS), refers to the process underlying the use of technologies in healthcare. HIS is developed to fully leverage technology, particularly the Internet, to provide better health care. HIS is a term used to describe the interaction of people, processes, and technology to assist operations and management in supplying essential data to improve the quality of healthcare services. As much as any other industry, the nature of the healthcare sector has evolved from a relatively stable to a dynamic one, and HIS has progressed through a variety of technological advancements [
1], while the use of technologies such as computer hardware and software to store, retrieve, distribute, and use health care information, data, and knowledge for communication and decision making is known as health information technology (HIT) [
2]. Furthermore, health informatics is a term associated with the cognitive information processing and communication aspects of medical practice, education, research, and supporting information science and technology [
3,
4].
The research of e-health is broad, ranging from theory development through major randomized controlled trials. The use of e-health varies by health care context or even by an individual, ranging from interventions or services such as apps, websites, and online discussion forums to real-world medical data collection, such as through the use of wearables [
5]. Ever since the COVID-19 outbreak began, every government and non-governmental organization has struggled to flatten the curve. In addition, systems were put in place that have played a significant role in assisting with contact tracing and breaking the pandemic chain, such as e-health and mHealth. With the spread of COVID-19, it has become important for individuals to track their health and take safety precautions when walking outside. COVID-19 has impacted not only the general public but also many working systems, as many began to work from home to minimize the spread of disease [
6]. As the public relied on digital information about the virus, it was necessary to develop apps specifically designed to collect data on COVID-19 and keep people updated. Several apps related to e-health were discussed. The team has collected information from all over the world and divided the apps into several categories: contact tracing, quarantine enforcing, symptom monitoring, and research-based (some apps had all in one) [
7]. E-health refers to the use of Information and Communications Technologies (ICT) in support of health and health-related activities, such as healthcare services, health surveillance, health literature, and health education, knowledge, and research [
8,
9], while mobile health (mHealth) is the use of mobile devices to monitor or detect biological changes in the human body, with data collected and used for healthcare and health status improvement by device management entities such as hospitals, clinics, or services providers [
10]. mHealth refers to delivering health services via the Internet and mobile devices to support healthcare goals. They have the same purpose of bringing services closer to the patients [
11,
12].
By installing an application, these devices allow individuals to manage their medical data and review their medical history, book appointments, get results from consultations and tests, and the like. Other medical practitioners can go through the individual’s past consultation history regardless of which hospital in the country they came from. Additionally, some applications enable a person to have virtual consultations with their medical practitioners. E-health and mHealth, therefore, minimize the number of times a person contacts someone else, especially high-risk individuals. E-health is the application of information and communication technologies that improve people’s health and well-being. It is cost-effective and secure [
13,
14].
E-health enhances user empowerment by allowing interaction between people, processes, and technology to aid information processing and communication activities in medical practice, education, and research to improve the quality of healthcare services [
15]. As a result, healthcare organizations can improve their service efficiency and efficacy [
16,
17].
The present research proposes a model in mHealth that expands previous e-health theory in terms of user empowerment [
18]. The model empowers users in three ways: as individual health actors, as social health agents, and as medical care partners. This study is significant because it accommodates an approach to the mHealth system to achieve best practice healthcare service, establish long-term users’ relationships with healthcare providers to improve user satisfaction and build health literacy among the public. This research is particularly significant for healthcare providers looking for new methods to improve their services and provide value [
19,
20]. It is also useful for IT developers who need to comprehend the concept of consumer behavior shift fully. This study will also benefit researchers who need to understand the challenges of each area and institution and end-users who would like to know their rights. When it comes to mHealth and behavior change, a comprehensive concept is often lacking but necessary for a long-term effect. There is inadequate evidence to allow the scaling up of mHealth interventions from a healthcare perspective. In addition, new approaches for improving the impact and efficiency of interventions are necessary [
21]. Apps do not always succeed because too much emphasis was placed on technical/technological data while the human dimension was overlooked. The suggested model incorporates these many viewpoints so that the patient’s experience, particularly during the COVID-19, can be used to suggest successful health-related solutions that are tailored to the needs of their users. This study will provide some insights to government and policymakers seeking a comprehensive solution for the next generation of mHealth for their citizens since it provides a mechanism to address complex challenges with a comprehensive response.
2. E-Health and Empowerment
HIT has tremendous potential for enabling clinical research, and it requires ongoing input from clinical research communities to solve both human aspects and technical challenges [
22]. The goal of healthcare companies’ early adoption of HIT is to improve the quality of service in the administration of healthcare data [
23,
24]. Furthermore, the accuracy, precision, and detail of information used in healthcare delivery have become increasingly important [
23]. One component that most businesses appreciate is ICT’s ability to improve existing features of health or functions that improve the flow of information in healthcare management [
25].
E-health initiatives are gaining traction in many countries to improve healthcare administration for healthcare practitioners and patients [
26]. For example, in Ontario, Canada, an e-health consortium offered three primary ways to enhance diabetes control, prescription management, and waiting times [
27]. These goals align with the e-health goals set forward by the World Health Organization in 2005, including healthcare services, health surveillance, health literature and education, knowledge, and research. E-health can also allow people to communicate with their healthcare providers over the Internet, opening new avenues for user/healthcare provider interaction [
28,
29].
The importance of users’ empowerment in e-health services has been highlighted in the literature. Numerous studies have investigated patients’ desires to access health information and use it to make better health decisions [
30,
31,
32,
33].
The model for consumer health informatics places the user at the center of the information transformation process [
31]. It explains how incorporating relevant and valid data into a shared decision-making environment can improve satisfaction with the care delivery process and measurable outcomes reflected in users’ health conditions. As a channel of communication, ICT, on the other hand, helps to aggregate and process data and act as a catalyst for feedback. Health information is used by people interested in promoting good health and specific health concerns [
34]. The search for health information and applying that knowledge to make health decisions is becoming more active among healthcare users. Print and electronic publications, healthcare practitioners, other consumers, and family and friends all seem to be good places to get health information [
32].
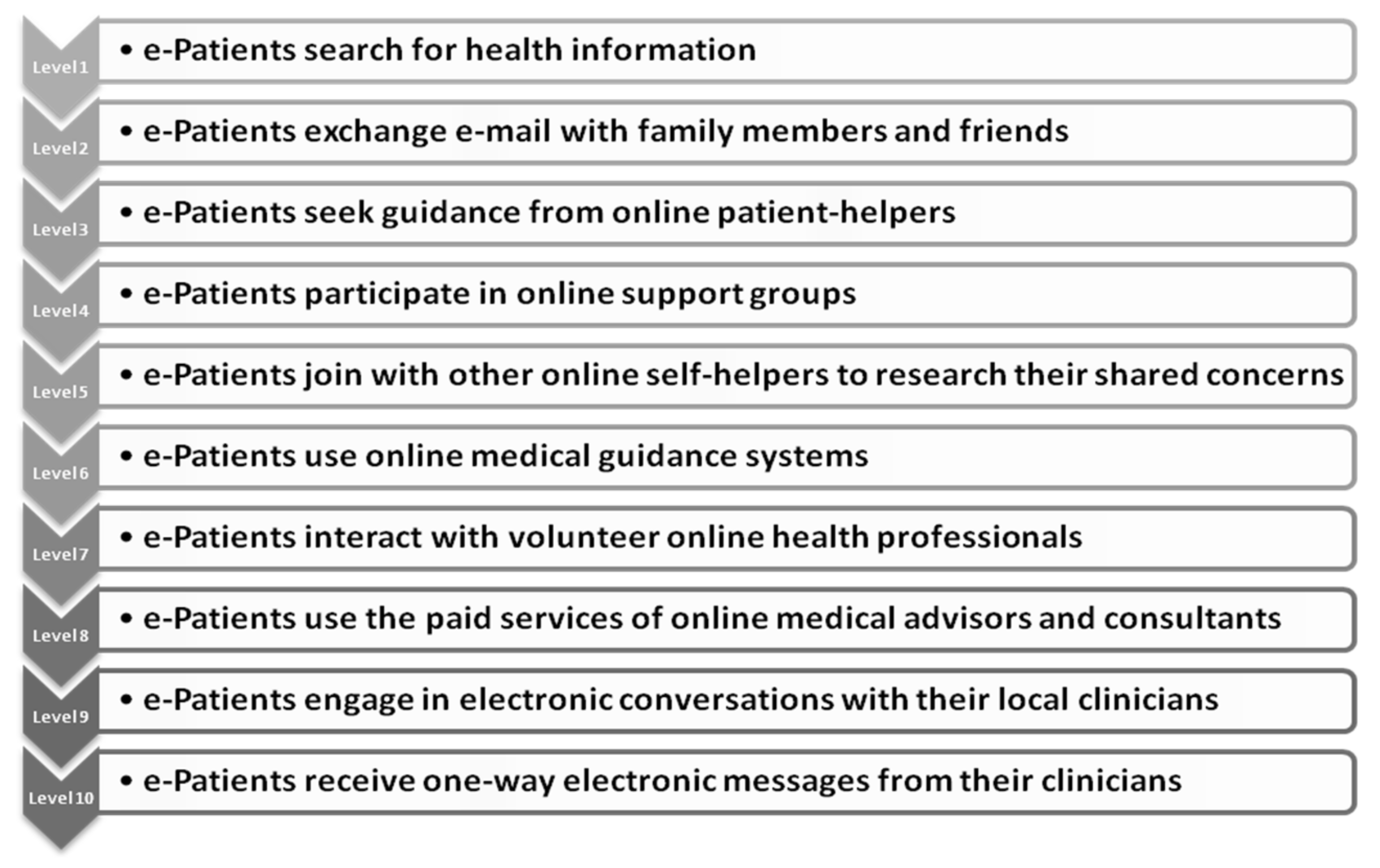
Modern healthcare users’ specific information demands as critical: “[Healthcare consumers] do not simply take whatever treatment their doctor offers when they have a major health issue [
31]. They’ll spend hours upon hours researching their ailment on the Internet, engaging with other patients and experts who share their interests, and following up on every lead on the finest new medicines they can find”. As shown at
Figure 1 that there are ten stages at which users participate in the access and use of healthcare information [
31].
Furthermore, consumer empowerment in health care in the era of the Internet and social media, asserting that the use of social media could indeed create new types of interactions with family, providers, and peers, as well as in the e-patient, who combines these new roles and technologies [
35]. However, the study does not reflect a comprehensive value set that consumers can obtain via data empowerment. Additionally, many e-health technologies do not succeed in bringing about long-term changes in healthcare practices. One explanation for this is that current e-health technology development frequently ignores the interdependencies between technology, human characteristics, and the socioeconomic context, resulting in technology with little impact on healthcare practices [
36]. Health professionals and consumers are in a great position to demand oversight that ensures safe and high-quality mHealth apps as mHealth expands into the domain of treatment [
37].
Previous research has emphasized the need to provide data access to users (patients). However, they could not indicate how a process of participation of patients and social networks could be incorporated into his customer experience model. As a result, this study bridges the gap in consumer participation that all aspects of data-generating systems are being integrated into the e-health scenario. That is why the proposed approach to empowering people to use Web/apps technology for enhanced services for all healthcare actors within the health ecosystem.
3. Web Technologies in Health Care
Many organizations, particularly healthcare services, have adjusted their business models since the emergence of Web 2.0. During a brainstorming session, O’Reilly and MediaLive International came up with the concept of Web 2.0 [
38]. “Web 2.0” refers to the idea that the Internet is a platform that contains social networks, which are groups of individuals that converse and interact. It is defined as a set of economic, social, and technological trends that, when combined, form the foundation for the next generation of the Internet—a distinct medium characterized by users’ participation in rapidly growing social networks that enable peer-to-peer collaboration, participation, and networking.
People can now obtain information about the things they are considering using from various sources, including organizations. Users’ expectations have evolved because of the abundance of information available to them [
39]. Organizations are rethinking their business strategy because of these developments and the customer’s ownership of the discussion [
40]. A technology platform, business rules, processes, and social features have helped change the approach that engages the customer in a collaborative conversation to create mutually beneficial value in a trustworthy and transparent business environment.
People are better equipped to respond to emergencies, consult with peers and health professionals about health issues as they arise, and access health services increasingly delivered through mHealth, such as remote patient monitoring, as smartphones and other mobile devices become more prevalent [
41]. Web 2.0 has had an impact on customer service in the healthcare industry. While the exact impact of the exponential growth in community social networking and support groups on wellness is still being investigated, it is an important subject for healthcare study [
42]. The goals of social empowerment and social network technology are identical in healthcare [
43].
Furthermore, the semantic web, sometimes known as “Web 3.0”, provides machine-readable material. The semantic technologies and the social computing environment are the two key platforms. These two platforms served two critical functions. Semantic technologies characterized open standards that could be used on top of the web. Many social web communities may be organized using the social computing environment, which allows human–machine cooperation [
44]. Web 3.0 is becoming increasingly widely used to process ever-increasing volumes of data. In fact, bioinformatics specialists are already searching for data from many systems and have begun to include rich semantic linkages into information tools for knowledge discovery. If we have the will to share clinical data publicly and honestly and expose it to examination, we can create more knowledge in medicine [
45,
46].
Patient empowerment logics are a reinforcement of personal autonomy and self-assertion processes, either through commercial relationships or through the social relationships that are also present, and a strengthening of control and standardization processes tied to typical power relationships in health [
47]. Therefore, social network empowerment must become an integral part of the process of social support, sharing, and exchange. Web/apps capabilities like social networking and semantic web must be incorporated into e-health/mHealth systems to improve the user’s empowering process. This study proposed an approach that allows each user to engage as a social health agent via a Web/app platform, sharing and supporting others in increasing their health literacy.
4. AI and E-Health
Healthcare reform is being driven by efforts to fulfill ever-increasing healthcare demands in the face of cost-cutting constraints, including the advancement of technology [
47]. Artificial intelligence (AI) is rapidly being used to administer digital health systems due to the fourth industrial revolution. With the availability of AI technologies, the government can gain much information on the current pandemic, such as understanding the virus, contact tracing, and detecting the origins of COVID-19 cases in a country [
48]. Artificial intelligence also means machines can think like human beings [
49]. Because AI is crucial for digital healthcare, more data collection and information sharing take place. In the case of e-health or mHealth applications, AI helps the healthcare system to shield citizens from their exposure to the virus. AI facilitates the probability of success of e-health/mHealth utilization. It is useful for real-time infection control, identifying high-risk patients, and can be utilized to track the spread of the virus. Moreover, it can analyze a patient’s past recorded data to calculate their mortality risk. AI can be used to address COVID-19 through population screening, medical assistance, notification, and infection control advice. Furthermore, it has the potential to become an evidence-based medical tool, as this technology has the potential to improve the COVID-19 patient’s planning, treatment, and reported outcomes [
50]. However, for AI to function efficiently, it needs data on COVID-19 to train on. Unfortunately, Big Data may make it difficult for AI to discern meaningful trends before they can be interpreted [
51]. The use of innovative and intelligent e-health/mHealth applications has helped a lot to reduce the number of people exposed to COVID-19 by providing a platform to assist the public with information and a standard operating procedure during this pandemic.
Countries worldwide have developed various health systems, countermeasures, and initiatives to halt the spread of the virus. Among these efforts were self-isolation and quarantine for suspected infection or displays of minor symptoms, the practice of good hygiene, the wearing of face masks, and the limitation of public gatherings [
52]. Various mHealth applications were quickly developed in response to the first wave of COVID-19 to limit the danger of virus exposure. The purposes of mHealth apps, particularly for combating the virus, include symptom monitoring, contact tracing, mobility surveillance, information sharing, and others.
Another innovative aspect of mHealth is that it can track a person’s contact history through Bluetooth and GPS. This allows the government to trace better and isolate possible transmissions and reduce further spread. Furthermore, those that are given isolation notices can be easily monitored via the application, thus dissuading these individuals from contacting other people before their recovery. For instance, in Brunei’s BruHealth, quarantine order, notices are sent via the application, requiring a person to log in daily while monitoring their contacts.
Furthermore, mHealth initiatives were developed as a way for the government to interact with the public most conveniently and efficiently possible. For instance, the Corona Health App, which German university partners created, gives users access to a survey investigating the impact of the virus on a person’s physical and mental health. Users are asked to complete a survey once a week to evaluate how their situation can be resolved. In addition, HOIA, a COVID-19 tracing app from Estonia, and the STAYAWAY smartphone app in Portugal have assisted these countries in informing the people if they have been exposed to or are in close contact with another person who has the virus.
The development, adoption, and implementation of a wide range of new e-health applications has a great promise for improving consumer and provider access to relevant health information, improving care quality, reducing health care errors, increasing collaboration, and encouraging healthy behavior adoption [
53]. From the first quarter of 2015 to the first quarter of 2021, the number of medical apps accessible in the Apple App Store is rapidly growing around the world. There were 53,979 iOS healthcare apps accessible during the last measured period, up 4.86 percent from the previous quarter.
5. Methods
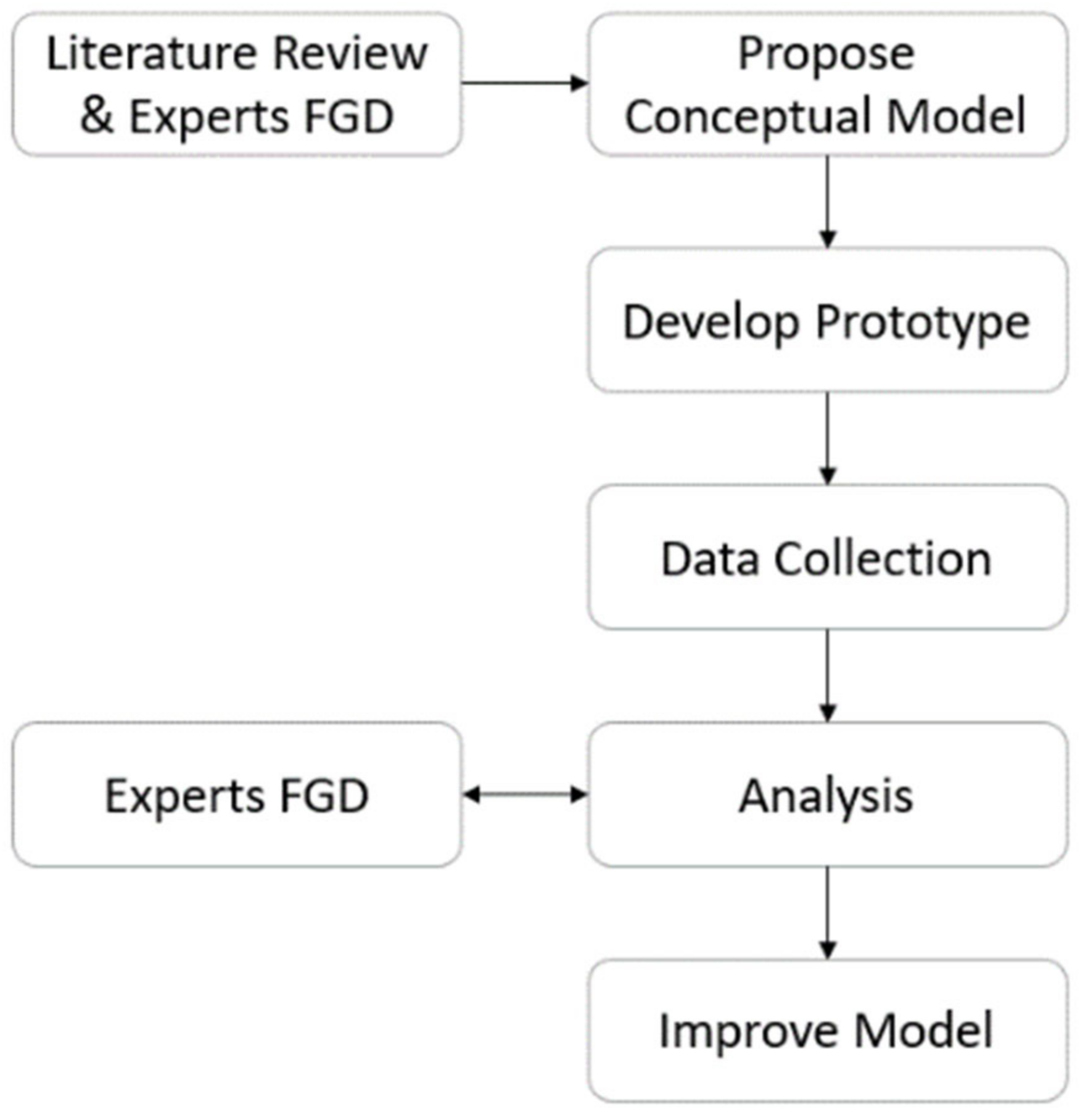
This study is built upon recent reviews of e-health and customer empowerment in healthcare organizations to develop a model. It employed thematic analysis, a qualitative method for identifying, analyzing, and reporting on patterns found in text data [
54]. Thematic analysis requires a thorough reading of the data and the identification of patterns, including explicit and implicit meaning embedded within the text [
55]. The relevant journals (EBSCO, ProQuest, Emerald, Insight, Science direct, Taylor and Francis, Wiley, JSTOR, and IEEE) search was conducted using keywords healthcare AND empowerment, social networks, Electronic Medical Records (EMRs), and Electronic Health Records (EHRs). These articles were reviewed to extract the issues and definitions of patient empowerment in an e-health setting. Three module components of the proposed e-health systems were identified based on the thematic analysis (personal, social network, and medical). Embedding social network features in e-health can empower patients to exchange information value among patients with similar conditions. Medical empowerments are derived from enabling EMRs’ to be accessible to patients, and personal health empowerment is derived from EHRs data availability. It is mostly generated on a thorough review of the literature and experts in the field via Focus Group Discussion (FGD) in the domains of health information systems and health practitioners and the outcomes of the first conceptual model. The concepts were then prototyped for testing and data collection in the field. The results were presented to experts in a second FGD, and the proposed model was fine-tuned because of the feedback (see
Figure 2). Respondents for this study were recruited from patients who utilized the prototype devices using the purposive sampling method. The data collection phase measures the actual versus expected outcome of the system. A private clinic in Indonesia has been chosen for the testbed of a prototype. The reasons were because the medical staff supported the systems and recommended participants to use the systems in real healthcare scenarios. In exchange, participants benefited from free health treatment as well as e-health services during the testing period (2015–2016) at the clinic.
6. Analysis
Consider the situation where patients are frantically waiting to be diagnosed because all the doctors are currently busy with other patients. The long queue of patients means that the process is inefficient, and due to this, patients may become dissatisfied. This means that healthcare providers must learn to allocate time more wisely. This situation requires a high level of attention: a physician must be able to diagnose quickly and effectively within the constraints of consultation time. Because a swift diagnosis benefits both the healthcare provider and the patient, the system enhances customer service. The physician will have complete information, knowledge, and understanding about the patient’s medical history, which the patient helped provide, saving a significant amount of time for both provider and patient because the medical records are viewed in their entirety. In other words, the system can improve the quality of consultation time and provide better customer service to fulfill patient expectations. Before diagnosing or analyzing the consulted symptoms, the physician must thoroughly view the patient’s history. This is possible because the physician is able to review the medical history report, which includes information such as the last medicine used, past diagnoses, lab results, and activities suggested by the health educator, among other things. However, in order to provide patients with medical data and personalized mHealth, the healthcare system must have officials on duty (health educators/health promoters) who can evaluate medical data and answer online questions. The officer on duty must be able to analyze medical data and be knowledgeable about the system’s technical features.
The types of e-health systems chosen for the required analysis represent a diverse set of approaches for addressing the customers’ needs for Web-enabled applications. In fact, the proposed system received superior ratings for meeting the needs of the customers. The results for the functional needs of the systems are summarized in
Table 1. The prototype systems compose three modules of Personal, Social (Networks), and Medical. The first feature is personal abilities. Here, the majority of users agree with the proposed systems. The Personal module offers the ability to view one’s own EMR, records health habits and activities, and supports emotional and spiritual components as part of healthcare.
Many healthcare organizations struggle to capture the message from social media conversations. Many of them do not consider social networks to build long-term relationships with their patients. As a result, healthcare management falls victim to patients’ judgments and criticisms regarding services provided on social networks, leading to skepticism of the hospital’s authority and jeopardizing the business in the long run.
Internal social networks are part of a strategy for isolating problems within the organization, with a focus on existing issues that can be easily monitored and resolved before they become unmanageable. Internal social networks that are controlled, managed, and maintained within the healthcare infrastructure are also proposed. Patients inside the healthcare center are more affected by this, as they are likely to have conversations with other patients/family members who share a common interest in their condition. Patients with similar conditions, for example, would be encouraged to share their experiences, learning, and information. Patients who have this resource can provide online material to share useful information with others. They can be the ideal area for supporting a group and sharing their experiences with all concerned, such as how the healthcare system provides treatment, how much it costs, what type of insurance the hospital accepts, and even what kind of food is offered. As a result, the size of this common group evolves, depending on the needs of the patients at that facility. Furthermore, this method increases customer loyalty.
The aim of linking internal and external social networks is to engage patients and export ideas, stimulate new service innovation, offer prompt feedback on existing services, and employ technology from individuals inside and outside the organization. Both types of networks play a variety of roles for the patient and family. Emotional support, service, influence, guidance, and information that a person can use to deal with a situation can all come through relationships. Furthermore, listening tools between social networks and mHealth systems provide a technique for capturing real-time data from social media and relaying it to the systems. This tool should be able to distinguish noise (the degree to which business activity is required) from actual data that have to be extracted to develop strategies.
Until the customer shares their displeasure through social networks and media, the healthcare provider may feel that everything is fine. In order to address this shortcoming, the healthcare provider must first isolate the problem, such as customer discontent, by responding quickly to rectify the problem before it becomes large and uncontrollable. Under the architecture proposed above, internal social networks could be a strategy to avoid such issues in the future.
7. Business Model
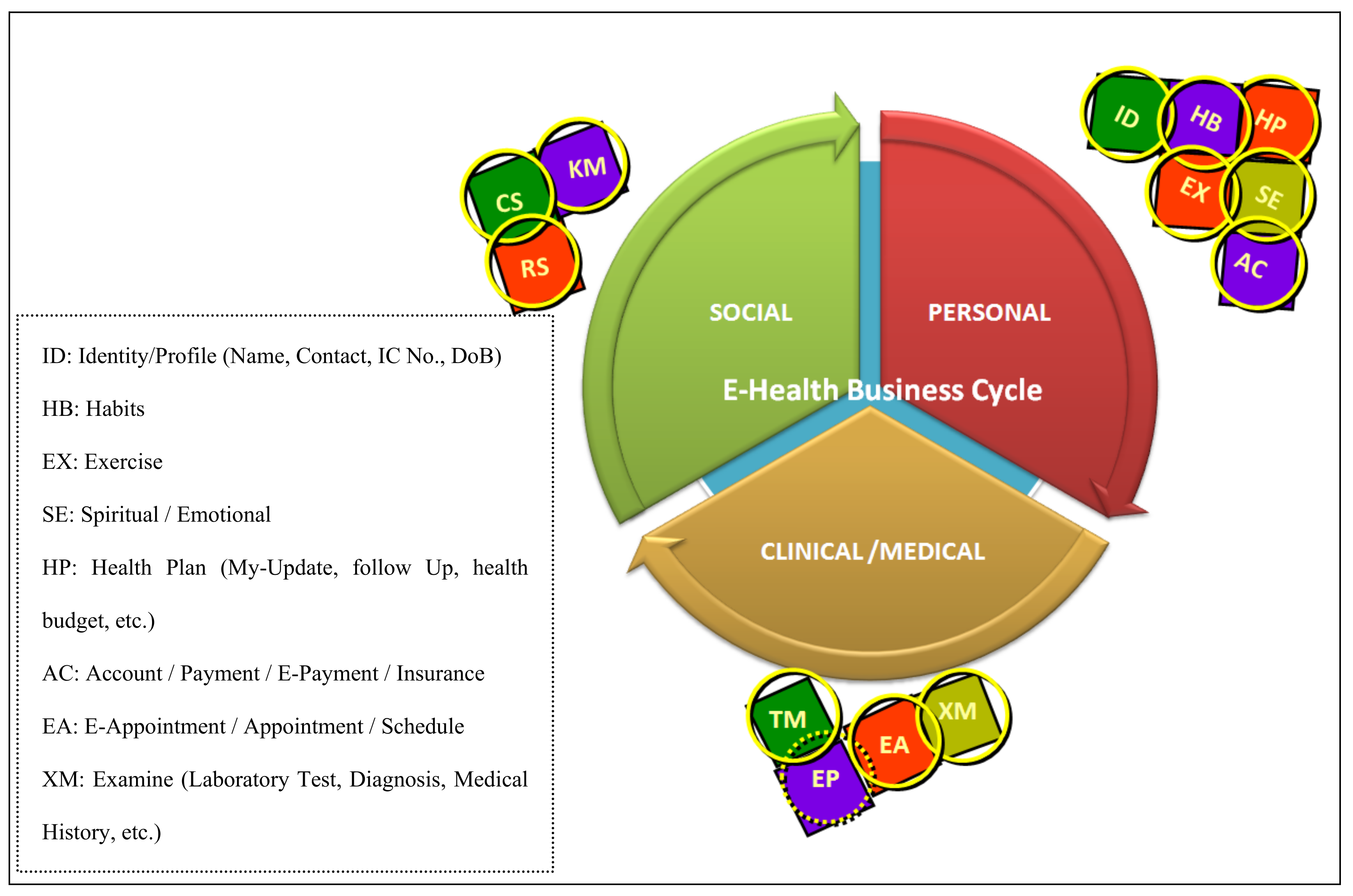
This section discusses the business model and scenario to present insights on the mHealth process in the context of user participation and interaction. The model accommodates different dimensions of personal health activities, social network participation, and electronic medical records. The circular structure of the primary activity categories captures the cyclic nature of the entire dimensions set. It displays a three-dimensional design that deconstructs the e-health scenario to simplify the business model. Patients’ roles are divided into three categories in the model: individual activities, social engagement, and electronic medical empowerments. Because of the modular design, each job consists of several subclasses that detail the function and organized activities within the e-health context between users and healthcare providers. The modular approach has the advantage of being extendible, allowing new modules or sub-modules to be easily integrated into future healthcare needs.
As depicted in
Figure 3, the approach demonstrates personal, social (networks), and medical empowerment. Healthcare organizations can tailor the deployment of the appropriate module to their own needs and procedures. The yellow circles in the sub-modules indicate that healthcare providers empower patients to have full access to information on that subclass, whereas the dashed yellow lines indicate that healthcare providers may only provide limited access to information, such as “for viewing only” and “no altering”. Finally, the absence of a circle means that healthcare providers do not allow their customers to access any information from the systems.
Patients with the ability to generate data can create electronic health records that can assist healthcare providers in diagnosing a patient based on the patient’s generated content. Today, many smart mobile devices can track physical activity, and these records can be integrated into the proposed system’s module. It’s the complete opposite of the traditional e-health system, where users don’t have enough ability to provide information. The model assists healthcare practitioners in empowering their patients so that providers can gain a better understanding of their patient’s health habits.
Furthermore, the integrated model can help healthcare organizations in determining which level of empowerment to apply. The modular approach can help organizations start the empowerment process in phases and then measure the performance in stages. The survey’s questionnaires were created using the model’s attributes.
Three different categories of descriptors are employed to illuminate the model’s central themes. First, the concept “personal health actor” refers to personal health practices that influence one’s health. Identity/Profile (ID), Personal Habits (HB), Exercise (EX), Emotional and Spiritual (SE), Personal Health Plan (HP), Personal Account (AC), and so on are all included in this concept. Second, users are classified as social health agents by the system. It refers to the activities of users that are related to social networking, sharing, and group support. Conversation (CS), Knowledge Management (KM), and Resolution (RS) are all involved. Third, the system’s core concepts are based on a set of principles that treat patients as medical care partners utilizing e-health services. It is divided into modules that include checkups, I/P therapy, and O/P treatment. E-Appointment (EA), Examination (XM), Treatment (TM), and E-Prescription (EP) are characteristics of these activities. There are also sub-sub-classes in each object. Object XM, for example, might be made up of chronic disease (cc) and non-chronic disease (nc). Diabetes (da), cancer (ca), and obesity (ob) are instances of chronic diseases. The object-oriented design allows an object to inherit a child object’s attribute, method, or operation.
The first role is derived from the personal health actor function. This function portrays an individual as a personal health actor who is connected to all personal health activities in the e-health services, which will affect their health status and services directly or indirectly. Personal Identity (ID), personal Habits of a patient (HB), Exercise activities (EX), Spiritual and Emotional activities (SE), personal Health Plan (HP), and personal Account information (AC) are examples of objects in this category. For example, ID sets contain personal information such as name, address, phone number, email address, login ID, password, etc. HB refers to an individual’s daily habits, such as eating, sleeping, and any other activities that may impact one’s health. The EX is an individual’s routine exercising activities that can be beneficial when recorded in the systems. As previously indicated, all subclasses within this category can be controlled entirely by customers. Customers can handle things on their own. The process replaces the current method in which healthcare workers enter patient data into systems. Now patients do it themselves. Clearly, this is a customer empowerment model which puts all activities under the control of the personal health actors or “gives them the right to do it themselves”.
The second process is the Social object class, in which a patient is positioned as a social health agent for others. This is a relatively new service in e-health systems. Customers engage in social media sites where they share and discuss their healthcare experiences with others. By incorporating the concept of social networks within e-health services, customers acting as social health agents enjoy a broad range of empowerment. Conversation (CS), chat, update status, forum, wikis, blog, Knowledge Management (KM), personal knowledge, group knowledge, and Requests for Service (RS) are all sub-classes in this category. Standard social network activities such as sharing and conversing on social media are referred to as CS. People nowadays utilize social media regularly. Updating one’s status on social media generates a discussion among one’s social circle. Including this scenario in e-health service is a demanding task. Patients with the same condition may, for example, share their experiences with other patients through social media. This sharing might turn into a virtual support group, strengthening their will to improve their health. Indeed, social media has an impact on the communication between doctors and patients. As a result, social networks may be included in this category.
In the area of healthcare, social networks are beneficial. However, many health providers have failed to acknowledge that the type of relationship, connection, and value gained in engaging with patients has changed. Patients communicate with their friends and the hospital by reporting their dissatisfaction [
56]. Social networking may impact the relationship between healthcare, patients, and society as a whole, potentially causing patients to lose trust in the system. Tardy integration of the social network model into the e-health strategy may jeopardize the business process in healthcare. In conclusion, the patient as social health agent is a type of empowerment within an e-health system that is critical to becoming a medium of sharing between patients and healthcare professionals to generate advantages for all parties [
57].
The third dimension is the medical dimension, in which the patient acts as a medical care partner in the healthcare process. This section looks at the sub-modules: Examination (XM), E-Appointment (EA), E-Prescription (EP), and E-Treatment (TM). XM is an online consultation between patients and medical professionals that can create a patient’s Electronic Medical Record (EMR). It is a standard service in any E-Health initiative; however, when empowerment is incorporated into these medical processes, the outcome of an e-consultation can differ from that of an E-Health system without empowerment aspects. Many healthcare providers, for example, prohibit patients from seeing their EMRs before their scheduled consultation. This might mean that every time a patient needs to see a different healthcare professional, they will have to undergo the same diagnosis. Similarly, whenever a patient seeks views from multiple doctors, the patient must disclose their symptoms and problems to each doctor. According to WHO (2005), the goal of e-health is to educate patients on their health status, condition, and history [
58]. As a result, empowerment in the medical object class is essential for educating patients and increasing their awareness of their medical history and condition [
59]. The EP subset facilitates the management of prescriptions, and users are more aware of what they are taking because they are able to access and learn about their medications.
In conclusion, the medical object class has the potential to transform a patient’s role from that of a recipient of care to that of a medical partner. They are a valuable resource for medical care, especially in the decision-making process, because they access knowledge and content. The following section delves deeper into each of the object classes.
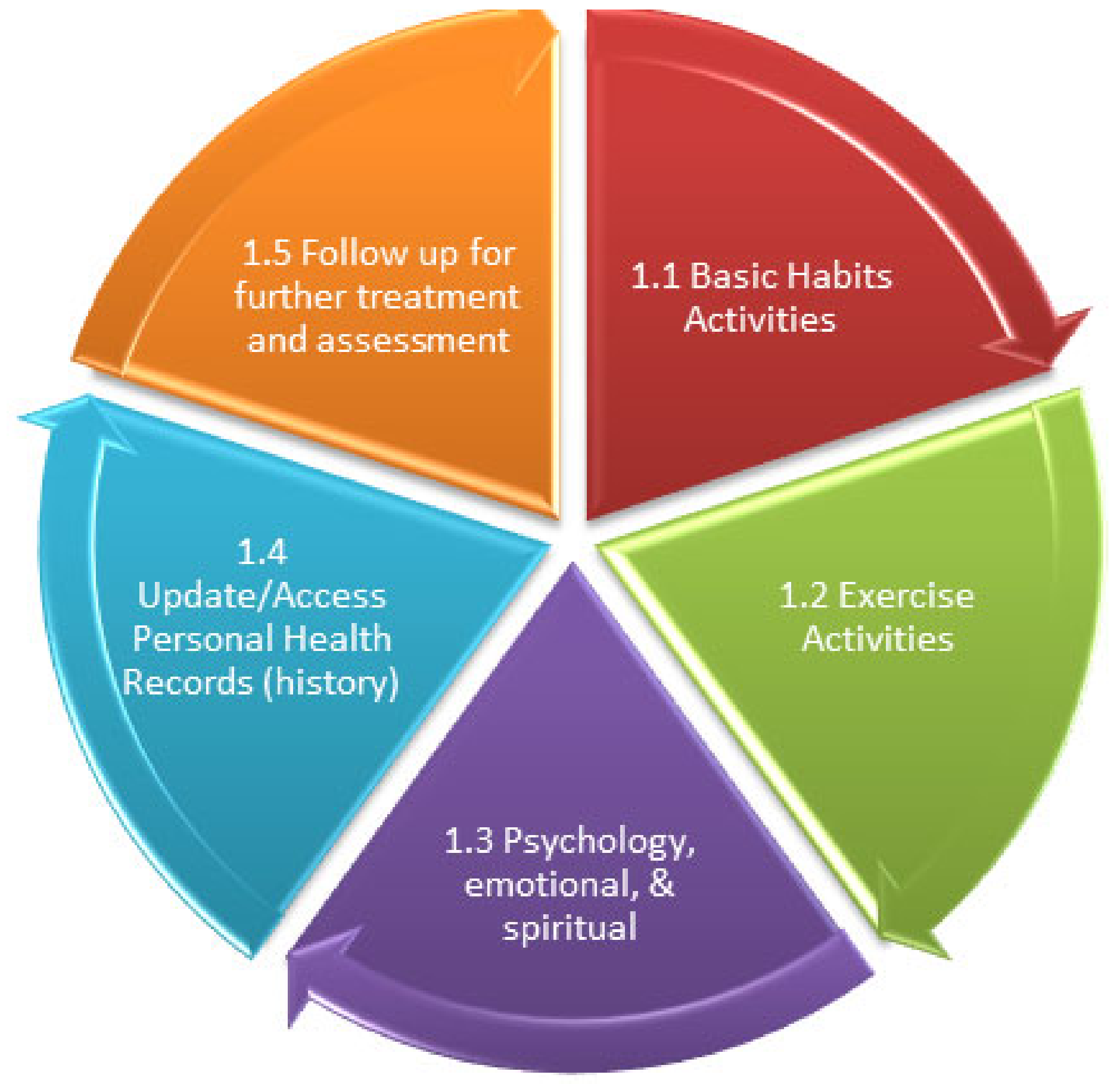
8. Personal Health Cycle
The Personal Health Cycle (PHC) describes the types of interactions that occur in healthcare settings. In the e-health business process, there are three sorts of interactions. They are the link between the patient and the provider, the patient and another patient, and the patient alone. The patient’s business object interaction is depicted in
Figure 4. Personal daily life refers to an individual’s activities that may impact his/her personal health status, either directly or indirectly.
8.1. Basic Habit
Actors: Patient/customer (update, delete, view)
Online health educator (view, comment)
Use Case: The basic healthy habit is a database about activities, which is believed to boost the chances for a healthy personal lifestyle. This scenario demonstrates the process when a user records or views a recommended activity. The process begins when the request is made. The daily habit workflow records and views the data. Once the data are stored, it may be retrieved from the database. The user may share the data to allow interested parties to display the report.
8.2. Exercise Activities
Actors: Patient/customer (update, delete, view)
Online health educator (view, comment)
Use Case: Exercise is a physical activity that records numbers of minutes/hours and the type of exercise regularly taken to maintain a healthy personal lifestyle. This scenario demonstrates the process when a user records and views an exercise activity. The process begins when the request is made. The daily habit workflow records and views the data. Once the data are stored, they may be retrieved from the database. The user may share the data to allow interested parties to display the report.
8.3. Psychological/Emotional/Spiritual Activities
Actors: Patient/customer (update, delete, view)
Online health educator (view, comment)
Use Case: Emotional and spiritual are routine spiritual and emotional activities that have been performed that affect personal health directly and indirectly. This scenario demonstrates the process when a user produces and records a checklist of those activities. The process begins when the request is made. The user may share the data to allow interested parties to display the report.
8.4. Update Personal Health Record
Actors: Patient/customer (update, delete, view)
Medical staff (update, delete, view)
Online health educator (view, comment)
Use Case: Updating health records is a self-health assessment of activities that an individual may conduct without the help of a health professional (weight, diet, glucose level, etc.). This scenario demonstrates the process when a user does checklists or records of those activities. The process begins when the request is made. Once the data are stored, they may be retrieved from the database. The user may share the data to allow interested parties to display the report.
8.5. Follow Up
Actors: Patient/customer (update, delete, view)
Online health educator (view, comment)
Use Case: Follow-up/exception is the condition where a user needs to take any action other than the above such as taking medicine, recording health conditions (headache, flu, cough, etc.). This scenario demonstrates the process when a user records any extraordinary activities. The process begins when the request is made. The user may share the data to allow interested parties, especially the health educator, to display the report.
9. Medical Care Cycle
The medical object interaction between a healthcare provider and patients is depicted in
Figure 5. This section details the major activities of medical treatment that patients get during the medical care cycle. Patients have complete control over their medical records and can access them anytime and from any location.
9.1. Schedule
Actors: Patient/customer (update, delete, view)
Use Case: Arrange for online consultation with online health educators. Define which topic one would like to discuss: physical, emotional, or spiritual. The patient searches the timetable for open slots. They can post questions for a specific doctor. The patient invites the doctor to see the patient’s profile when they locate a free space on the schedule. Next, the patient schedules an appointment and selects a media type: text, audio, or video. When a patient requires a procedure that is not currently accessible in the clinic due to a lack of available slots or because the clinic does not provide that service, the receptionist or doctor can assist in finding open slots in other clinics.
9.2. Examine
Actors: Online health educator (view, comment)
Use Case: The health educator will examine and try to have a complete overview of the patient’s profile, health records, medical history, and all related information loaded by the patient so that the next process will be quick and effective.
9.3. Treatment
Actors: Online health educator (view, comment)
Patient/customer (view)
Use Case: This is a consultation or communication process between patients and health educators. The consultation’s notes are recorded, and copies of the consultation are forwarded to the patient’s email for future record.
9.4. Prescription
Actors: Online health educator (view, comment)
Patient/customer (view)
Use Case: After the consultation session, a health educator may provide a prescription if necessary. A prescription is written on the prescription form, which is forwarded to the patient’s email.
9.5. Referral
Actors: Online health educator (view, comment)
Patient/customer (view)
Use Case: The online health educator may issue a Referral if the condition of the patient needs further physical assessment. A referral form is completed and forwarded to the patient’s email and the online consultation results. The health educator concern also provides online material, which may be relevant to the patient’s current condition.
10. Social Health Cycle
Figure 6 shows the cycle of the social life of an individual or patient. Social life refers to the customer’s social activities. Healthcare organizations must consider the adoption of social networks in their organization as tools for a strategy to maintain long-lasting relationships with their patients, especially in a competitive environment [
60]. E-empowerment is considered a process of conversation and communication through social networks in which experiences, values, and supports are expressed in informal ways. With the Web 2.0 technologies, all types of interactions can generate conversations and supports that benefit both customers and healthcare providers in creating a sales, marketing, and customer service strategy.
10.1. Sharing and Conversation
Actors: Online health educator (update, view, comment, delete)
Patient/customer (view)
Use Case: Tag, share, rate, and promote relevant materials of interest among members of those communities, using their own patient/community-developed vocabularies and concepts that everyone understands.
10.2. Listening Tool
Actors: Online health educator (update, view, comment, delete)
Marketing team (view, comment)
Use Case: Based on their function and objectives, actors capture messages from conversations in social networks and forums. For instance, the marketing team captures any concern relating to the services, customers’ demands, or any complaints raised by customers on social media.
10.3. Route
Actors: Online health educator (update, view, comment, delete)
Healthcare staff (update, view, comment, delete)
Use Case: Actors pass any relevant messages related to healthcare services to the appropriate department for a follow-up to improve services.
10.4. Resolve/Follow-up
Actors: Healthcare staff (update, view, comment, delete)
Use Case: Actors resolve the problems discussed in social media.
10.5. Referral Handling
Actors: Healthcare management/staff (update, view, comment, delete)
Online health educator (view, update, comment)
Patient/customers (view, comment)
Use Case: Healthcare management and/or staff respond to the problems raised earlier from the conversations in social media.
11. Front-End Architecture
The front-end architecture aims to create clear, complete, easy, and friendly user interfaces [
61]. These services can be classified into three broad ranges of services offered by object classes Medical, Personal, and Social Networks, respectively. Patients are included in object class Social Networks as social agents, while object class Personal refers to a patient acting as an individual actor, and object class Medical refers to a patient engagement as a medical partner.
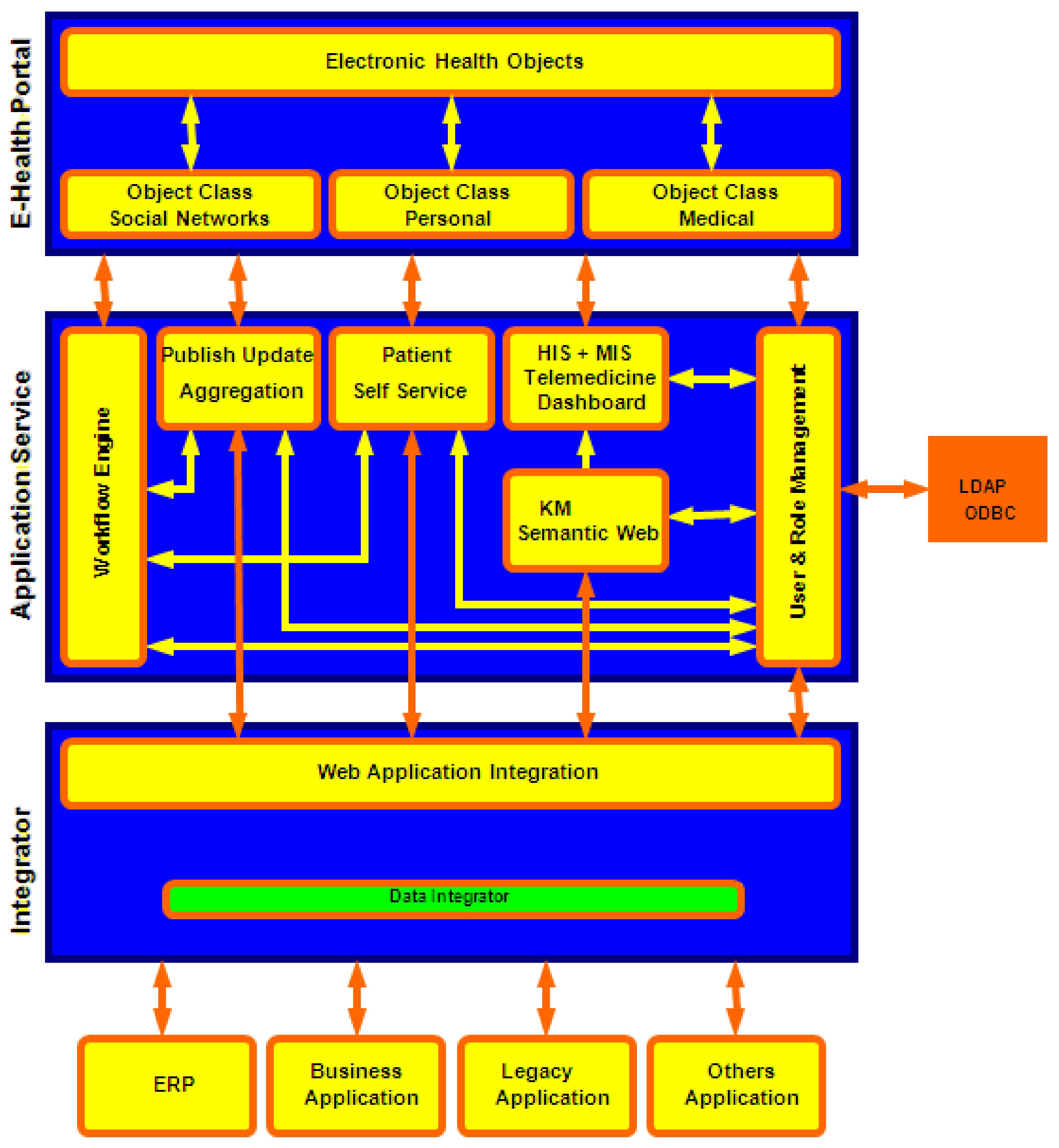
The proposed systems’ front-end architecture is shown in
Figure 7. It considers Electronic Health Objects (EHOs) as collections of objects with their inherent attributes and behaviors, allowing users to interact and generate data. The architecture’s business model is governed by the E-Health portal, which combines public health promotion, personalized displays of the right information to the right users at the right time, customizable sites where users can create custom pages, social networking platforms, and interactive medical information.
From the organizational perspective, an implementation of the Social CRM is proposed to provide a strong foundation to build an integrated E-Health system that can electronically incorporate patient empowerment [
62,
63]. Application services comprise a range of modular and specialized vertical applications that are tightly integrated into the back-end enterprise system. These applications can run on Web browsers, SMS, and mobile applications [
63]. A healthcare organization will benefit from implementing social networks with an e-health portal front-end solution based on the proposed model. The major benefits are the one-stop solution for managing customers’ relationships and systems availability. Healthcare organizations have the availability of high-volume transactions, especially for online service and promotion.
12. Conclusions
The study presents a model to use social networks to achieve a healthcare organization’s business objective in implementing e-health. The study’s focus is on customer service, which provides a distinct value for each activity while also allowing customers to participate in the suggested systems. As its core role comprises self-managed data and authorization to enable patients to contribute information about their health, the model accommodates many aspects of empowerment in healthcare systems. This is essential for healthcare companies since it allows patients to gain access to more health information. In addition, the COVID-19 pandemic has revealed that digital technologies play a part in handling a crisis. Artificial intelligence has helped governments track the pandemic by implementing mobile health apps for monitoring purposes during the pandemic.