Not All Demands Are Exhausted for Healthcare Workers. A Cross-Lagged Study on the Buffering Effect of Leadership Resources
Abstract
:1. Introduction
1.1. The Effects of Quantitative and Emotional Demands on Exhaustion among Healthcare Workers
1.2. Moderating Effect of Leadership
1.3. The Aim of Study
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measurement
2.3. Analytical Procedure
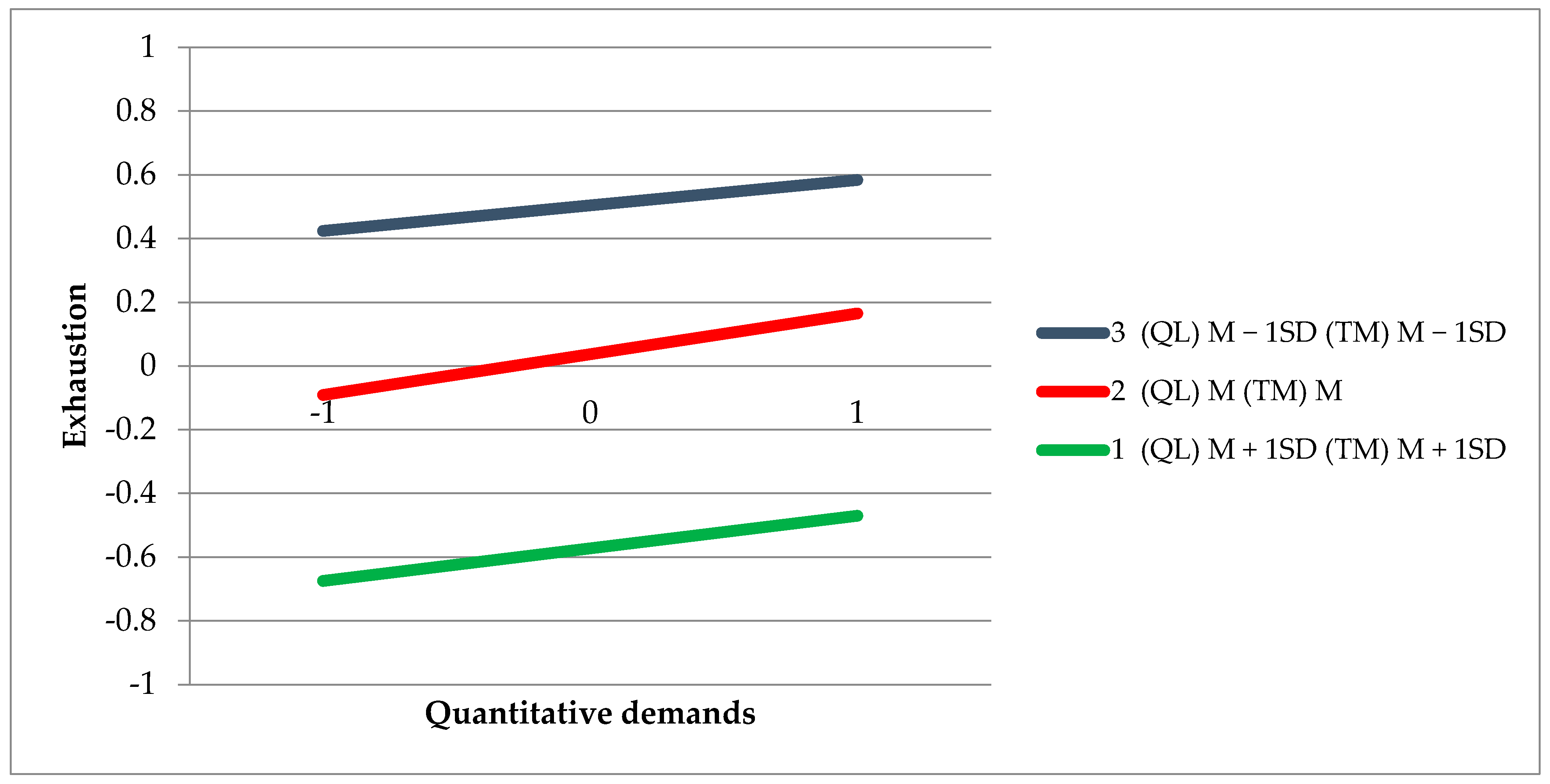
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Models | Χ2 | df | RMSEA | PClose | 90 LLCI | 90 ULCI | SRMR | TLI | GFI | CFI |
|---|---|---|---|---|---|---|---|---|---|---|
| Job demand—Measurement 1 | 344.456 | 40 | 0.070 | 0.000 | 0.063 | 0.077 | 0.0507 | 0.918 | 0.961 | 0.940 |
| Job demand—Measurement 2 | 241.387 | 40 | 0.067 | 0.000 | 0.059 | 0.075 | 0.0552 | 0.924 | 0.961 | 0.945 |
| Leadership resources—Measurement 1 | 150.337 | 19 | 0.066 | 0.000 | 0.057 | 0.076 | 0.0311 | 0.968 | 0.976 | 0.978 |
| Leadership resources—Measurement 2 | 165.250 | 19 | 0.081 | 0.000 | 0.070 | 0.093 | 0.0426 | 0.954 | 0.964 | 0.969 |
| Exhaustion—Measurement 1 | 330.281 | 16 | 0.110 | 0.000 | 0.100 | 0.121 | 0.0749 | 0.860 | 0.954 | 0.920 |
| Exhaustion—Measurement 2 | 252.283 | 16 | 0.116 | 0.000 | 0.104 | 0.129 | 0.0785 | 0.851 | 0.948 | 0.915 |
References
- Abdulah, D.M.; Musa, D.H. Insomnia and stress of physicians during COVID-19 outbreak. Sleep Med. X 2020, 2, 100017. [Google Scholar] [CrossRef]
- Fiorillo, A.; Gorwood, P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry J. Assoc. Eur. Psychiatr. 2020, 63, e32. [Google Scholar] [CrossRef] [Green Version]
- Baka, Ł. Coronavirus anxiety and exhaustion among Polish front-line healthcare workers—The mediation effect of insomnia. Int. J. Occup. Med. Environ. Health 2021, 34, 263–273. [Google Scholar] [CrossRef]
- Jimmieson, N.L.; Tucker, M.K.; Walsh, A.J. Interaction effects among multiple job demands: An examination of healthcare workers across different contexts. Anxiety Stress Coping 2017, 30, 317–332. [Google Scholar] [CrossRef]
- Moreno-Jiménez, J.E.; Blanco-Donoso, L.M.; Chico-Fernández, M.; Belda Hofheinz, S.; Moreno-Jiménez, B.; Garrosa, E. The job demands and resources related to COVID-19 in predicting emotional exhaustion and secondary traumatic stress among health professionals in Spain. Front. Psychol. 2021, 12, 564036. [Google Scholar] [CrossRef]
- Hobfoll, S.E. Conservation of resources theory: Its implication for stress, health, and resilience. In The Oxford Handbook of Stress, Health, and Coping; Oxford Library of Psychology; Oxford University Press: New York, NY, USA, 2011; pp. 127–147. [Google Scholar]
- Nguyen, L.H.; Drew, D.A.; Graham, M.S.; Joshi, A.D.; Guo, C.-G.; Ma, W.; Mehta, R.S.; Warner, E.T.; Sikavi, D.R.; Lo, C.-H.; et al. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health 2020, 5, e475–e483. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain. Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Van Vegchel, N.; de Jonge, J.; Söderfeldt, M.; Dormann, C.; Schaufeli, W. Quantitative versus emotional demands among swedish human service employees: Moderating effects of job control and social support. Int. J. Stress Manag. 2004, 11, 21–40. [Google Scholar] [CrossRef] [Green Version]
- Demerouti, E.; Bakker, A.B.; Nachreiner, F.; Schaufeli, W.B. The job demands—Resources model of burnout. J. Appl. Psychol. 2001, 86, 499–512. [Google Scholar] [CrossRef]
- Fu, W.; Wang, C.; Zou, L.; Guo, Y.; Lu, Z.; Yan, S.; Mao, J. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Transl. Psychiatry 2020, 10, 225. [Google Scholar] [CrossRef] [PubMed]
- Dewa, C.S.; Loong, D.; Bonato, S.; Trojanowski, L. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. BMJ Open 2017, 7, e015141. [Google Scholar] [CrossRef] [PubMed]
- Hall, L.H.; Johnson, J.; Watt, I.; Tsipa, A.; O’Connor, D.B. Healthcare staff wellbeing, burnout, and patient safety: A systematic review. PLoS ONE 2016, 11, e0159015. [Google Scholar] [CrossRef]
- Bronkhorst, B.; Tummers, L.; Steijn, B.; Vijverberg, D. Organizational climate and employee mental health outcomes: A systematic review of studies in health care organizations. Health Care Manag. Rev. 2015, 40, 254–271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuoppala, J.; Lamminpää, A.; Liira, J.; Vainio, H. Leadership, job well-being, and health effects—A systematic review and a meta-analysis. J. Occup. Environ. Med. 2008, 50, 904–915. [Google Scholar] [CrossRef]
- Montano, D.; Reeske, A.; Franke, F.; Hüffmeier, J. Leadership, followers’ mental health and job performance in organizations: A comprehensive meta-analysis from an occupational health perspective. J. Organ. Behav. 2017, 38, 327–350. [Google Scholar] [CrossRef]
- Skakon, J.; Nielsen, K.; Borg, V.; Guzman, J. Are leaders’ well-being, behaviours and style associated with the affective well-Being of Their Employees? A systematic review of three decades of research. Work Stress 2010, 24, 107–139. [Google Scholar] [CrossRef]
- Koff, S.Z. Nursing in the European Union: Anatomy of a Profession; Routledge: New York, NY, USA, 2017. [Google Scholar]
- OECD; European Union. Health at a Glance: Europe 2020: State of Health in the EU Cycle; OECD Publishing: Paris, France, 2020. [Google Scholar]
- Simon, M.; Kümmerling, A.; Hasselhorn, H. Work-home conflict in the european nursing profession. Int. J. Occup. Environ. Health 2004, 10, 384–391. [Google Scholar] [CrossRef]
- Maxwell, S.E.; Cole, D.A.; Mitchell, M.A. Bias in cross-sectional analyses of longitudinal mediation: Partial and complete mediation under an autoregressive model. Multivar. Behav. Res. 2011, 46, 816–841. [Google Scholar] [CrossRef] [Green Version]
- Hasselhorn, H.; Tackenberg, P.; Müller, H. Work Conditions and Intent to Leave the Profession Among Nursing Staff in Europe; Report No 7:2003; SALTSA: Stockholm, Sweden, 2003. [Google Scholar]
- Naczelna Izba Pielęgniarek i Położnych—Samorząd [Main Chamber of Nurses and Midwives—Local Government]. Available online: https://nipip.pl/ (accessed on 6 September 2021).
- Giusti, E.M.; Pedroli, E.; D’Aniello, G.E.; Stramba Badiale, C.; Pietrabissa, G.; Manna, C.; Stramba Badiale, M.; Riva, G.; Castelnuovo, G.; Molinari, E. The psychological impact of the COVID-19 outbreak on health professionals: A cross-sectional study. Front. Psychol. 2020, 11, 1684. [Google Scholar] [CrossRef] [PubMed]
- ICN. International Council of Nurses. Available online: https://www.icn.ch/homepage (accessed on 28 July 2021).
- ICN. ICN Reaction: WHO DG Dr Tedros Confirms at Least 115,000 Health Workers Have Died Due to Pandemic. 2021. Available online: https://www.icn.ch/news/icn-reaction-who-dg-dr-tedros-confirms-least-115000-health-workers-have-died-due-pandemic (accessed on 25 July 2021).
- Statista. Poland: COVID-19 Infections and Deaths in Healthcare 2021, by Profession. Available online: https://www.statista.com/statistics/1246201/poland-covid-19-infections-and-deaths-in-healthcare/ (accessed on 25 July 2021).
- Karasek, R.A. Job demands, job decision latitude, and mental strain: Implications for job redesign. Adm. Sci. Q. 1979, 24, 285. [Google Scholar] [CrossRef]
- Meijman, T.F.; Mulder, G. Psychological aspects of workload. In Handbook of Work and Organizational: Work Psychology, 2nd ed.; Psychology Press: Hove, UK, 1998; Volume 2, pp. 5–33. [Google Scholar]
- Lee, R.T.; Ashforth, B.E. A meta-analytic examination of the correlates of the three dimensions of job burnout. J. Appl. Psychol. 1996, 81, 123–133. [Google Scholar] [CrossRef]
- McMahan, J. A Meta-Analytic Examination of the Dimensions of Teacher Burnout and Demand and Resource Correlates. Master’s Thesis, University of Tennessee, Knoxville, TN, USA, 2003. [Google Scholar]
- Alarcon, G.M. A meta-analysis of burnout with job demands, resources, and attitudes. J. Vocat. Behav. 2011, 79, 549–562. [Google Scholar] [CrossRef]
- Aronsson, G.; Theorell, T.; Grape, T.; Hammarström, A.; Hogstedt, C.; Marteinsdottir, I.; Skoog, I.; Träskman-Bendz, L.; Hall, C. A systematic review including meta-analysis of work environment and burnout symptoms. BMC Public Health 2017, 17, 264. [Google Scholar] [CrossRef] [Green Version]
- Trufelli, D.C.; Bensi, C.G.; Garcia, J.B.; Narahara, J.L.; Abrão, M.N.; Diniz, R.W.; Miranda, V.D.C.; Soares, H.P.; Del Giglio, A. Burnout in cancer professionals: A systematic review and meta-analysis. Eur. J. Cancer Care 2008, 17, 524–531. [Google Scholar] [CrossRef] [PubMed]
- Lim, N.; Kim, E.; Kim, H.; Yang, E.; Lee, S.M. Individual and work-related factors influencing burnout of mental health professionals: A meta-analysis. J. Employ. Couns. 2010, 47, 86–96. [Google Scholar] [CrossRef]
- Yates, M.; Samuel, V. Burnout in oncologists and associated factors: A systematic literature review and meta-analysis. Eur. J. Cancer Care 2019, 28, e13094. [Google Scholar] [CrossRef] [PubMed]
- Oksanen, T.; Kouvonen, A.; Kivimäki, M.; Pentti, J.; Virtanen, M.; Linna, A.; Vahtera, J. Social capital at work as a predictor of employee health: Multilevel evidence from work units in Finland. Soc. Sci. Med. 2008, 66, 637–649. [Google Scholar] [CrossRef]
- Söderfeldt, B.; Söderfeldt, M.; Muntaner, C.; O’Campo, P.; Warg, L.E.; Ohlson, C.G. Psychosocial work environment in human service organizations: A conceptual analysis and development of the demand-control model. Soc. Sci. Med. 1996, 42, 1217–1226. [Google Scholar] [CrossRef]
- The World Bank. Employment in Services (% of Total Employment) (Modeled ILO Estimate). 2021. Available online: https://data.worldbank.org/indicator/SL.SRV.EMPL.ZS (accessed on 25 July 2021).
- Zapf, D. Emotion work and psychological well-being: A review of the literature and some conceptual considerations. Hum. Resour. Manag. Rev. 2002, 12, 237–268. [Google Scholar] [CrossRef]
- Moskowitz, J.T. Emotion and coping. In Emotions: Currrent Issues and Future Directions; Emotions and Social Behavior; Guilford Press: New York, NY, USA, 2001; pp. 311–336. [Google Scholar]
- Mayne, T.J. Emotions and health. In Emotions: Currrent Issues and Future Directions; Emotions and Social Behavior; Guilford Press: New York, NY, USA, 2001; pp. 361–397. [Google Scholar]
- Gross, J. Emotional expression in cancer onset and progression. Soc. Sci. Med. 1989, 28, 1239–1248. [Google Scholar] [CrossRef]
- Kemeny, M.E.; Shestyuk, A. Emotions, the neuroendocrine and immune systems, and health. In Handbook of Emotions, 3rd ed.; Guilford Press: New York, NY, USA, 2008; pp. 661–675. [Google Scholar]
- Consedine, N.S. Health-promoting and health-damaging effects of emotions the view from developmental functionalism. In Handbook of Emotions, 3rd ed.; Guilford Press: New York, NY, USA, 2008; pp. 676–690. [Google Scholar]
- Beal, D.J.; Trougakos, J.P.; Weiss, H.M.; Green, S.G. Episodic processes in emotional labor: Perceptions of affective delivery and regulation strategies. J. Appl. Psychol. 2006, 91, 1053–1065. [Google Scholar] [CrossRef] [Green Version]
- Hochschild, A.R. The Managed Heart: Commercialization of Human Feeling; University of California Press: Oakland, CA, USA, 2003. [Google Scholar]
- Brotheridge, C.; Grandey, A. Emotional labor and burnout: Comparing two perspectives of “people work”. J. Vocat. Behav. 2002, 60, 17–39. [Google Scholar] [CrossRef] [Green Version]
- Berthelsen, H.; Westerlund, H.; Hakanen, J.J.; Kristensen, T.S. It is not just about occupation, but also about where you work. Community Dent. Oral Epidemiol. 2017, 45, 372–379. [Google Scholar] [CrossRef] [Green Version]
- Wieclaw, J.; Agerbo, E.; Mortensen, P.B.; Burr, H.; Tüchsen, F.; Bonde, J.P. Work related violence and threats and the risk of depression and stress disorders. J. Epidemiol. Community Health 2006, 60, 771–775. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bakker, A.B.; Schaufeli, W.B.; Sixma, H.J.; Bosveld, W.; Dierendonck, D.V. Patient demands, lack of reciprocity, and burnout: A five-year longitudinal study among general practitioners. J. Organ. Behav. 2000, 21, 425–441. [Google Scholar] [CrossRef]
- De Jonge, J.; Le Blanc, P.M.; Peeters, M.C.W.; Noordam, H. Emotional job demands and the role of matching job resources: A cross-sectional survey study among health care workers. Int. J. Nurs. Stud. 2008, 45, 1460–1469. [Google Scholar] [CrossRef] [PubMed]
- Duarte, J.; Berthelsen, H.; Owen, M. Not all emotional demands are the same: Emotional demands from clients’ or co-workers’ relations have different associations with well-being in service workers. Int. J. Environ. Res. Public. Health 2020, 17, 7738. [Google Scholar] [CrossRef] [PubMed]
- Näring, G.; Vlerick, P.; de Ven, B.V. Emotion work and emotional exhaustion in teachers: The job and individual perspective. Educ. Stud. 2012, 38, 63–72. [Google Scholar] [CrossRef] [Green Version]
- Idris, M.A.; Dollard, M.F.; Yulita, Y. Psychosocial safety climate, emotional demands, burnout, and depression: A longitudinal multilevel study in the Malaysian private sector. J. Occup. Health Psychol. 2014, 19, 291–302. [Google Scholar] [CrossRef] [PubMed]
- Lorente Prieto, L.; Salanova Soria, M.; Martínez Martínez, I.; Schaufeli, W. Extension of the job demands-resources model in the prediction of burnout and engagement among teachers over time. Psicothema 2008, 20, 354–360. [Google Scholar]
- Sundin, L.; Hochwälder, J.; Lisspers, J. A longitudinal examination of generic and occupational specific job demands, and work-related social support associated with burnout among nurses in Sweden. Work Read. Mass 2011, 38, 389–400. [Google Scholar] [CrossRef] [Green Version]
- Van de Ven, B.; van den Tooren, M.; Vlerick, P. Emotional job resources and emotional support seeking as moderators of the relation between emotional job demands and emotional exhaustion: A two-wave panel study. J. Occup. Health Psychol. 2013, 18, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Van de Ven, B.; Vlerick, P. Testing the triple-match principle among technology employees. Eur. J. Work Organ. Psychol. 2013, 22, 658–669. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. The job demands-resources model: State of the art. J. Manag. Psychol. 2007, 22, 309–328. [Google Scholar] [CrossRef] [Green Version]
- Berthelsen, H.; Hakanen, J.J.; Westerlund, H. Copenhagen psychosocial questionnaire—A validation study using the job demand-resources model. PLoS ONE 2018, 13, e0196450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaufeli, W.B.; Bakker, A.B. Job demands, job resources, and their relationship with burnout and engagement: A multi-sample study. J. Organ. Behav. 2004, 25, 293–315. [Google Scholar] [CrossRef] [Green Version]
- Bean-Mellinger, B. Differences Between Task-Oriented Leaders & Relational-Oriented Leaders. 2019. Available online: https://smallbusiness.chron.com/differences-between-taskoriented-leaders-relationaloriented-leaders-35998.html (accessed on 28 July 2021).
- Lewin, K.; Lippitt, R.; White, R.K. Patterns of aggressive behavior in experimentally created “social climates”. J. Soc. Psychol. 1939, 10, 271–299. [Google Scholar] [CrossRef]
- Fleishman, E.A.; Peters, D.R. Interpersonal values, leadership attitudes and managerial “success”. Pers. Psychol. 1962, 15, 127–143. [Google Scholar] [CrossRef]
- Likert, R. The Human Organization: Its Management and Values; McGraw-Hill: New York, NY, USA, 1967. [Google Scholar]
- Fiedler, F.E. The contingency model: New direction for leadership utilization. J. Contemp. Bus. 1974, 3, 65–79. [Google Scholar]
- Burns, J.M. Leadership; Harper & Row: New York, NY, USA, 1978. [Google Scholar]
- Fleishman, E.A.; Harris, E.F. Patterns of leadership behavior related to employee grievances and turnover. Pers. Psychol. 1962, 15, 43–56. [Google Scholar] [CrossRef]
- Judge, T.A.; Piccolo, R.F.; Ilies, R. The forgotten ones? The validity of consideration and initiating structure in leadership research. J. Appl. Psychol. 2004, 89, 36–51. [Google Scholar] [CrossRef] [Green Version]
- Rosenberg, S.; Nelson, C.; Vivekananthan, P.S. A multidimensional approach to the structure of personality impressions. J. Pers. Soc. Psychol. 1968, 9, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Wojciszke, B.; Dowhyluk, M.; Jaworski, M. Moral competence-related traits: How do they differ? Pol. Psychol. Bull. 1998, 29, 283–294. [Google Scholar]
- Yukl, G. Effective leadership behavior: What we know and what questions need more attention. Acad. Manag. Perspect. 2012, 26, 66–85. [Google Scholar] [CrossRef]
- Behrendt, P.; Matz, S.; Göritz, A.S. An integrative model of leadership behavior. Leadersh. Q. 2017, 28, 229–244. [Google Scholar] [CrossRef]
- Yammarino, F.J.; Spangler, W.D.; Bass, B.M. Transformational leadership and performance: A longitudinal investigation. Leadersh. Q. 1993, 4, 81–102. [Google Scholar] [CrossRef]
- Gupta, V.K.; Huang, R.; Niranjan, S. A longitudinal examination of the relationship between team leadership and performance. J. Leadersh. Organ. Stud. 2010, 17, 335–350. [Google Scholar] [CrossRef]
- Tse, H.H.M.; Chiu, W.C.K. Transformational leadership and job performance: A social identity perspective. J. Bus. Res. 2014, 67, 2827–2835. [Google Scholar] [CrossRef]
- Jyoti, J.; Bhau, S. Impact of transformational leadership on job performance: Mediating role of leader-member exchange and relational identification. SAGE Open 2015, 5, 2158244015612518. Available online: https://journals.sagepub.com/doi/full/10.1177/2158244015612518 (accessed on 2 June 2021). [CrossRef] [Green Version]
- Bakker, A.B.; van Emmerik, H.; Euwema, M.C. Crossover of burnout and engagement in work teams. Work Occup. 2006, 33, 464–489. [Google Scholar] [CrossRef]
- Javed, B.; Abdullah, I.; Zaffar, M.A.; ul Haque, A.; Rubab, U. Inclusive leadership and innovative work behavior: The role of psychological empowerment. J. Manag. Organ. 2019, 25, 554–571. [Google Scholar] [CrossRef] [Green Version]
- Javed, B.; Khan, A.K.; Arjoon, S.; Mashkoor, M.; ul Haque, A. Openness to experience, ethical leadership, and innovative work behavior. J. Creat. Behav. 2020, 54, 211–223. [Google Scholar] [CrossRef]
- Joniaková, Z.; Jankelová, N.; Blštáková, J.; Némethová, I. Cognitive diversity as the quality of leadership in crisis: Team performance in health service during the COVID-19 pandemic. Healthcare 2021, 9, 313. [Google Scholar] [CrossRef] [PubMed]
- Jankelová, N.; Joniaková, Z.; Blštáková, J.; Skorková, Z.; Procházková, K. Leading employees through the crises: Key competences of crises management in healthcare facilities in coronavirus pandemic. Risk Manag. Healthc. Policy 2021, 14, 561–573. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.-C.; Chen, C.-F. Antecedents and consequences of nurses’ burnout: Leadership effectiveness and emotional intelligence as moderators. Manag. Decis. 2018, 56, 777–792. [Google Scholar] [CrossRef]
- Lee, K.-E. Moderating effects of leader-member exchange (LMX) on job burnout in dietitians and chefs of institutional foodservice. Nutr. Res. Pract. 2011, 5, 80–87. [Google Scholar] [CrossRef]
- Wu, H.; Qiu, S.; Dooley, L.M.; Ma, C. The relationship between challenge and hindrance stressors and emotional exhaustion: The moderating role of perceived servant leadership. Int. J. Environ. Res. Public. Health 2020, 17, 282. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; LePine, J.A.; Buckman, B.R.; Wei, F. It’s not fair … or is it? The role of justice and leadership in explaining work stressor-job performance relationships. Acad. Manag. J. 2014, 57, 675–697. [Google Scholar] [CrossRef]
- Cavanaugh, M.A.; Boswell, W.R.; Roehling, M.V.; Boudreau, J.W. An empirical examination of self-reported work stress among U.S. managers. J. Appl. Psychol. 2000, 85, 65–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Russell, L.M. An empirical investigation of high-risk occupations: Leader influence on employee stress and burnout among police. Manag. Res. Rev. 2014, 37, 367–384. [Google Scholar] [CrossRef]
- Syrek, C.J.; Apostel, E.; Antoni, C.H. Stress in highly demanding IT jobs: Transformational leadership moderates the impact of time pressure on exhaustion and work-life balance. J. Occup. Health Psychol. 2013, 18, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Ahern, S.; Loh, E. Leadership during the COVID-19 pandemic: Building and sustaining trust in times of uncertainty. BMJ Lead. 2020. Available online: https://bmjleader.bmj.com/content/leader/early/2020/09/29/leader-2020-000271.full.pdf (accessed on 5 September 2021). [CrossRef]
- Anderson, L. Leadership during crisis. Lead. Lead. 2018, 2018, 49–54. [Google Scholar] [CrossRef]
- Pejtersen, J.H.; Kristensen, T.S.; Borg, V.; Bjorner, J.B. The second version of the Copenhagen psychosocial questionnaire. Scand. J. Public Health 2010, 38, 8–24. [Google Scholar] [CrossRef]
- Baka, Ł. Kopenhaski Kwestionariusz Psychospołeczny (COPSOQ II): Podręcznik do Polskiej Wersji Narzędzia [Copenhagen Psychosocial Questionnaire (COPSOQ II). A Manual for the Polish Version of the Tool]; CIOP—PIB: Warszawa, Poland, 2019. [Google Scholar]
- Baka, Ł.; Basińska, B.A. Psychometryczne właściwości polskiej wersji Oldenburskiego Kwestionariusza Wypalenia Zawodowego (OLBI) [Psychometric properties of the Polish version of the Oldenburg Burnout Inventory (OLBI)]. Med. Pr. 2016, 67, 29–41. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics; Pearson Education: Boston, MA, USA, 2013. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 2nd ed.; Methodology in the Social Sciences; Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Hayes, A.F. PROCESS: A Versatile Computational Tool for Observed Variable Mediation, Mod-Eration, and Conditional Process Modeling (White Paper). Available online: http://www.afhayes.com/index.html (accessed on 28 July 2021).
- Lepine, J.A.; Podsakoff, N.P.; Lepine, M.A. A meta-analytic test of the challenge stressor-hindrance stressor framework: An explanation for inconsistent relationships among stressors and performance. Acad. Manag. J. 2005, 48, 764–775. [Google Scholar] [CrossRef] [Green Version]
- Bakker, A.B.; Sanz-Vergel, A.I. Weekly work engagement and flourishing: The role of hindrance and challenge job demands. J. Vocat. Behav. 2013, 83, 397–409. [Google Scholar] [CrossRef]
- Fillion, L.; Tremblay, I.; Truchon, M.; Côté, D.; Struthers, C.W.; Dupuis, R. Job satisfaction and emotional distress among nurses providing palliative care: Empirical evidence for an integrative occupational stress-model. Int. J. Stress Manag. 2007, 14, 1–25. [Google Scholar] [CrossRef]
- Rutter, D.R.; Fielding, P.J. Sources of occupational stress: An examination of British prison officers. Work Stress 1988, 2, 291–299. [Google Scholar] [CrossRef]
- Newmeyer, M.; Keyes, B.; Gregory, S.; Palmer, K.; Buford, D.; Mondt, P.; Okai, B. The Mother Teresa effect: The modulation of spirituality in using the CISM model with mental health service providers. Int. J. Emerg. Ment. Health 2014, 16, 251–258. [Google Scholar] [CrossRef] [Green Version]
- McCabe, R.; Nowak, M.; Mullen, S. Nursing careers: What motivated nurses to choose their profession? Aust. Bull. Labour 2005, 31, 384–406. [Google Scholar]
- McQueen, A.C.H. Emotional intelligence in nursing work. J. Adv. Nurs. 2004, 47, 101–108. [Google Scholar] [CrossRef]
- Bolton, S. Changing faces: Nurses as emotional jugglers. Sociol. Health Illn. 2001, 23, 85–100. [Google Scholar] [CrossRef]
- Chua, R.Y.J.; Ingram, P.; Morris, M.W. From the head and the heart: Locating cognition- and affect-based trust in managers’ professional networks. Acad. Manag. J. 2008, 51, 436–452. [Google Scholar] [CrossRef] [Green Version]
- Connelly, B.L.; Crook, T.R.; Combs, J.G.; Ketchen, D.J.; Aguinis, H. Competence- and integrity-based trust in interorganizational relationships: Which matters more? J. Manag. 2018, 44, 919–945. [Google Scholar] [CrossRef] [Green Version]
- Lui, S.S.; Ngo, H. The role of trust and contractual safeguards on cooperation in non-equity alliances. J. Manag. 2004, 30, 471–485. [Google Scholar] [CrossRef]
- Sitkin, S.B.; Roth, N.L. Explaining the limited effectiveness of legalistic “remedies” for trust/distrust. Organ. Sci. 1993, 4, 367–392. [Google Scholar] [CrossRef]
- Gausdal, A.H.; Makarova, J. Trust and safety onboard. WMU J. Marit. Aff. 2017, 2, 197–217. [Google Scholar] [CrossRef]
- Bass, B.I.; Cigularov, K.P.; Chen, P.Y.; Henry, K.L.; Tomazic, R.G.; Li, Y. The effects of student violence against school employees on employee burnout and work engagement: The roles of perceived school unsafety and transformational leadership. Int. J. Stress Manag. 2016, 23, 318–336. [Google Scholar] [CrossRef]
- Rugulies, R.; Sørensen, J.K.; Madsen, I.E.H.; Nordentoft, M.; Sørensen, K.; Framke, E. Can leadership quality buffer the association between emotionally demanding work and risk of long-term sickness absence? Eur. J. Public Health 2021. [Google Scholar] [CrossRef]
- Madsen, I.E.H.; Hanson, L.L.M.; Rugulies, R.; Theorell, T.; Burr, H.; Diderichsen, F.; Westerlund, H. Does good leadership buffer effects of high emotional demands at work on risk of antidepressant treatment? A prospective study from two Nordic countries. Soc. Psychiatry Psychiatr. Epidemiol. 2014, 49, 1209–1218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Engel, S.; Wörfel, F.; Maria, A.S.; Wolter, C.; Kleiber, D.; Renneberg, B. Leadership climate prevents emotional exhaustion in German police officers. Int. J. Police Sci. Manag. 2018, 20, 217–224. [Google Scholar] [CrossRef]


| Measurement 1 | Measurement 2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | SKE | KUR | M | SD | SKE | KUR | t | p | d | |
| (EX) Exhaustion | 2.18 | 0.51 | −0.383 | −0.300 | 2.13 | 0.49 | −0.326 | −0.049 | 2.968 | 0.003 | 0.095 |
| (QL) Quality of leadership | 60.81 | 20.36 | −0.208 | 0.096 | 64.38 | 19.57 | −0.143 | 0.015 | 5.431 | <0.001 | 0.179 |
| (TM) Trust in management | 61.56 | 16.12 | 0.006 | 0.413 | 64.41 | 17.35 | 0.002 | −0.390 | 5.233 | <0.001 | 0.170 |
| (QD) Quantitative demands | 35.01 | 16.81 | 0.179 | −0.146 | 33.30 | 16.93 | −0.034 | −0.544 | 3.014 | 0.003 | 0.101 |
| (ED) Emotional demands | 62.45 | 21.26 | −0.344 | −0.357 | 60.57 | 21.79 | −0.273 | −0.393 | 2.920 | 0.004 | 0.087 |
| (HE) Hiding emotions demands | 58.98 | 21.58 | −0.226 | −0.313 | 59.54 | 21.10 | −0.101 | −0.349 | 0.808 | 0.419 | 0.026 |
| Measurement 1 | Measurement 2 | |
|---|---|---|
| Exhaustion (EX1) | Exhaustion (EX2) | |
| (QL) Quality of leadership | −0.313 ** | −0.347 ** |
| (TM) Trust in management | −0.370 ** | −0.399 ** |
| (QD) Quantitative demands | 0.421 ** | 0.431 ** |
| (ED) Emotional demands | 0.024 | 0.021 |
| (HE) Hiding emotions demands | 0.131 ** | 0.081 ** |
| Variable | Significance of the Model | F | p | R2 |
|---|---|---|---|---|
| Significance of the Interaction | ||||
| (QD) quantitative demands | model | 58.0285 | <0.001 | 0.2521 |
| interaction for quantitative demands | 3.8993 | 0.0485 | ||
| (ED) emotional demands | model | 54.9471 | <0.001 | 0.2418 |
| interaction for emotional demands | 2.1513 | 0.1427 | ||
| (HE) hiding emotions demands | model | 54.4765 | <0.001 | 0.2405 |
| interaction for hiding emotions demands | 0.4685 | 0.4938 |
| Moderator 1 | Moderator 2 | SE | p | LLCI | ULCI |
|---|---|---|---|---|---|
| (QL) Quality of Leadership | (TM) Trust in Management | ||||
| (QL) M − 1SD | (TM) M − 1SD | 0.0812 | 0.0422 | 0.0029 | 0.1596 |
| (QL) M − 1SD | (TM) M | 0.1408 | 0.0005 | 0.0622 | 0.2194 |
| (QL) M − 1SD | (TM) M + 1SD | 0.2004 | 0.0022 | 0.0720 | 0.3288 |
| (QL) M | (TM) M − 1SD | 0.1078 | 0.0114 | 0.0243 | 0.1913 |
| (QL) M | (TM) M | 0.1299 | 0.0000 | 0.0748 | 0.1851 |
| (QL) M | (TM) M + 1SD | 0.1521 | 0.0002 | 0.0735 | 0.2306 |
| (QL) M + 1SD | (TM) M − 1SD | 0.1344 | 0.0389 | 0.0069 | 0.2618 |
| (QL) M + 1SD | (TM) M | 0.1190 | 0.0048 | 0.0365 | 0.2016 |
| (QL) M + 1SD | (TM) M + 1SD | 0.1037 | 0.0138 | 0.0212 | 0.1863 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baka, Ł.; Ścigała, D.; Grala, K. Not All Demands Are Exhausted for Healthcare Workers. A Cross-Lagged Study on the Buffering Effect of Leadership Resources. Sustainability 2021, 13, 10623. https://doi.org/10.3390/su131910623
Baka Ł, Ścigała D, Grala K. Not All Demands Are Exhausted for Healthcare Workers. A Cross-Lagged Study on the Buffering Effect of Leadership Resources. Sustainability. 2021; 13(19):10623. https://doi.org/10.3390/su131910623
Chicago/Turabian StyleBaka, Łukasz, Dawid Ścigała, and Krzysztof Grala. 2021. "Not All Demands Are Exhausted for Healthcare Workers. A Cross-Lagged Study on the Buffering Effect of Leadership Resources" Sustainability 13, no. 19: 10623. https://doi.org/10.3390/su131910623
APA StyleBaka, Ł., Ścigała, D., & Grala, K. (2021). Not All Demands Are Exhausted for Healthcare Workers. A Cross-Lagged Study on the Buffering Effect of Leadership Resources. Sustainability, 13(19), 10623. https://doi.org/10.3390/su131910623






